Abstract
PURPOSE
Compare the effect of conventional static stretching and muscle chain stretching, as proposed by the global posture reeducation method, in the manual therapy of patients with chronic neck pain.
METHODS
Thirty-three female patients aged 35 to 60 years old, 31 of whom completed the program, were randomly divided into two groups: The global posture reeducation group (n=15) performed muscle chain stretching, while the conventional stretching group (n=16) performed conventional static muscle stretching. Both groups also underwent manual therapy. Patients were evaluated before and after treatment and at a six-week follow-up appointment and tested for pain intensity (by means of visual analog scale), range of motion (by goniometry), and health-related quality of life (by the SF-36 questionnaire). The treatment program consisted of two 1-hour individual sessions per week for six weeks. Data were statistically analyzed at a significance level of p<0.05.
RESULTS
Significant pain relief and range of motion improvement were observed after treatment in both groups, with a slight reduction at follow-up time. Quality of life also improved after treatment, except for the global posture reeducation group in one domain; at follow-up, there was improvement in all domains, except that both groups reported increased pain. There were no significant differences between groups
CONCLUSION
Conventional stretching and muscle chain stretching in association with manual therapy were equally effective in reducing pain and improving the range of motion and quality of life of female patients with chronic neck pain, both immediately after treatment and at a six-week follow-up, suggesting that stretching exercises should be prescribed to chronic neck pain patients.
Keywords: Muscle stretching exercises, Neck pain, Physical therapy
INTRODUCTION
Pain is an “unpleasant sensory and emotional experience associated with actual or potential tissue damage.”1 In chronic pain, the sensorial process becomes abnormal, leading to detectable changes in central nervous system data processing, motor control, and the experience of pain itself.2 Pain may lead a person to stop working or exercising.3
Chronic neck pain is a sensation of hyperalgia to skin palpation, ligaments, and muscles during both active and passive movement.4 Mechanical neck pain has been described as having no detectable or specific etiology (such as inflammation or infection), and it may be reproduced by provocative stimuli. It is usually located at the lower neck region between the occipital region and the first thoracic vertebra.5
Neck pain is most common among women in their 50s, with innumerable consequences.6 Its prevalence among women has been shown in some countries, but no studies could be found on neck pain prevalence in Brazil.
Hanten et al.7 and Lee et al.8 observed that neck pain causes range of motion (RoM) reduction, which may be linked to mechanical restriction between two or more vertebrae. According to Barnsley,9 such restriction may be caused by pain, fiber contracture, bone ankylosis, or muscle spasm. A patient with neck pain may also present a posture imbalance resulting from shortening and increased activation of suboccipital, sternocleidomastoid, upper trapezius, pectoralis, and rotator cuff muscles.10
Physical therapies for treating chronic pain include different exercises. Conventional physical therapy uses static muscle stretching, which consists of stretching a muscle up to a tolerable point and sustaining the position for a certain period of time. In Brazil, France, Italy, and Spain, therapists are increasingly resorting to a method called global posture reeducation (GPR),11 which focuses on entire muscle groups instead of targeting individual muscles. Based on the existence of muscle chains – didactically divided into posterior and anterior chains12 – this method proposes global stretching of antigravity muscles. While static stretching of a single muscle or a small group of muscles usually lasts 30 seconds,13 in GPR, all muscles of the same chain are simultaneously stretched during a 15 minute posture, avoiding compensations. Bertherat14 reported Meziere’s attempts to decrease spinal curvature, observed that a different muscle had been stressed, and finally concluded that the cause of deformation was a shortening of the posterior muscle chain brought about by everyday activities.
Besides muscle stretching, manual therapy has been used as a form of preparation to ease stretching. Therein, patients subjected to protocols of both manual therapy and stretching have exhibited higher satisfaction levels and better performances when compared to those who underwent only manual therapy.10
Several Brazilian physical therapists have been using the GPR method with satisfactory empiric results. Although the method is often clinically practiced, few studies show its efficacy, and no studies were found on its use in neck pain. In view of the high incidence of neck pain and its consequences, especially in women, the purpose of the present study was to compare the effects of two kinds of stretching, GPR and static conventional stretching, and their association with manual therapy in relieving pain and improving RoM and health-related quality of life in female patients with chronic neck pain.
