Abstract
Therapy-related myeloid neoplasm is the term recently proposed by the World Health Organization to cover the spectrum of malignant disorders previously described as therapy-related myelodysplastic syndrome or therapy-related acute myeloid leukemia. In this perspective article, Dr. Larson explores the important question of whether the poor prognosis of these conditions reflects t-MN per se or, rather, associated findings such as complex cytogenetics that are also seen, although less frequently, in de novo myeloid neoplasms. See related article on page 542.
Therapy-related myeloid neoplasm (t-MN) is the term recently proposed by the World Health Organization to cover the spectrum of malignant disorders previously described as therapy-related myelodysplastic syndrome (t-MDS) or therapy-related acute myeloid leukemia (t-AML). t-MN is a well recognized clinical syndrome occurring as a late complication following cytotoxic therapy.1–5 The term therapy-related leukemia is descriptive and based on a patient’s history of exposure to cytotoxic agents. Although a causal relationship is implied, the mechanism remains to be proven. These neoplasms are thought to be the direct consequence of mutational events induced by cytotoxic therapy, or via the selection of a myeloid clone with a mutator phenotype that has a markedly elevated risk for mutational events. Several distinct clinical and cytogenetic subtypes of t-MN are recognized and closely associated with the nature of the preceding treatment. The latency between the primary diagnosis and therapy-related disease ranges between a few months to several years, depending in part on the cumulative dose or dose intensity of the preceding cytotoxic therapy, as well as the exposure to specific agents. The majority of patients have clonal chromosome abnormalities in their bone marrow cells at diagnosis. A spectrum of morphological abnormalities is observed.4,5 There is a continuum in the percentage of marrow blasts from t-MDS to overt acute leukemia, and rapid progression from the former to the latter. Thus, it is reasonable to consider this as a single clinical syndrome. The clinical course is typically progressive and relatively resistant to conventional therapies used for leukemias arising de novo.
Alkylating agents are clearly mutagenic and leukemogenic. Topoisomerase-II inhibitors, especially mitoxantrone in studies from Europe and etoposide and doxorubicin in the USA, can induce t-MN, perhaps augmented by granulocyte colony-stimulating factor (G-CSF). The routine addition of G-CSF to cancer therapy has been controversial. It has been suggested that the ability of G-CSF to promote proliferation prior to repair of damaged stem cells, which might otherwise undergo apoptosis, may contribute to leukemogenesis. Although life-saving with regard to severe infections, G-CSF has been associated with a significantly increased cumulative hazard of AML over time in patients with severe congenital neutropenia. More recently, t-MN has been seen in patients, particularly solid organ transplant recipients, following treatment with immunosuppressive therapies not previously thought to cause DNA damage directly. A mechanism for the development of t-MN has been proposed for azathioprine, an immunosuppressant widely used in recipients of organ transplants, through selection of a mutator phenotype to allow the emergence of AML with abnormalities of chromosomes 5 and 7.2
The etiology and specific predisposing features of therapy-related leukemia remain elusive since fortunately only a small fraction of patients exposed to cytotoxic therapy develop the syndrome. It has not yet been possible to determine whether the development of t-MN is a stochastic event, occurring by chance, or whether certain individuals are at higher risk – perhaps due to a DNA-repair deficiency or a heritable predisposition, such as altered drug metabolism. The identification of such an underlying pre-existing condition would help the screening and counseling of patients at the time of treatment for their primary disease.
We have previously reported that the frequency of an inactivating polymorphism in the NQO1 gene (NAD(P)H:quinone oxidoreductase) is increased among individuals with t-MN.6 Both homozygotes as well as heterozygotes, who are at risk of treatment-induced mutation or loss of the remaining wild-type allele in their hematopoietic stem cells, may be particularly vulnerable to leukemogenic changes induced by carcinogens. Other polymorphisms involving detoxifying enzymes have also been reported.7 A large Japanese study of patients with de novo AML and t-AML found that the NQO1 polymorphism was more strongly associated with t-AML than were polymorphisms in GST-M1, GST-T1 and CYP3A4.8
In general, two paths of investigation have been explored. The first involves meticulous clinicopathological and cytogenetic analyses, and more recently molecular analyses, of individual cases as they present with therapy-related leukemia.3,4,9
The second involves large scale epidemiological surveys of patients at risk. There are now many such studies of each type in the literature. After long-term follow-up, hundreds of cases of therapy-related leukemia among cancer survivors have now been reported on and analyzed. Although MDS and AML occasionally occur in cancer survivors treated only with surgery, suggesting a possible predisposition to malignant diseases, the risk of therapy-related leukemia is shared by patients with non-malignant primary disorders if they have received cytotoxic treatment.1,2,4
Classical therapy-related myeloid leukemia
In the classic form of therapy-related leukemia that follows treatment with alkylating agents and/or radiation therapy, the blood and bone marrow findings resemble those seen in primary MDS, although the degree of dysgranulopoiesis and dysmegakaryocytopoiesis is typically greater.
