Abstract
BACKGROUND
Even with anti-hypertensive therapy, it is difficult to maintain optimal systemic blood pressure values in hypertensive patients. Exercise may reduce blood pressure in untreated hypertensive, but its effect when combined with long-term anti-hypertensive therapy remains unclear. Our purpose was to evaluate the acute effects of a single session of aerobic exercise on the blood pressure of long-term-treated hypertensive patients.
METHODS
Fifty treated hypertensive patients (18/32 male/female; 46.5±8.2 years; Body mass index: 27.8±4.7 kg/m2) were monitored for 24 h with respect to ambulatory (A) blood pressure after an aerobic exercise session (post-exercise) and a control period (control) in random order. Aerobic exercise consisted of 40 minutes on a cycle-ergometer, with the mean exercise intensity at 60% of the patient’s reserve heart rate.
RESULTS
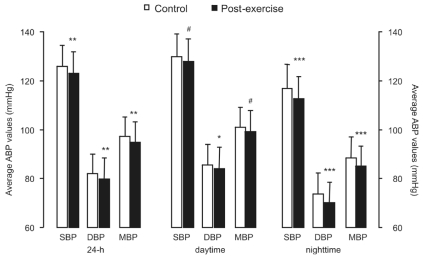
Post-exercise ambulatory blood pressure was reduced for 24 h systolic (126±8.6 vs. 123.1±8.7 mmHg, p=0.004) and diastolic blood pressure (81.9±8 vs. 79.8±8.5 mmHg, p=0.004), daytime diastolic blood pressure (85.5±8.5 vs. 83.9±8.8 mmHg, p=0.04), and nighttime S (116.8±9.9 vs. 112.5±9.2 mmHg, p<0.001) and diastolic blood pressure (73.5±8.8 vs. 70.1±8.4 mmHg, p<0.001). Post-exercise daytime systolic blood pressure also tended to be reduced (129.8±9.3 vs. 127.8±9.4 mmHg, p=0.06). These post-exercise decreases in ambulatory blood pressure increased the percentage of patients displaying normal 24h systolic blood pressure (58% vs. 76%, p=0.007), daytime systolic blood pressure (68% vs. 82%, p=0.02), and nighttime diastolic blood pressure (56% vs. 72%, p=0.02). Nighttime systolic blood pressure also tended to increase (58% vs. 80%, p=0.058).
CONCLUSION
A single bout of aerobic exercise reduced 24h ambulatory blood pressure levels in long-term-treated hypertensive patients and increased the percentage of patients reaching normal ambulatory blood pressure values. These effects suggest that aerobic exercise may have a potential role in blood pressure management of long-term-treated hypertensive.
Keywords: Hypertension, Exercise, Blood Pressure, Treated Hypertension
INTRODUCTION
Systemic arterial hypertension is a highly prevalent disease,1,2 affecting approximately one billion individuals worldwide, and is a major risk factor associated with increased all-cause and cardiovascular mortality.2 Cardiovascular risk is dependent on systemic arterial blood pressure (BP), with optimal values below 120/80 mmHg.2,3 Systemic arterial hypertension treatments include lifestyle modifications and pharmacological interventions.2 However, major pharmacological trials have demonstrated that maintaining BP at normal levels is difficult,4 with only 25 to 62% of patients being properly controlled.4–6
Among lifestyle modifications, physical activity is important because it has been associated with a lower incidence of hypertension in different populations.7–9 Additionally, physical activity reduces the BP of hypertensive and normotensive subjects,10 with greater and longer-lasting reductions observed in subjects with higher BP levels.14 Several studies have shown that just a single set of dynamic exercise can decrease BP to below basal levels in hypertensive subjects and that this hypotensive effect remains for several hours after exercise.11–14 This acute exercise-mediated BP reduction is clinically significant.14 However, post-exercise BP reduction has only been reported in uncontrolled hypertensive patients not taking medication; therefore, it is necessary to investigate whether this effect also occurs in long-term-treated hypertensive patients taking anti-hypertensive medications.
Thus, the goal of the present study was to evaluate the effect of a single bout of aerobic exercise on BP in patients receiving long-term anti-hypertensive treatment.
