Abstract
Background
Needlescopic appendectomies (NA) have been performed since the 1990s. We sought to systematically analyze trials comparing NA with laparoscopic appendectomies (LA) in the management of appendicitis.
Methods
We performed a systematic review of the literature. We compared and analyzed clinical trials on NA and LA to generate summative data expressed as standardized mean differences (SMD).
Results
Of 5 retrieved trials from the electronic database 2 trials involving 412 patients met our inclusion criteria. In the fixed-effects models, NA took longer than LA, and this time difference was statistically significant: SMD 0.20 min, 95% confidence interval 0.01–0.40, p = 0.030, z1 = 2.09. In both fixed-and random-effects models, the difference in total hospital stay and in perioperative complications between the NA and LA groups were nonsignificant. Furthermore, in both fixed-and random-effects models, NA was associated with a higher conversion rate to open appendectomy than LA. There was no heterogeneity between the trials (Q = 0.34, p = 0.55).
Conclusion
Needlescopic appendectomy can be a safe and effective procedure for the management of appendicitis. It is comparable to LA in terms of hospital stay and perioperative complications. However, NA is associated with a longer duration of surgery and a higher conversion rate, indicating technical challenges of the procedure. Before recommending routine use of the needlescopic technique for appendectomy, a major multicentre randomized controlled trial is necessary.
Abstract
Contexte
On effectue des appendicectomies au trocart optique (needlescope) depuis les années 1990. Nous avons voulu analyser de manière systématique les études qui ont comparé les appendicectomies au trocart optique aux appendicectomies laparoscopiques dans la prise en charge de l'appendicite.
Méthodes
Nous avons procédé à une revue systématique de la littérature. Nous avons comparé et analysé les études cliniques ayant porté sur les appendicectomies au trocart optique et les appendicectomies laparoscopiques afin de générer des données sommatives exprimées sous forme de différence moyenne standardisée (DMS).
Résultats
Sur 5 études recensées à partir de bases de données électroniques, 2 regroupant 412 patients répondaient à nos critères d'inclusion. Selon les modèles à effets fixes, l'appendicectomie au trocart optique a pris plus de temps que l'appendicectomie laparoscopique et cette différence de temps s'est révélée statistiquement significative (DMS 0,20 minute; intervalle de confiance à 95 %, 0,01–0,40; p = 0,030; zl = 2,09). Dans les modèles, tant à effets fixes qu'aléatoires, les différences de durée totale de l'hospitalisation et de complications périopératoires entre les groupes soumis à l'appendicectomie au trocart optique et à l'appendicectomie laparoscopique n'ont pas été significatives. De plus, dans les modèles à effets fixes et aléatoires, l'appendicectomie au trocart optique a été associée à un taux de conversion plus élevé à l'appendicectomie ouverte, comparativement à l'appendicectomie laparoscopique. On n'a noté aucune hétérogénéité entre les études (Q = 0,34; p = 0,55).
Conclusion
L'appendicectomie au trocart optique peut être une technique sécuritaire et efficace pour la prise en charge de l'appendicite. Elle est comparable à l'appendicectomie laparoscopique pour ce qui est de la durée du séjour hospitalier et des complications périopératoires. Toutefois, l'appendicectomie au trocart optique demande plus de temps et est associée à un taux de conversion plus élevé, ce qui témoigne des défis techniques de l'intervention. Avant de recommander l'utilisation d'emblée d'une technique au trocart optique pour l'appendicectomie, il faudra procéder à une grande étude multicentrique contrôlée et randomisée sur ce type d'intervention.
Open appendectomy performed through a grid iron incision in the right lower quadrant was first introduced in the 19th century1,2 and remained mainly unchallenged until the introduction of laparoscopic appendectomy (LA) in 1983 by Semm,3,4 a gynecologist. This was an important change in the management of appendicitis owing to advantages like improved wound-healing,5 shorter hospital stay,6 markedly reduced postoperative pain7 and good cosmetic results,8 all all of which lead to an early return to normal daily activities.9,10 The launch of needlescopic instruments, defined as those 3-mm or less in diameter, sparked further excitement in the 1990s.11 The first successful needlescopic appendectomy (NA) was reported in 1994.12 In theory, NA is beneficial to patients because of the smaller trocar wounds and hence less tissue trauma associated with this minimally invasive approach. It was therefore intriguing to evaluate NA further. Studies comparing NA and LA have been reported, but their conclusions have been limited by study design, study type or study sample.
