SYNOPSIS
Objectives
Orofacial clefts are common birth defects that often require multiple surgeries and medical treatments during childhood. We used health-care insurance claims data to estimate health-care expenditures for infants and children ≤10 years of age with an orofacial cleft.
Methods
The data were derived from the 2000–2004 MarketScan® Commercial Claims and Encounters databases, which include person-specific information on health-care use, expenditures, and enrollment for approximately 50 large employers, health plans, and government and public organizations. Health insurance claims data from 821,619 children ≤10 years of age enrolled in employer-sponsored plans during 2004 were analyzed. Expenditures for inpatient admissions, outpatient services, and prescription drug claims were calculated for children with and those without an orofacial cleft.
Results
The difference in annual mean costs (i.e., incremental costs) between children aged 0 through 10 years with an orofacial cleft and those without an orofacial cleft was $13,405. The mean and median costs for children ≤10 years of age with an orofacial cleft were eight times higher than for children of the same age without an orofacial cleft. Mean costs for infants with a cleft and another major, unrelated defect were 25 times higher than those for an infant without a cleft, and five times higher than for infants with an isolated cleft.
Conclusion
These findings document substantially elevated medical care costs for privately insured children with an orofacial cleft. Additional study of the economic burden associated with this condition should include a broader range of economic costs.
Orofacial clefts are common birth defects that occur when the tissues of the lip or palate do not join properly during embryologic development.1 National estimates adjusted for maternal race/ethnicity indicate that the prevalence of cleft palate in the U.S. is 6.4 per 10,000 live births, and the prevalence of cleft lip with and without cleft palate is 10.5 per 10,000 live births.2 Treatment for orofacial clefts often includes multiple surgeries and medical treatments during childhood.1,3 In addition to long-term morbidity, an increased risk of mortality has been noted among children and adults with cleft lip and palate.4,5
Little information is currently available concerning the economic effect of orofacial clefts on children, families, and society. With regard to orofacial clefts, cost analyses are important for estimating the benefits of primary prevention, allocating resources for research, assessing expenditures associated with secondary conditions among affected children, and evaluating treatment methodologies.6 The most recent estimate of the lifetime costs associated with cleft lip or palate—$101,000 per each new case—is based on data from a 1988 cohort.7 Snowden et al. used data from four national and two state data systems to estimate the costs of medically treated craniofacial conditions and reported an estimated cost of $11,350 per case of craniofacial congenital anomaly, which included cleft lip and palate.8 Finally, the findings of a recent report indicated that the mean neonatal hospital charges were $33,387 for an infant with cleft palate and $15,387 for an infant with cleft lip with or without cleft palate.9
In addition to a general paucity of data on health-care expenditures for children with an orofacial cleft, the available studies are limited in that the cost estimates were not specific to cleft phenotype (e.g., cleft lip, cleft palate, and cleft lip and palate), nor did they take into account whether the defect occurred in isolation; in combination with another major, unrelated defect; or as part of a syndrome. Because use and expenditure data are essential for monitoring trends in health and evaluating current and future health-care needs, we used health-care insurance claims data from a privately insured population in the U.S. to estimate health-care expenditures for infants and children ≤10 years of age with an orofacial cleft. We evaluated medical care expenditures according to the type of cleft and whether the cleft was an isolated defect or occurred in combination with another major, unrelated defect or syndrome.
METHODS
The data used for this analysis were obtained from the 2000–2004 MarketScan® Commercial Claims and Encounters databases, which consist of person-specific information on health-care use, expenditures, and enrollment for employees and dependents of approximately 50 large employers. The database is constructed by combining and standardizing multiple databases that Thomson Reuters builds on behalf of large employers and health plans across the nation. Data on health services use, medical care expenditures, and enrollment for inpatient and outpatient services and outpatient prescription drugs are included in the database and were evaluated for this study.
