Abstract
Background
Trauma care benefits from the use of imaging technologies. Trauma patients and trauma team members are exposed to radiation during the continuum of care. Knowledge of exposure amounts and effects are important for trauma team members.
Methods
We performed a review of the published literature; keywords included “trauma,” “patients,” “trauma team members,” “wounds,” “injuries,” “radiation,” “exposure,” “dose” and “computed tomography” (CT). We also reviewed the Board on Radiation Effects Research (BEIR VII) report, published in 2005 and 2006.
Results
We found no randomized controlled trials or studies. Relevant studies demonstrated that CT accounts for the single largest radiation exposure in trauma patients. Exposure to 100 mSv could result in a solid organ cancer or leukemia in 1 of 100 people. Trauma team members do not exceed the acceptable occupation radiation exposure determined by the National Council of Radiation Protection and Management. Modern imaging technologies such as 16- and 64-slice CT scanners may decrease radiation exposure.
Conclusion
Multiple injured trauma patients receive a substantial dose of radiation. Radiation exposure is cumulative. The low individual risk of cancer becomes a greater public health issue when multiplied by a large number of examinations. Though CT scans are an invaluable resource and are becoming more easily accessible, they should not replace careful clinical examination and should be used only in appropriate patients.
Abstract
Contexte
La traumatologie bénéficie des technologies d'imagerie, mais leur utilisation expose les patients polytraumatisés et les équipes de traumatologie à des radiations durant le continuum des soins. Il est important pour les membres des équipes soignantes de savoir à quelles quantités ils sont exposés et d'en connaître les effets.
Méthodes
Nous avons procédé à une revue de la littérature publiée à ce sujet à partir de mots clés, y compris « trauma », « patients », « trauma team members », « wounds », « injuries », « radiation », « exposure », « dose » et « computed tomography (CT) ». Nous avons aussi passé en revue les rapports du Board on Radiation Effects Research (BEIR VII), publiés en 2005 et 2006.
Résultats
Nous n'avons pas trouvé d'essais ni d'études randomisés et contrôlés. Les études pertinentes ont révélé que la tomographie représente la plus importante source d'exposition aux radiations chez les polytraumatisés. L'exposition à 100 mSv pourrait causer le cancer d'un organe plein ou la leucémie chez 1 personne sur 100. Les équipes de traumatologie ne sont pas soumises à une exposition excédant les seuils d'exposition professionnelle acceptables établis par le National Council of Radiation Protection and Management. Les technologies modernes d'imagerie, comme les tomodensitomètres à 16 et à 64 coupes, pourraient réduire l'exposition à la radiation.
Conclusion
Les polytraumatisés reçoivent une dose substantielle de radiations. L'exposition à la radiation est cumulative. Le faible risque individuel de cancer devient un problème de santé publique plus important lorsqu'il est multiplié par un grand nombre d'examens. Bien que la tomodensitométrie demeure une ressource inestimable et de plus en plus accessible, elle ne doit pas se substituer à un examen clinique attentif et on la réservera aux patients appropriés.
Initial assessment and resuscitation in trauma addresses immediate life-threatening injury. The principles are well described in the Advanced Trauma Life Support manual (ATLS).1 Adjuncts to the initial evaluation are frequent careful clinical examination, ultrasound and diagnostic peritoneal lavage. With advances in imaging technology, computed tomography (CT) and occasionally fluoroscopy are now used to evaluate those areas that are not readily amenable to accurate clinical examination or plain radiography. Widespread application of imaging technology requires knowledge of levels of radiation exposure to patients and trauma team members. Understanding the potential risks of this exposure is essential.
The objective of our study was to describe radiation exposure for patients and trauma team members and to examine the potential risk of medical imaging radiation exposure. Our intention was to bring awareness of this issue to all health care workers, especially the members of the trauma team.
METHODS
We performed a literature review using MEDLINE, EMBASE, PubMed and the Cochrane databases. We searched the following keywords: “computed tomography,” “CT,” “x-rays,” “radiographs,” “angiography,” “fluoroscopy,” “radiology,” “radiation,” “radiation dose,” “effective dose,” “radiation exposure,” “dosimetry,” “trauma,” “polytrauma,” “wounds” and “injuries.” We limited studies to those involving humans. We identified additional papers by cross-referencing bibliographies of retrieved articles. We reviewed the Board on Radiation Effects Research (BEIR VII) report, first published in 2005 by the National Research Council2 with phase 2 published in 2006,3 in preparing this manuscript. Finally, we reviewed postgraduate work leading to a master's thesis on dosimetry associated with newer CT imaging technologies.4 We reviewed relevant studies dating from 1980 to 2006. There were no randomized controlled trials.