We sought to use meta-analysis as a tool to compare the outcomes of LA and NA with respect to duration of surgery, total hospital stay, conversion rate and perioperative complications. The specific questions we sought to answer are as follows:
Does NA significantly reduce the duration of surgery?
What is the difference in total hospital stay associated with these techniques?
What is the conversion rate in NA?
Does NA reduce the incidence of perioperative complications?
METHODS
We identified relevant studies on NA versus LA published between January 1997 and January 2007 in the MEDLINE, EMBASE, CINAHL, Cochrane library and PubMed databases. We used the terms “trials on needlescopic appendectomy/appendicectomy,” “minimally invasive appendectomy/appendicectomy” and “key hole surgery for appendicitis” in combination with the medical subject headings “needlescopic versus conventional laparoscopic appendicectomy” and “minimal versus conventional laparoscopic appendectomy/appendicectomy.” We also obtained relevant articles referenced in these studies. We used the “related article” function to widen our search criteria, and we reviewed all abstracts, comparative studies, nonrandomized trials and citations scanned.
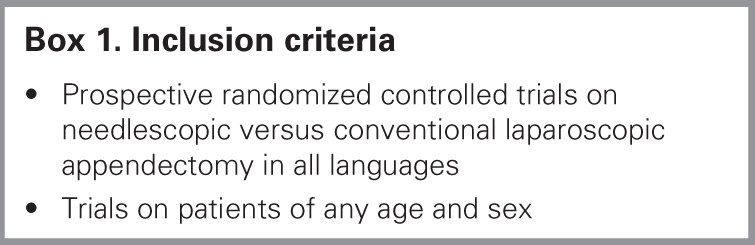
We reviewed each article to assess eligibility for inclusion in this systematic review. Our inclusion criteria are listed in Box 1. We analyzed randomized controlled trials comparing NA and LA. We analyzed 4 outcome variables: duration of surgery, hospital stay, conversion rate and perioperative complications. Two of us (M.M.S. and M.A.K.) extracted the data independently, with complete agreement. We defined complication as a condition that developed due to surgery and required either repeat surgery or further medical treatment or prolonged the length of stay in hospital. Our data included the following complications: wound infection (with evidence of cellulites and positive culture), wound abscess (which required incision and drainage), intra-abdominal abscess (which required either surgical or radiological drainage), urinary tract infection (where urine culture was positive), chest infection (confirmed on chest radiography), prolonged ileus (no bowel sounds after 72 hours), relaparotomy for any reason and intraoperative or postoperative destabilizing hemorrhage. The criteria to define NA and LA are described in Box 2.
Box 1.
Box 2.

A senior statistician (E.C.) performed statistical analyses using Excel 2003 for Windows XP (Microsoft). For continuous data (e.g., duration of surgery, hospital stay), we used the Hedges g statistic to calculate standardized mean differences (SMDs). We combined the SMDs using inverse variance weights in the fixed-effects model and the DerSimonian–Laird method in the random-effects model.12 We summarized binary data (e.g., complications, recurrence) as risk ratios (RR) and combined them using the Mantel–Haenszel method under the fixed-effects model and the DerSimonian–Laird method under the random-effects model. In each case, we performed a heterogeneity test to determine whether the fixed-effects model was appropriate. When standard deviations (SDs) were not reported in the studies, we estimated SDs either from ranges or p values.13 We used forest plots for the graphical display of results from this review. Subgroup and sensitivity analyses were not feasible owing to the limited number of studies included in our review. Publication bias was also difficult to assess for the same reason.
RESULTS
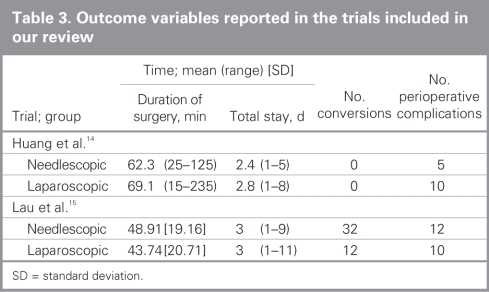
Figure 1 depicts our search results. We retrieved 5 trials comparing NA and LA involving a total of 1098 patients from the electronic databases. Two randomized controlled trials14,15 involving 412 patients met our inclusion criteria (Box 1). We excluded 3 trials9,16,17 owing to the reasons mentioned in Table 1. Characteristics of each trial are provided in Table 2. There were a total of 200 patients in the needlescopic group and 212 patients in the laparoscopic group. The outcome variables extracted from these trials are shown in Table 3.

Fig. 1. Flow chart outlining the literature search.
