Abstract
OBJECTIVES
To investigate the correlation and agreement between the intraocular pressure peaks detected during the water drinking test and the modified diurnal tension curve in untreated glaucomatous eyes.
INTRODUCTION
It has been suggested that the intraocular pressure peaks detected during the water drinking test predict the peaks observed during a 24-hour diurnal tension curve. A more feasible and practical test for assessing intraocular pressure peaks in glaucomatous eyes during office hours would be of great clinical utility.
METHODS
This was a prospective study involving open angle glaucoma patients without anti-glaucoma medication submitted to the modified diurnal tension curve and water drinking test on the same day. The intraocular pressure peaks during the water drinking test and the modified diurnal tension curve were reported and compared. Statistical analysis was performed to assess the correlation and agreement between intraocular pressure peak measurements.
RESULTS
The correlation between intraocular pressure peaks during the water drinking test and modified diurnal tension curve was significant and strong (Pearson’s Correlation Coefficient r=0.780, p<0.0001). Limited agreement was observed between these measurements. Eighty-two percent of intraocular pressure peaks were higher during the water drinking test than the modified diurnal tension curve.
DISCUSSION
These findings suggest that the water drinking test may be used as tool to assess risk factors for glaucomatous patients.
CONCLUSION
Intraocular pressure peaks detected during the water drinking test could be used in clinical practice to both estimate the peaks observed during the modified diurnal tension curve and assess the status of the eye’s outflow facility.
Keywords: Fluctuation, intraocular pressure, stress test, correlation, water drinking test
INTRODUCTION
Intraocular pressure (IOP) is the main risk factor for the development and progression of glaucoma.1–5 Routine office measurements may not detect IOP peaks in roughly 30% of patients,4 and this detection failure may be responsible for visual field progression in apparently controlled patients.5
Twenty-four hour daily tension curves (DTC) can estimate IOP peaks and fluctuations to provide the practitioner with more reliable information regarding the short-term IOP profile. However, 24-hour IOP monitoring may be unfeasible and time consuming for both patients and physicians; thus, it may be a restricted tool in clinical practice.
The modified diurnal tension curve (mDTC), an alternative that involves IOP measurements every 2 or 3 hours during office hours, is more feasible and may provide better information regarding the IOP profile than single IOP measurements.
Stress tests, such as the glucose-50 test for diabetes6 and dobutamine stress echo in cardiology,7 have been used in general medicine to assess risk factors for different types of disease.
The water drinking test (WDT) has been used as a stress test to evaluate how an eye is able to deal with a transient IOP elevation.8–11 Recent studies have shown the relationship between the WDT results and the severity and progression of glaucoma.10,11 It has been proposed that there is a significant correlation between the IOP peaks detected during the WDT and the 24-hour DTC.8–10
The aim of this study is to assess whether there is correlation between IOP peaks detected during the WDT and mDTC in untreated open angle glaucomatous eyes.
MATERIALS AND METHODS
Approval from the Institutional Review Board Ethics Committee was obtained for this study. The study followed the principles of the Declaration of Helsinki, and informed consent was obtained from all participants enrolled in the study.
This was a prospective intervention study involving primary open angle glaucoma patients. Glaucoma was defined by the presence of typical optic neuropathy12 with associated visual field (VF) defects that were demonstrated in at least two consecutive reliable examinations using Humphrey standard automated perimetry (Humphrey Inc., Dublin, CA, USA). Gonioscopic evaluation was performed in all patients, and only those who presented open angles (i.e., such that the pigmented trabeculum was visible in all four sectors without indentation) were enrolled in the study. Subjects with severe stage glaucoma (vertical cup/disc ratio larger than 0.8 and mean deviation value ≤ −12.0 dB), submitted to previous intraocular procedures, and those who were receiving topical and/or systemic medication that could interfere with IOP measurements were excluded.
Following screening, eligible patients began the required washout periods for current ocular medication as follows: 4 weeks for beta-adrenergic receptor antagonists and prostaglandin analogs, 2 weeks for adrenergic agonists, and 5 days for cholinergic agonists and carbonic anhydrase inhibitors. Patients whose ocular hypotensive therapy required a 4-week washout had an additional safety check visit 2 weeks prior to the baseline measurement. If a patient’s IOP had risen to a level thought to be detrimental (based on the severity of VF damage) at the time of the safety visit, the patient was withdrawn from the study. After this period, all patients were submitted to the mDTC and underwent IOP measurements at 8 am, 10 am, 12 pm, 2 pm, and 4 pm. After the last measurement, the WDT was performed. This procedure involved ingestion of 1 liter of tap water in 5 minutes, and IOP measurements 15, 30, and 45 minutes later. Goldman Tonometry was used in both situations.