Anemia and thrombocytopenia are extremely common. Leukopenia may also be present. Marked dysplastic changes are observed in all three cell lines. Mild to marked reticulin fibrosis may be present. Auer rods are rarely seen, and myeloperoxidase and non-specific esterase reactivity are often only weakly expressed.
Clonal chromosomal abnormalities, often of a complex nature, are identified in most cases of classical t-MN.1,3–5 Loss of part or all of chromosomes 5 and/or 7 are the characteristic findings, and have been reported in over 90% of cases in some series.4 The karyotypes are often complex. The most common single abnormality is monosomy 7, followed in frequency by deletion of the long arm of chromosome 5 [del(5q)] and by monosomy 5. These same abnormalities are observed in primary MDS and de novo AML, especially in older patients and in those with occupational exposure to potential carcinogens such as benzene.
Therapy-related leukemia following topoisomerase-II inhibitors
The leukemias secondary to agents that target topoisomerase-II typically result in translocations involving the MLL gene on chromosome 11, band q23, and less commonly, the AML1 gene on chromosome 21, band q22.3,4 At first, the association was linked only to the epipodophyllotoxins, etoposide and teniposide. However, subsequent reports have also implicated DNA intercalating agents such as doxorubicin and mitoxantrone. In contrast to classic t-MN, these leukemias have a much shorter latency between initiation of chemotherapy for the primary cancer and the development of leukemia. In addition, a preceding MDS is not common.
Genetic pathways and co-operating mutations in the etiology of therapy-related myeloid neoplasms
Particular mechanisms of DNA damage that lead either to chromosomal deletions or to balanced translocations may underlie the differences in latencies between the two forms of t-MN.1 In the case of chromosomal deletions, one allele of a putative tumor suppressor gene may be inactivated. Before the affected cell would gain a proliferative advantage, however, the second allele might also have to be deleted or mutated. More recent evidence suggests that haploinsufficiency of individual genes, such as EGR1 on chromosome 5q, may allow for malignant transformation.10
However, even loss of both alleles of an individual tumor suppressor may not be sufficient to confer a malignant phenotype. As described in the model of colorectal tumorigenesis, multiple tumor suppressor genes or oncogenes may need to be mutated to ultimately transform a cell. This series of genetic changes may require an extended period of time, thus explaining the long latency of alkylator-induced t-MN. In contrast, balanced chromosome translocations result in the activation of cellular oncogenes in a dominant fashion. These rearrangements, such as those involving the MLL gene at 11q23, may yield a fusion gene that acts as a dominant oncogene. Whereas this fusion gene alone may not be sufficient to fully transform a hematopoietic progenitor cell, relatively fewer genetic events may be required for progression to the leukemic phenotype.
Pedersen-Bjergaard and his colleagues have proposed eight different genetic pathways for the multistep development of t-MN.11 There is growing evidence that mutations in a limited number of molecular pathways may co-operate in the genesis of leukemia. Gilliland and colleagues have described an emerging paradigm in AML, namely, the cooperation between constitutively activated tyrosine kinase molecules, such as FLT3, and transcription factor fusion proteins.12 In this model, the activated tyrosine kinase confers dysregulated proliferative and/or antiapoptotic activity, whereas the fusion protein impairs normal differentiation pathways but has a limited effect on cellular proliferation. Gene expression array experiments with CD34-positive t-AML cells have provided evidence to support this hypothesis.9
Loss of TAL1, GATA1, and EKLF expression has been observed, and these might result in impaired differentiation of hematopoietic cells, whereas overexpression of FLT3, PIK3C2B, and BCL2 result in a proliferative and survival advantage.
Factors that influence outcome in therapy-related myeloid neoplasms
Therapy-related leukemia is generally a fatal disease. The life-threatening complications of this disorder are the result of persistent and profound cytopenias due to the failure of normal hematopoiesis regardless of the fraction of myeloblasts accumulating in the bone marrow or blood. There has been general agreement that patients with t-MN have a shorter survival than patients with de novo AML, and the possible reasons are not hard to enumerate.
