SYNOPSIS
Objectives
Routine measles-mumps-rubella (MMR) vaccine use has greatly decreased the incidence of mumps in the U.S. However, a resurgence of mumps occurred in 2006. We investigated the large outbreak at a university and assessed risk factors for disease.
Methods
We described the outbreak and conducted a case-control study. We interviewed case students (identified from student health service and health department records) and control students (selected from a randomly ordered administrative list) and assessed their vaccination status. We compared case students with ≥2 MMR doses and control students with ≥2 MMR doses in univariate and multivariate analyses.
Results
The mean age of the 174 case students was 20.9 years; 65% were women. Ninety-seven case students and 147 control students were enrolled in the study. Two-dose MMR coverage was 99% among case and control students with complete records. Only 33% of case students reported exposure to someone with mumps. Case students were more likely than control students to be aged 18 to 19 years (vs. aged 22 years, adjusted odds ratio [AOR] = 5.55; 95% confidence interval [CI] 2.09, 14.74), to report exposure to mumps (AOR=2.31, 95% CI 1.13, 4.73), and to have worked/volunteered on campus (AOR=2.91, 95% CI 1.33, 6.33). Also, women in dormitories had increased odds of mumps compared with men in dormitories.
Conclusion
High two-dose MMR coverage was not sufficient to prevent the outbreak. Further study is needed to better understand the effects of dormitory residency and gender on mumps transmission. Clinicians should be vigilant for mumps in young adults presenting with parotitis regardless of immunization history.
Mumps is a vaccine-preventable disease characterized by acute parotitis. In 1977, the Advisory Committee on Immunization Practices (ACIP) recommended one dose of mumps vaccine for all children.1,2 In 1989, ACIP recommended that two doses of measles vaccine, preferably given as measles-mumps-rubella (MMR) vaccine, be administered to all school-aged children and people entering college to improve measles control.3 Routine use of MMR greatly decreased the number of reported mumps cases in the U.S. to a low of 231 cases in 2003—a 99% decrease from the 185,691 cases reported in 1968.3,4
In 2006, the U.S. experienced a mumps resurgence that primarily affected Midwestern states.5–7 In March 2006, the Lawrence-Douglas County Health Department (LHD) in Kansas was notified of a cluster of mumps cases among students at the state's largest university. The county had last experienced a mumps outbreak 18 years earlier.8 During that 1988–1989 outbreak, which occurred before implementation of the two-dose MMR policy, 10- to 14-year-olds had the highest incidence of mumps, and most cases occurred in three junior high schools with high one-dose MMR coverage. During the 2006 outbreak, the university estimated high two-dose MMR coverage among its nearly 25,000 students. It had initiated a two-dose MMR policy for matriculation in 1993, in part because measles cases had occurred among its students in the early 1990s. The Kansas Department of Health and Environment (KDHE) and the Centers for Disease Control and Prevention (CDC) initiated an investigation at the university to describe the 2006 mumps outbreak and identify risk factors for developing mumps.
METHODS
Outbreak description
In Kansas, health-care practitioners, laboratories, and hospitals are required to report mumps cases to the local health department or KDHE. We used databases from KDHE, LHD, and the university's student health service (SHS) to identify students reported with suspected mumps. For outbreak description, mumps was defined in three ways: (1) illness in a student attending the university who reported acute onset of parotitis, (2) a male student who reported orchitis, or (3) a symptomatic student in whom either mumps virus was isolated by culture or mumps viral RNA was detected by polymerase chain reaction (PCR) from a clinical specimen. The onset of symptoms had to be from February 1 to May 8, 2006. We attempted to review medical records of all reported cases. We excluded from analyses students whose medical records described a likely non-mumps etiology for their illnesses.
Case-control study to assess risk factors for mumps
Cases and controls.
To identify possible risk factors for developing mumps, we conducted a case-control study among undergraduate students. We attempted to interview all students included in the outbreak description. A case student was defined as an undergraduate who (1) reported to investigators parotid gland swelling for at least two days (i.e., the student was asked, “Did you have swelling of the parotid glands, the glands near your ears and cheeks?”) or (2) reported testicular pain or swelling, or (3) a symptomatic student in whom mumps virus was detected by culture or PCR. The onset of symptoms had to be from February 1 to May 8, 2006.