RESULTS
Definitions
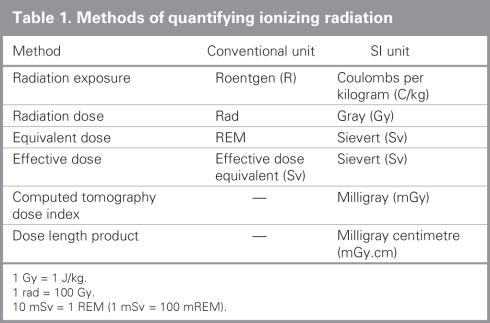
Methods used to quantify ionizing radiation are summarized in Table 1.
Table 1
Radiation exposure (Roentgens) is the concentration of radiation at a specific point in air and is the ionization produced in a specific volume of air.5 It does not reveal how much energy the irradiated tissues absorb.
Radiation dose or absorbed dose (Rads or Grays) describes the amount of energy absorbed per unit mass at a specific point. It does not account for the differing radiation sensitivity of organs and therefore cannot be used for comparisons between examinations in different parts of the body.5–7
Equivalent dose is a modification of the absorbed dose that incorporates weighting factors to account for the different biologic effects of various sources of radiation. These are referred to as REMs in conventional units and Sieverts in SI units: 100 REM = 1 Sievert.
Effective dose, also referred to in both systems as Sieverts, takes into account where the radiation dose is being absorbed and attempts to estimate the whole-body dose that would be required to produce the same risk as the partial-body dose that was actually delivered in a localized radiologic procedure. It is currently the best measurement available as it allows comparison with other types of radiation exposure, including natural background radiation. Specific to CT scans is the CT dose index and dose length product.
CT dose index (CTDI) represents the dose in a single slice.
Dose length product (DLP) is the product of the CTDI and the scan length.
Sources of radiation exposure
Background radiation refers to about 1.0–3.0 mSv per year and accounts for 80%–85% of all radiation exposure.7 Both cosmic/solar radiation and emissions from radon account for natural exposure in roughly equal amounts. Human sources of radiation exposure account for 15%–20% of the annual population exposure, the major source being medical imaging.8–10
Radiation dose in trauma patients
Trauma patients undergo a large number of radiologic studies during their stays in hospital. Kim and colleagues9 reported that in a series of critically ill trauma patients at the University of Pennsylvania (mean injury severity score [ISS] 32.2, standard deviation [SD] 15.0), the average number of studies per patient was 70.1 (SD 29.0) plain film radiographs, 7.8 (SD 4.1) CT scans, 2.5 (SD 2.6) fluoroscopic studies and 0.065 (SD 0.33) nuclear medicine studies. The cumulative effective radiation dose per patient over the course of their stays (mean 2 mo) was 106 (SD 56) mSv per patient. The authors focused on the most severely injured patients, with stays in the surgical intensive care unit (ICU) lasting longer than 30 days.
Consistent with previous statistics from the literature, Kim and colleagues9 also found that CT scans constituted less than 10% of the total number of studies performed but accounted for two-thirds of the radiation dose.11 Fluoroscopic studies such as angioembolization for both diagnosis and treatment of injuries are also used frequently in these trauma patients, whereas nuclear medicine studies are uncommon.9 The strongest predictor of the cumulative effective radiation dose was the number of CT scans obtained.
In Kim's study,9 the mean cumulative effective dose in critically ill trauma patients was 30 times higher than the average yearly radiation dose from all sources for individuals in the US. Wedegartner and colleagues12 studied radiation exposure from whole-body multislice CT and organ-specific CT in polytrauma patients. They found that the effective dose ranged from 5 mSv for organ-specific scans to 20 mSv for whole-body scans.