SUBJECTS AND METHODS
Thirty-three women, ranging in age from 35 to 60 years old, were initially selected, while 31 completed the study. Subjects were recruited from a list supplied by the Outpatient Orthopedics and Rheumatology Clinic of the Londrina State University Hospital and randomly distributed into two groups, using a random numbers table. The GPR group (n=15) performed muscle stretching according to the technique of global posture reeducation, and the static stretching group (n=16) performed conventional static muscle stretching. During the study, two subjects halted treatment for professional reasons.
The study was approved by the ethics commission for the analysis of research projects of Hospital das Clínicas of the São Paulo University Medical School (SP, Brazil). All subjects were instructed on the purpose of the study and provided written consent.
Participants were selected according to the following criteria: diagnosis of primary mechanical, either myogenous or arthrogenous, neck pain and pain lasting for over 12 weeks. Subjects with a neurologic deficit in their upper limbs, such as hypertonia, hypotonia, hyporeflexia, absence of reflex, and vertebral instability, or with a previous history of spine surgery or whiplash were excluded. All patients had been previously diagnosed by experienced staff at the Orthopedics and Rheumatology Clinic. In many cases, X-rays were used for diagnosis. Patients were selected for this study by reading through medical records to evaluate who met the inclusion criteria.
The required sample size was calculated using an 80% statistical power to detect a 30% difference in the intervention group. An N≤5% and a confidence interval of 95% were considered significant.
Procedures
All the procedures (assessment and treatment) were performed by a trained researcher at the physical therapy clinic. Pain intensity was evaluated by means of a visual analog scale (VAS) ranging from 0 cm to 10 cm, wherein the patient marked a point according to her level of pain; a higher score corresponded to more intense pain.
Cervical spine range of motion was measured using a goniometer and always conducted in the same order: flexion, extension, lateral flexion, and rotation, with the subject sitting with her head and trunk held erect. The universal goniometer is an instrument frequently used to quantify restrictions in range of motion15. Physical therapists use the RoM measurement to quantify limitations at the beginning of treatment and to quantify the effectiveness of interventions.16
Health-related quality of life was assessed by applying the Medical Outcome Study Short-Form 36 Health Survey (SF-36) translated and validated into Portuguese;17 its 36 questions are grouped into eight domains: physical functioning, physical component of pain, bodily pain, general health, vitality, social functioning, emotional component of pain, mental health, and an open-ended item comparing current health to that one year earlier. For each category, scores ranged from 0 to 100, wherein a higher value indicated a better quality of life.
All evaluations were made before, immediately after, and at a follow-up six weeks after treatment.
Treatment protocol
Patients attended two weekly physical therapy sessions during a six-week period. At each 60 minute individual session, the patient received manual therapy for 30 minutes and stretched for another 30 minutes. At the beginning of the session, with the patient lying down on her back and all limbs relaxed, pompage maneuvers were performed as described by Bienfait,18 in association with breathing exercises, in order to stretch the fasciae that connect the shoulder and cervical spine muscles. Each maneuver was repeated three times and maintained during five breaths.