We desired a similar number of interviewed control and case students (about 125 each). Estimating a response rate of 25% to 33%, we selected 450 potentially eligible control students from a randomly ordered list of undergraduates enrolled in spring 2006. Six were subsequently excluded because they attended a satellite campus, resulting in 444 potentially eligible control students. A control student was defined as an undergraduate who did not have symptoms suggestive of mumps from January 1 to May 8, 2006.
Data collection.
We administered a questionnaire to case students by telephone or in person. Case students were questioned about their course of illness, medical care, vaccination status, residence type, mumps exposure, and work and travel history. We interviewed potential control students by telephone. They were screened for symptoms suggestive of mumps, and we terminated interviews with students who might have had mumps in 2006. The remainder of the questions were similar to those asked of case students. We conducted all interviews from May 8 to June 14, 2006.
We determined each student's mumps vaccination status by reviewing hard-copy immunization records required for admission to the university and immunization documents in SHS medical records. If these records were incomplete, we reviewed data in the SHS electronic immunization database, attempted to contact the student for the immunization record, or located information for their physician so that the record could be obtained.
Statistical analysis.
We compared case students with ≥2 MMR doses and control students with ≥2 MMR doses in univariate analyses by Chi-square tests, and determined odds ratios (ORs) with 95% confidence intervals (CIs). Factors significantly associated with disease by univariate analysis (p<0.05) were considered in multivariate logistic regression modeling. To identify independent risk factors for mumps, we used a backward selection procedure to eliminate nonsignificant variables until all remaining variables were significant at p<0.05. We assessed for interaction between variables.
RESULTS
Outbreak description
Cases.
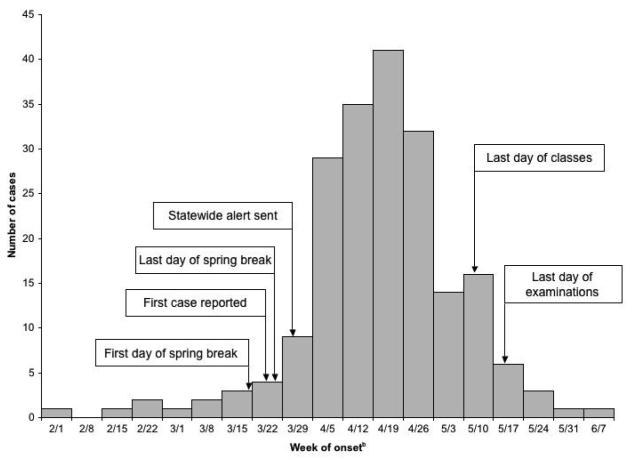
A total of 174 mumps cases among university students were reported to KDHE (Figure) with illness onset from February 1 to May 8, 2006; 164 cases occurred among undergraduate students (0.9% of 19,155 students) and 10 cases occurred among graduate students (0.2% of 5,899 students). The mean age was 20.9 years (range: 18.6 to 33.5). Women accounted for 113 of the case students (65%), and 137 case students (77%) were white. At least 167 case students (96%) had ≥2 MMR doses; five students with incomplete/missing records were counted as not having two doses. Two case students with complete records each had one MMR.
Figure.
Epidemic curve of the mumps outbreak at a Kansas university, February 1 to June 13, 2006a
aThis date is one incubation period (25 days) after the last day of final examinations.
bThis date is the first day of the one-week period represented by the column.
The first case identified at the university was reported to KDHE on March 24, 2006, and a cluster of three cases was reported on March 27. On March 30, KDHE sent a statewide alert about the outbreak to physicians and public health practitioners. Prior to the alert, seven students with parotitis had sought medical care and had not been reported to KDHE as suspected mumps cases; these were identified retrospectively. A total of 12 case students had received medical care before the cluster report; the first had symptom onset eight weeks earlier, on February 2, 2006. Eleven of the 12 early case students were treated with antibiotics at their first medical visit and two were additionally prescribed dexamethasone. The two earliest case students were not able to identify a source for their illness; during part of their likely exposure period, one had traveled outside Kansas to a non-outbreak state, and one had traveled to Mexico.