Ott and coworkers13 recently reported a median exposure of 68 mREM (0.68 mSv) in 224 trauma (mixed adult and pediatric) patients (mean ISS 16). The number of patients undergoing CT was not provided. In their study, the dosimeter was placed on the patients' wrists, thus removing it from the beam in most cases of trauma CT imaging where the arms are extended. Whole-body exposure would thus be higher. Despite this, 22 patients had exposures greater than 1000 mREM (10 mSv) and 2 patients had exposures greater than 10 000 mREM (100 mSv). Previous findings in the pediatric population have led to suggestions for more restrictive use of CT in children.14–16
In 2007, a series of 172 major trauma patients requiring admission were studied at the Sunnybrook Health Sciences Centre in Toronto, Ont., with a mean ISS of 22.7. Dosimeters were placed on the neck, chest and groin. Mean injury severity scores were greater than 20. Total effective dose for patients was 22.7 mSv. In contrast with the study by Kim and colleagues,9 the Sunnybrook series included all trauma service admissions, not just patients with a prolonged stay in the ICU. The ICU patients in Kim's study averaged 5 times as many plain radiographs and twice as many CT scans. Tien and colleagues'17 findings were consistent, as 22% of the Sunnybrook patients had thyroid doses greater than 100 mSv (mean 156 mSv).
Computed tomography
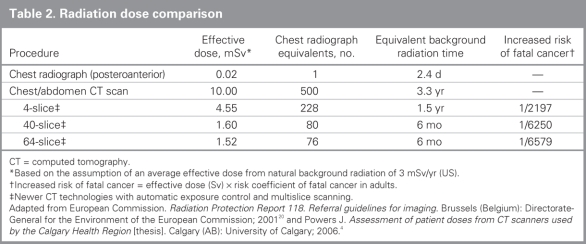
Since their introduction more than 30 years ago, and more notably since the introduction of spiral CT in the late 1980s, CT scans have become central to imaging evaluation.6 Improvements in speed and resolution have led to lower thresholds for the use of CT and new applications.6,7 The annual number of CT examinations in the United States has risen from 3.6 million in 1980 to 33 million in 1998.18 One whole-body CT scan (single or 4-slice) may involve an effective dose equal to 500 chest radiographs and is equivalent to the average national background radiation received over a period of more than 3 years (Table 2).19
Table 2
The dose delivered by single-slice CT ranges from less than 1 mSv to more than 30 mSv per body region studied.8,10 If there are multiple scans of the same area to study organ perfusion (phases), the total effective radiation dose is multiplied by the number of phases. The doses from a single full-body single-slice CT examination are about 10 mSv.20 Whole-body dose for chest/abdomen CT protocols for scanners using automated exposure controls appear to be reduced4 (Table 2).
Radiation exposure to trauma team members
Trauma team members and paramedical personnel resuscitating trauma patients are exposed to some radiation.19,21–23 Exposure occurs when initial radiographs are taken during resuscitation.21,24 Additional exposures may occur while supporting patients during adjunct investigations. The overall radiation dose accumulated by each team member depends on the number of films, imaging modality and distance from the radiating source.19,24
When the ATLS protocol for radiographs is followed during the initial resuscitation phase, residents, based on historical work hours, are exposed to more ionizing radiation than both nurses and emergency physicians.24 They received an average dose of 0.20 (SD 0.28) mSv per year compared with 0.035 (SD 0.02) mSv per year among nurses and 0.033 (SD 0.02) mSv per year among emergency physicians. These results represent the amount of radiation that one would receive without any protective garments, as Ciraulo and colleagues24 performed the study with the dosimeters on the outside of the lead garment. Presumably, the effective dose of radiation to trauma team members would be lower than that mentioned previously. Nurses appear to receive a greater amount of radiation per film than residents and emergency physicians: 4.0 × 10-4 mSv compared with 2.6 × 10-4 mSv for residents and 0.1 × 10-4 mSv for emergency physicians. Nurses are usually closer to the field of irradiation during resuscitations and radiologic investigations,21,24 drawing blood, administering medications, inserting catheters, etc. The trauma team members were not exposed to doses exceeding those recommended for background exposure25 or the National Council of Radiation Protection and Management acceptable occupational radiation exposure level of 50 mSv per year.26,27
Effects of radiation
Radiation is associated with 2 types of risk.13 Stochastic risks are the effects of chance mutations. These occur at random but may be assigned a probability based on radiation exposure (e.g., radiation-induced cancers). Current models suggest a linear relation between dose and biological effect with no safe threshold. Deterministic risks are predictable effects that occur with radiation exposure and increase in direct relation to exposure (e.g., sunburn).