Children with clefts were identified by the presence of an International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code of 749.0–749.2 as any diagnosis code in an inpatient or outpatient claim. To maximize the likelihood of ascertaining an orofacial cleft diagnosis during any health-care encounter, data from 2000 through 2004 were used to identify children with an orofacial cleft. However, we only evaluated expenditures for health-care encounters that occurred during 2004, irrespective of when the diagnosis was noted. Because of substantial declines in the frequency of clefts diagnosed among older children in this data source, we restricted the analysis to infants and children ≤10 years of age. Children with codes for other birth defects (ICD-9-CM 740–759) on an inpatient admission or outpatient claim were reviewed by a clinical geneticist and classified as isolated (children with an orofacial cleft code with or without the presence of minor defects) or multiple/syndrome (children with an orofacial cleft code and a syndrome or other major, unrelated defect). The classification was based solely on ICD-9-CM codes, but generally followed guidelines developed for the National Birth Defects Prevention Study.10
We included children who were continuously enrolled during 2004 in a fee-for-service plan and for whom data on pharmaceutical claims were available. The comparison group consisted of all other children ≤10 years of age who were continuously enrolled in a fee-for-service plan during 2004 with available data on pharmaceutical claims. Age was calculated as the age of the child as of December 1, 2004, regardless of whether the child had an encounter during that month. Because age in months was not available in the dataset and efforts to restrict the infant (age 0) subgroup to a criteria of at least 11 months of continuous enrollment resulted in the exclusion of nearly all infants born in 2004, we identified all infants with an age of 0 recorded in the 2004 enrollment data and followed the infant back to 2003 or forward to 2005 to identify the first 12 months of life for which at least 11 months of continuous enrollment data were available. Thus, infants with less than 11 months of continuous enrollment were excluded from the analysis. Enrollees with and those without claims were included in the study population, and costs for nonusers were set to $0.
The data used for this analysis were extracted from the MarketScan Research Databases;11 analyses were conducted using SAS® version 9.1.12 Administrative prevalence was calculated as the number of children with orofacial clefts divided by the total number of children continuously enrolled during 2004. Birth hospitalizations lasting less than four days were excluded from the inpatient admissions, but longer birth hospitalizations were included because it was assumed that most of the costs for longer birth hospitalizations were associated with medical complications and not the birth itself.
Total expenditures were calculated as the sum of insurance reimbursements and out-of-pocket expenditures by families. Total expenditures were used as a proxy for the costs of health-care services, although mean expenditures vary by the type of payer. Mean and median total expenditures and expenditures for inpatient admissions, outpatient services, and prescription drug claims were calculated for children with and those without an orofacial cleft. Incremental costs were also calculated and represent the difference between the mean or median costs for children with an orofacial cleft and the mean or median costs for those without an orofacial cleft. Because a considerable proportion of infants were classified as having another major, unrelated defect or syndrome, we elected to stratify these data by infants and noninfants to reduce potential bias due to skewed cost estimates.
RESULTS
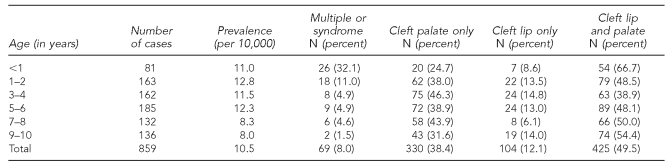
After all exclusions were applied, a total of 821,619 children ≤10 years of age were continuously enrolled in a fee-for-service plan during 2004. Of these children, 859 had a medical diagnosis of an orofacial cleft recorded for an inpatient or outpatient encounter during the period 2000–2004 (Table 1). The administrative prevalence of orofacial clefts for all children ≤10 years of age was 10.5 per 10,000, with the highest prevalence—12.8 per 10,000—noted among children 1 and 2 years of age. After age 6, the prevalence of orofacial clefts declined to approximately 8.0 per 10,000. Approximately 32% of infants (aged <1 year) with an orofacial cleft were classified as having a major, unrelated defect or syndrome compared with only 5% of children aged 3 through 8 and less than 2% of 9- to 10-year-olds. A diagnosis of cleft lip and palate was observed most frequently (50%) for children ≤10 years of age with an orofacial cleft, followed by cleft palate only (38%) and cleft lip only (12%). This pattern was similar for all age groups except children 3 and 4 years of age, for whom the most frequent diagnosis was cleft palate only (46%).
Table 1.
Administrative prevalence of orofacial clefts and distribution of cleft type among children ≤10 years of age among a privately insured U.S. population, MarketScan® Research Database, 2004
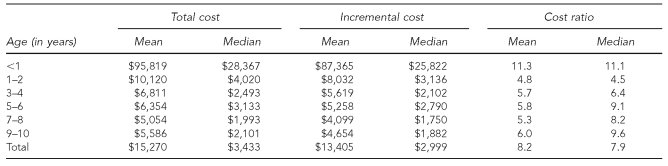
Mean total expenditures during 2004 for children with clefts were highest for infants ($95,819) and decreased with increasing age to a minimum of $5,054 at 7 to 8 years of age (Table 2). Median expenditures, which reflect the annual health-care cost for the average child with a cleft, also decreased with increasing age: from $28,367 for infants to approximately $2,000 at 7 to 10 years of age.
Table 2.