METHODS
Study Design
All volunteers were selected from the hypertension group at the University Hospital of the University of Sao Paulo. They underwent clinical evaluation and maximal graded exercise testing. Two 24 hour (24 h) ambulatory BP (ABP) monitoring were performed after a session of aerobic exercise (post-exercise) and after a nonexercise control period (control). The local ethics committee approved all procedures. The volunteers read a detailed description of the protocol and provided written informed consent.
Population
Middle-aged hypertensive volunteers receiving treatment for arterial hypertension for 9.4 ± 6.1 years, with office BP < 140/90 mmHg, without changes in drug therapy during the preceding 3 months or limitations on physical activity were recruited. Medical history and clinical evaluation were used to exclude persons with cardiovascular, renal, or pulmonary problems, diabetes, and chronic physical or psychological disorders. The maximal graded exercise test (Bruce protocol)15 was performed to exclude the presence of coronary artery disease and determine the physical exercise workload. Because beta-blockers can greatly limit exercise-induced heart rate increases,16 the maximal exercise test was performed at the same time of day as the exercise session with patients taking their current medication. Subjects participating in regular physical activity (more than once a week) for the last 6 months were also excluded. In all, 104 patients were screened. A total of 50 hypertensive patients (32 women; 21 postmenopausal) were eligible during the screening process and participated in the study. The reasons for ineligibility included uncontrolled office BP (28 patients), changes in drug therapy (5), type 2 diabetes (11 patients), and pre-participation in physical activity programs (10 patients). The demographics and drug regimens of the studied patients are summarized in Table 1. The results of the maximal exercise tests are displayed in Table 2.
Table 1.
Subjects’ characteristics
| Variable | Men | Women
|
Total | |
|---|---|---|---|---|
| Pre-menopause | Post-menopause | |||
| N | 18 | 11 | 22 | 50 |
| Age (years) | 45.8 ± 9.8 | 40.4 ± 3.7 * | 52.3 ± 3.4 | 46.5 ± 8.2 |
| BMI (kg/m2) | 27.8 ± 3.8 | 28.9 ± 6.5 | 26.7 ± 4.2 | 27.8 ± 4.7 |
| Waist circumference (cm) | 91.5 ± 9.6 | 90.7 ± 11.5 | 88.4 ± 11.3 | 90.1 ± 11.3 |
| Office BP (mmHg) | ||||
| Systolic | 133.4 ± 7.2 | 130.5 ± 8.2 | 126.4 ± 10.6 | 129.6 ± 9.2 |
| Diastolic | 86.3 ± 3.1 | 85.1 ± 5.3 | 82.1 ± 8.1 | 85.3 ± 4.2 |
| Medication | ||||
| Diuretic | 72% | 54% | 59% | 62% |
| ACEI | 38% | 27% | 40% | 35% |
| β-blocker | 33% | 45% | 36% | 38% |
| CaCI | 6% | |||
| Mono-therapy | 56% | 63% | 50% | 56% |
| Combination-therapy | 44% | 37% | 50% | 44% |
N: number of patients; F: female; M: male; BMI: body mass index; ACEI: angiotensin-converting enzyme inhibitor; CaCI: calcium channel blocker. Mono-therapy: patients receiving single-drug therapy; Combination-therapy: patients receiving multiple-drug therapy.
: significant different from post-menopause women (p<0.001)
Table 2.
Maximal exercise testing
| Variable | Non-β-blocker | β-blocker |
|---|---|---|
| Exercise time (min) | 7.0 ± 1.9 | 7.7 ± 2. 0 |
| METs | 7.3 ± 1.1 | 7.8 ± 1.3 |
| BP (mmHg) | ||
| Rest | ||
| Systolic | 134.6 ± 12.8 | 140.3 ± 15.2 |
| Diastolic | 91.5 ± 9.8 | 93.3 ± 9.6 |
| Peak | ||
| Systolic | 205.0 ± 25.1 | 214.0 ± 26.7 |
| Diastolic | 102.1 ± 17.2 | 106.7 ± 11.1 |
| Heart Rate (bpm) | ||
| Rest | 72.2 ± 7.7 | 70.7 ± 9.5 |
| Peak | 159.7 ± 16.2 | 160.2 ± 9.0 |
| % predicted | 91.3 ± 8.2 | 91.0 ± 6.1 |
Non-β-blocker: patients do not receiving β-blocker therapy; β-blocker: patients receiving β-blocker therapy. BP: blood pressure.
