Abstract
Background:
Most patients with ischemic stroke present to the emergency department beyond the approved 3-hour time window for thrombolytic or other revascularization therapies. Clopidogrel and aspirin loading is commonly used to prevent deterioration in other acute vascular occlusive events. This pilot study examined the safety of antiplatelet loading in acute ischemic stroke and transient ischemic attack.
Methods:
Forty patients with stroke or transient ischemic attack symptoms, not eligible for revascularization, received a single dose of 375 mg of clopidogrel and 325 mg of aspirin within 36 hours of stroke onset. All patients were admitted to a comprehensive stroke department and monitored for neurologic deterioration (2-point increase on National Institutes of Health stroke scale [NIHSS] score) and bleeding complications until hospital day 7 or discharge. NIHSS was performed at 24 hours postadmission and on hospital day 7 or discharge, whichever came first.
Results:
A total of 40 patients were loaded with 375 mg of clopidogrel and 325 mg of aspirin (mean 12 hours 32 minutes). Mean admission NIHSS score was 6. There were no cases of systemic hemorrhage or mortality. A single symptomatic intracranial hemorrhage (2.5%) was detected 43 hours posttreatment. When compared with matched control subjects, loaded patients were no more likely to experience hemorrhage and significantly less likely to experience neurologic deterioration (odds ratio 17.2; P < .002).
Conclusions:
Loading with 375 mg of clopidogrel and 325 mg of aspirin appears to be safe when administered up to 36 hours after stroke and transient ischemic attack onset in this pilot study. Neurologic deterioration may be decreased and warrants further study.
Keywords: Acute stroke, antiplatelet, platelet, stroke, transient ischemic attack
At this time, there are no approved urgent therapies for most patients with ischemic stroke who present outside of treatment window for recombinant tissue plasminogen activator or endovascular therapies aimed at achieving revascularization. In addition, those who present with rapidly resolving deficit or low National Institutes of Health stroke scale (NIHSS) score are generally not considered for thrombolytic treatment. No standard treatment is accepted for these patients, although approximately one third of them may be at high risk for neurologic deterioration and recurrent vascular events.1 This pilot study examined the safety of clopidogrel and aspirin loading in patients with acute ischemic stroke (AIS) and transient ischemic attack (TIA) within 36 hours of symptom onset.
Several clinical trials have assessed the safety of acute antiplatelet therapy in ischemic stroke and coronary syndromes.2-6 The Abciximab in AIS (AbESTT) study evaluated the safety of abciximab infusion within 24 hours of symptom onset, and found no symptomatic intracranial hemorrhage (ICH) within 5 days after treatment (asymptomatic hemorrhage rates 7% treated group, 5% placebo group). Although not powered for efficacy, the trial showed a trend toward higher rates of minimal residual deficits among the antiplatelet group. The subsequent AbESTT-II trial was halted as a result of bleeding concerns in the treatment group.2 Mandava et al3 studied the safety of abciximab and heparin infusion for patients within 6 hours of anterior circulation symptoms, and 24 hours of basilar artery thrombosis. Patients were treated with an initial bolus of abciximab followed by a 12-hour infusion and weight-adjusted heparin infusion. One asymptomatic and no symptomatic ICHs were reported.
Administration of high doses of clopidogrel and aspirin can achieve accelerated platelet inhibition in the acute setting.7,8 Loading doses of 300 mg of clopidogrel at least 6 hours before a coronary intervention reduces the risk of recurrent vascular events.5 Nonloading doses of clopidogrel require 3 to 5 days for full inhibition of platelet aggregation, whereas loading doses of 300 mg of clopidogrel show significant inhibition within 6 hours.7
The combination of aspirin and clopidogrel is being assessed in two current stroke prevention studies, although neither aims to determine the effect of antiplatelet loading on acute stroke outcome. The FASTER trial is a randomized, controlled trial comparing clopidogrel plus aspirin with placebo plus aspirin in patients with TIA and minor ischemic stroke within 12 hours of symptom onset. Patients randomized to receive clopidogrel are given 300 mg followed by 75 mg/day for 90 days. The ATARI trial will assign 3000 patients with TIA, within 12 hours of symptoms, to treatment with aspirin and will randomize to clopidogrel or placebo. Patients randomized to receive clopidogrel are given 300 mg followed by 75 mg/day. The primary end point for FASTER is stroke incidence at 90 days whereas ATARI will assess stroke, myocardial infarction, or vascular death at 6 months.9 No study to date has assessed the safety or efficacy of acute clopidogrel plus aspirin loading in acute and transient cerebral ischemia in relation to inpatient neurologic worsening.
Methods
This pilot study was performed at our institution. All patients were admitted to our stroke service and monitored in a comprehensive stroke department. Hospital treatment was the same for loaded versus nonloaded patients.