Incremental costs and cost ratios for orofacial clefts among children ≤10 years of age among a privately insured U.S. population, MarketScan® Research Database, 2004
Overall, the mean and median costs for children ≤10 years of age with orofacial clefts were eight times higher than for children of the same age without an orofacial cleft (Table 2). The difference in individual mean costs (i.e., incremental costs) between children ≤10 years of age with an orofacial cleft and those without an orofacial cleft was $13,405. For infants with an orofacial cleft, mean and median costs were 11 times higher than for children without a cleft, and the mean incremental cost per child was $87,365. In general, the mean costs for children ≥1 year of age with orofacial clefts were five to six times higher than those for children of the same age without orofacial clefts. The median cost ratios for children ≥1 year of age with orofacial clefts ranged from 4.5 for 1- to 2-year-olds to 9.6 for 9- to 10-year-olds.
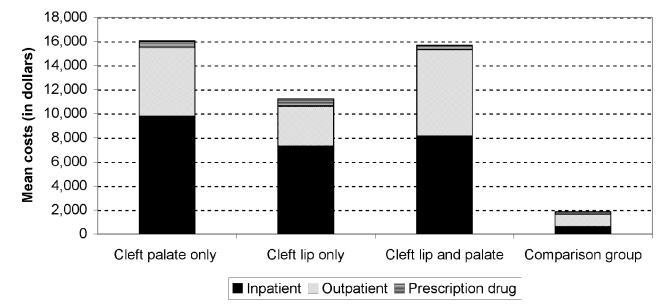
The Figure depicts the mean component costs (i.e., inpatient, outpatient, and prescription drugs) according to cleft phenotype for children with and those without an orofacial cleft. Total mean costs for children with cleft palate only and cleft lip and palate were approximately 1.4 times greater than total mean costs for children with cleft lip only. For all phenotypes, more than half of the total mean costs were attributable to inpatient admissions, compared with 32% for the comparison group. Overall, prescription drug costs for children with orofacial clefts were two to three times higher than those for children without clefts.
Figure.
Mean component costs for children ≤10 years of age with or without an orofacial cleft among a privately insured U.S. population, MarketScan® Research Database, 2004
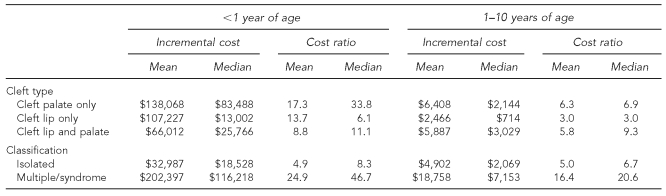
Mean costs for children 1 to 10 years of age with cleft palate only and cleft lip and palate were approximately six times higher than mean costs for children of the same age without an orofacial cleft, whereas mean costs for children 1 to 10 years of age with cleft lip were three times higher (Table 3). Mean cost ratios for infants ranged from 8.8 for cleft lip and palate to 17.3 for cleft palate only. The mean incremental cost for children 1 to 10 years of age with an orofacial cleft and another major, unrelated defect or syndrome was nearly four times higher than the incremental cost for a child of the same age with an isolated cleft. Incremental costs for infants with a cleft and another major, unrelated defect were six times higher than for infants with an isolated cleft. Mean costs for infants with a cleft and another major, unrelated defect were 25 times higher than those for an infant without a cleft.
Table 3.
Incremental costs and cost ratios for orofacial clefts by type and classification among children ≤10 years of age among a privately insured U.S. population, MarketScan® Research Database, 2004
DISCUSSION
These findings indicate that the mean and median costs for children with an orofacial cleft were approximately eight times greater than for children without a cleft, and suggest a substantial economic burden associated with orofacial clefts, particularly for those with another major, unrelated defect or syndrome. In contrast, a previous study based on California data from the period 1988–1989 reported that medical costs were 2.5 times higher for children <5 years of age with a cleft and only 1.5 times higher for children 5 through 17 years of age with a cleft.13 These findings suggest that the relative use of medical care by U.S. children with an orofacial cleft has increased substantially during the last two decades. A similar increase in relative costs has been reported for children with Down syndrome,14 but not for children with spina bifida.15
Although the cost estimates presented in this article were limited to a privately insured population of children, they can contribute to a greater understanding of the medical care costs associated with orofacial clefts and the potential benefits of prevention strategies. Indeed, the additional study of such costs has been identified as a priority for future public health research in orofacial clefts.6 It should be noted, however, that the costs presented in this article are estimates of the relative costs for a population of children with orofacial clefts compared with children without orofacial clefts. The expenditures in this study represent costs for all health-care encounters during 2004, not just those costs directly associated with the medical treatment for orofacial clefts.