After manual therapy maneuvers, patients performed muscle stretching according to the group to which they had been assigned:
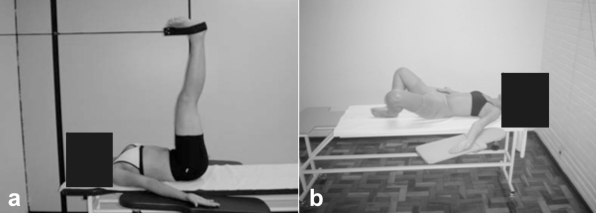
GPR group: Stretched muscle chains as described by Marques,12 keeping two stretching postures for 15 minutes each. In order to stretch the posterior muscle chain (upper trapezius, levator scapulae, suboccipitalis, erector spinae, gluteus maximus, ischiotibials, triceps surae, and foot intrinsic muscles), the patient lay in the supine position with the occipital, lumbar, and sacral spine stabilized, with the lower limbs at 90° hip flexion, and performed gradual knee extensions (Figure 1A). In order to stretch the anterior muscle chain (diaphragm, pectoralis minor, scalene, sternocleidomastoid, inter-costalis, iliopsoas, arm, forearm, and hand flexors), the patient lay in the supine position with the upper limbs abducted at 30° and the forearms supine. The pelvis was kept in retroversion, while the lumbar spine remained stabilized. Hips were flexed, abducted, and laterally rotated, with the soles of the feet touching each other. Gradually, respecting the patient’s limits, the lower limbs were extended as much as possible while maintaining the tibiotarsal angle at 90°(Figure 1b).
Conventional stretching group: performed stretching of upper trapezius, suboccipitalis and back of the neck, pectoralis major and minor, rhomboids, finger and wrist flexors, forearm pronators, finger and wrist extensors, forearm supinators, and paravertebral muscles.19 Each exercise was auto-passively repeated twice for 30 seconds and done slowly at normal breathing rhythm and with no compensations allowed. The total stretching time was equivalent to that of the GPR group.
Figure 1.
Global posture reeducation stretching positions: a) posterior muscle chain stretching; b) anterior muscle chain stretching
Statistics
Evaluation results are expressed as means and standard deviations. Data normality was verified by the Shapiro-Wilk W test. Intragroup analysis was performed by the paired t test for parametric variables, and the Wilcoxon test was performed for non-parametric variables. For comparative analysis between groups, parametric variables were assessed by the t test, while non-parametric variables were analyzed using the Mann-Whitney test. The significance level was set at α<0.05.
RESULTS
Patients’ characteristics are summarized in Table 1. No significant differences were observed between the groups in either the anthropometric or clinical data (p>0.05).
Table 1.
Patients’ clinical and demographic data, according to group
| Features | GPR group (n=15) | Conventional stretching group (n=16) |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Age (years) | 44.4 (7.8) | 48.7 (7.3) |
| Weight (Kg) | 62.5 (7.1) | 65.8 (8.3) |
| Height (cm) | 158.5 (6.4) | 157.6 (5.8) |
| Pain location | n (%) | n (%) |
| Neck posterior region | 15 (100) | 16 (100) |
| Shoulders | 11 (73.3) | 7 (43.7) |
| Upperlimbs | 10 (66.6) | 7 (43.7) |
| Medication used | n (%) | n (%) |
| None | 1 (6.7) | 3 (18.8) |
| Antiinflammatory | 9 (60) | 8 (50) |
| Analgesics | 6 (40) | 8 (50) |
| Anti-depressive | 3 (20) | 2 (12.5) |
| Muscle relaxer | 6 (40) | 2 (12.5) |
| Medication frequency | n (%) | n (%) |
| Frequent | 14 (93.3) | 13 (81,2) |
| No use | 1(6,6) | 3 (18,8) |
| Physical activity | n (%) | n (%) |
| Sedentary | 11 (73.3) | 11 (68.8) |
| Active | 4 (26.7) | 5 (31.2) |
| Profession | n (%) | n (%) |
| Housewife | 7 (46.6) | 8 (50) |
| Administrative | 4 (26.7) | 4 (25) |
| Liberal and technical | 4 (26.7) | 4 (25) |
Statistically significant pain relief (as measured by VAS) and RoM improvement were found in both groups between pre- and post-treatment evaluations; a slight loss was detected in both groups at follow-up (Table 2).
Table 2.