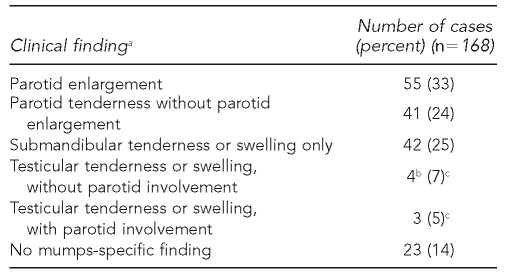
Medical records were reviewed for 168 case students (97%). Parotid enlargement was documented in 55 case students (33%) (Table 1). Testicular tenderness or swelling was the only mumps-associated finding in four cases (7% of men). No case student was diagnosed with meningitis, although one underwent computed tomography of the head to evaluate a worsening headache. No case student was hospitalized.
Table 1.
Clinical features among students with mumps: main clinical finding described in medical record
aFor women, or men without testicular involvement, the following hierarchy was used for classification: parotid enlargement >parotid tenderness >submandibular tenderness or swelling >no mumps-specific finding.
bTwo case students also had submandibular tenderness or swelling.
cPercent of 61 cases among men
Forty case students who met the study case definition or had mumps-specific findings described in the medical record were dormitory residents: 35 women and five men. The university had eight dormitories, each with a population of 267 to 906 students. Only one dormitory reported no cases. The overall mumps incidence among the 2,151 women in dormitories was 1.6% (range: 0% to 3.1% at individual dormitories; mean: 1.5%), and among the 1,575 men, the incidence was 0.3% (range: 0% to 1.1% at individual dormitories; mean: 0.2%).
The KDHE laboratory tested buccal swabs from 17 students, and mumps virus was isolated from three of them (18%). At outside laboratories, mumps virus was isolated from two additional students and mumps RNA was detected by PCR in eight others.
Control measures.
In its March 30, 2006, alert, KDHE recommended students with mumps be isolated for nine days after symptom onset. On April 7, KDHE changed the recommendation to four days because the infectious period of mumps was considered to be up to four days after onset of active disease.9 The isolation recommendation was changed back to nine days on April 25, after definitive guidelines from CDC were published10 and to comply with Kansas regulations.
SHS alerted students and employees about the outbreak using posters and e-mails, and the university newspaper published outbreak updates. People with mumps symptoms were advised to seek medical care. SHS also reviewed its electronic immunization database and sent letters to students who did not have documentation of two MMR doses, offering free vaccination.
Case-control study
Enrollment.
Of the 164 cases reported among undergraduates, 126 (77%) were successfully interviewed and 97 (77%) met the study case definition. Interviewed case students were similar to all eligible cases in characteristics available: proportion that was aged 18 to 19 years, female, or dormitory residents (data not shown). One case had been selected as a potential control and was excluded from the control group. Of the 443 potential control students, 147 (33%) were successfully interviewed. Interviewed control students were similar to the group of potentially eligible control students in characteristics available: proportion that was aged 18 to 19 years, female, or full-time students (data not shown).
MMR coverage.
A complete mumps immunization record was obtained for 99% (96/97) of case students and 97% (141/145) of control students (excluding one control student born before 19572 and one with prior mumps disease). Ninety-nine percent (95/96) of case students and 99% (140/141) of control students with complete records had received ≥2 MMR doses before the outbreak.
Mumps in enrolled cases.
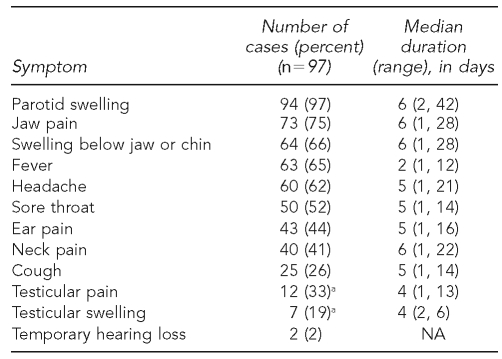
Among the 77 (79%) students who had fully recovered by the time of interview and who provided information on illness duration, the median duration of illness was eight days (range: 2 to 63 days). Parotid gland swelling, the main criterion in the case definition, was reported by 97% of case students (Table 2). Testicular pain was reported by 33% of men and testicular swelling by 19%.
Table 2.