Table 1
Table 2
Table 3
Methodological quality of included studies
The methodological quality of included trials is explained comprehensively in Table 4. We used the Mantel– Haenszel fixed-effects model to compute robustness and susceptibility to any outliers among these trials. The allocation concealment and blinding of investigators or assessors were not clearly reported in the studies; consequently, we considered the methodological quality of the trials to be inadequate, and the results of our review may be considered biased.
Table 4
Duration of surgery
In the fixed-effects models, NA lasted longer than LA, and this time difference was statistically significant: fixed-effects model SMD 0.20 minutes, 95% confidence interval (CI) 0.01–0.40, p = 0.030, z1 = 2.09. However, in the random-effects model, statistically there was no difference between the 2 approaches: SMD 0.13 minutes, 95% CI –0.23 to 0.50, p = 0.48, z1 = 0.70 (Fig. 2). There was no heterogeneity between the trials (Q = 1.86, p = 0.17).
Fig. 2. Comparison of the duration of needlescopic and laparoscopic appendectomy. CI = confidence interval.
Hospital stay
In both fixed-and random-effects models, the difference in total hospital stay between the NA and LA groups was statistically nonsignificant: fixed-effects model SMD –0.03 d, 95% CI –0.20 to 0.16, p = 0.74, z1 = –0.32 and random-effects model SMD –0.007 d, 95% CI –0.09 to 0.7, p = 0.87, z1 = -0.16 (Fig. 3). There was no heterogeneity between the trials (Q = 0.80, p = 0.36).
Fig. 3. Comparison of the hospital stays of patients who had needlescopic versus laparoscopic appendectomies. CI = confidence interval.
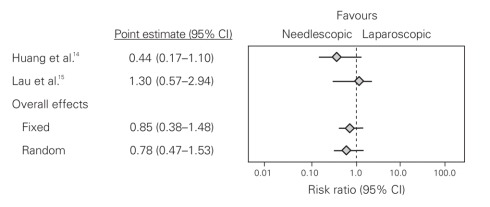
Perioperative complications
In both fixed-and random-effects models, the difference in the perioperative complication rate between the NA and LA groups was statistically nonsignificant: fixed-effects model RR 0.80, 95% CI 0.44–1.48, p = 0.49, z1 = –0.68 and random-effects model RR 0.85, 95% CI 0.47–1.53, p = 0.59, z1 = –0.53 (Fig. 4). There was no heterogeneity between the trials (Q = 2.99, p = 0.08).
Fig. 4. Comparison of the preioperative complications experienced by patients who had needlescopic versus laparoscopic appendectomies. CI = confidence interval.
Conversion rate
In both fixed and random-effects models, NA was associated with a higher conversion rate to open appendectomy than LA, which was statistically significant: fixed-effects model RR 2.80, 95% CI 1.50–5.23, p = 0.001, z1 = 3.25 and random-effects model RR 2.80, 95% CI 1.51–5.21, p = 0.001, z1 = 3.26 (Fig. 5). There was no heterogeneity between the trials (Q = 0.34, p = 0.55).
Fig. 5. Comparison of the conversion rate to open appendectomy associated with needlescopic and laparoscopic appendectomies. CI = confidence interval.
DISCUSSION
Needlescopic appendectomy is an evolving technique. General surgeons are practising it with great caution owing to lack of level-I evidence. Our systematic review attempts to provide some evidence on this issue. It is the hope of those pioneering this field that it will extend the benefits already proven for LA versus open appendectomy.18 For example, the use of smaller 2- to 3-mm ports, rather than 5- or 10-mm ports, will further hasten recovery and reduce postoperative pain and length of hospital stay.19 In experienced hands, NA is a feasible procedure and can be performed safely in select patients, especially in young girls, for the treatment of acute appendicitis. It is less invasive and cosmetically superior to LA.20 We observed no difference in perioperative complications between the 2 techniques or in the resulting length of stay in hospital. The higher conversion rate to open appendectomy observed in the NA group is indicative of the initial technical difficulties surgeons have to face using finer instruments. However, with current instrumentation and the skill level of general surgeons, NA understandably will take longer than the more traditional laparoscopic procedures, and after a learning curve, improved and high-quality results may be achieved.
Advocates of NA believe that an element of surgical trauma is due to the skin wound and tissue handling. If we can operate with a smaller skin wound and more gentle tissue handling without compromising access, a better outcome is anticipated. Thus, surgeons must strike a balance between trauma secondary to surgery and adequate access. Our systematic review may pave the way for NA, a less invasive procedure for acute appendicitis, but further exploration and investigation are required. Our study shows that NA has some statistically significant benefits over LA, and after achieving the necessary technical experience, surgeons can consider performing this procedure in patients with acute appendicitis.