24-h ambulatory blood pressure monitoring
The 24 h ABP monitoring was performed after an exercise session (post-exercise) and after a nonexercise control period (50 minutes of rest in the sitting position) in random order using a Spacelabs model 90207 ABP monitor (Spacelabs Medical Inc., Redmond, WA). Both control and post-exercise 24-h ABP monitoring began at the same time of day (between 6 and 7 p.m.) and were separated by 2 to 7 days. All recordings were started on a weekday other than Friday.
Subjects were instructed to perform their habitual daily activities, not to engage in formal physical activity, and to relax and straighten the arm during the recording interval for daytime ABP monitoring. Subjects were also asked to document their hours of sleep, time at work, time at leisure activities, and time of medication. The monitor was programmed to measure BP every 15 minutes during the daytime and every 20 minutes during nighttime periods. The daytime and nighttime periods were based on the time patients got into and out of bed.
Individual BP measurements were reviewed for missing and erroneous values. Readings were purged if data were missing, systolic BP was lower than diastolic BP, systolic BP was >240 mmHg or <50 mmHg, or diastolic BP was >140 mmHg or <40 mmHg. System-tagged data were purged if systolic BP deviated by more than ± 50 mmHg or diastolic BP deviated by more than ± 20 mmHg from surrounding values. An average of 89.2±3.1 measurements was taken during each ABP monitoring session; 87.8±9.5% of measurements were then analyzed.
For analysis, 24-h ABP monitoring data were classified by 24-h, daytime, and nighttime periods for systolic, diastolic, and mean BP.
Exercise
The exercise session took place in the evening (5 to 6 p.m.) and consisted of 40 minutes of aerobic exercise on a cycle-ergometer and 5 minutes of warm-up and cool-down. Exercise intensity was determined according to the workload reached during the maximal graded exercise test and was set at 60% of the reserve heart rate. The reserve heart rate was calculated by taking the difference between the peak and resting heart rates, then multiplying this number by the intensity of exercise, and adding it to the resting heart rate, according to the Karvonen method.17 Peak and resting heart rates were obtained through the graded exercise test. Heart rates were monitored during all exercise sessions using a heart rate monitor (Polar Beat, Polar Electro Inc., Finland).
Statistical methods
ANOVA was used to compare subject demographics between men and pre- and post-menopause women. Paired t-test was used to compare ABP monitoring data. Wilcoxon signed rank test was used to compare the percentage of patients with normal ABP monitoring data between control and post-exercise ABP measurements (24 h BP < 130/80 mmHg, daytime BP < 135/85 mmHg, and nighttime BP < 120/70 mmHg).18 Data are presented as the mean ± standard deviation. The level of significance was set at p ≤ 0.05. SPSS 13.0 software was used to perform statistical analyses.
RESULTS
Because there were more women than men and more post- than pre-menopause women, we first compared the results based on sex and menopause status. However, ANOVA did not detect any effects of sex and menopause status for any measure. Thus, the results were not grouped by sex or menopause status.
Despite the fact that all patients were receiving antihypertensive therapy and office BP was < 140/90mm Hg, only 14 patients showed normal control ABP levels for all reading periods. The prevalence of masked hypertension (office BP < 140/90 mmHg but daytime ABP ≥ 135/85 mmHg)18 was 52% and similar to the 48% observed for high nighttime ABP levels (Table 3).
Table 3.
Prevalence of normal ambulatory blood pressure
| Reading period | N | Percentage |
|---|---|---|
| 24-hour | 16 | 32 % |
| Daytime | 24 | 48 % |
| Nighttime | 26 | 52 % |
| All Periods | 14 | 28 % |
Normal ABP: < 130/80 mmHg for 24-h; < 135/85 mmHg for daytime; and < 120/70 for nighttime.
Exercise was beneficial to ABP, as seen in Figure 1. Statically significant post-exercise decreases were observed in systolic, diastolic, and mean 24-h ABP; diastolic daytime ABP; and systolic, diastolic, and mean nighttime ABP. Post-exercise systolic and mean daytime ABP tended to decrease (p=0.06).
Figure 1.
