Abstract
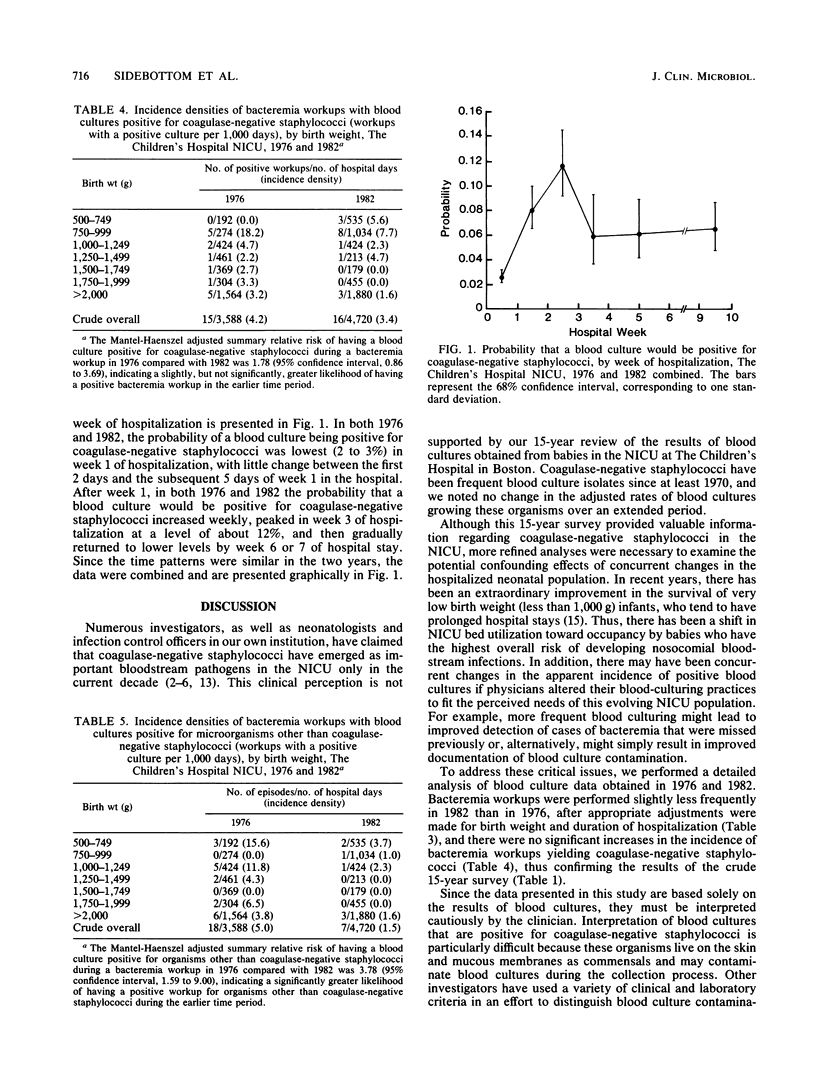
Investigators worldwide, as well as the neonatologists and infection control team at our hospital, have reported that the incidence of coagulase-negative staphylococcal bacteremia in critically ill neonates has increased dramatically in recent years. To investigate these claims, we examined the results of all blood cultures obtained from 1970 to 1984 in our neonatal intensive care unit. Throughout this study period, coagulase-negative staphylococci were prominent blood culture isolates (crude overall incidence of 4.4 positive bacteremia workups per 100 neonates admitted; range, 2.5 to 6.7), representing 26.3 to 69.6% of all positive cultures. There was no significant increase in incidence over time by analysis of linear trend. Detailed analysis of data from 1976 and 1982 (two selected years for which complete information concerning culturing practices and patient characteristics was available) revealed that these observations were not explained by changes in the frequency of blood culturing. In both 1976 and 1982, the probability that a blood culture would grow coagulase-negative staphylococci increased steadily from 2 to 3% shortly after admission to reach a level of about 12% in week 3 of hospitalization, before declining to an intermediate level thereafter. This pattern is more consistent with nosocomial bacteremia than with contamination of blood cultures. Contrary to clinical reports, coagulase-negative staphylococci have been the principal pathogens isolated from blood cultures in our neonatal intensive care unit since at least 1970, with no measurable increase over the subsequent 14 years.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Archer G. L. Coagulase-negative staphylococci in blood cultures: the clinician's dilemma. Infect Control. 1985 Dec;6(12):477–478. doi: 10.1017/s019594170006358x. [DOI] [PubMed] [Google Scholar]
- Battisti O., Mitchison R., Davies P. A. Changing blood culture isolates in a referral neonatal intensive care unit. Arch Dis Child. 1981 Oct;56(10):775–778. doi: 10.1136/adc.56.10.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgart S., Hall S. E., Campos J. M., Polin R. A. Sepsis with coagulase-negative staphylococci in critically ill newborns. Am J Dis Child. 1983 May;137(5):461–463. doi: 10.1001/archpedi.1983.02140310043012. [DOI] [PubMed] [Google Scholar]
- Calnen G., Campognone P., Peter G. Coagulase-negative staphylococcal bacteremia in newborns. Clin Pediatr (Phila) 1984 Oct;23(10):542–544. doi: 10.1177/000992288402301002. [DOI] [PubMed] [Google Scholar]
- Donowitz L. G., Haley C. E., Gregory W. W., Wenzel R. P. Neonatal intensive care unit bacteremia: emergence of gram-positive bacteria as major pathogens. Am J Infect Control. 1987 Aug;15(4):141–147. doi: 10.1016/0196-6553(87)90137-4. [DOI] [PubMed] [Google Scholar]