Symptoms reported by interviewed students with mumps
aPercent of 37 cases among men
NA = not available
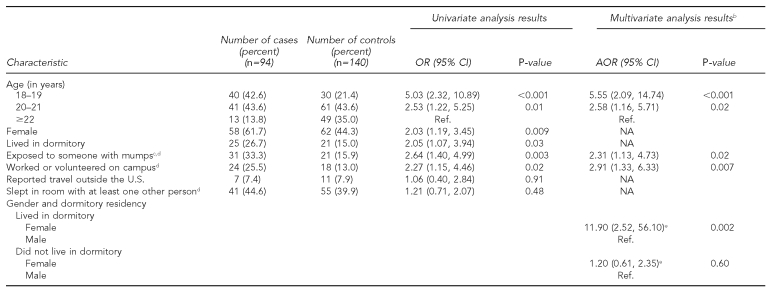
Risk factors for mumps.
By univariate analyses, case students were more likely than control students to be women and aged <22 years; they were also more likely to have reported exposure to someone with mumps, to have lived in a dormitory, and to have worked or volunteered on campus (Table 3). Factors not associated with case status included race/ethnicity, full-time student status, sleeping in a room with at least one or two other people, sharing a bathroom with at least one other person, usually dining on campus, belonging to a fraternity or sorority, traveling outside the U.S., and traveling to another state with a known mumps outbreak.
Table 3.
Univariate and multivariate analysis of risk factors for mumps disease among undergraduate students with ≥2 MMR dosesa
aAmong the 97 case students, 95 had complete immunization records (91 had two MMRs, three had three MMRs, one had one MMR), and two had incomplete or missing records. The three case students that did not have a record of ≥2 MMRs were excluded from analysis. Among the 147 control students, 141 had complete immunization records (136 had two MMRs, four had three MMRs, one had no MMR), one was considered immune because of prior history of mumps disease, one was born before 1957 and considered immune from natural exposure, and four had incomplete or missing records. The seven control students that did not have a record of ≥2 MMRs or who were considered immune from previous exposure were excluded from analysis.
bFinal model (case students: n=93; control students: n=130) included age, gender, dormitory residency, exposure to person with mumps, and working or volunteering on campus.
cExposure to mumps was assessed by the question, “During the month before your illness [for case students] or during the time period March 1, 2006, through May 6, 2006 [for control students], were you in close contact (meaning within 3 feet for several hours) with someone who was ill with mumps?”
dResults are missing for some people.
eMales in dormitory vs. males not in dormitory: AOR=0.21 (95% CI 0.05, 0.92; p=0.04); females in dormitory vs. females not in dormitory: AOR=2.06 (95% CI 0.70, 6.08; p=0.19); females in dormitory vs. males not in dormitory: AOR=2.47 (95% CI 0.85, 7.19; p=0.10)
MMR = measles-mumps-rubella vaccine
OR = odds ratio
CI = confidence interval
AOR = adjusted odds ratio
Ref. = reference group
NA = not applicable
By multivariate analysis, case students were more likely than control students to be aged <22 years (adjusted odds ratio [AOR] for age 18 to 19 years vs. age ≥22 years = 5.55, 95% CI 2.09, 14.74), to have reported exposure to someone with mumps (AOR=2.31, 95% CI 1.13, 4.73), and to have worked or volunteered on campus (AOR=2.91, 95% CI 1.33, 6.33) (Table 3). The effect of dormitory residency on mumps risk was modified by gender; women in dormitories had increased odds of mumps compared with men in dormitories, but among people living elsewhere, women did not have significantly increased odds of mumps compared with men.
DISCUSSION
This large mumps outbreak was unexpected at a campus with high two-dose MMR coverage among its students. The overall reported clinical mumps attack rate among the nearly 19,000 undergraduate students was 0.9% through May 8, 2006. In five reported college outbreaks (student populations ranging from 1,500 to 9,000 students) that occurred in 1986–1987, before the two-dose MMR recommendation was made, attack rates ranged from 0.4% to 2.7%, with a mean attack rate of 1.6%.11 While differences in attack rates can be expected because of differences in students' mumps vaccination coverage and immunity from childhood exposure to wild-type virus, other factors might also influence this estimate (e.g., whether mumps exposure was indeed widespread, the timing of the outbreak relative to the academic year, case definition, and case ascertainment).
