Abstract
Background
Gastrointestinal (GI) complications following coronary artery bypass grafting (CABG), although infrequent, are associated with significant morbidity and mortality. It has been suggested that systemic inflammatory response plays an important role in these complications. Cardiopulmonary bypass (CPB) is well known to cause increased systemic inflammation, and therefore it has been proposed that performing CABG using an off-pump technique could substantially minimize the risk of GI complications. Prolonged CPB duration has been shown to be an independent predictor of GI complications; however, the effect of avoiding CPB altogether through off-pump procedures has not been thoroughly examined. We sought to compare the incidence of GI complications in patients undergoing on-pump and off-pump CABG.
Methods
We analyzed prospectively entered data on 2451 patients who underwent isolated CABG between January 2000 and October 2004. We compared GI complication rates in 5 predetermined areas (GI bleed, ileus, pancreatitis, ischemic bowel and cholecystitis) among patients who had on-pump CABG with those of patients who had off-pump CABG. We also compared in-hospital mortality due to these complications between the 2 groups.
Results
We compared data for a total of 2010 patients in the on-pump group and 441 in the off-pump group. In the on-pump group, 30 (1.49%) patients experienced GI complications compared with 4 (0.91%) in the off-pump group (p = 0.34). Gastrointestinal bleed was the most common complication in the off-pump group. Eight patients in the on-pump group experienced ischemic bowels compared with no patients in the off-pump group. Six patients (0.3%) in the on-pump group died from GI complications, whereas no patients in the off-pump group died from such complications (p = 0.25).
Conclusion
We found no significant difference in the total number of GI complications between the off-pump and on-pump groups; however, trends could be seen in the types of GI complications that occurred in the 2 groups. Owing to the relatively infrequent occurrence of GI complications, a larger scale study would be beneficial to determine whether the differences observed would be significant.
Abstract
Contexte
Les complications gastro-intestinales (GI) après une chirurgie de pontage coronarien sont rares, mais elles sont associées à une morbidité et une mortalité importantes. Certains ont évoqué le rôle contributif de la réponse inflammatoire systémique dans ce type de complication. On sait en effet que la circulation extracorporelle cause une inflammation systémique, d'où l'hypothèse selon laquelle la réalisation des pontages coronariens au moyen d'une technique ne faisant pas appel à la circulation extracorporelle réduirait substantiellement le risque de complications GI. La durée prolongée des interventions de pontage est un facteur prédicteur indépendant des complications GI. Toutefois, les autres techniques permettant d'éviter complètement la circulation extracorporelle n'ont pas fait l'objet d'études approfondies. Nous avons voulu comparer l'incidence des complications GI chez des patients ayant subi un pontage coronarien selon qu'ils étaient ou non sous circulation extracorporelle.
Méthodes
Après saisie prospective des données de 2451 patients ayant subi un pontage coronarien simple entre janvier 2000 et octobre 2004, nous avons procédé à une analyse. Nous avons comparé les taux de 5 types de complications GI prédéterminées (saignements GI, iléus, pancréatite, ischémie intestinale et cholécystite) chez des patients soumis à un pontage coronarien avec ou sans circulation extracorporelle. Nous avons aussi comparé la mortalité perhospitalière résultant de ces complications entre les 2 groupes.
Résultats
En tout, nous avons comparé les données de 2010 patients du groupe avec circulation extracorporelle et de 441 patients du groupe sans circulation extracorporelle. Dans le groupe avec circulation extracorporelle, 30 patients (1,49 %) ont eu des complications GI, contre 4 (0,91 %) dans le groupe sans circulation extracorporelle (p = 0,34). Les saignements gastro-intestinaux ont été la complication la plus fréquente dans le groupe sans circulation extracorporelle. Dans le groupe avec circulation extracorporelle, 8 patients ont présenté une ischémie intestinale, comparativement à aucun patient dans le groupe sans circulation extracorporelle. Enfin, dans le groupe avec circulation extracorporelle, 6 patients (0,3 %) sont décédés des suites de complications GI, tandis qu'aucun patient du groupe sans circulation extracorporelle n'est décédé de telles complications (p = 0,25).
Conclusion
Nous n'avons observé aucune différence significative quant au nombre total des complications GI entre les groupes avec ou sans circulation extracorporelle. Il a toutefois été possible de dégager certaines tendances relativement au type de complications GI observées dans les 2 groupes. Étant donné la relative rareté des complications GI, une étude à plus grande échelle serait indiquée pour déterminer si les différences observées sont véritablement significatives.
Gastrointestinal complications following coronary artery bypass grafting (CABG), although infrequent, are associated with significant morbidity and mortality. Previous studies have suggested that cardiopulmonary bypass (CPB) could contribute to these complications. Potential pathophysiological mechanisms that have been suggested include splanchnic hypotension and systemic inflammatory response.1–3 Cardiopulmonary bypass is known to cause increased systemic inflammation, and therefore many have suggested that performing CABG off-pump could substantially minimize the risk of gastrointestinal (GI) complications. Studies have investigated whether differences in GI complications exist between patients who underwent on-pump CABG and those who had the procedure off-pump.4–7 These studies have shown mixed results in terms of the difference in total number of GI complications between the 2 groups; however, differences have been shown in the types of GI complications that occurred in the 2 groups.8 We sought to provide further insight into the possible benefits of off-pump versus on-pump CABG.