The IOP peaks of the right eye of each eligible subject were recorded and compared. For statistical analysis, Pearson’s coefficient (r) and the Bland-Altman plots were used to study the correlation and agreement between the mDTC and WDT peaks, respectively. Computerized analysis was performed using MedCalc® (MedCalc Software version 9.3.2.0, Belgium).
RESULTS
Ninety-seven patients (97 eyes) fulfilled the inclusion criteria and completed the study.
The average age was 43.2 years (± 6.4). Females were 60.8% of the studied population, and 30.9% were black.
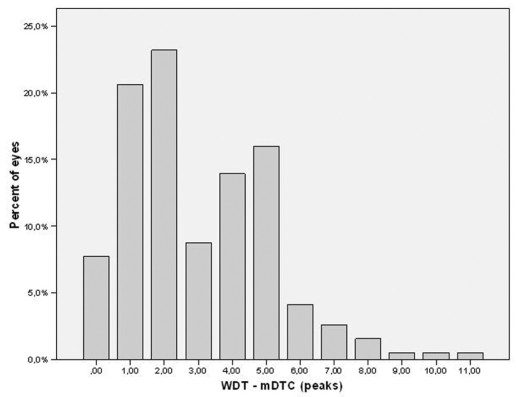
Figure 1 shows the distribution frequency of differences between IOP peaks during the WDT and mDTC.
Figure 1.
Distribution frequency of the differences between IOP peaks during the WDT and mDTC
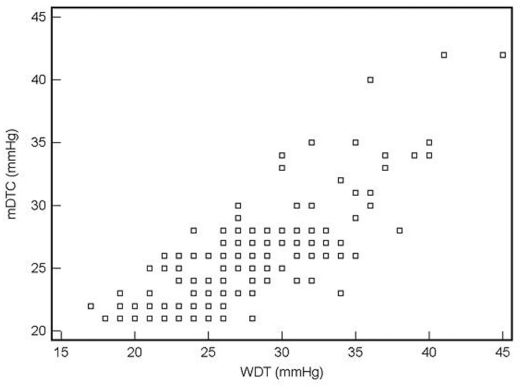
The WDT peak was significantly correlated with the mDTC peak (Person’s Correlation Coefficient r=0.780 for a 95% confidence interval between 0.716 to 0.831, p<0.0001) (Figure 2).
Figure 2.
Correlation between IOP peaks during the WDT and mDTC
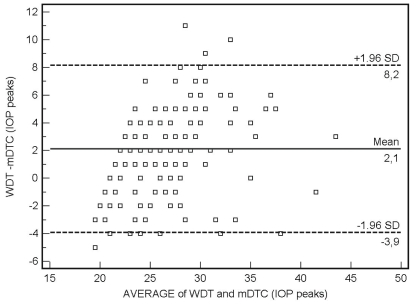
Figure 3 shows a Bland-Altman Plot demonstrating limited agreement between IOP peak measurements. The 95% limits of agreement between the WDT and mDTC IOP peaks ranged from −3.9 mmHg to 8.2 mmHg. In 52.5% of the tests, the agreement was within ± 2 mmHg.
Figure 3.
Agreement between the WDT and mDTC peaks
Eighty-two percent of eyes showed higher IOP peaks during the WDT than the mDTC (95% confidence interval between 0.0 and 6.99 mmHg).