Average twenty-four hour (24 h), daytime, and nighttime ABP values after a single exercise session (post-exercise) or a nonexercise control period (control). SBP: systolic BP; DBP: diastolic BP; MBP: mean BP. Asterisks denote a significant difference from control period (*p=0.04; **p≤0.004; ***p≤0.0001). #Tended to be different from control period (p=0.06)
Figure 2 shows that decreases in post-exercise ABP increased the prevalence of normal 24 h and daytime systolic ABP, as well as diastolic nighttime ABP. The prevalence of normal post-exercise 24h and daytime diastolic ABP did not increase significantly, but post-exercise systolic nighttime ABP tended to increase (p=0.058). These post-exercise BP improvements resulted in a decrease in the prevalence of masked hypertension from 52% (control) to 28% (post-exercise).
Figure 2.
Percentage of patients with twenty-four hour (24 h), daytime, and nighttime normal (< 130/80 mmHg for 24-h, < 135/85 mmHg for daytime, and < 120/70 for nighttime) ABP after a single exercise session (post-exercise) or a nonexercise control period (control.). A: systolic blood pressure; B: diastolic blood pressure. Asterisks denote a significant difference from control period (*p=0.02; **p=0.007). #Tended to be different from control period (p=0.058)
Because the effect of exercise on postexercise ABP reduction is related to the basal BP level,14 we also separately analyzed the effect of exercise on subjects with higher and lower control ABP levels by subdividing them into groups with control ABP above and below the median values (see Table 4). Aerobic exercise only reduced ABP (by 2.6–7.1 mmHg) in the subjects with higher control ABP levels (Figure 3).
Table 4.
Median blood pressure values.
| SBP | DBP | |
|---|---|---|
| 24-hour | 127.5 | 81.5 |
| Daytime | 132.0 | 84.5 |
| Nighttime | 116.5 | 73.5 |
SBP: systolic blood pressure; DMP: diastolic blood pressure; MBP: mean blood pressure.
Figure 3.
Average twenty-four hour (24-h), daytime and nighttime ABP values after a single exercise session (post-exercise) or a nonexercise control period (control) for patients with control BP above (A) and below (B) the median value. SBP: systolic BP. DBP: diastolic BP. Asterisks denote a significant difference from control period (*: p<0.05; **: p=0.001; ***: p≤0.0001)
DISCUSSION
Exercise has been shown to markedly improve the function of a number of cardiopulmonary parameters19–21 and aerobic power.22 The primary finding of this research is that a single session of aerobic exercise reduced systolic, diastolic, and mean ABP in sedentary middle-aged long-term-treated hypertensive patients for a substantial portion of the subsequent 24 h period. This decrease resulted in an increased percentage of patients with normal ABP levels. To the best of our knowledge, this is the first study to evaluate the effects of a single bout of aerobic exercise on ABP in long-term-treated hypertensive patients who did not have a washout period before the start of the study.
Post-exercise BP reduction occurs in normotensive and untreated hypertensive, young, middle-aged, and older men and women.12–14,23 However, when BP is measured by ABP monitoring, post-exercise ABP reduction is only significant in untreated hypertensive and prehypertensive subjects; normotensive subjects showed no difference.12,14,24 The present observations that only subjects with higher control ABP levels showed substantial decreases of systolic, diastolic, and mean ABP are consistent with these previous findings; however, the basal BP levels of treated hypertensive patients in this study were lower than the BP levels of untreated hypertensive in previous studies.11–13,25
The average ABP reduction observed after exercise was similar to the post-exercise ABP reduction described in several other studies13,25 but greater than that observed in other studies where no ABP reduction was found.11,26 These discrepancies may be caused by different intensities of the exercise performed. In studies where no post-exercise ABP reductions were found, exercise was of either low18 or maximal intensity.26 Low-intensity aerobic exercise yields smaller and shorter-lasting ABP reductions than moderate-intensity aerobic exercise.24 It is thus possible that low-intensity aerobic exercise is not sufficient to sustain post-exercise ABP reduction long enough to be detected by ABP monitoring. On the other hand, maximal exercise results in markedly different hemodynamic, hormonal, and neural responses than submaximal exercise; therefore, it is possible that a lack of sustained ABP reduction after maximal exercise26 may be the result of the exercise intensity.