Patients with acute ischemia, presenting to our emergency department between January and June 2005, were prospectively treated in an open-label, nonrandomized protocol of antiplatelet loading with 375 mg of clopidogrel and 325 mg of aspirin. Protocol inclusion criteria included: (1) age 18 years or older; (2) not eligible for recombinant tissue plasminogen activator or any other acute reperfusion therapy; and (3) clinical symptoms of acute stroke or TIA with onset no more than 36 hours before treatment. The diagnosis of stroke or TIA was based on clinical examination by a stroke specialist. Exclusion criteria were: (1) any history of ICH or systemic hemorrhage; (2) any evidence of hemorrhage on baseline brain imaging; (3) international normalized ratio greater than 1.5; (4) allergy to aspirin or clopidogrel; (5) platelet count less than 100,000/mm3; (6) hematocrit less than 30 mg/dL; and (7) glucose less than 50 mg/dL or greater than 400 mg/dL. The primary safety aim was symptomatic hemorrhage with a secondary end point of neurologic deterioration. The purpose of this pilot study was to establish preliminary safety and feasibility of antiplatelet loading in this population.
Eligible patients received a loading dose of 375 mg of clopidogrel and 325 mg of aspirin orally within 36 hours of stroke symptom onset. Per hospital protocol, patients remained on antiplatelet medication for the duration of hospitalization. Postloading antiplatelet drug and dosing was at the discretion of the admitting practitioner as to only examine the variable of antiplatelet loading and not particular secondary prevention regimens (Fig 1).
Figure 1.
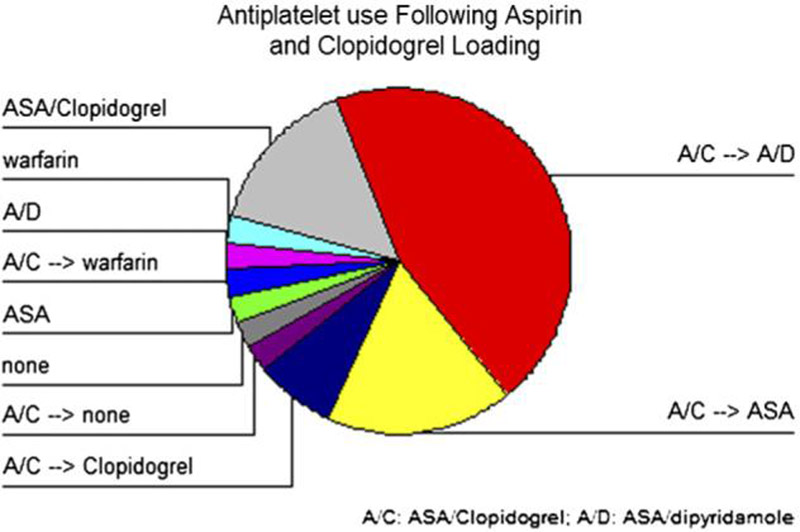
Antiplatelets used after aspirin (ASA) and clopidogrel loading. In-hospital antiplatelet use postloading was at discretion of admitting practitioner. ASA (81 mg) and clopidogrel (75 mg) (A/C) was used during acute stroke admission then patients were transitioned (→) to long-term antiplatelet or anticoagulation therapy at discharge. A/D, Aspirin/dipyridamole ER.
Baseline medical history, clinical examination, NIHSS, electrocardiogram, laboratory tests, brain imaging (computed tomography or magnetic resonance imaging), medication history, and demographic information were assessed. Per stroke service protocol, all patients had follow-up brain imaging within 30 ± 6 hours of loading and for any neurologic deterioration. All computed tomography scans were reviewed by an independent neuroradiologist, blinded to treatment. Dictated reports were reviewed by the researchers and data were obtained on hemorrhage, infarct size, and diffusion-weighted image results in the sample. A complete blood cell count was performed on admission and within 72 hours. ICH grading was based on the European Cooperative Acute Stroke Study hemorrhage scale.10 All patients were monitored for the primary outcome measure until hospital day 7 or discharge. NIHSS was performed at 24 hours postload and day 7 or discharge. A clinically significant neurologic deterioration was defined as a greater than 2-point increase on NIHSS score whereas neurologic improvement was defined as a greater than or equal to 2-point decrease or a score of 0.
This phase of the LOAD study was a retrospective review of an initial exploratory prospective hospital protocol. Subsequent studies to more formally evaluate the safety and efficacy of aspirin and Clopidogrel loading will be registered with a clinical trials database, and approved by our committee for the protection of human subjects. This was an initial exploratory protocol for care and not a clinical trial. Informed consent was not obtained from this initial cohort of patients because the protocol was a preliminary observational study of drugs that were already routinely being used in these patients with stroke, at doses commonly administered for other conditions, and because the data analysis was derived from a retrospective review of our database. The specific aims of the study and variables to examine were determined before data analysis.