METHODS
We selected patients who underwent a CABG procedure between Jan. 1, 2000, and Oct. 1, 2004, from the cardiovascular-thoracic (CVT) database at the London Health Sciences Centre university hospital. We excluded patients who had concomitant procedures such as valve repair/replacement or surgical ventricular remodelling. The University of Western Ontario institutional ethics board approved our study protocol.
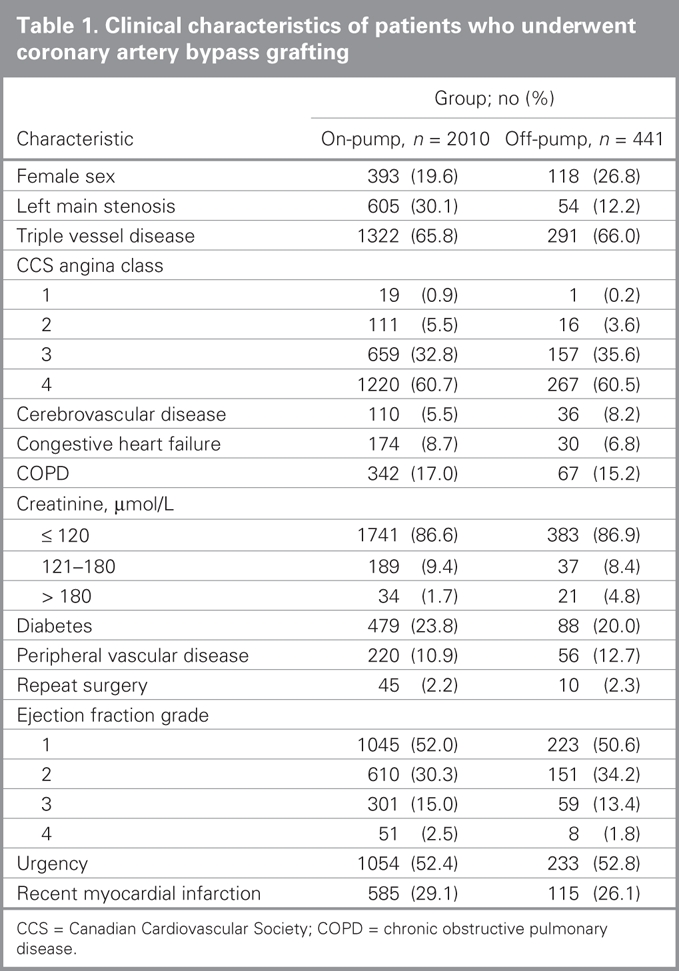
We entered clinical characteristics of all patients into the CVT database at the time of admission. Variables recorded included sex, body mass index, angina class, recent myocardial infarction, diabetes, peripheral vascular disease, cerebrovascular disease, renal dysfunction, chronic obstructive pulmonary disease, ejection fraction grade, left main stenosis, triple vessel disease and repeat surgery.
The main outcome measure was the occurrence of GI complications. We included only patients whose GI complications arose on their initial hospital admissions. We defined GI complications as follows:
Upper GI bleed presenting with melena or hematemesis and drop of Hb2g and requiring endoscopic diagnosis
Paralytic ileus lasting 4 days or more and either requiring nasogastric suction or causing increase in length of stay in hospital
Intestinal ischemia confirmed by laparascopy, endoscopy or autopsy
Acute pancreatitis presenting with abdominal pain and elevated serum amylase levels and positive ultrasound or computed tomography findings
Acute cholecystitis confirmed during surgery or by endoscopic retrograde cholangiopancreatography
We did not include patients with transient ileus, hepatic dysfunction, asymptomatic amylasemia or Clostridium difficile colonization.
We obtained the charts of all patients who experienced any GI complications within 30 days after the CABG procedure. We also reviewed the CVT database, and we reviewed the charts of all patients for whom there was reference to a possible GI problem. We assessed all charts against our previously mentioned criteria for a GI complication.
We compared continuous data using the Student t test. We compared nominal data using χ2 and Fisher exact tests where indicated.
RESULTS
During our study period, 2451 patients met the eligibility criteria. This included 2010 patients in the on-pump group and 441 in the off-pump group. Patient characteristics are summarized in Table 1.
Table 1
In the on-pump group, 30 (1.49%) patients experienced GI complications, compared with 4 (0.91%) in the off-pump group. The between-group difference was not statistically significant (p = 0.34). Six patients (0.3%) in the on-pump group died from GI complications, whereas no patients in the off-pump group died from such complications (p = 0.25). The most common complication in the on-pump group was ileus, whereas the most common complication in the off-pump group was GI bleed. The number of ischemic guts that occurred was 0.4% in the on-pump group compared with 0% in the off-pump group. Eight patients in the on-pump group experienced ischemic bowels, whereas no patients in the off-pump group experienced this complication. Table 2 compares the incidence of GI complications in the 2 groups.