Exposures in medical imaging are potentially associated with stochastic risks of carcinogenesis, specifically the development of leukemia, solid organ and thyroid cancers.24,28 Other long-term effects attributed to irradiation are cataracts, sterilization and birth defects.25,29 The 2005 recommendation of the International Commission on Radiological Protection lists an acceptable occupational radiation exposure level of 1 mSv per year.30,31 In 1990, the lifetime risk of attributable cancer (solid organ or leukemia) was estimated at 0.8% for patients exposed to a 100-mSv scan.3,15,32 This risk estimate, as well as most estimates published in the literature, is based on the 1990 results of the Life Span Study cohort of survivors of Hiroshima and Nagasaki.15,33 These were published by the National Academy of Sciences in their Biological Effects of Ionizing Radiation (BEIR) V report.15 Interestingly, 65% of Nagasaki and Hiroshima survivors were exposed to less than 100 mSv.3 The Sunnybrook trauma series suggested an attributable increase of 190 cancer deaths per 100 000 patients exposed to imaging studies after major trauma based on 1990 risk estimates.17
Although many papers quantifying radiation risk continue to refer to the 1990 data, this information has recently been updated. In 2005 and 2006, the risk estimates were increased as a result of further study of the A-bomb survivors in the BEIR VII report.3 Several important conclusions were drawn from this report. The principal finding was that exposure to 100 mSv would result in a solid organ cancer or leukemia developing in 1 person in 100 (0.01/mSv). The BEIR assumes a linear nonthreshold model for risks associated with radiation exposure. The lifetime risk of cancer from all other causes is 42 in 100.3,34,35 For comparison, they stated that lifetime risk of dying from a motor vehicle crash in the United States was 1 in 773 (about 1 in 100 in Canada).36
The BEIR VII risk estimates allow an estimation of relative risk. The relative risk of lifetime cancer after exposure to 100 mSv would be 1.024. The relative risk in the University of Pennsylvania series was 1.025 and that in the Sunnybrook series was 1.005 (1.037 in the high-exposure subgroup). For a single 4.55-mSv CT, the relative risk would be 1.001.
Effects of radiation on children and pregnancy
Radiation exposure in children merits particular attention. The rate of childhood cancer was increased by 40% up to the age of 15 with an increase detected at radiation doses of 10–20 mSv.3,37 Studies have also concluded that there was a linear dose relation between ionizing radiation exposure and the development of radiation-induced cancers.3,16 Importantly, the lifetime risk attributable to a single small dose of radiation at a given age is greater for children.3,15,16
Most centres attempt to minimize exposure to pregnant patients. A recent review by Smits and colleagues38 failed to discover any properly conducted trials confirming adverse outcomes with exposure of the fetus to plain radiography. In utero exposure of the fetus to radiation resulted in excess cancers with exposures of 10 mSv.39 Others have calculated small risks of cancer associated with plain imaging (spine and pelvic radiographs).40,41 Experimental data confirm that mammalian embryos and fetuses are highly radiosensitive, and teratogenesis remains a strong theoretical concern despite no definitive clinical studies.39
DISCUSSION
Trauma teams routinely acquire images as adjuncts to clinical evaluation in the care of trauma patients with multiple injuries. The risk of radiation exposure to both patients and to trauma team members is often overlooked. Our review highlights a need to educate physicians, nurses, therapists and paramedical personnel on these risks.
Application of published clinical decision rules reduces the number of imaging studies. The estimated potential reduction in CT scans for patients with minor head injuries would be 37% with the adoption of the Canadian CT head rule.42 Implementation of the Canadian C-spine rule reduced radiograph ordering rates from 67% to 50% (25% relative reduction).43 The development of similar guidelines for imaging of truncal trauma could potentially reduce imaging. Imaging should be preceded by careful clinical assessment.
Protective strategies such as CT dose optimization for all scanners and maximal use of shielding should be considered. The long-term effects of medical imaging deserve further study. Computed tomography remains the most cost-effective and accurate method to evaluate severe blunt abdominal trauma in hemodynamically normal patients.44 It is an invaluable tool for excluding blunt traumatic aortic injury and occult cervical spine fractures. It is increasingly being used to identify occult vascular injuries. The lifetime risk of cancer is 1 in 100 for a 100-mSv exposure.3 Single and 4-slice whole-body CT images have delivered effective doses of 10 mSv.4 The radiation exposure is reduced with a single 64-slice chest/abdominal CT scan with an exposure of 2 mSv resulting in a potential lifetime risk of cancer of 1 in 15 000. Many severely injured patients reach much higher exposures during the course of their hospital admissions in large part owing to repeat studies.9 Trauma teams should be aware of the radiation dose administered with essential imaging modalities and that radiation dose is a cumulative risk for their patients.