To our knowledge, our systematic review is the only comprehensive review of NA to date. It highlights the need for a major multicentre double-blind prospective randomized controlled trial on NA because in this review only 2 randomized controlled trials involving a small number of patients with various stages of appendicitis were retained for analysis. In the meantime, NA may be considered an alternate option for removal of the appendix.
Contributors: Drs. Sajid and Baig designed the study. Drs. Sajid and Khan acquired the data, which Drs. Sajid, Khan and Cheek analyzed. Drs. Sajid and Baig wrote the article, which Drs. Khan and Cheek reviewed. All authors approved the final version for publication.
Competing interests: None declared.
Accepted for publication Dec. 11, 2007
Correspondence to: Dr. M.S. Sajid SpR General Surgery Worthing & Southlands Hospitals NHS Trust Worthing, West Sussex BN11 2DH United Kingdom fax 01903 285 052 surgeon1wrh@hotmail.com
References
- 1.Fitz RH. Perforating inflammation of vermiform appendix: with special reference to its early diagnosis and treatment. AmJ Med Sci 1886;92:321-46.
- 2.McBurney C. The incision made in the abdominal wall in cases of appendicitis. Ann Surg 1894;20:38-43. Available: www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1493708 (accessed 2009 Feb. 25). [DOI] [PMC free article] [PubMed]
- 3.Semm K. Endoscopic appendectomy. Endoscopy 1983;15:59-64. [DOI] [PubMed]
- 4.Berry J Jr, Malt RA. Appendicitis near its centenary. Ann Surg 1984;200:567-75. [DOI] [PMC free article] [PubMed]
- 5.Ortega AE, Hunter JG, Peters JH, et al. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. Am J Surg 1995;2:208-12. [DOI] [PubMed]
- 6.Tang E, Ortega AE, Anthone GJ. Intraabdominal abscess following laparoscopic and open appendectomies. Surg Endosc 1996;10:327-8. [DOI] [PubMed]
- 7.Chung RS, Rowland DY, Li P. A meta-analysisof randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg 1999;177:250-6. [DOI] [PubMed]
- 8.Azaro EM, Amaral PC, Ettinger JE. Laparoscopic versus open appendectomy: a comparative study. JSLS 1999;3:279-83. [PMC free article] [PubMed]
- 9.Croce E, Olmi S, Azzola M, et al. Laparoscopic appendectomy and minilaparoscopic approach; a retrospective review after 8 years' experience. JSLS 1999;3:285-92. [PMC free article] [PubMed]
- 10.Heikkinen TJ, Haukipuro K, Hulkko A. Cost-effective appendectomy. Open or laparoscopic? A prospective randomized study. Surg Endosc 1998;12:1204-8. [DOI] [PubMed]
- 11.Gagner M, Garcia-Ruiz A. Technical aspects of minimally invasive abdominal surgery performed with needlescopic instruments. Surg Laparosc Endosc 1998;8:171-9. [PubMed]
- 12.Cochrane RA, Hay DJ. A microlap appendectomy: case report. Minim Invasive Ther Allied Technol 1997;6:168-9.
- 13.Egger M, Smith GD, Altman DG. Systematic reviews in healthcare. London: BMJ Publishing; 2006.
- 14.Huang M, Wei P, Wu C, et al. Needlescopic, laparoscopic and open appendectomy: a comparative study. Surg Laparosc Endosc Percutan Tech 2001;11:306-12. [DOI] [PubMed]
- 15.Lau DHW, Yau KK, Chung CC, et al. Comparison of needlescopic appendectomy versus conventional laparoscopic appendectomy. A randomized controlled trial. Surg Laparosc Endosc Percutan Tech 2005;15:75-9. [DOI] [PubMed]
- 16.Mostafa G, Matthews BD, Sing RF, et al. Mini-laparoscopic versus laparoscopic approach to appendectomy. BMC Surg 2001;1:4. [DOI] [PMC free article] [PubMed]
- 17.Chock A, Seslar S, Stoopen E, et al. Needlescopic appendectomy. Surg Endosc 2003;17:1451-3. [DOI] [PubMed]
- 18.Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech 2007;17:245-55. [DOI] [PubMed]
- 19.Matthews BD, Mostafa G, Harold KL, et al. Minilaparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech 2001;11:351-5. [DOI] [PubMed]
- 20.Schier F. Laparoscopic appendectomy with 1.7 mm instruments. Pediatr Surg Int 1998;14:142-3. [DOI] [PubMed]