Although the population we studied consisted of hypertensive patients who were responsive to pharmacological treatment (office BP < 140/90 mmHg), there was a high prevalence of masked hypertension (52%). Because the prevalence of masked hypertension in treated hypertensive patients has been shown to range from 7 to 20%,18,27 the hypertension treatments in the present study could be interpreted as ineffective. However, when only hypertensive patients responsive to treatment are analyzed, the prevalence of masked hypertension has been shown to range from 27 to 55%,28 similar to the 52% observed in the present study.
In the present study, the percentage of subjects with normal ABP levels increased for all measurement periods after exercise. With this increase, 72% and 68% of patients reached normal daytime and nighttime normal ABP levels, respectively; this improvement represents a masked hypertension prevalence of 28% after exercise. These results show that aerobic exercise could facilitate antihypertensive treatment and, thus, improve patient prognoses.
Another important point of our study is the interval period between experimental protocols (exercise vs. nonexercise). Because this interval varied from 2 to 7 days, one could argue that patients who exercised first and then underwent the nonexercise session after 48 hours may still showing post-exercise effects during nonexercise 24 h ABP monitoring. However, previous studies have shown that although post-exercise hypotension may persist for up to 22 hours after exercise bout, it is usually not observed beyond the first 12 h.14 Nonexercise measurements of patients who exercised first and then underwent the nonexercise session after 48 hours were therefore probably unaffected by earlier exercise session.
The exact mechanism for the post-exercise hypertension observed in the present study remains unclear but is most likely multifactorial. Acute decreases in BP by physical exercise may be related to reduced peripheral resistance rather than cardiac output, with the exception of older hypertensive subjects. Two mechanisms have been proposed to explain this decrease in peripheral resistance: sympathetic inhibition and altered vascular responsiveness after exercise.14 Reduced sympathetic outflow after exercise has been reported in humans,29,30 but the mechanisms are unclear. Resetting the operating point of the arterial baroreflex to lower BP,30 augmented GABAA signaling in the rostral ventrolateral medulla,31 and substance P receptors32 in the nucleus tractus solitarius as well as central vasopressin V1 receptors33 have all been shown to contribute to reduced sympathetic outflow after exercise session and, thus, may have contributed to the acute post-exercise BP reduction observed in the present study. Blunted vascular responsiveness to α-adrenergic stimulation,30,34 as well as increased local release of nitric oxide, prostaglandins, adenosine, and ATP,30,35 are also factors associated with changes in vascular responsiveness after acute exercise and may have also contributed to the post-exercise BP reduction observed in this study.
The main limitation of our study is that, although their BP levels were controlled by drug therapy, the subjects were using different quantities and qualities of medication; it is unknown whether different drugs may have influenced the post-exercise ABP reduction. Another limitation is that the exercise test was performed on a motor treadmill, while the exercise session was performed on a cycle-ergometer, as it has been shown that the heart rate response to treadmill exercise testing in sedentary subjects is 10–15% greater than the heart rate response to cycle-ergometer exercise testing.36 Thus, we calculated 60% of the reserve heart rate on the treadmill and subtracted 10% to adjust it to the cycle-ergometer.
In summary, a single aerobic exercise session reduced ambulatory blood pressure in long-term-treated hypertensive patients and increased the percentage of subjects with normal ambulatory blood pressure levels. These effects suggest that aerobic exercise may be an important tool for blood pressure management of long-term-treated hypertension patients.
ACKNOWLEDGEMENT
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP # 2002/06923-9).