Outcomes for treated patients were compared with historical control patients (n = 39) from the stroke service registry, with patients being individually matched for age, sex, time to presentation, and baseline NIHSS score. Nonparametric testing was used for statistical analysis because of the nonnormal distribution of time to presentation. All patients administered loading doses of clopidogrel and aspirin were used for analysis.
This analysis was specifically designed as a pilot study to examine the preliminary safety and feasibility of pursuing a randomized clinical trial properly powered for safety and efficacy. The pilot study sample size was based on the number of consecutive, eligible patients who presented within the review period. The data examined for this study were obtained from our stroke team database, which prospectively captures variables related to demographics, stroke-specific variables, and hospital course on every patient with stroke admitted to our stroke service.
Results
A total of 40 patients (52.5% male) were administered a loading dose of 375 mg of clopidogrel and 325 mg of aspirin at a mean of 12 hours and 32 minutes after symptom onset (range: 1 hour and 49 minutes-36 hours [SEM 1 hour 39 minutes]). The baseline characteristics of the patients are described in Table 1. The mean age of the sample was 64 years (range: 35-87 years) with a mean admission NIHSS score of 6, median 4 (SD 6), and range of 0 to 25.
Table 1.
Baseline patient demographics and characteristics
| Age, y | 64 (mean) | |
| Sex | N (%) | |
| Male | 21 (52.5%) | |
| Female | 19 (47.5%) | |
| Race | N | |
| White | 13 | |
| Black | 16 | |
| Hispanic-white | 11 | |
| Hispanic-nonwhite | 0 | |
| Other | 0 | |
| History of stroke/TIA | N (%) | |
| TIA | 2 | |
| Infarct | 9 | |
| ICH | 0 | |
| NIHSS score (mean) | ||
| Admission | 6 | |
| 24 h | 4 | |
| Discharge/day 7 | 3 | |
| Time to presentation | ||
| Male | 523 min | |
| Female | 586 min | |
| Symptom onset to Rx | ||
| Mean | 12 h 32 min | |
| Median | 8 h 25 min | |
| Admission glucose | 153 (mean) | |
| Length of stay | 4.75 days | |
| Current antithrombotic use | N (%) | |
| Aspirin | 3 (7.5%) | |
| Clopidogrel | 1 (2.5%) | |
| Aggrenox | 2 (5.0%) | |
| Warfarin | 1 (2.5%) | |
| None | 33 (82.5%) | |
| Time to presentation, | N (%) | |
| 0-3 h | 7 (17.5%) | |
| 3 h 1 min-6 h | 11 (27.5%) | |
| 6 h 1 min-12 h | 7 (17.5%) | |
| 12 h 1 min-24 h | 15 (37.5%) | |
| Discharge disposition | N (%) | |
| Home | 26 (65.0%) | |
| Inpatient rehabilitation | 8 (20.0%) | |
| Skilled nursing facility | 2 (5.0%) | |
| Nursing home | 1 (2.5%) | |
| Other | 2 (5.0%) | |
| NIHSS score on presentation | N (%) | |
| 0 | 6 (15%) | |
| 1-5 | 18 (45%) | |
| 6-10 | 9 (22%) | |
| 11-15 | 4 (10%) | |
| 16-20 | 1 (3%) | |
| >20 | 2 (5%) | |
ICH, intracranial hemorrhage; NIHSS, National Institutes of Health stroke scale; Rx, prescription; TIA, transient ischemic attack.
No cases of ICH were detected by scheduled brain imaging. In addition, there were no cases of systemic hemorrhage or mortality in this study. No cases of asymptomatic ICH were detected. A single symptomatic intracranial hemorrhage (2.5%) was detected 43 hours posttreatment. This patient's baseline imaging was notable for a hypodense area greater than one third the middle cerebral artery territory.
No participants experienced neurologic deterioration by 24 hours and 97.5% (n = 39) had no deterioration by discharge or hospital day 7. On the contrary, 37.5% (n = 15) had neurologic improvement by 24 hours and 57.5% (n = 23) by discharge.
Treated patients were compared with matched control subjects obtained from our stroke team patient database. Participants were individually matched on age, sex, race, baseline NIHSS score, and time to presentation. In this pilot study, loaded patients were significantly less likely to experience neurologic deterioration with antiplatelet loading (odds ratio 17.2; P < .002) compared with matched control subjects.
Discussion
Practitioners who treat patients with AIS and TIA who present outside of the time window for revascularization therapies have limited treatment options to offer these patients.