Before notification of this outbreak, most physicians who evaluated the Kansas university students with parotitis did not suspect mumps as the etiology. After many years of high vaccine coverage among children and adolescents, mumps had become an illness rarely reported (and likely rarely seen) by clinicians in the U.S. Even after the outbreak was identified, diagnosing mumps was not always straightforward. Many students sought initial care early in their illness, presenting with rather nonspecific signs and symptoms. Furthermore, from clinical descriptions during the pre-vaccine era, the submandibular gland may be the only gland involved in 10% to 15% of patients12 and submandibular gland swelling can be virtually indistinguishable from anterior cervical lymphadenopathy.13 This can lead to over- or underdiagnosis of mumps. In the pre-vaccine era, epididymo-orchitis occurred in 20% to 38% of postpubertal males.14,15 In our investigation, testicular involvement was described in the medical records of 11% of men, but 33% of men reported testicular pain or swelling during our interview. The lower proportion of cases with orchitis by medical record review might be because medical care was sought before orchitis had developed, while interviews were usually conducted after recovery and assessed the full course of mumps.
Several risk factors were found to be associated with mumps in the case-control study; some of these factors were also identified in the case-cohort study performed during the outbreak.16 In our study, younger students had increased odds of developing mumps, and students aged 18 to 19 years had the highest odds. At large universities such as this one, first- and second-year students are often in classes with larger numbers of students than those who are in their third and fourth years, potentially increasing exposure to infectious people during outbreaks. Although details of social interactions were not assessed in our investigation, differences in behavior may have increased mumps exposure for younger students. During a mumps outbreak among young adults in Canada, attendance at a specific type of party (rave) was a risk factor for mumps, while attending bars, clubs, concerts, or other social events was not.17 At three Illinois universities with mumps outbreaks in 1986–1987, students in lower classes had an increased risk of mumps compared with students in upper classes by univariate analyses, and this held true for dormitory residents at the one university in which stratification of data was possible.18
At the Illinois universities, the difference in risk was believed to be caused by underimmunization (with one MMR) of younger students who did not have previous exposure to wild-type virus. Although underimmunization was not a factor in our outbreak, it is possible that older students at our university were better protected because of prematriculation exposure to wild-type virus, while younger students were less well protected in 2006 because they had no prior exposure to wild-type virus and were protected only by vaccine. Given the low reported incidence of mumps in the U.S. when the Kansas university students were children, however, a substantial difference in exposure between birth cohorts separated by only a few years is not very likely.
Other factors, such as working or volunteering on campus, may have increased disease odds by allowing exposure to a greater number of students. While dormitory residents may also be expected to have increased odds of disease because of possible increased exposure, this was not a consistent finding in our analysis. In our study, women in dormitories were at increased odds of developing mumps compared with men in dormitories. Only five mumps cases occurred among men in dormitories; why this number is so low is not clear. Women in dormitories may have been more likely than men to associate in groups with close physical contact, facilitating transmission. One could also postulate that men were less likely to seek medical care for an illness that has no specific treatment. This assessment, however, is not supported by the finding that among non-dormitory residents, there was no difference in disease odds between men and women. In the Illinois college outbreaks, only results of univariate analyses were available; dormitory residents had an increased risk of mumps and there was no significant difference in mumps risk by gender among all students.18
Close, prolonged exposure to someone with mumps was also associated with developing disease in our study, but only 33% of cases reported such exposure. In the remaining majority of cases, transmission may have occurred from an infectious person who never developed classic mumps, or from an infectious person before developing classic mumps (and the exposed student was never aware of the index case's illness). Only 38% of case subjects in the Illinois college outbreaks18 and 48% in a Tennessee high school outbreak (with high one-dose coverage)19 reported prior contact with someone who had mumps. Despite differences in vaccination status among these outbreak populations, the similarly low proportion of case students who reported exposure suggests a universal explanation, and transmission from minimally symptomatic people seems most likely. Viral shedding from unvaccinated, minimally symptomatic people has been documented;20,21 however, the frequency of such infections among people with two MMR doses is not known.
If transmission from minimally symptomatic people played an important role in this outbreak, one may question whether isolation of clinical cases was a valuable control measure. The effectiveness of isolating mumps cases had previously been questioned in unvaccinated children because of transmission from cases before the onset of parotitis and from minimally symptomatic people.21 Implementing isolation recommendations required substantial effort among SHS, university housing, and LHD staff.22 The change in the recommended number of isolation days created confusion among clinicians, public health practitioners, and students. Increasing the recommended days of isolation near the end of the semester might have exaggerated the decrease in reported cases; some physicians reported this change led them to be more stringent in diagnosing mumps because of the perceived educational and social impact the longer isolation period had on students. Additionally, anecdotal reports indicated that some students with mumps did not seek medical care at the end of the semester, fearing isolation orders would prevent them from completing final examinations. Ideally, studies would be performed to assess the overall benefits and risks of isolation measures for mumps among highly vaccinated university populations; in practice, such studies are exceedingly difficult to perform.