The national estimates of cleft palate only (6.4 per 10,000 live births) and cleft lip with or without cleft palate (10.5 per 10,000 live births)2 derived from birth defects surveillance data were considerably higher than comparable estimates based on our administrative data (4.0 per 10,000 and 6.4 per 10,000, respectively). The former estimates were based on data from population-based surveillance systems, which have more complete and accurate ascertainment than do administrative data systems. In addition, children with an orofacial cleft might be more likely to be covered by public health insurance, which could have contributed to the lower prevalence among this privately insured population.
Approximately 92% of the children in our study population were found to have an isolated cleft. This proportion was considerably higher than other estimates, which indicated that 64% to 70% of clefts were isolated.16,17 However, the proportion of infants in this analysis found to have an isolated cleft (68%) was consistent with the aforementioned estimates. Because the multiple or syndrome classification used in this analysis relied on a code-based review without additional description, it is likely that a proportion of cases were misclassified, particularly among older children. Underascertainment of syndromic or other major defect diagnoses and orofacial clefts diagnoses in older children might have been due to other factors, such as death; incomplete notation of the ICD-9-CM code during the health-care encounter—either because the health-care provider felt that the additional diagnosis was not relevant to the current treatment or because the child entered the system at a later age and the birth diagnosis was not noted on the claim; possible lack of financial incentives to note the other diagnosis; or attrition, as children moved to other insurance mechanisms as they got older. This misclassification would have had the effect of overstating the costs for isolated defects; the effect on costs for children with multiple major defects or syndromes is unknown.
Limitations
The results of this study were subject to several limitations. MarketScan® data are based on a sample of privately insured children covered by large corporate employee health plans; thus, the cost estimates are not necessarily representative of all children in the U.S. Although multiple years of data were used to identify orofacial cleft diagnoses, it is likely that a proportion of cases were not ascertained, particularly among older children, because the condition was not noted during any encounter. The administrative prevalence of orofacial clefts declined from 12.3 per 10,000 among 5- and 6-year-old children to 8.0 per 10,000 among children 9 to 10 years of age. This suggests that, once a cleft is repaired, the condition might be less likely to be noted during a subsequent health-care encounter. Accordingly, cost differences were most pronounced among infants.
Elevated costs in older children with orofacial clefts may be due to secondary surgeries or medical treatments for other related or unrelated conditions. These data were also limited because no information was available on maternal and infant characteristics, such as maternal age and race/ethnicity, that might be associated with a greater risk of orofacial clefts.18 Lastly, the cost estimates derived in this analysis might have underestimated the actual direct medical costs associated with orofacial clefts for children who were covered by more than one health-care plan. Because we restricted the analysis to infants with at least 11 months of continuous enrollment, infants who died during the first few months of life were not included in this analysis and were therefore not included in the cost estimates.
CONCLUSION
The medical care costs for this privately insured population of children with an orofacial cleft were substantially higher than those for a comparable group of children without an orofacial cleft, and were indicative of the economic burden associated with this condition. Furthermore, families of children with an orofacial cleft might face other nonmedical costs that could not be assessed in this analysis, such as educational assessments, special education, child care, transportation, lost productivity or earnings, and forgone employment for caregivers.6,19,20 There is also some evidence that orofacial clefts among children, particularly among adolescents, are associated with other long-term outcomes, such as behavioral and emotional difficulties,21 lower self-concept,22 and lower health-related quality of life scores because of speech and aesthetic concerns.23 As such, additional study of the financial burden and quality of life for children with an orofacial cleft and their families is warranted.
Acknowledgments
The authors thank Richard Olney, MD, MPH, for his assistance in the review and classification of children with orofacial clefts.