A number of potential factors explain the poor outcome of patients with therapy-related leukemia. The persistence of the primary malignant disease, particularly metastatic cancer or lymphoma, causes morbidity and mortality independently of the bone marrow failure caused by the leukemia. Injury to organs and their vascular supply from prior treatment may compromise the ability of these patients to receive intensive remission induction chemotherapy or hematopoietic cell transplantation (HCT). There may be depletion of normal hematopoietic stem cells as a consequence of previous therapy, so that these patients suffer prolonged cytopenias after induction chemotherapy. The bone marrow stroma may have been damaged, especially by therapeutic radiation to fields that include the pelvis or lumbosacral spine, so that it will not support regeneration of normal hematopoiesis. Patients with t-MN are often chronically immunosuppressed from their prior disease or on-going therapy or may have dysfunctional phagocytes, and thus are often colonized with pathogenic or antibiotic-resistant bacteria and fungi. Following prior supportive care, patients may be refractory to additional transfusion support and, therefore, not ideal candidates for intensive myelosuppressive chemotherapy. Finally, the high frequency of unfavorable cytogenetic aberrations arising during or after chemoradiotherapy appears to result in the rapid emergence of chemotherapy resistance in t-MN stem cells.
Treatment of therapy-related myeloid leukemia
The survival of patients with t-MN is often poor despite prompt diagnosis and treatment. There is a paucity of prospective treatment data since these patients are most often excluded from frontline clinical trials. There are no randomized studies comparing standard AML therapy to other forms of treatment. In a nationwide Japanese study of 256 patients with t-MDS (41%) or t-AML (59%), a poor prognosis was associated with abnormalities of chromosome 5, hypoproteinemia, a high level of C-reactive protein, thrombocytopenia, and persistence of the primary malignancy.13 The median age was 61 years. The median survival was only 9.7 months. The majority of the Japanese patients (72%) received antileukemia chemotherapy, either a standard combination using an anthracycline plus cytarabine, or low dose cytarabine, or tretinoin (ATRA) in the case of seven patients with therapy-related acute promyelocytic leukemia (t-APL). A complete remission was seen in 85 patients (46%). The median remission duration was 8.2 months.
Poor hematopoietic reserves make the administration of standard AML therapy difficult. Many patients have poor tolerance for the acute toxicity of treatment. Because t-MN evolves in the milieu of chemotherapy, the malignant cells are relatively drug-resistant. Expression of the multidrug resistance phenotype is common. In a review of 644 t-AML patients treated with a variety of standard AML chemotherapy regimens, only 182 (28%) achieved a complete remission.14 Individual small series report complete remission rates of 40–50%. This is considerably lower than the 65–80% complete remission rate observed in patients with de novo AML. In addition, remissions are often short even when confirmed cytogenetically and consolidated intensively.15
Hematopoietic cell transplantation for therapy-related myeloid neoplasms
The treatment most likely to cure t-MN is allogeneic HCT. Several small case series have described survival rates of about 20–30% for these patients.1,16,17 However, chronic and cumulative toxicities from prior chemoradiotherapy influence the ability to perform HCT and adversely affect survival. Early deaths from regimen-related toxicity are more common after HCT for t-MN than for primary AML.
In this issue of the journal, Kroger and colleagues in the European Group for Blood and Marrow Transplantation (EBMT) group report on the outcomes of 461 patients with t-MN who underwent allogeneic HCT between 1981 and 2006.18 Overall, only about one-third were cured, but these results appear to be improving over time. Multivariable analyses predict a more favorable outcome for younger patients (<40 years), those with normal cytogenetics, and those transplanted in first complete remission. Thus, for patients who have chemotherapy-responsive t-MN, allogeneic HCT can be curative, but it is unfortunately not often successful. Non-myeloablative, reduced intensity allogeneic HCT is under investigation for those who are not eligible for myeloablative HCT.
The EBMT registry has also reported on 65 t-MN patients who underwent autologous HCT.19 The median age of these patients was 39 years (range, 3–69). Estimates of overall and disease-free survival at 3 years were 35% and 32%, respectively. The relapse rate was lower for patients transplanted in first complete remission (48% vs. 89%, p=0.05). Age over 40 years resulted in higher transplant-related mortality (47% vs. 7%, p=0.01).