Limitations
This investigation had several limitations. First, the enrollment rate was low among potential control students, raising the concern that enrolled control students may not have been highly representative of all students without mumps. The enrolled control students, however, were similar to all potential control students in factors available for comparison. Second, we investigated case students who sought medical care; how many cases, if any, did not seek medical care and how these differed from cases that did is not known. Third, our case definition relied largely on clinical criteria; however, our definition was similar to the CDC/Council of State and Territorial Epidemiologists definition, and by reviewing medical records we were able to document mumps-specific features for most cases.
CONCLUSION
As in most of the U.S., mumps in Kansas had required little attention in the recent past, until 2006. This outbreak demonstrates that high two-dose MMR coverage is not sufficient to prevent all mumps outbreaks. Although our study was not designed to assess possible waning vaccine-induced immunity, this clearly is an important question to be answered.7,16,23 In future outbreaks, we also suggest the effect of dormitory residency and gender on mumps transmission be further investigated and recommend that students in dormitories be systematically queried for mumps so that possible undiagnosed cases can be included in analyses. Clinicians should also be vigilant for mumps in young adults presenting with parotitis regardless of immunization history.
Acknowledgments
The authors thank the following people for their contributions: Jennifer Hill, Daniel Neises, Martha Siemsen, Trudy Shane, Amanda Huston, Cheryl Banez Ocfemia, and D. Charles Hunt of the Kansas Department of Health and Environment; Patty Quinlan, Sherry Rhine, Diane Hendy, and Joe Gillespie of the Watkins Memorial Health Center, University of Kansas; Barbara Schnitker, DeeAnne Schoefeld, Linda Cowles, and Kathy Colson of the Lawrence-Douglas County Health Department; and John Aldahondo, Angela Calugar, Lumbe Davis, Edith Gary, Holly Groom, Penina Haber, Janine Hines, Elaine R. Miller, Mary A. Mulholland, Umesh Parashar, Cassandra A. Rolle, Richard A. Schieber, Peter Starling, Min Tao, Reina M. Turcios-Ruiz, Marleen van Gelder, Tureka L. Watson, Bayo C. Willis, and Katherine Wytovich of the Mumps Response Team at the Centers for Disease Control and Prevention (CDC).
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC.
REFERENCES
- 1.Recommendation of the Immunization Practices Advisory Committee (ACIP): mumps vaccine. MMWR Morb Mortal Wkly Rep. 1982;31(46):617–20. 625. [PubMed] [Google Scholar]
- 2.Watson JC, Hadler SC, Dykewicz CA, Reef S, Phillips L. Measles, mumps, and rubella—vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1998;47(RR-8):1–57. [PubMed] [Google Scholar]
- 3.Mumps prevention. MMWR Morb Mortal Wkly Rep. 1989;38(22):388–92. 397–400. [PubMed] [Google Scholar]
- 4.McNabb SJ, Jajosky RA, Hall-Baker PA, Adams DA, Sharp P, Anderson WJ, et al. Summary of notifiable diseases—United States, 2005. MMWR Morb Mortal Wkly Rep. 2007;54(53):1–92. [PubMed] [Google Scholar]
- 5.Brief report: update: mumps activity—United States, January 1–October 7, 2006. MMWR Morb Mortal Wkly Rep. 2006;55(42):1152–3. [PubMed] [Google Scholar]
- 6.Mumps epidemic—Iowa, 2006. MMWR Morb Mortal Wkly Rep. 2006;55(13):366–8. [PubMed] [Google Scholar]
- 7.Dayan GH, Quinlisk MP, Parker AA, Barskey AE, Harris ML, Schwartz JM, et al. Recent resurgence of mumps in the United States. N Engl J Med. 2008;538:1580–9. doi: 10.1056/NEJMoa0706589. [DOI] [PubMed] [Google Scholar]
- 8.Hersh BS, Fine PE, Kent WK, Cochi SL, Kahn LH, Zell ER, et al. Mumps outbreak in a highly vaccinated population. J Pediatr. 1991;119:187–93. doi: 10.1016/s0022-3476(05)80726-7. [DOI] [PubMed] [Google Scholar]
- 9.Mumps. In: Atkinson W, Hamborsky J, McIntyre L, Wolfe S, editors; Atkinson W, Hamborsky J, McIntyre L, Wolfe S, editors. Epidemiology and prevention of vaccine-preventable diseases. 10th ed. Washington: National Immunization Program, CDC (US); 2007. pp. 149–58. [Google Scholar]
- 10.Centers for Disease Control and Prevention (US) CDC health update: corrected: multi-state mumps outbreak. [cited 2008 Jan 18]. Available from: URL: http://www2a.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00244.