Footnotes
This research was supported in part by an appointment to the Research Participation Program at the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention (CDC), administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.Arosarena OA. Cleft lip and palate. Otolaryngol Clin North Am. 2007;40:27–60. doi: 10.1016/j.otc.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Canfield MA, Honein MA, Yuskiv N, Xing J, Mai CT, Collins JS, et al. National estimates and race/ethnic-specific variation of selected birth defects in the United States, 1999–2001. Birth Defects Res A Clin Mol Teratol. 2006;76:747–56. doi: 10.1002/bdra.20294. [DOI] [PubMed] [Google Scholar]
- 3.Bender PL. Genetics of cleft lip and palate. J Pediatr Nurs. 2000;15:242–9. doi: 10.1053/jpdn.2000.8148. [DOI] [PubMed] [Google Scholar]
- 4.Christensen K, Juel K, Herskind AM, Murray JC. Long-term follow-up study of survival associated with cleft lip and palate at birth. BMJ. 2004;328:1405. doi: 10.1136/bmj.38106.559120.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ngai CW, Martin WL, Tonks A, Wyldes MP, Kilby MD. Are isolated facial cleft lip and palate associated with increased perinatal mortality? A cohort study from the West Midlands Region, 1995–1997. J Matern Fetal Neonatal Med. 2005;17:203–6. doi: 10.1080/14767050500072854. [DOI] [PubMed] [Google Scholar]
- 6.Yazdy MM, Honein MA, Rasmussen SA, Frias JL. Priorities for future public health research in orofacial clefts. Cleft Palate Craniofac J. 2007;44:351–7. doi: 10.1597/06-233.1. [DOI] [PubMed] [Google Scholar]
- 7.Economic costs of birth defects and cerebral palsy—United States, 1992. MMWR Morb Mortal Wkly Rep. 1995;44(37):694–9. [PubMed] [Google Scholar]
- 8.Snowden CB, Miller TR, Jensen AF, Lawrence BA. Costs of medically treated craniofacial conditions. Public Health Rep. 2003;118:10–7. doi: 10.1016/S0033-3549(04)50212-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects—United States, 2003. MMWR Morb Mortal Wkly Rep. 2007;56(2):25–9. [PubMed] [Google Scholar]
- 10.Rasmussen SA, Olney RS, Holmes LB, Lin AE, Keppler-Noreuil KM, Moore CA. Guidelines for case classification for the National Birth Defects Prevention Study. Birth Defects Res A Clin Mol Teratol. 2003;67:193–201. doi: 10.1002/bdra.10012. [DOI] [PubMed] [Google Scholar]
- 11.SAS Institute, Inc. SAS: Version 9.1. Cary (NC): SAS Institute, Inc; 2003. [Google Scholar]
- 12.Thomson Medstat. Marketscan Database. Ann Arbor (MI): Thomson Medstat; 2004. [Google Scholar]
- 13.Waitzman NJ, Scheffler RM, Romano PS. The cost of birth defects: estimates of the value of prevention. Lanham (MD): University Press of America; 1996. [Google Scholar]
- 14.Boulet SL, Molinari NA, Grosse SG, Honein MA, Correa-Villasenor A. Health care expenditures for children with Down syndrome in a privately insured population. J Pediatr. 2008;153:241–6. doi: 10.1016/j.jpeds.2008.02.046. [DOI] [PubMed] [Google Scholar]
- 15.Ouyang L, Grosse SD, Armour BS, Waitzman NJ. Health care expenditures of children and adults with spina bifida in a privately insured U.S. population. Birth Defects Res A Clin Mol Teratol. 2007;79:552–8. doi: 10.1002/bdra.20360. [DOI] [PubMed] [Google Scholar]
- 16.Jones MC. Etiology of facial clefts: prospective evaluation of 428 patients. Cleft Palate J. 1988;25:16–20. [PubMed] [Google Scholar]
- 17.Tolarova MM, Cervenka J. Classification and birth prevalence of orofacial clefts. Am J Med Genet. 1998;75:126–37. [PubMed] [Google Scholar]
- 18.DeRoo LA, Gaudino JA, Edmonds LD. Orofacial cleft malformations: associations with maternal and infant characteristics in Washington State. Birth Defects Res A Clin Mol Teratol. 2003;67:637–42. doi: 10.1002/bdra.10114. [DOI] [PubMed] [Google Scholar]
- 19.Anderson D, Dumont S, Jacobs P, Azzaria L. The personal costs of caring for a child with a disability: a review of the literature. Public Health Rep. 2007;122:3–16. doi: 10.1177/003335490712200102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuhlthau KA, Perrin JM. Child health status and parental employment. Arch Pediatr Adolesc Med. 2001;155:1346–50. doi: 10.1001/archpedi.155.12.1346. [DOI] [PubMed] [Google Scholar]
- 21.Millard T, Richman LC. Different cleft conditions, facial appearance, and speech: relationship to psychological variables. Cleft Palate Craniofac J. 2001;38:68–75. doi: 10.1597/1545-1569_2001_038_0068_dccfaa_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 22.Broder H, Strauss RP. Self-concept of early primary school age children with visible or invisible defects. Cleft Palate J. 1989;26:114–7. [PubMed] [Google Scholar]
- 23.Damiano PC, Tyler MC, Romitti PA, Momany ET, Jones MP, Canady JW, et al. Health-related quality of life among preadolescent children with oral clefts: the mother's perspective. Pediatrics. 2007;120:e283–90. doi: 10.1542/peds.2006-2091. [DOI] [PubMed] [Google Scholar]