REFERENCES
- 1.Guimarães AC. Hypertension in Brazil. J Hum Hypertens. 2002;16(Suppl 1):S7–S10. doi: 10.1038/sj.jhh.1001332. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of High-Normal Blood Pressure on the Risk of Cardiovascular Disease. N Engl J Med. 2001;345:1291–97. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 4.Zanchetti A, Waeber B. Hypertension: which aspects of hypertension should we impact on and how? J Hypertens. 2006;24(Suppl 5):S2–S5. doi: 10.1097/01.hjh.0000240039.97472.f1. [DOI] [PubMed] [Google Scholar]
- 5.Julius S, Kjeldsen SE, Weber M for the VALUE trial group. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomized trial. Lancet. 2004;363:2022–31. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- 6.Niiranen TJ, Kantola IM, Vesalainen R, Johanson J, Ruuska MJ. A comparison of home measurement and ambulatory monitoring of blood pressure in the adjustment of antihypertensive treatment. Am J Hypertens. 2006;19:468–74. doi: 10.1016/j.amjhyper.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 7.Paffenbarger RS, Jr, Jung DL, Leun RW, Hyde RT. Physical activity and hypertension: an epidemiological view. Ann Med. 1991;23:319–27. doi: 10.3109/07853899109148067. [DOI] [PubMed] [Google Scholar]
- 8.Haapanen N, Miilunpalo S, Vuori I, Oja P, Pasanen M. Association of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in middle-aged men women. Int J Epidemiol. 1997;26:739–47. doi: 10.1093/ije/26.4.739. [DOI] [PubMed] [Google Scholar]
- 9.Hayashi T, Tsumura K, Suematsu C, Okada K, Fujii S, Endo G. Walking to work and the risk for hypertension in men: the Osaka Health Survey. Ann Intern Med. 1999;130:21–6. doi: 10.7326/0003-4819-131-1-199907060-00005. [DOI] [PubMed] [Google Scholar]
- 10.Whelton SP, Chin A, Xin X, He J. Effects of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 11.Wallace JP, Bogle PG, King BA, Krasnoff JB, Jastremski CA. A comparison of 24-h average blood pressures and blood pressure load following exercise. Am J Hypertens. 1997;10:728–34. doi: 10.1016/s0895-7061(97)00070-8. [DOI] [PubMed] [Google Scholar]
- 12.Pescatello LS, Miller BMA, Danias PG, Werner M, Hess M, Baker C, et al. Dynamic exercise normalizes resting blood pressure in mildly hypertensive premenopausal women. Am Heart J. 1999;138:916–21. doi: 10.1016/s0002-8703(99)70017-7. [DOI] [PubMed] [Google Scholar]
- 13.Taylor-Tolbert NS, Dengel DR, Brown MD, McCole SD, Pratley RE, Ferrell RE, et al. Ambulatory blood pressure after acute exercise in older men with essential hypertension. Am J Hypertens. 2001;13:44–51. doi: 10.1016/s0895-7061(99)00141-7. [DOI] [PubMed] [Google Scholar]
- 14.American College of Sports Medicine. Position Stand: Exercise and Hypertension. Med Sci Sports Exerc. 2004;36:533–53. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 15.Bruce RA. Exercise testing of patients with coronary heart disease. Principles and normal standards for evaluation. Ann Clin Res. 1971;3:323–32. [PubMed] [Google Scholar]
- 16.Ades PA, Woelfel EE, Hiatt WR, Fee C, Rolfs R, Brammell HL, et al. Exercise hemodynamic effects of beta-blockade and intrinsic sympathomimetic activity. Eur J Clin Pharmacol. 1989;36:5–10. doi: 10.1007/BF00561015. [DOI] [PubMed] [Google Scholar]
- 17.Karvonen M, Kentala K, Mustala O. The effects of training on heart rate: a longitudinal study. Ann Med Exper Biol Fenn. 1957;35:307–15. [PubMed] [Google Scholar]
- 18.Alessi A, Brandão AA, Pierin A, Feitosa AM, Machado CA, de Moraes, et al. IV Guideline for Ambulatory Blood Pressure Monitoring - II Guideline for Home Blood Pressure Monitoring. Arq Bras Cardiol. 2005;85 (suppl 2):1–18. doi: 10.1590/S0066-782X2005002100001. [DOI] [PubMed] [Google Scholar]