Contributors: Drs. Hui, MacGregor and Kortbeek designed the study. All authors acquired and analyzed the data, wrote and reviewed the article and provided approval for publication.
Competing interests: None declared.
Accepted for publication Sep. 25, 2007
Correspondence to: Dr. J.B. Kortbeek Department of Surgery Calgary Health Region and University of Calgary 1403-29 St. NW, Rm. 1034 Calgary AB T2N 2T9 john.kortbeek@albertahealthservices.ca
References
- 1.Alexander RH, Proctor HJ; American College of Surgeons. Committee on Trauma. Advanced trauma life support course for physicians: ATLS. 5th ed. Chicago (IL): The College; 1993.
- 2.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation NRC. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 1. Washington (DC): National Academies Press; 2005. [PubMed]
- 3.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation NRC. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2. Washington (DC): National Academies Press; 2006. [PubMed]
- 4.Powers J. Assessment of patient doses from CT scanners used by the Calgary Health Region [thesis]. Calgary (AB): University of Calgary; 2006.
- 5.McNitt-Gray MF. AAPM/RSNA physics tutorial for residents: topics in CT. Radiation dose in CT. Radiographics 2002;22:1541-53. [DOI] [PubMed]
- 6.Mayo JR, Aldrich J, Muller NL. Radiation exposure at chest CT: a statement of the Fleischner Society. Radiology 2003;228:15-21. [DOI] [PubMed]
- 7.Frush DP. Review of radiation issues for computed tomography. Semin Ultrasound CT MR 2004;25:17-24. [DOI] [PubMed]
- 8.UNSCEAR 2000. The United Nations Scientific Committee on the Effects of Atomic Radiation. Health Phys 2000;79:314. [PubMed]
- 9.Kim PK, Gracias VH, Maidment AD, et al. Cumulative radiation dose caused by radiologic studies in critically ill trauma patients. J Trauma 2004;57:510-4. [DOI] [PubMed]
- 10.Mettler FA Jr, Wiest PW, Locken JA, et al. CT scanning: patterns of use and dose. J Radiol Prot 2000;20:353-9. [DOI] [PubMed]
- 11.Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology 2004;230:619-28. [DOI] [PubMed]
- 12.Wedegartner U, Lorenzen M, Nagel HD, et al. [Diagnostic imaging in polytrauma: comparison of radiation exposure from whole-body MSCT and conventional radiography with organ-specific CT] [Article in German]. Rofo 2004;176:1039-44. [DOI] [PubMed]
- 13.Ott M, McAlister J, VanderKolk WE, et al. Radiation exposure in trauma patients. J Trauma 2006;61:607-9. [DOI] [PubMed]
- 14.Fenton SJ, Hansen KW, Meyers RL, et al. CT scan and the pediatric trauma patient — Are we overdoing it? J Pediatr Surg 2004;39:1877-81. [DOI] [PubMed]
- 15.Committee on the Biological Effects of Ionizing Radiation (BEIR V) NRC. Health effects of exposure to low levels of ionizing radiation: BEIR V. Washington (DC): National Academies Press; 1990. [PubMed]
- 16.Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176: 289-96. [DOI] [PubMed]
- 17.Tien HC, Tremblay LN, Rizoli SB, et al. Radiation exposure from diagnostic imaging in severely injured trauma patients. J Trauma 2007;62:151-6. [DOI] [PubMed]
- 18.Nickoloff EL, Alderson PO. Radiation exposures to patients from CT: reality, public perception, and policy. AJR Am J Roentgenol 2001;177:285-7. [DOI] [PubMed]
- 19.Grover S, Kumar J, Gupta A, et al. Protection against radiation hazards: regulatory bodies, safety norms, dose limits and protection devices. Indian J Radiol Imaging 2002;12:157-67.
- 20.European Commission. Radiation Protection Report 118. Referral guidelines for imaging. Brussels (Belgium): Directorate-General for the Environment of the European Commission; 2001.