Cytogenetics affect the outcome of therapy-related myeloid leukemia
The most informative data on the prognostic impact of karyotype on outcome in t-AML were reported by the German AML Cooperative Group (AMLCG).20 This group compared karyotype analysis and survival between 93 patients with t-AML and 1091 with de novo AML; all received intensive treatment. Favorable, intermediate, and unfavorable karyotypes were observed in 26%, 28%, and 46% of t-AML patients, and in 22%, 57%, and 20% of de novo AML patients. Overall, the median survival was 10 months for patients with t-AML compared to 15 months for patients with de novo AML (p=0.0007).
In an updated analysis of the German AMLCG study, the survival of 121 patients with t-AML was compared to that of 1511 patients with de novo AML according to karyotype.21 All received intensive AML therapy. The median survival for the t-AML patients ranged from 27 months for those with a favorable karyotype to 6 months for those with an unfavorable karyotype. Importantly, about half of the patients with t-AML (58/121) had an unfavorable karyotype, whereas only about 20% (302/1511) of the de novo AML patients had an unfavorable karyotype. For those with a favorable karyotype, the median survival had not been reached after 5 years for the 306 de novo AML patients compared to 27 months for the 29 t-AML patients (p=0.02). Within the large intermediate risk cytogenetic group, no significant difference in survival was observed between the t-AML and de novo AML patients. An unfavorable karyotype predicted a very short survival in both groups of AML patients.
Treatment of therapy-related leukemia with balanced chromosomal rearrangements
In marked contrast to the poor outcome overall for t-AML, those patients who develop t-APL with t(15;17) or patients with t(8;21) or inv(16) have treatment outcomes that are similar to those of patients with de novo AML with the same chromosomal rearrangements. However, non-leukemia co-morbidities or persistent primary malignancy may still have an impact on ultimate survival. In a report on 106 cases of t-APL identified between 1982–2001 in France, Spain, and Belgium, the characteristics of the t-APL patients were similar to those of de novo APL patients.22 In addition, more than 80% of those treated with anthracycline-based chemotherapy and/or ATRA achieved a complete remission. Ten of the complete responders relapsed, and seven others died from persistent primary tumor. The actuarial survival was 58% at 8 years, and did not differ between groups of patients analyzed by primary treatment (chemotherapy, radiotherapy, or both) or prior exposure to particular drugs (alklyating agents, topoisomerase-II inhibitors, or both).
Among patients analyzed at the International Workshop in Chicago in 2000, 33 of 39 intensively treated patients (85%) with t-AML and inv(16), and 24 of 35 (69%) with t(15;17) achieved a complete remission.23 Both subgroups were associated with prior exposure to topoisomerase-II inhibitors, but importantly, 21% of the inv(16) patients and 29% of the t(15;17) patients had received only radiotherapy previously. The median overall survival for t-AML patients with either inv(16) or t(15;17) was 29 months after receiving intensive AML therapy.
Only 12 of the 33 inv(16) patients who achieved complete remission relapsed. Five underwent HCT in first complete remission (4 allogeneic; 1 autologous), and all five were alive and leukemia-free at last follow-up. The responding patients were significantly younger than the six who did not achieve complete remission (median, 44 years vs. 62 years, p=0.012). In the inv(16) subgroup, patients less than 55 years of age had improved survival when compared to older patients. The median survival in the group of younger patients (n=26) was longer than 3 years, but was only 12 months for the 13 older patients (p=0.006).
Seventy-two t-AML patients with t(21q22) were also studied at the International Workshop.24 Their median survival was 14 months, and 18% were alive after 5 years. Patients with t(8;21) had a more favorable outcome than those with other 21q22 rearrangements (p=0.014). The median survival times were 17 months for the 11 t-AML patients with only t(8;21) and 31 months for the 33 patients with t(8;21) plus other abnormalities (p=0.6).
Fifty-three patients with t(21q22) received intensive AML therapy; the median survival for the seven who underwent HCT was 31 months compared to 17 months for those who did not. Mutations in cKIT were not studied.