Pain and range of motion (RoM) mean values of both groups at pre- and post-treatment evaluations and at follow-up, and p values for the comparisons pre X post, pre X follow-up, and post X follow-up
| GPR group (n=15) | Conventional stretching group (n=16) | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-treat | Post-treat | Follow-up | p | Pre-treat | Post-treat | Follow-up | p | |
| Pain (VAS cm) | 6,6 | 2 | - | 0,000* | 7,2 | 1,6 | - | 0,000* |
| 6,6 | - | 3,2 | 0,003* | 7,2 | - | 2,7 | 0,000* | |
| - | 2 | 3,2 | 0,100 | - | 1,6 | 2,7 | 0,124 | |
| RoM (°) | ||||||||
| Flexion (0–5)** | 48 | 58,5 | - | 0,000* | 51,0 | 60,5 | - | 0,000* |
| 48 | - | 56,5 | 0,000* | 51,0 | - | 59,5 | 0,000* | |
| - | 58,5 | 56,5 | 0,041* | - | 60,5 | 59,5 | 0,142 | |
| Extension (0–0)** | 43 | 48,0 | - | 0,000* | 44,0 | 47,5 | - | 0,001* |
| 43 | - | 46,5 | 0,001* | 44,0 | - | 47,0 | 0,000* | |
| - | 48,0 | 46,5 | 0,054 | - | 47,5 | 47,0 | 0,441 | |
| Right bending (0–0)** | 34,5 | 38,0 | - | 0,001* | 33,0 | 39,5 | - | 0,000* |
| 34,5 | - | 36,5 | 0,013* | 33,0 | - | 38,5 | 0,001* | |
| - | 38,0 | 36,5 | 0,102 | - | 39,5 | 38,5 | 0,133 | |
| Left bending (0–0)** | 33,0 | 36,5 | - | 0,000* | 33,0 | 38,5 | - | 0,000* |
| 33,0 | - | 36,0 | 0,003* | 33,0 | - | 38,0 | 0,000* | |
| - | 36,5 | 36,0 | 0,388 | - | 38,5 | 38,0 | 0,533 | |
| Rotation to right (0–5)** | 45,5 | 50,5 | - | <0,001* | 46,5 | 50,5 | - | <0,001* |
| 45,5 | - | 50,0 | <0,001* | 46,5 | - | 50,0 | <0,001* | |
| - | 50,5 | 50,0 | 0,273 | - | 50,5 | 50,0 | 0,465 | |
| Rotation to left (0–5)** | 44,0 | 49,0 | - | 0,000* | 45,5 | 49,5 | - | 0,000* |
| 44,0 | - | 48,5 | 0,001* | 45,5 | - | 49,0 | 0,001* | |
| - | 49,0 | 48,5 | 0,123 | - | 49,5 | 49,0 | 0,694 | |
statistically significant difference; pre-treat = before treatment; post-treat = immediately after treatment;
Normal range
Concerning health-related quality of life, improvement was observed after treatment, except for the GPR group in the general health domain. At follow-up, both groups reported more pain than immediately after treatment and improvements in all other domains, although not statistically significant (Table 3). No significant differences could be observed between groups (p>0.05).
Table 3.
SF-36 mean scores of both groups at pre- and post-treatment evaluations and at follow-up, and p values for the comparisons pre X post, pre X follow-up, and post X follow-up
| SF-36 domain | GPR group (n=15) | Conventional stretching group (n=16) | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-treat | Post-treat | Follow-up | p | Pre-treat | Post-treat | Follow-up | P | |
| Physical functioning | 61,7 | 73 | - | 0,025* | 56,6 | 74,1 | - | 0,003* |
| 61,7 | - | 80,3 | 0,001* | 56,6 | - | 79,1 | 0,001* | |
| - | 73 | 80,3 | 0,032* | - | 74,1 | 79,1 | 0,162 | |
| Role-physical | 41,7 | 78,3 | - | 0,020* | 17,2 | 71,9 | - | 0,001* |
| 41,7 | - | 80 | 0,006* | 17,2 | - | 81,2 | 0,000* | |
| - | 78,3 | 80 | 0,892 | - | 71,9 | 81,2 | 0,398 | |
| Bodily pain | 30,3 | 68,3 | - | 0,001* | 34,6 | 67,1 | - | 0,000* |
| 30,3 | - | 64,3 | 0,001* | 34,6 | - | 64,7 | 0,000* | |
| - | 68,3 | 64,3 | 0,346 | - | 67,1 | 64,7 | 0,556 | |
| General health | 66,1 | 71,7 | - | 0,152 | 65,9 | 80,5 | - | 0,007* |
| 66,1 | - | 77,7 | 0,023* | 65,9 | - | 83,9 | 0,000* | |
| - | 71,7 | 77,7 | 0,107 | - | 80,5 | 83,9 | 0,091 | |
| Vitality | 40,7 | 56,7 | - | 0,010* | 43,8 | 66,9 | - | 0,001* |
| 40,7 | - | 61,3 | 0,001* | 43,8 | - | 66,9 | 0,004* | |