- 19.Guimarães GV, Carvalho VO, Bocchi EA. Reproducibility of the self-controlled six-minute walking test in heart failure patients. Clinics. 2008;63:201–6. doi: 10.1590/s1807-59322008000200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bocalini DS, dos Santos L, Serra AJ. Physical exercise improves the functional capacity and quality of life in patients with heart failure. Clinics. 2008;63:437–42. doi: 10.1590/S1807-59322008000400005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carvalho VO, Guimarães GV, Ciolac EG, Bocchi EA. Heart rate dynamics during a treadmill cardiopulmonary exercise test in optimized beta-blocked heart failure patients. Clinics. 2008;63:479–82. doi: 10.1590/S1807-59322008000400011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Santos-Silva PR, Fonseca AJ, Castro AW, Greve JM, Hernandez AJ. Reproducibility of maximum aerobic power (VO2max) among soccer players using a modified heck protocol. Clinics. 2007;62:391–6. doi: 10.1590/s1807-59322007000400004. [DOI] [PubMed] [Google Scholar]
- 23.MacDonald JR, MacDougall JD, Hogben CD. The effects of exercise duration on post-exercise hypotension. J Hum Hypertens. 2000;14:125–9. doi: 10.1038/sj.jhh.1000953. [DOI] [PubMed] [Google Scholar]
- 24.Quinn TJ. Twenty-four hour, ambulatory blood pressure responses following acute exercise: impact of exercise intensity. J Hum Hypertens. 2000;14:547–53. doi: 10.1038/sj.jhh.1001106. [DOI] [PubMed] [Google Scholar]
- 25.Park S, Jastremski CA, Wallace JP. Time of day for exercise on blood pressure reduction in dipping and nondipping hypertension. J Hum Hypertens. 2005;19:597–605. doi: 10.1038/sj.jhh.1001901. [DOI] [PubMed] [Google Scholar]
- 26.Somers VK, Conway J, Coats A, Isea J, Sleight P. Postexercise hypotension is not sustained in normal and hypertensive subjects. Hypertension. 1991;18:211–5. doi: 10.1161/01.hyp.18.2.211. [DOI] [PubMed] [Google Scholar]
- 27.Pierdomenico SD. The odyssey of masked hypertension in the HOMERUS trial. Am J Hypertens. 2007;20:1266–7. doi: 10.1016/j.amjhyper.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Pierdomenico SD, Cuccurullo F, Mezzetti A. Masked hypertension in treated hypertensive patients. Am J Hypertens. 2006;19:873–4. doi: 10.1016/j.amjhyper.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 29.Floras JS, Sinkey CA, Aylard PE, Seals DR, Thoren PN, Mark AL. Postexercise hypotension and sympathoinhibition in borderline hypertensive men. Hypertens. 1989;14:28–35. doi: 10.1161/01.hyp.14.1.28. [DOI] [PubMed] [Google Scholar]
- 30.Halliwill JR, Taylor JA, Eckberg DL. Impaired sympathetic vascular regulation in humans after acute dynamic exercise. J Physiol. 1996;495:279–88. doi: 10.1113/jphysiol.1996.sp021592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kajekar R, Chen CY, Mutoh T, Bonham AC. Gaba(a) receptor activation at medullary sympathetic neurons contributes to postexercise hypotension. Am J Physiol Heart Circ Physiol. 2002;282:H1615–24. doi: 10.1152/ajpheart.00725.2001. [DOI] [PubMed] [Google Scholar]
- 32.Chen CY, Munch PA, Quail AW, Bonham AC. Postexercise hypotension in conscious SHR is attenuated by blockade of substance P receptors in NTS. Am J Physiol Heart Circ Physiol. 2002;283:H1856–62. doi: 10.1152/ajpheart.00827.2001. [DOI] [PubMed] [Google Scholar]
- 33.Collins HL, Rodenbaugh DW, Dicarlo SE. Central blockade of vasopressin V(1) receptors attenuates postexercise hypotension. Am J Physiol Regul Integr Comp Physiol. 2001;281:R375–80. doi: 10.1152/ajpregu.2001.281.2.R375. [DOI] [PubMed] [Google Scholar]
- 34.Patil RD, Dicarlo SE, Collins HL. Acute exercise enhances nitric oxide modulation of vascular response to phenylephrine. Am J Physiol. 1993;265:H1184–8. doi: 10.1152/ajpheart.1993.265.4.H1184. [DOI] [PubMed] [Google Scholar]
- 35.Rao SP, Collins HL, Dicarlo SE. Postexercise alpha-adrenergic receptor hyporesponsiveness in hypertensive rats is due to nitric oxide. Am J Physiol Regul Integr Comp Physiol. 2002;282:R960–8. doi: 10.1152/ajpregu.00490.2001. [DOI] [PubMed] [Google Scholar]
- 36.Bunc V, Heller J. Exercise intensity conversion from a bicycle ergometer to a treadmill. J Sports Med Phys Fitness. 1991;31:490–3. [PubMed] [Google Scholar]