DISCUSSION
Mean IOP, IOP peaks, and IOP fluctuation are important risk factors for the progression of glaucoma,2,3,13,14 but precise IOP assessment is very difficult in clinical practice. A 24-hour DTC would better characterize a given patient’s short-term IOP profile. However, the cost and labor involved make the determination of the 24-hour IOP course difficult and not possible for all patients. Previous studies observed significant correlations between IOP peaks measured during the 24-hour DTC and WDT.8,9,15 The WDT is a stress test that was widely used a few decades ago to diagnose open angle glaucoma;9,16 due to its high incidence of false positive and false negative results, however, it was deemed inadequate. Recently, the emphasis on the value of this test has changed. It has been used as a surrogate marker for the outflow facility reserve and may indicate the likelihood of progression.17 Brubaker suggested that the WDT is a clinically useful test for assessing the status of outflow facility.18 Previous studies have also suggested the importance of the WDT as a risk factor for the development of glaucomatous VF defects. Based on a large prospective study (Collaborative Glaucoma Study), Armaly and coworkers19,20 reported in the 1980s that the pressure change after drinking water is one of five potential risk factors significantly related to the development of glaucomatous VF defects in patients with ocular hypertension. Yoshikawa et al also showed that the WDT was the most clinically relevant useful predictor of VF progression in normal tension glaucomatous eyes.11 Susanna et al. demonstrated that eyes with similar IOP levels under steady state conditions can respond to pressure perturbations differently in terms of both the pressure rise and speed of recovery. In more affected eyes, the pressure rises higher for a longer time than it does in less affected eyes.21
The mechanisms involved in the WDT are not completely understood. After water or any hypotonic fluid is consumed, water is absorbed into the blood and body tissues (including the eye). This is associated with a consequent rise in IOP. The ability of the eye to recover from this transient IOP rise depends on the outflow facility. The rapid inflow of aqueous humor and the impaired facility of outflow in the glaucomatous eye may partially lead to IOP elevation. Brucculeri et al. suggested that factors affecting aqueous drainage may explain the water drinking effect.22
The mDTC has become a common practice and consists of four to five IOP measurements taken during office hours (from 8 am to 6 pm). However, this test may miss as much as 70% of IOP peaks due to both IOP variability and the fact that 70% of the highest IOP levels occur in the morning in the supine position.1,23,24
The present study showed that there is a strong correlation between the peak of the WDT and that of the mDTC; however, the agreement between these peaks is limited (Bland-Altman Plot in Figure 3). It is interesting to note that 82% of the WDT peaks were higher than the mDTC peaks.
In order to understand the practical implications of our findings, the clinician should be reminded of the definitions of correlation and agreement. Correlation indicates the strength and direction of the linear relationship between two variables. Once an independent continuous variable (x) increases, the other variable (y) will increase, decrease, or remain stable depending on the degree of association between them. The strong and positive correlation between the IOP peaks during the WDT and mDTC can thus be interpreted as follows. If an eye presents high IOP peaks during this stress test, this eye might also present higher peaks during the mDTC. However, this does not mean that the values are the same. Roughly 82% of the IOP peaks were higher during the WDT, and the difference between them averaged 2mm Hg. Thus, the two methods show limited agreement after statistical analysis. Because of the considerable inter-observer and intra-observer variability in the accuracy of IOP measurements made with Goldman tonometry (around 2 mmHg), however, the relevance of such a difference may be diminished during WDT evaluation in a clinical practice. Moreover, even though most IOP peaks usually occur between 5 and 7 am in a complete DTC (gold standard), the mDTC performed in this study started at 8 am. This may have led to a failure to detect IOP peaks,23 which may explain the limited agreement between the methods.
In summary, this study corroborates previous reports that demonstrate the clinical applicability of the WDT as a useful tool for assessing both the status of the eye’s outflow facility and the likelihood of glaucoma progression.11,17–20
Furthermore, prospective studies are necessary to evaluate whether measurements obtained during the WDT and mDTC are important indicators of prognostic outcome in glaucoma patients.
REFERENCES
- 1.Liu JH. Diurnal measurement of intraocular pressure. J Glaucoma. 2001;10:S39–41. doi: 10.1097/00061198-200110001-00015. [DOI] [PubMed] [Google Scholar]