| - | 56,7 | 61,3 | 0,444 | - | 66,9 | 66,9 | 0,859 | |
| Social function | 51,7 | 70,8 | - | 0,032* | 57,8 | 82,8 | - | 0,003* |
| 51,7 | - | 80 | 0,011* | 57,8 | - | 83,6 | 0,002* | |
| - | 70,8 | 80 | 0,115 | - | 82,8 | 83,6 | 0,833 | |
| Role- emotional | 57,8 | 80 | - | 0,015* | 41,7 | 75 | - | 0,018* |
| 57,8 | - | 84,4 | 0,006* | 41,7 | - | 83,3 | 0,009* | |
| - | 80 | 84,4 | 0,612 | - | 75 | 83,3 | 0,345 | |
| Mental health | 53,9 | 64,3 | - | 0,050* | 54,5 | 66,3 | - | 0,035* |
| 53,9 | - | 66,1 | 0,030* | 54,5 | - | 66,3 | 0,046* | |
| - | 64,3 | 66,1 | 0,875 | - | 66,3 | 66,3 | 0,888 | |
statistically significant difference; pre-treat = before treatment; post-treat = immediately after treatment
DISCUSSION
The present results indicate that both muscle chain stretching and conventional static stretching, in association with manual therapy, were equally effective in reducing pain and improving range of motion and quality of life of patients with chronic neck pain, with no significant differences between groups. Furthermore, six weeks after treatment, practically all gains were maintained.
Both groups exhibited RoM improvement, especially in the flexion range, which increased by approximately 10° in both groups. Since the normal range is 65°, it may be said that subjects were close to normal flexion after therapy (Table 2). In other movements, the RoM increased less dramatically. The impact of stretching on flexibility improvements has been widely investigated.20 The increased range of motion is associated with flexibility gains, which, in turn, are linked to pain tolerance, muscle-tendon viscoelastic properties,21,22 and an increased number of sarcomeres in series.23,24
Pain intensity scores, as measured by VAS, were also lower both at the end of treatment and at follow-up. Bronfort et al,25 among others, have shown positive results in associating exercises with manual therapy for relieving pain. Some studies have shown that massage, mobilization, and exercises were more effective than electrotherapy, thermotherapy, or cryotherapy in reducing pain and improving functional capacity.26,27 In the present study, the choice of associating stretching to pompage was due to the latter being a safer form of manual therapy compared to joint manipulation, wherein adverse effects are rarely seen.28 According to Bronfort et al,25 frequent adverse effects include pain worsening, discomfort, dizziness, visual disturbance, and ear symptoms.
According to Wang et al,10 Bronfort et al,25 and Evans et al,29 patients who performed exercises and had manual therapy exhibited higher levels of satisfaction and performance when compared to patients who only received manual therapy.
Our results indicate that patients in both groups reported improvement in the health-related quality of life. A possible explanation to this lies in the role of stretching in reducing pain and increasing RoM, which together may have led to a perceived well-being and thus to the report of an improved quality of life.
Positive results in both quality of life and RoM generally persisted six weeks after the end of the treatment. At the follow-up, there was a slight worsening in pain compared to the end of treatment in both VAS scores and in reported bodily pain in SF-36, although the differences were not significant. This suggests the need for a continuous exercise program so that patients can maintain the positive results obtained with treatment.
