SYNOPSIS
Objective
Relatively few studies have investigated characteristics associated with multivitamin use in pregnant women in the U.S. We examined multivitamin use among pregnant and nonpregnant women of childbearing age, in relation to socioeconomic factors, demographic data, health behaviors, and health status.
Methods
This investigation used 2004 data from the Behavioral Risk Factor Surveillance System (BRFSS), a cross-sectional study of noninstitutionalized adults aged 18 years or older. Analyses were limited to women 18 to 44 years of age in states and territories where questions about multivitamin use were asked.
Results
Overall, 78% of pregnant women reported multivitamin use, compared with 47% of women who were not pregnant. Using logistic regression, two factors were found to be significantly associated with multivitamin use in pregnant women: income and marital status. Among nonpregnant women, the significant predictors were age, income, physical activity, education level, desire for a child in the near future, race/ethnicity, body mass index, and cigarette smoking status.
Conclusion
We found differences in the reported use of multivitamins between pregnant and nonpregnant women of childbearing age as well as predictors of use.
Adequate vitamin and mineral intake is important for the health of women of childbearing age, both for themselves and their infants. Deficiencies in some vitamins and minerals early in pregnancy can result in permanent damage to the fetus.1 For example, supplements that contain folic acid decrease the risk of some birth defects.2–5
Pregnancy increases the nutritional requirements for some vitamins and minerals, particularly iron. During pregnancy, many women do not get the daily recommended intake of micronutrients through dietary means.6 Several health organizations recommend iron supplementation during pregnancy to help pregnant women meet their iron requirements. The Centers for Disease Control and Prevention recommends routine low-dose iron supplementation for all pregnant women, beginning at the first prenatal visit.7 This recommendation is supported by the Institute of Medicine (IOM) of the National Academy of Sci-ences.8 The U.S. Public Health Service and IOM recommend that all women capable of becoming pregnant consume 400 micrograms of folic acid per day, either as a supplement, from fortified foods, or both.9,10 The American Thyroid Association recommends iodine supplementation for all pregnant and lactating women in the U.S. and Canada.11
The IOM recommends multivitamins that contain iron, zinc, copper, calcium, folic acid, and vitamins D, C, B6, and B12 (note that iodine is not included) for some groups of pregnant women, such as those with iron-deficiency anemia or poor-quality diets, vegetarians, cigarette smokers, and those who consume alcohol.10
The proportion of women 20 to 74 years of age who report taking any dietary supplements has increased from 38% to 57% in the U.S., according to National Health and Nutrition Examination Surveys conducted in the early 1970s to 2000.12 In 2000, the National Health Interview Survey found similar results, with 57% of women reporting using vitamin-mineral supplements within the previous 12 months, and 47% reporting the use of multivitamins.13 In 2001, a survey in 13 states found 56% of men and women reported any vitamin or supplement use, with females reporting higher use than males.14 A report based on the 1988 National Maternal and Infant Health Survey reported that 97% of mothers said they were advised to take multivitamin supplements during pregnancy; 81% of this group reported multivitamin use during pregnancy, while 26% reported multivitamin use before pregnancy.15 In 2000, another survey on multivitamin use in the month before pregnancy found the prevalence (four times per week or more) ranged from 25% to 41% (n=19 states).16
We examined the proportion of pregnant and nonpregnant women who reported use of multivitamins and the characteristics associated with their use in the two groups. Data from the 2004 Behavioral Risk Factor Surveillance System (BRFSS), a state-based telephone survey of adults aged 18 years or older, were used for these analyses. Questions concerning multivitamin use were administered in 14 states and U.S. territories in the 2004 survey.
METHODS
The BRFSS is an ongoing telephone health survey system that annually collects data on health behaviors and health status in the U.S. The design and characteristics of the BRFSS are described elsewhere.17,18 In 2004, a module for vitamin and supplement use was administered to participants aged 18 to 44 years by 14 states and U.S. territories (Arizona, Colorado, Florida, Kentucky, Minnesota, Montana, Nebraska, North Carolina, North Dakota, Texas, Virginia, Wisconsin, Puerto Rico, and the U.S. Virgin Islands). The module asked participants about their current use of vitamin pills or supplements. Those who indicated using vitamins or supplements were asked if any of those taken were a multivitamin. Women were classified as currently taking multivitamins or not currently taking multivitamins. Those classified as not currently taking multivitamins included women reporting supplement use but not multivitamins, as well as women who reported no supplement or vitamin use.