- 11.Mumps outbreaks on university campuses—Illinois, Wisconsin, South Dakota. MMWR Morb Mortal Wkly Rep. 1987;36(30):496–8. 503–5. [PubMed] [Google Scholar]
- 12.Maldonado Y. Mumps. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson textbook of pediatrics. 17th ed. Philadelphia: Saunders; 2003. pp. 1035–6. [Google Scholar]
- 13.Krugman S, Katz S. Mumps (epidemic parotitis) In: Krugman S, editor. Infectious diseases of children. 7th ed. St. Louis: Mosby; 1981. pp. 195–207. [Google Scholar]
- 14.Litman N, Baum SG. Mumps virus. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 6th ed. Philadelphia: Elsevier; 2005. pp. p. 2003–8. [Google Scholar]
- 15.Cherry JD. Mumps virus. In: Feigin RD, Cherry JD, editors. Textbook of pediatric infectious diseases. 4th ed. Philadelphia: W.B. Saunders; 1998. pp. 2075–83. [Google Scholar]
- 16.Cortese MM, Jordan HT, Curns AT, Quinlan PA, Ens KA, Denning PM, et al. Mumps vaccine performance among university students during a mumps outbreak. Clin Infect Dis. 2008;46:1172–80. doi: 10.1086/529141. [DOI] [PubMed] [Google Scholar]
- 17.Buxton J, Craig C, Daly P, Bigham M, Bell A, Fyfe M. An outbreak of mumps among young adults in Vancouver, British Columbia, associated with “rave” parties. Can J Public Health. 1999;90:160–3. doi: 10.1007/BF03404498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sosin DM, Cochi SL, Gunn RA, Jennings CE, Preblud SR. Changing epidemiology of mumps and its impact on university campuses. Pediatrics. 1989;84:779–84. [PubMed] [Google Scholar]
- 19.Briss PA, Fehrs LJ, Parker RA, Wright PF, Sannella EC, Hutcheson RH, et al. Sustained transmission of mumps in a highly vaccinated population: assessment of primary vaccine failure and waning vaccine-induced immunity. J Infect Dis. 1994;169:77–82. doi: 10.1093/infdis/169.1.77. [DOI] [PubMed] [Google Scholar]
- 20.Henle G, Henle W, Wendell K, Rosenberg P. Isolation of mumps virus from human beings with induced apparent or inapparent infections. J Exp Med. 1948;88:223–32. doi: 10.1084/jem.88.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunell PA, Brickman A, O'Hare D, Steinberg S. Ineffectiveness of isolation of patients as a method of preventing the spread of mumps. Failure of the mumps skin-test antigen to predict immune status. N Engl J Med. 1968;279:1357–61. doi: 10.1056/NEJM196812192792502. [DOI] [PubMed] [Google Scholar]
- 22.Soud FA, Cortese MM, Curns AT, Edelson PJ, Bitsko RH, Jordan HT, et al. Isolation compliance among university students during a mumps outbreak, Kansas 2006. Epidemiol Infect. 2009;137:30–7. doi: 10.1017/S0950268808000629. [DOI] [PubMed] [Google Scholar]
- 23.Date AA, Kyaw MH, Rue AM, Klahn J, Obrecht L, Krohn T, et al. Long-term persistence of mumps antibody after receipt of 2 measles-mumps-rubella (MMR) vaccinations and antibody response after a third MMR vaccination among a university population. J Infect Dis. 2008;197:1662–8. doi: 10.1086/588197. [DOI] [PMC free article] [PubMed] [Google Scholar]