Our results did not show differences between groups, that is, between the two kinds of stretching. Each stretching modality has specific features. Global or muscle chain stretching is active and requires the patient’s perception and concentration under a trained therapist’s supervision, whereas conventional stretching is simpler and may be passive or auto-passive and easily learned. Nonetheless, the two stretching programs produced equivalent results.
It might be argued that the stretching time is different in both programs; however, the total stretching time was equal in both groups, and there are no studies that suggest that a longer duration (15 minutes) of stretching is more effective than a shorter one (30 seconds).
The balance between groups may also be explained by the fact that, while in GPR, the stretch force is slowly and gradually distributed along the muscles that make up the muscle chain, while in conventional stretching, the force is more intense but focused and for a shorter period of time. In both cases, the same process, that is, viscoelastic stress relaxation,30 takes place, and muscles are maintained in a static elongated position, regardless of the type of stretching.
Furthermore, the similarity of observed results may be due to the fact that both stretching regimes were performed under the supervision of the same therapist, with the same care and according to the same principles: keeping a regular breathing rhythm with no inspiratory block, never provoking pain, and avoiding compensations; that is, while a muscle segment is being stretched, the compensating shortening of other distant muscles is not allowed.
This explanation might also account for the similar results obtained by Rosário et al,31 Cabral et al,32 and Maluf,33 who also compared the two kinds of stretching and found them to be equally effective.
A literature review34 concluded that the GPR method has been shown to be an effective treatment technique for musculoskeletal diseases. Only one study comparing muscle chain and conventional stretching35 with results that favor GPR was found in literature. Unfortunately, those findings cannot be compared to the results obtained in this study since patients in that study had ankylosing spondilytis.
This study has limitations, such as a small sample size, absence of a control group, and the short follow-up period. Patients were also told not to change their usual medications, which may have helped in reducing pain. At the end of treatment, 90% of subjects reported a reduction in medication usage.
CONCLUSION
Conventional stretching and muscle chain stretching, in association to manual therapy, were equally effective in reducing pain and improving range of motion and quality of life in female patients with chronic neck pain, both immediately after treatment and at a follow-up six weeks later. Since muscle stretching is a low-cost treatment, it should be pursued more often for treating chronic neck pain.
REFERENCES
- 1.Merskey H, Bogduk N, editors. Classification of chronic pain. 2nd ed. Seattle: IASP Task Force on Taxonomy; 1994. [Google Scholar]
- 2.Farina S, Tinazzi M, Le Pera D, Valeriani M. Pain-related modulation of the human motor cortex. Neurol Res. 2003;25:130–42. doi: 10.1179/016164103101201283. [DOI] [PubMed] [Google Scholar]
- 3.Häkkinen A, Salo P, Tarvainen U, Wiren K, Ylinen J. Effect of manual therapy and stretching on neck muscle strength and mobility in chronic neck pain. J Rehabil Med. 2007;39:575–9. doi: 10.2340/16501977-0094. [DOI] [PubMed] [Google Scholar]
- 4.Ylinen J. Physical exercises and functional rehabilitation for the management of chronic neck pain. Eura Medicophys. 2007;43:119–32. [PubMed] [Google Scholar]
- 5.Bogduk N. Neck pain: an update. Aust Fam Physician. 1988;17:75–80. [PubMed] [Google Scholar]