The 2004 BRFSS included questions on perceived general health, self-reported weight and height, physical activity, smoking status, and alcohol consumption. Pregnancy status was assessed, as was overall health condition (self-rated as excellent, very good, good, fair, or poor). Self-reported weight and height were used to calculate body mass index (BMI) in kilograms/meters2 (kg/m2) for nonpregnant women, who were then classified as underweight (BMI<18.5 kg/m2), normal weight (BMI≥18.5 kg/m2 and <25 kg/m2), overweight (BMI≥25 kg/m2 and <30 kg/m2), or obese (BMI≥30 kg/m2).
One question was used to assess leisure-time physical activity: “During the past 30 days, other than your regular job, did you participate in any physical activities or exercise such as running, calisthenics, golf, gardening, or walking?” Respondents were considered physically active if they responded “yes” and physically inactive if they responded “no.” Participants were asked about their health-care coverage, including health insurance, prepaid plans such as health maintenance organizations, or government plans such as Medicare. The annual household income from all sources was categorized into eight levels.
Smoking status was assessed by asking respondents if they had smoked at least 100 cigarettes in their entire life. Those who responded “yes” were also asked if they currently smoked cigarettes every day, some days, or not at all. Respondents were considered current smokers if they reported that they had smoked at least 100 cigarettes in their lifetime and also reported they currently smoke cigarettes.
The following question was used to assess alcohol consumption: “A drink is one beer, one glass of wine, one wine cooler, one cocktail, or one shot of liquor. During the past 30 days, how often have you had at least one drink of any alcoholic beverage?” Women were classified as either having had or not having had alcohol in the previous 30 days.
For nonpregnant women, after a number of screening questions, some women were asked about their desire to have children: “How do you feel about having a child now or sometime in the future?” Women who responded that they wanted to have a child in the future were asked how soon they would want to have a child. These women were classified into four time ranges. For this question, we coded women at three levels: (1) they would like a child less than 12 months from now, (2) they would like a child between 12 months and less than two years from now, and (3) all other women.
We restricted analyses to women of known pregnancy status and multivitamin use. Descriptive statistics with 95% confidence intervals are provided for pregnant and nonpregnant women. We used logistic regression to determine characteristics most strongly related to multivitamin use. We used a full model with all socio-demographic, health behaviors, and health status variables as the starting point, and used a backward-elimination process to determine the most significant predictors of multivitamin use. Analyses were performed separately for pregnant and nonpregnant women. We used the SPSS® Version 1319 module for analyses to account for the complex sample design and survey weighting of the data.