The LOAD study is a retrospective review of a prospective hospital protocol to administer loading doses of aspirin and clopidogrel to patients with ischemic stroke and TIA within 36 hours of stroke symptom onset. This analysis supports the further study of antiplatelet loading in patients ineligible for thrombolytics or endovascular procedures.
Based on our data resulting from this preliminary study, antiplatelet loading with 375 mg of clopidogrel plus 325 mg of aspirin appears safe. This approach appears to be feasible for practitioners and patients, and establishes the usefulness of a future study powered for safety and efficacy. The researchers plan to design a randomized clinical trial powered to confirm the safety and efficacy of antiplatelet loading in AIS and TIA with the current doses followed by dose escalation studies. The evaluation of stroke subtypes and degree of antiplatelet loading benefit may also help in patient selection for loading. The ability of the admitting practitioner to determine postloading antiplatelet use lends to the generalizability of future studies as a more accurate reflection of true clinical practice.
Although these results are encouraging, there are significant limitations to this pilot study. First, the sample was a convenience sample intended to establish the feasibility of a larger scale trial powered for both safety and efficacy. The nature of the sample limits the validity and generalizability of the result. Second, platelet aggregation studies could have significantly added to the causal link between better outcome and antiplatelet loading. Future studies will include measures of platelet aggregation and correlation of degree of platelet inhibition and neurologic outcome. Third, the mean NIHSS score (6) is lower than the mean NIHSS score seen in clinical practice. This may be explained by the enrollment of patients with TIAs (15%) into the study and the increased use of intra-arterial revascularization by our stroke service for patients who may be outside of the approved recombinant tissue plasminogen activator window but may benefit from endovascular therapies. In addition, 3 clinical trials were ongoing at the time of LOAD enrollment that included patients up to 6 hours after symptom onset with higher NIHSS scores. An increased sample size in future studies may provide a more representative sample. The lower mean NIHSS score may also contribute to the lower rate of symptomatic hemorrhage.
Antiplatelet loading may decrease the risk of stroke progression and neurologic deterioration. It is possible that the loading dose in our pilot study produces enough platelet inhibition but less chance of bleeding compared with abciximab, accounting for the favorable trends in our data compared with AbESTT-II trial. Loading of these drugs is a cost-effective means of achieving accelerated platelet inhibition in select patients with AIS and TIA. If proven efficacious, antiplatelet loading would present a treatment option for the thousands of patients with stroke ineligible for revascularization therapies.
References
- 1.Barber PA, Zhang J, Demchuk A, et al. Why are stroke patients excluded from TPA therapy? Neurology. 2001;56:1015. doi: 10.1212/wnl.56.8.1015. [DOI] [PubMed] [Google Scholar]
- 2.Abciximab Emergent Stroke Treatment Trial I. Emergency administration of abciximab for treatment of patients with acute ischemic stroke: Results of a randomized phase 2 trial. Stroke. 2005;36:880–890. doi: 10.1161/01.STR.0000157668.39374.56. [DOI] [PubMed] [Google Scholar]
- 3.Mandava P, Lick SD, Rahman MA, et al. Initial safety experience of abciximab and heparin for acute ischemic stroke. Cerebrovasc Dis. 2005;19:276–278. doi: 10.1159/000084371. [DOI] [PubMed] [Google Scholar]
- 4.CAPRIE Steering Committee A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischemic events (CAPRIE) Lancet. 1996;348:1329. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 5.The Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial I. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 6.Diener H-C, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischemic stroke or transient ischemic attack in high-risk patients (MATCH): Randomized, double-blind, placebo-controlled trial. Lancet. 2004;364:331–337. doi: 10.1016/S0140-6736(04)16721-4. [DOI] [PubMed] [Google Scholar]
- 7.Hochholzer W, Trenk D, Frundi D, et al. Time dependence of platelet inhibition after a 600-mg loading dose of clopidogrel in a large, unselected cohort of candidates for percutaneous coronary intervention. Circulation. 2005;111:2560–2564. doi: 10.1161/01.CIR.0000160869.75810.98. [DOI] [PubMed] [Google Scholar]
- 8.Sabatine MS, Cannon CP, Gibson CM, et al. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med. 2005;352:1179–1189. doi: 10.1056/NEJMoa050522. [DOI] [PubMed] [Google Scholar]
- 9.Hankey GJ. Ongoing and planned trials of antiplatelet therapy in the acute and long-term management of patients with ischemic brain syndromes: Setting a new standard of care. Cerebrovasc Dis. 2004;17:11–16. doi: 10.1159/000075299. [DOI] [PubMed] [Google Scholar]
- 10.Kaste M, Hacke W, Fieschi C, et al. Results of the European cooperative acute stroke study (ECASS) Cerebrovasc Dis. 1995;5:225. [Google Scholar]