- 2.The Advanced Glaucoma Intervention Study (AGIS):7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am J Ophthalmol. 2000;130:429–40. doi: 10.1016/s0002-9394(00)00538-9. [DOI] [PubMed] [Google Scholar]
- 3.The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol. 1998;126:498–505. doi: 10.1016/s0002-9394(98)00272-4. [DOI] [PubMed] [Google Scholar]
- 4.Drance SM. Diurnal variation of intraocular pressure in treated glaucoma. Arch Ophthalmol. 1963;70:302–11. doi: 10.1001/archopht.1963.00960050304004. [DOI] [PubMed] [Google Scholar]
- 5.Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Lindenmuth K, et al. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma. 2000;9:134–42. doi: 10.1097/00061198-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Decode Study Group, the European Diabetes Epidemiology Group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-h diagnostic criteria. Arch Intern Med. 2001:397–405. doi: 10.1001/archinte.161.3.397. [DOI] [PubMed] [Google Scholar]
- 7.Berthe C, Pierard LA Hiernaux M, Trotteur G, Lempereur P, Carlier J, et al. Predicting the extent and location of coronary artery disease in acute myocardial infarction by echocardiography during dobutamine infusion. Am J Cardiol. 1986:1167–72. doi: 10.1016/0002-9149(86)90376-0. [DOI] [PubMed] [Google Scholar]
- 8.Helal J. Contribuição ao estudo da pressão intraocular: picos da pressão intraocular na curva diária e na prova de sobrecarga hídrica. Rev Bras Oftal. 1988;47:75–80. [Google Scholar]
- 9.Frankelson EN. The role of water test in evaluation of glaucoma control. Can J Ophthalmol. 1974;9:408–10. [PubMed] [Google Scholar]
- 10.Susanna R, Vessani RM, Sakata L, Zacarias LC, Hatanaka M. The relation between intraocular pressure peak in the water drinking test and visual field progression in glaucoma. Br J Ophthalmol. 2005;89:1298–301. doi: 10.1136/bjo.2005.070649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshikawa K, Inoue T, Inoue Y. Normal tension glaucoma: the value of predictive tests. Acta Ophthalmol (Copenh) 1993;71:463–70. doi: 10.1111/j.1755-3768.1993.tb04619.x. [DOI] [PubMed] [Google Scholar]
- 12.Susanna R, Vessani RM. New findings in the evaluation of the optic disc in glaucoma diagnosis. Curr Opin Ophthalmol. 2007;18:122–8. doi: 10.1097/ICU.0b013e328040bfe0. [DOI] [PubMed] [Google Scholar]
- 13.Nouri-Mahdavi K, Hoffman D, Coleman AL, Liu G, Li G, Gaasterland D, et al. Advanced Glaucoma Intervention Study. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology. 2004;111:1627–35. doi: 10.1016/j.ophtha.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 14.Bengtsson B, Leske MC, Hyman L, Heijl A Early Manifest Glaucoma Trial Group. Fluctuation of intraocular pressure and glaucoma progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:205–9. doi: 10.1016/j.ophtha.2006.07.060. [DOI] [PubMed] [Google Scholar]
- 15.Hu WD, Medeiros FA, Alencar LMP, Liu JH, Susanna R, Weinreb RN. The correlation between the water drinking test and 24 hour intraocular pressure measurements in glaucomatous eyes. Poster presented during the Meeting of the Association for Research in Vision and Ophthalmology (ARVO); May 2007; Fort Lauderdale-FL. [Google Scholar]
- 16.Roth JA. Inadequate diagnostic value of the water drinking test. Br J Ophthalmol. 1974;58:55–61. doi: 10.1136/bjo.58.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Susanna R, Vessani RM, Sakata L, Zacarias LC, Hatanaka M. The relation between intraocular pressure peak in the water drinking test and visual field progression in glaucoma. Br J Ophthalmol. 2005;89:1298–301. doi: 10.1136/bjo.2005.070649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brubaker RF. Importance of outflow facility. Int Glaucoma Rev. 2001;3:5. [Google Scholar]
- 19.Armaly MF. Lessons to be learned from the Collaborative Glaucoma Study. Surv Ophthalmol. 1980;25:139–44. doi: 10.1016/0039-6257(80)90089-2. [DOI] [PubMed] [Google Scholar]
- 20.Armaly MF, Krueger DE, Maunder L, Becker B, Hetherington J, Jr, Kolker AE, et al. Bioestatistical analysis of the Collaborative Glaucoma Study. I. Summary report of the risk factors for glaucomatous visual field defects. Arch Ophthalmol. 1980;98:2163–71. doi: 10.1001/archopht.1980.01020041015002. [DOI] [PubMed] [Google Scholar]
- 21.Susanna R, Jr, Hatanaka M, Vessani RM, Pinheiro A, Morita C. Correlation of asymmetric glaucomatous visual field damage and water drinking test response. Invest Ophthalmol Vis Sci. 2006;47:641:4. doi: 10.1167/iovs.04-0268. [DOI] [PubMed] [Google Scholar]
- 22.Brucculeri M, Hammel T, Harris A, Malinovsky V, Martin B. Regulation of intraocular pressure after water drinking. J Glaucoma. 1999;8:111–6. [PubMed] [Google Scholar]
- 23.Liu JH, Bouligny RP, Kripke DF, Weinreb RN. Nocturnal elevation of intraocular pressure is detectable in the sitting position. Invest Ophthalmol Vis Sci. 2003;44:4439–42. doi: 10.1167/iovs.03-0349. [DOI] [PubMed] [Google Scholar]
- 24.Liu JH, Sit AJ, Weinreb RN. Variation of 24-hour intraocular pressure in healthy individuals: right eye versus left eye. Ophthalmology. 2005;112:1670–5. doi: 10.1016/j.ophtha.2005.05.007. [DOI] [PubMed] [Google Scholar]