For logistic regression analyses of pregnant women, some variable categories were combined due to small numbers: the older two age groups were combined into one age group (35 to 44 years of age); income categories were collapsed into four levels; for marital status, “previously married” and “never married” were combined; for race/ethnicity, “Hispanic” and “other/not specified” were combined; and for self-reported health, the “good” and “fair/poor” categories were combined.
RESULTS
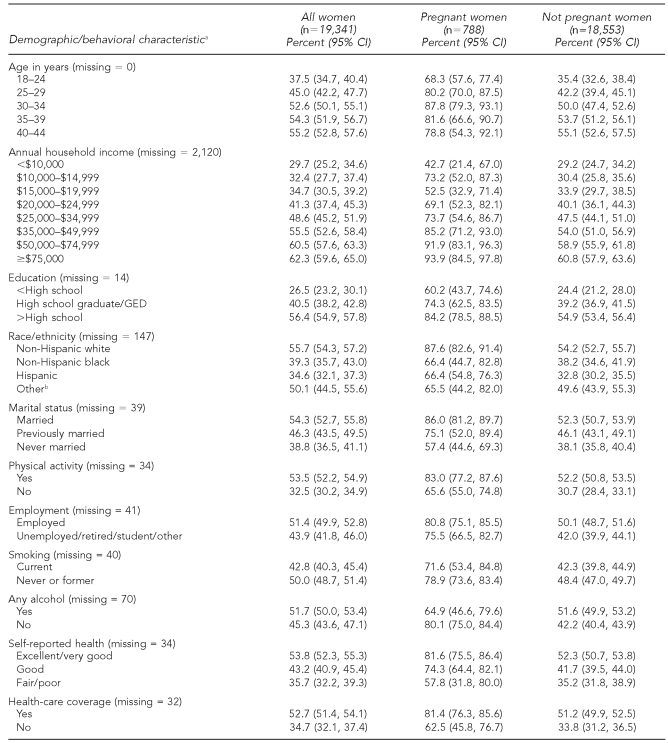
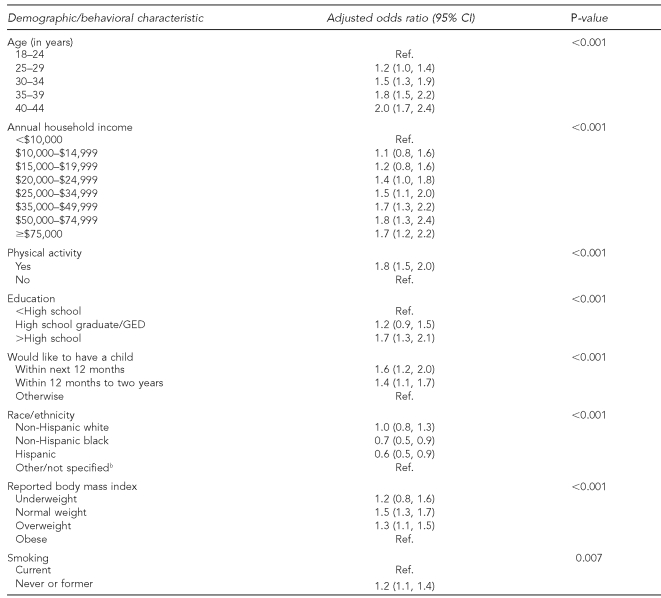
Of 20,263 interviews with women 18 to 44 years of age in the 14 U.S. states and territories, pregnancy status was unknown in 129 (<1%) and multivitamin use was unknown in 840 (4%) of the women. Removing those with unknown pregnancy and/or unknown multivitamin use resulted in 19,341 women, of whom 788 reported they were pregnant. Of the women who reported use of “any vitamin pills or supplements,” 89% reported using multivitamins. Overall, the proportion of pregnant women reporting multivitamin use was 78%, which was significantly higher compared with 47% in nonpregnant women (p<0.001). Among all women (pregnant and nonpregnant), reported multivitamin use was higher in older women, upper-income groups, physically active women, more educated women, non-Hispanic white women, nonsmokers, married women, those self-reporting excellent or very good health, and women with health-care coverage (Table 1).
Table 1.
Multivitamin use in pregnant and nonpregnant women aged 18 to 44 years by various demographic and behavioral characteristics, 14 states and U.S. territories, BRFSS 2004
aMissing represents responses for don't know/not sure, refused, and nonresponse.
bIncludes non-Hispanic/other race/multiracial
BRFSS = Behavioral Risk Factor Surveillance System
CI = confidence interval
GED = general educational development
NA = not applicable
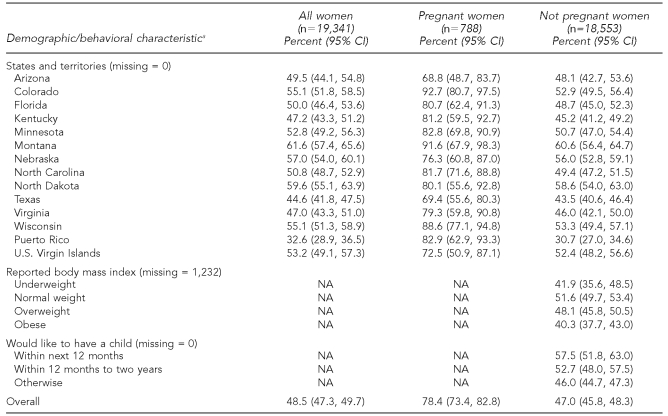
Table 2 presents the final logistic regression model of predictors of multivitamin use for pregnant women with the two significant predictors: annual household income and marital status. Women with higher household incomes were more likely to report multivitamin use (controlling for marital status), and women who were in the combined group of currently or previously married were more likely to report multivitamin use compared with never-married women (controlling for income).
Table 2.
Characteristics associated with multivitamin use in pregnant women aged 18 to 44 years, in 14 states and U.S. territories,a BRFSS 2004
aIncludes Arizona, Colorado, Florida, Kentucky, Minnesota, Montana, Nebraska, North Carolina, North Dakota, Texas, Virginia, Wisconsin, Puerto Rico, and the U.S. Virgin Islands
BRFSS = Behavioral Risk Factor Surveillance System
CI = confidence interval
Ref. = reference group
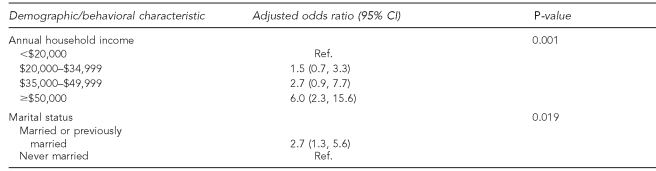
In the logistic regression analyses of nonpregnant women, several variables were significant predictors of multivitamin use: older age, higher household income, physical activity, higher education levels, desire to have a child within two years, non-Hispanic white race/ethnicity, not obese, and a former smoker or someone who never smoked (Table 3).