- Fleer A., Senders R. C., Visser M. R., Bijlmer R. P., Gerards L. J., Kraaijeveld C. A., Verhoef J. Septicemia due to coagulase-negative staphylococci in a neonatal intensive care unit: clinical and bacteriological features and contaminated parenteral fluids as a source of sepsis. Pediatr Infect Dis. 1983 Nov-Dec;2(6):426–431. doi: 10.1097/00006454-198311000-00003. [DOI] [PubMed] [Google Scholar]
- Freeman J., McGowan J. E., Jr Day-specific incidence of nosocomial infection estimated from a prevalence survey. Am J Epidemiol. 1981 Dec;114(6):888–901. doi: 10.1093/oxfordjournals.aje.a113259. [DOI] [PubMed] [Google Scholar]
- Freeman J., Platt R., Sidebottom D. G., Leclair J. M., Epstein M. F., Goldmann D. A. Coagulase-negative staphylococcal bacteremia in the changing neonatal intensive care unit population. Is there an epidemic? JAMA. 1987 Nov 13;258(18):2548–2552. [PubMed] [Google Scholar]
- Goldmann D. A., Leclair J., Macone A. Bacterial colonization of neonates admitted to an intensive care environment. J Pediatr. 1978 Aug;93(2):288–293. doi: 10.1016/s0022-3476(78)80523-x. [DOI] [PubMed] [Google Scholar]
- Kirchhoff L. V., Sheagren J. N. Epidemiology and clinical significance of blood cultures positive for coagulase-negative staphylococcus. Infect Control. 1985 Dec;6(12):479–486. doi: 10.1017/s0195941700063591. [DOI] [PubMed] [Google Scholar]
- Kumar M. L., Jenson H. B., Dahms B. B. Fatal staphylococcal epidermidis infections in very low-birth-weight infants with cytomegalovirus infection. Pediatrics. 1985 Jul;76(1):110–112. [PubMed] [Google Scholar]
- Munson D. P., Thompson T. R., Johnson D. E., Rhame F. S., VanDrunen N., Ferrieri P. Coagulase-negative staphylococcal septicemia: experience in a newborn intensive care unit. J Pediatr. 1982 Oct;101(4):602–605. doi: 10.1016/s0022-3476(82)80718-x. [DOI] [PubMed] [Google Scholar]
- Noel G. J., Edelson P. J. Staphylococcus epidermidis bacteremia in neonates: further observations and the occurrence of focal infection. Pediatrics. 1984 Nov;74(5):832–837. [PubMed] [Google Scholar]
- Paneth N., Kiely J. L., Wallenstein S., Marcus M., Pakter J., Susser M. Newborn intensive care and neonatal mortality in low-birth-weight infants: a population study. N Engl J Med. 1982 Jul 15;307(3):149–155. doi: 10.1056/NEJM198207153070303. [DOI] [PubMed] [Google Scholar]
- Weinstein M. P., Reller L. B., Murphy J. R., Lichtenstein K. A. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. I. Laboratory and epidemiologic observations. Rev Infect Dis. 1983 Jan-Feb;5(1):35–53. doi: 10.1093/clinids/5.1.35. [DOI] [PubMed] [Google Scholar]