- 21.Tan GA, Van Every B. Staff exposure to ionizing radiation in a major trauma centre. ANZ J Surg 2005;75:136-7. [DOI] [PubMed]
- 22.Van Every B, Petty RJ. Measurements of computed tomography radiation scatter. Australas Phys Eng Sci Med 1992;15:15-24. [PubMed]
- 23.Weiss EL, Singer CM, Benedict SH, et al. Physician exposure to ionizing radiation during trauma resuscitation: a prospective clinical study. Ann Emerg Med 1990;19:134-8. [DOI] [PubMed]
- 24.Ciraulo DL, Marini CP, Lloyd GT, et al. Do surgical residents, emergency medicine physicians, and nurses experience significant radiation exposure during the resuscitation of trauma patients? J Trauma 1994;36:703-5. [DOI] [PubMed]
- 25.Fitzgerald RH, Reines HD, Wise J. Diagnostic radiation exposure in trauma patients. South Med J 1983;76:1511-4. [DOI] [PubMed]
- 26.Braun BJ, Skiendzielewski JJ. Radiation exposure of emergency physicians. Ann Emerg Med 1982;11:535-40. [DOI] [PubMed]
- 27.Grazer RE, Meislin HW, Westerman BR, et al. A nine-year evaluation of emergency department personnel exposure to ionizing radiation. Ann Emerg Med 1987;16:340-2. [DOI] [PubMed]
- 28.Ron E. Ionizing radiation and cancer risk: evidence from epidemiology. Pediatr Radiol 2002;32:232-7. [DOI] [PubMed]
- 29.Boice JD. Cancer following medical irradiation. Cancer 1981; 47(Suppl): 1081-90. [DOI] [PubMed]
- 30.Casarett G, Bair WJ, Meinhold CB. NCRP Report No. 91. Recommendations on limited exposure to ionizing radiation. Bethesda (MD) National Council on Radiation Protection & Measurements; 1980. p. 3-10.
- 31.International Commission on Radiation Protection. Development of the Draft 2005 recommendations of the ICRP: a collection of papers. A report of ICRP supporting guidance 4. Ann ICRP 2004;34 Suppl:1-44, iii-xiii. [DOI] [PubMed]
- 32.Preston DL, Shimizu Y, Pierce DA, et al. Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer disease mortality: 1950-1997. Radiat Res 2003;160:381-407. [DOI] [PubMed]
- 33.1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP 1991;21:1-201. [PubMed]
- 34.Garfinkel L. Probability of developing or dying of cancer. United States, 1991. Stat Bull Metrop Insur Co 1995;76:31-7. [PubMed]
- 35.Slovis TL. CT and computed radiography: the pictures are great, but is the radiation dose greater than required? AJR Am J Roentgenol 2002;179:39-41. [DOI] [PubMed]
- 36.Injury Surveillance Canada. Road Safety in Canada — an overview. Ottawa (ON): Transport Canada.; 2004. Cat. No. H39-4/32-2004E-PDF.
- 37.Cox R, Muirhead CR, Stather JW, et al. Risk of radiation-induced cancer at low doses and low dose rates for radiation protection purposes. Vol 6. Chilton (UK): National Radiological Protection Board [British]; 1995.
- 38.Smits AK, Paladine HL, Judkins DZ, et al. Clinical inquiries. What are the risks to the fetus associated with diagnostic radiation exposure during pregnancy? J Fam Pract 2006;55:441-2, 444. [PubMed]
- 39.Streffer C, Shore R, Konermann G, et al. Biological effects after prenatal irradiation (embryo and fetus). A report of the International Commission on Radiological Protection. Ann ICRP 2003;33:5-206. [PubMed]
- 40.Damilakis J, Perisinakis K, Vrahoriti H, et al. Embryo/fetus radiation dose and risk from dual X-ray absorptiometry examinations. Osteoporos Int 2002;13:716-22. [DOI] [PubMed]
- 41.Lowe SA. Diagnostic radiography in pregnancy: risks and reality. Aust N Z J Obstet Gynaecol 2004;44:191-6. [DOI] [PubMed]
- 42.Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA 2005;294:1519-25. [DOI] [PubMed]
- 43.Kerr D, Bradshaw L, Kelly AM. Implementation of the Canadian C-spine rule reduces cervical spine x-ray rate for alert patients with potential neck injury. J Emerg Med 2005;28:127-31. [DOI] [PubMed]
- 44.Navarrete-Navarro P, Vazquez G, Bosch JM, et al. Computed tomography vs clinical and multidisciplinary procedures for early evaluation of severe abdomen and chest trauma–a cost analysis approach. Intensive Care Med 1996;22:208-12. [DOI] [PubMed]