Table 3.
Characteristics associated with multivitamin use in nonpregnant women aged 18 to 44 years, in 14 states and U.S. territories,a BRFSS 2004
aIncludes Arizona, Colorado, Florida, Kentucky, Minnesota, Montana, Nebraska, North Carolina, North Dakota, Texas, Virginia, Wisconsin, Puerto Rico, and the U.S. Virgin Islands
bIncludes non-Hispanic/other race/multiracial
BRFSS = Behavioral Risk Factor Surveillance System
CI = confidence interval
Ref. = reference group
GED = general educational development
DISCUSSION
The goals of this investigation were to determine the percentage of women of childbearing age who use multivitamins and predictors of multivitamin use. The percentage of women reporting multivitamin use in this study was slightly higher than that reported by some surveys,19 but was consistent with the trend of increase in daily use of multivitamins by U.S. adults.20 The association of daily multivitamin use with being non-Hispanic white, better educated, having a higher income, and being more physically active among nonpregnant women is consistent with other studies.20–22
The results of this investigation found a strong association between pregnancy and use of multivitamins in women of childbearing age from a relatively large dataset (>19,000 women) representative of 14 U.S. states and territories. Adequate vitamin and mineral intake is important for the health of women and their infants, but some pregnant women have insufficient intake of certain vitamins and minerals in their diet.6 The IOM recommends multivitamin supplements for pregnant women with poor-quality diets, but some have suggested recommending that all women of childbearing age use multivitamins.23 Two groups of pregnant women for which multivitamins may be particularly important are those who smoke cigarettes or drink alcohol. Both of these groups were found to be less likely to report multivitamin use, although the differences were not statistically significant.
Limitations
This cross-sectional survey had several limitations. The results were based on 14 U.S. states and territories, where it was decided to ask the vitamin and supplement questions, and therefore cannot be generalized to the entire U.S. population. Information about the duration of multivitamin use, dose, contents, and frequency was not collected. Furthermore, self-reported use of iron-containing multivitamin/mineral supplements among low-income pregnant women has been found to overestimate use.24 The same has been found for self-reported prenatal multivitamin/mineral supplements.25 Therefore, the estimates reported may overestimate true use of multivitamins.
Although household income was found to be an important predictor of multivitamin use, this question had a relatively large percentage of nonresponse and refusals (11%). However, less than a 1% difference in multivitamin use was reported between those who provided an income range compared with those who did not.
Approximately 78% of pregnant women reported using multivitamins, with income and marital status being the two most significant predictors of reported use. Among nonpregnant women who would like to have a child within the next 12 months, only 58% reported multivitamin use.
CONCLUSION
Pregnancy was a significant predictor of multivitamin use among women aged 18 to 44 in our sample, and sociodemographic predictors of use differed by pregnancy status. Data on vitamin and supplement use among women of childbearing age should be presented separately for pregnant and nonpregnant women.
Acknowledgments
The authors thank Lina Balluz, MPH, ScD, Mary Serdula, MD, MPH, and Arshia Sabet-Payman, MD, for their comments.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Picciano MF. Pregnancy and lactation: physiologic adjustments, nutritional requirements and the role of dietary supplements. J Nutr. 2003;133:S1997–2002. doi: 10.1093/jn/133.6.1997S. [DOI] [PubMed] [Google Scholar]
- 2.Botto LD, Mulinare J, Erickson JD. Occurrence of congenital heart defects in relation to maternal multivitamin use. Am J Epidemiol. 2000;151:878–84. doi: 10.1093/oxfordjournals.aje.a010291. [DOI] [PubMed] [Google Scholar]
- 3.Correa A, Botto L, Liu Y, Mulinare J, Erickson JD. Do multivitamin supplements attenuate the risks for diabetes-associated birth defects? Pediatrics. 2003;111(5 Part 2):1146–51. [PubMed] [Google Scholar]
- 4.Goh YI, Bollano E, Einarson TR, Koren G. Prenatal multivitamin supplementation and rates of congenital anomalies: a meta-analysis. J Obstet Gynaecol Can. 2006;28:680–9. doi: 10.1016/S1701-2163(16)32227-7. [DOI] [PubMed] [Google Scholar]