DISCUSSION
Incidence of gastrointestinal complications in the literature ranges from 0.4% to 3.7%, with mortality ranging from 12% to 50%.9,10 The rate of GI complications in our study was 1.3%.
Previous studies have examined in-depth risk factors contributing to GI complications in on-pump cardiac surgery procedures.11 It has been shown that prolonged CPB duration is an independent predictor of GI complications.11 Yet, it remains to be determined whether CPB itself, even without a prolonged duration, increases the incidence of GI complications. With the continued advancements in technology, off-pump beating heart and minimally invasive CABG have continued to gain popularity as favourable alternatives to CPB. Although the literature reports decreased mortality and morbidity in off-pump versus on-pump CABG, only a few studies have compared the incidence of GI complications between these 2 techniques.4–7 Two retrospective studies found no statistical significance in the total number of GI complications between off-pump and on-pump procedures.4,5 A prospective randomized study found that the incidence of CPB, including cardioplegic arrest, was a statistically significant independent predictor of postoperative GI complications in patients undergoing CABG.7
We found no statistically significant difference in the total number of GI complications between the off-pump and on-pump groups. We observed clear trends in the types of GI complications that occurred in the 2 groups. As in the previous studies investigating GI complications,4–7 we found that GI bleed was the most common complication in the off-pump group. We also found that 8 ischemic bowels occurred in the on-pump group compared with 0 in the off-pump group. This finding corresponds with those of previous studies, which all showed that ischemic bowel was more common in the on-pump group.4–7
Although we did not find any significant difference between the on-pump and off-pump CABG groups regarding GI complications, we observed interesting trends in the types of GI complications that occurred in each group. Owing to the relatively infrequent occurrence of GI complications, a larger study with greater statistical power would be beneficial to determine whether the trends observed here are significant.
Contributors: Drs. Croome, Kiaii and Novick designed the study. Dr. Croome and Ms. Fox acquired the data, which Drs. Croome, Kiaii, Quantz, McKenzie and Novick analyzed. Dr. Croome wrote the article. All authors reviewed the article and approved publication.
Competing interests: None declared.
Accepted for publication Nov. 20, 2007
Correspondence to: Dr. K.P. Croome Division of General Surgery 11-457 Platts Lane London ON N6G 3H2 krisbelize@hotmail.com
References
- 1.Gaer JA, Shaw AD, Wild R., et al. Effect of cardiopulmonary bypass on gastrointestinal perfusion and function. Ann Thorac Surg 1994;57:371-5. [DOI] [PubMed]
- 2.Velissaris T, Tang A, Murray M, et al. A prospective randomized study to evaluate splanchnic hypoxia during beating heart and conventional coronary revascularization. Eur J Cardiothorac Surg 2003;23:917-24. [DOI] [PubMed]
- 3.Matata BM, Sosnowski AW, Galinanes M. Off-pump bypass graft operation significantly reduces oxidative stress and inflammation. Ann Thorac Surg 2000;69:785-91. [DOI] [PubMed]
- 4.Musleh GS, Patel NC, Grayson AD, et al. Off-pump coronary artery bypass surgery does not reduce gastrointestinal complications. Eur J Cardiothorac Surg 2003;23:170-4. [DOI] [PubMed]
- 5.Sanisoglu I, Guden M, Bayramoglu Z, et al. Does off-pump CABG reduce gastrointestinal complications? Ann Thorac Surg 2004;77:619-25. [DOI] [PubMed]
- 6.Christenson JT, Schmuziger M, Maurice J, et al. Gastrointestinal complications after coronary artery bypass grafting. J Thorac Cardiovasc Surg 1994;108:899-906. [PubMed]
- 7.Raja SG, Ahmad HM. Predictors of gastrointestinal complications after conventional and beating heart coronary surgery. Surg J R Coll Surg Edinb Irel 2003;1:221-8. [DOI] [PubMed]
- 8.Sanisoglu I, Guden M, Bayramoglu Z, et al. Does off-pump CABG reduce gastrointestinal complications? Ann Thorac Surg 2004;77:619-25. [DOI] [PubMed]
- 9.Ott MJ, Buchman TG, Baumgartner WA. Postoperative abdominal complications in cardiopulmonary bypass patients — a case-controlled study. Ann Thorac Surg 1995;59:1210-3. [DOI] [PubMed]
- 10.Ohri SK, Desai JB, Gaer JA, et al. Intraabdominal complications after cardiopulmonary bypass. Ann Thorac Surg 1991;52:826-31. [DOI] [PubMed]
- 11.Perugini RA, Orr RK, Porter D, et al. Gastrointestinal complications following cardiac surgery: an analysis of 1477 cardiac surgery patients. Arch Surg 1997;132:352-7. [DOI] [PubMed]