Recommendations for the treatment of therapy-related myeloid neoplasms
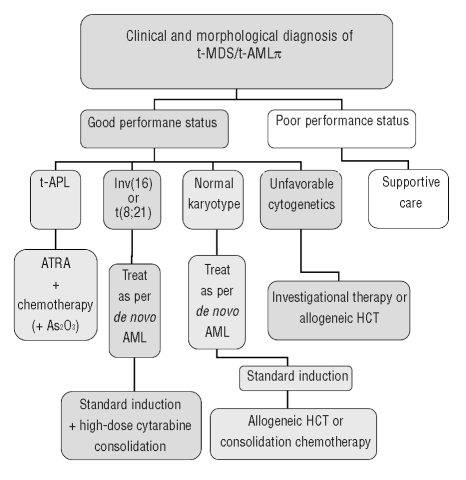
Figure 1 shows a treatment algorithm for the management of patients who develop t-MN. Primary considerations are the patient’s performance status, which likely reflects age, co-morbidities, the status of the primary disease, and the presence of complications from primary therapy, as well as the clonal abnormalities detected in the t-MN cells.
Figure 1.
Decision tree for the management of therapy-related myeloid neoplasms.
In general, these patients should be encouraged to participate in prospective clinical trials that are appropriately designed for other AML patients with similar cytogenetic abnormalities. Patients who have an HLA-matched donor should be considered for allogeneic HCT, although patients with favorable karyotypes may do well with conventional chemotherapy.
References
- 1.Godley LA, Larson RA. The syndrome of therapy-related myelodysplasia and myeloid leukemia. In: Bennett John M., editor. The Myelodysplastic Syndromes Pathobiology and Clinical Management. Marcel Dekker; New York: 2002. pp. 139–76. [Google Scholar]
- 2.Offman J, Opelz G, Doehler B, Cummins D, Halil O, Banner NR, et al. Defective DNA mismatch repair in acute myeloid leukemia/myelodysplastic syndrome after organ transplantation. Blood. 2004;104:822–8. doi: 10.1182/blood-2003-11-3938. [DOI] [PubMed] [Google Scholar]
- 3.Rowley JD, Olney HJ. International workshop on the relationship of prior therapy to balanced chromosome aberrations in therapy-related myelodysplastic syndromes and acute leukemia: overview report. Genes Chromos Cancer. 2002;33:331–45. doi: 10.1002/gcc.10040. [DOI] [PubMed] [Google Scholar]
- 4.Smith SM, Le Beau MM, Huo D, Karrison T, Sobecks RM, Anastasi J, et al. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood. 2003;102:43–52. doi: 10.1182/blood-2002-11-3343. [DOI] [PubMed] [Google Scholar]
- 5.Vardiman JW, Arber DA, Brunning RD, Larson RA, Matutes E, Baumann I, Thiele J. Therapy-related myeloid neoplasms. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Fourth Ed. Lyon, France: IARC Press; 2008. pp. 127–9. [Google Scholar]
- 6.Larson RA, Wang Y, Banerjee M, Wiemels J, Hartford C, Le Beau MM, et al. Prevalence of the inactivating 609C-->T polymorphism in the NAD(P)H:quinone oxidoreductase (NQO1) gene in patients with primary and therapy-related myeloid leukemia. Blood. 1999;94:803–7. [PubMed] [Google Scholar]
- 7.Allan JM, Wild CP, Rollinson S, Willett EV, Moorman AV, Dovey GJ, et al. Polymorphism in glutathione S-transferase P1 is associated with susceptibility to chemotherapy-induced leukemia. Proc Natl Acad Sci USA. 2001;98:11592–7. doi: 10.1073/pnas.191211198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naoe T, Takeyama K, Yokozawa T, Kiyoi H, Seto M, Uike N, et al. Analysis of genetic polymorphism in NQO1, GST-M1, GST-T1, and CYP3A4 in 469 Japanese patients with therapy-related leukemia/ myelodysplastic syndrome and de novo acute myeloid leukemia. Clin Cancer Res. 2000;6:4091–5. [PubMed] [Google Scholar]
- 9.Qian Z, Fernald AA, Godley LA, Larson RA, Le Beau MM. Expression profiling of CD34+ hematopoietic stem/progenitor cells reveals distinct subtypes of therapy-related acute myeloid leukemia. Proc Natl Acad Sci USA. 2002;99:14925–30. doi: 10.1073/pnas.222491799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joslin JM, Fernald AA, Tennant TR, Davis EM, Kogan SC, Anastasi J, et al. Haploinsufficiency of EGR1, a candidate gene in the del(5q), leads to development of myeloid disorders. Blood. 2007;110:719–26. doi: 10.1182/blood-2007-01-068809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pedersen-Bjergaard J, Chistiansen DH, Desta F, Andersen MK. Alternative genetic pathways and cooperating genetic abnormalities in the pathogenesis of therapy-related myelodysplasia and acute myeloid leukemia. Leukemia. 2006;20:1943–9. doi: 10.1038/sj.leu.2404381. [DOI] [PubMed] [Google Scholar]