- 5.Shaw GM, Lammer EJ, Wasserman CR, O'Malley CD, Tolarova MM. Risks of orofacial clefts in children born to women using multivitamins containing folic acid periconceptionally. Lancet. 1995;346:393–6. doi: 10.1016/s0140-6736(95)92778-6. [DOI] [PubMed] [Google Scholar]
- 6.Pick ME, Edwards M, Danielle M, Ryan EA. Assessment of diet quality in pregnant women using the healthy eating index. J Am Diet Assoc. 2005;105:240–6. doi: 10.1016/j.jada.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 7.Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep. 1998;47(RR-3):1–29. [PubMed] [Google Scholar]
- 8.Institute of Medicine, Food and Nutrition Board. Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. Washington: National Academies Press; 2001. [PubMed] [Google Scholar]
- 9.Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. MMWR Recomm Rep. 1992;41(RR-14):1. [PubMed] [Google Scholar]
- 10.Institute of Medicine, Subcommittee for a Clinical Applications Guide. Nutrition during pregnancy and lactation: an implementation guide. Washington: National Academy Press; 1992. [Google Scholar]
- 11.Becker DV, Braverman LE, Delange F, Dunn JT, Franklyn JA, Hollowell JG, et al. Iodine supplementation for pregnancy and lactation—United States and Canada: recommendations of the American Thyroid Association. Thyroid. 2006;10:949–51. doi: 10.1089/thy.2006.16.949. [DOI] [PubMed] [Google Scholar]
- 12.Breifel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutri. 2004;24:401–31. doi: 10.1146/annurev.nutr.23.011702.073349. [DOI] [PubMed] [Google Scholar]
- 13.Yu SM, Kogan MD, Huang ZJ. Vitamin-mineral supplement use among U.S. women, 2000. J Am Med Womens Assoc. 2003;58:157–64. [PubMed] [Google Scholar]
- 14.Balluz LS, Okoro CA, Bowman BA, Serdula ML, Mokdad AH. Vitamin or supplement use among adults, Behavioral Risk Factor Surveillance System, 13 states, 2001. Public Health Rep. 2005;120:117–23. doi: 10.1177/003335490512000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu SM, Keppel KG, Singh GK, Kessel W. Preconceptional and prenatal multivitamin-mineral supplement use in the 1988 National Maternal and Infant Health Survey. Am J Public Health. 1996;86:240–2. doi: 10.2105/ajph.86.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams LM, Morrow B, Lansky A, Beck LF, Barfield W, Helms K, et al. Surveillance for selected maternal behaviors and experiences before, during, and after pregnancy: Pregnancy Risk Assessment Monitoring Systems (PRAMS), 2000. MMWR Surveill Summ. 2003;52(11):1–14. [PubMed] [Google Scholar]
- 17.Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment: recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Surveill Summ. 2003;52(9):1–16. [PubMed] [Google Scholar]
- 18.Remington PL, Smith MY, Williamson DF, Anda RF, Gentry EM, Hogelin GC. Design, characteristics, and usefulness of state-based behavioral risk factor surveillance: 1981–87. Public Health Rep. 1988;103:366–75. [PMC free article] [PubMed] [Google Scholar]
- 19.SPSS, Inc. SPSS: Version 13.0. Chicago: SPSS, Inc.; 2004. [Google Scholar]
- 20.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160:339–49. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- 21.Millen AE, Dodd KW, Subar AF. Use of vitamin, mineral, nonvitamin, and nonmineral supplements in the United States: the 1987, 1992, and 2000 National Health Interview Survey results. J Am Diet Assoc. 2004;104:942–50. doi: 10.1016/j.jada.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 22.Balluz LS, Kieszak SM, Philen RM, Mulinare J. Vitamin and mineral supplement use in the United States. Arch Fam Med. 2000;9:258–62. doi: 10.1001/archfami.9.3.258. [DOI] [PubMed] [Google Scholar]
- 23.Keen CL, Zidenberg-Cherr S. Should vitamin-mineral supplements be recommended for all women with childbearing potential? Am J Clin Nutr. 1994;59(2) Suppl:S532–8. doi: 10.1093/ajcn/59.2.532S. [DOI] [PubMed] [Google Scholar]
- 24.Jasti S, Siega-Riz AM, Cogswell ME, Hartzema AG, Bentley ME. Pill count adherence to prenatal multivitamin/mineral supplement use among low-income women. J Nutr. 2005;135:1093–101. doi: 10.1093/jn/135.5.1093. [DOI] [PubMed] [Google Scholar]
- 25.Jasti S, Siega-Riz AM, Cogswell ME, Hartzema AG. Correction for errors in measuring adherence to prenatal/multivitamin/mineral supplement use among low-income women. J Nutr. 2006;136:479–83. doi: 10.1093/jn/136.2.479. [DOI] [PubMed] [Google Scholar]