- 12.Gilliland DG, Jordan CT, Felix CA. The molecular basis of leukemia. Hematology Am Soc Hematology Education Program. 2004:80–97. doi: 10.1182/asheducation-2004.1.80. [DOI] [PubMed] [Google Scholar]
- 13.Takeyama K, Seto M, Uike N, Hamajima N, Ino T, Mikuni C, et al. Therapy-related leukemia and myelodysplastic syndrome: a large-scale Japanese study of clinical and cytogenetic features as well as prognostic factors. Int J Hematol. 2000;71:144–52. [PubMed] [Google Scholar]
- 14.Kantarjian HM, Estey EH, Keating MJ. Treatment of therapy-related leukemia and myelodysplastic syndrome. Hematol Oncol Clin North Am. 1993;7:81–107. [PubMed] [Google Scholar]
- 15.Larson RA, Wernli M, Le Beau MM, Daly KM, Pape LH, Rowley JD, et al. Short remission durations in therapy-related leukemia despite cytogenetic compete responses to high-dose cytarabine. Blood. 1988;72:1333–9. [PubMed] [Google Scholar]
- 16.Anderson JE, Gooley TA, Schoch G, Anasetti C, Bensinger WI, Clift RA, et al. Stem cell transplantation for secondary acute myeloid leukemia: evaluation of transplantation as initial therapy or following induction chemotherapy. Blood. 1997;89:2578–85. [PubMed] [Google Scholar]
- 17.Yakoub-Agha I, de La Salmonière P, Ribaud P, Sutton L, Wattel E, Kuentz M, et al. Allogeneic bone marrow transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia: a long-term study of 70 patients – report of the French Society of Bone Marrow Transplantation. J Clin Oncol. 2000;18:963–71. doi: 10.1200/JCO.2000.18.5.963. [DOI] [PubMed] [Google Scholar]
- 18.Kroger N, Brand R, van Biezen A, Zander A, Dierlamm J, Niederwieser D, et al. Risk factors for therapy-related myelodysplastic syndrome and acute myeloid leukemia treated with allogeneic stem cell transplantation. Haematologica. 2009;94:542–49. doi: 10.3324/haematol.2008.000927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kröger N, Brand R, van Biezen A, Cahn JY, Slavin S, Blaise D, et al. Autologous stem cell transplantation for therapy-related acute myeloid leukemia and myelodysplastic syndrome. Myelodysplastic Syndromes Subcommittee of The Chronic Leukaemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT) Bone Marrow Transplant. 2006;37:183–9. doi: 10.1038/sj.bmt.1705226. [DOI] [PubMed] [Google Scholar]
- 20.Schoch C, Kern W, Schnittger S, Hiddemann W, Haferlach T. Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): an analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia. 2004;18:120–5. doi: 10.1038/sj.leu.2403187. [DOI] [PubMed] [Google Scholar]
- 21.Kern W, Haferlach T, Schnittger S, Hiddemann W, Schoch C. Prognosis in therapy-related acute myeloid leukemia and impact of karyotype. J Clin Oncol. 2004;22:2510–1. doi: 10.1200/JCO.2004.99.301. [DOI] [PubMed] [Google Scholar]
- 22.Beaumont M, Sanz M, Carli PM, Maloisel F, Thomas X, Detourmignies L, et al. Therapy-related acute promyelocytic leukemia. J Clin Oncol. 2003;21:2123–7. doi: 10.1200/JCO.2003.09.072. [DOI] [PubMed] [Google Scholar]
- 23.Andersen MK, Larson RA, Mauritzson N, Schnittger S, Jhanwar SC, Pedersen-Bjergaard J. Balanced chromosome abnormalities inv(16) and t(15;17) in therapy-related myelodysplastic syndromes and acute leukemia: report from an International Workshop. Genes Chromosomes Cancer. 2002;33:395–400. doi: 10.1002/gcc.10043. [DOI] [PubMed] [Google Scholar]
- 24.Slovak ML, Bedell V, Popplewell L, Arber DA, Schoch C, Slater R. 21q22 balanced chromosome aberrations in therapy-related hematological disorders: report from an International Workshop. Genes Chromosomes Cancer. 2002;33:379–94. doi: 10.1002/gcc.10042. [DOI] [PubMed] [Google Scholar]