- 6.Bovim G, Schrader H, Sand T. Neck pain in general population. Spine. 1994;19:1307–9. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Hanten WP, Olson SL, Russel JL, Lucio RM, Campbell AH. Total head excursion and resting head posture: normal and patient comparisons. Arch Phys Med Rehabil. 2000;81:62–6. doi: 10.1016/s0003-9993(00)90223-5. [DOI] [PubMed] [Google Scholar]
- 8.Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine. 2004;29:33–40. doi: 10.1097/01.BRS.0000103944.10408.BA. [DOI] [PubMed] [Google Scholar]
- 9.Barnsley L. Neck pain. In: Klippel JH, Dieppe PA, editors. Rheumatology. 2nd ed. London: Mosby-Year Book; 1998. pp. 41–2. [Google Scholar]
- 10.Wang WTJ, Olson SL, Campbell AH, Hanten WP, Gleeson PB. Effectiveness of physical therapy for patients with neck pain: an individual approach using a clinical decision-making algorithm. Am J Phys Med Rehabil. 2003;82:203–18. doi: 10.1097/01.PHM.0000052700.48757.CF. [DOI] [PubMed] [Google Scholar]
- 11.Souchard PE. Principes et originalité de la reéducation posturale globale. Paris: Le Pousoë; 2003. [Google Scholar]
- 12.Marques AP. Cadeias musculares: um programa para ensinar avaliação fisioterapêutica global. São Paulo: Manole; 2005. [Google Scholar]
- 13.Bandy WD, Irion JM, Briggler M. The effect of time and frequency of static stretching on flexibility of the hamstring muscles. Phys Ther. 1997;77:1090–6. doi: 10.1093/ptj/77.10.1090. [DOI] [PubMed] [Google Scholar]
- 14.Bertherat T. Le corps a ses raisons: auto-guérison et anti-gymnastique . Paris: Seuil; 1976. [Google Scholar]
- 15.Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67:1867–72. doi: 10.1093/ptj/67.12.1867. [DOI] [PubMed] [Google Scholar]
- 16.Tousignant M, de Bellefeuille L, O’Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension. Spine. 2000;1(25):324–30. doi: 10.1097/00007632-200002010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Ciconelli RM, Ferraz MB, Santos W. Tradução para a língua portuguesa e validação do questionário genérico de qualidade de vida SF-36. Rev Bras Reumatol. 1999;39:143–9. [Google Scholar]
- 18.Bienfait M. Fáscias e pompages. São Paulo: Summus; 1999. [Google Scholar]
- 19.Kisner C, Colby LA. Exercícios terapêuticos – fundamentos e técnicas. São Paulo: Manole; 1992. [Google Scholar]
- 20.Halbertsma JPK, Mulder I, Göeken LNH, Eisma WH. Repeated passive stretching: acute effect on the passive muscle moment and extensibility of short hamstrings. Arch Phys Med Rehabil. 1999;80:407–14. doi: 10.1016/s0003-9993(99)90277-0. [DOI] [PubMed] [Google Scholar]
- 21.Taylor DC, Brooks DE, Ryan JB. Viscoelastic characteristics of muscle: passive stretching versus muscular contractions. Med Sci Sports Exerc. 1997;29:1619–24. doi: 10.1097/00005768-199712000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Ferreira GNT, Teixeira-Salmela LF, Guimarães CQ. Gains in flexibility related to measures of muscular performance: impact of flexibility on muscular performance. Clin J Sport Med. 2007;17:276–81. doi: 10.1097/JSM.0b013e3180f60b26. [DOI] [PubMed] [Google Scholar]
- 23.Chan SP, Hong Y, Robinson PD. Flexibility and passive resistance of the hamstrings of young adults using two different static stretching protocols. Scand J Med Sci Sports. 2001;11:81–6. doi: 10.1034/j.1600-0838.2001.011002081.x. [DOI] [PubMed] [Google Scholar]
- 24.Coutinho EL, Gomes ARS, França CN, Oishi J, Salvini TF. Effect of passive stretching on the immobilized soleus muscle fiber morphology. Braz J Med Biol Res. 2004;37:1853–61. doi: 10.1590/s0100-879x2004001200011. [DOI] [PubMed] [Google Scholar]
- 25.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26:788–99. doi: 10.1097/00007632-200104010-00020. [DOI] [PubMed] [Google Scholar]
- 26.Vasseljen O, Johansen BM, Westgaard RH. The effect of pain reduction on perceived tension and EMG-recorded trapezius muscle activity in workers with shoulder and neck pain. Scand J Rehabil Med. 1995;27:243–52. [PubMed] [Google Scholar]
- 27.Provinciali L, Baroni M, Illuminati L, Ceravolo MG. Multimodal treatment to prevent the late whiplash syndrome. Scand J Rehabil Med. 1996;28:105–11. [PubMed] [Google Scholar]
- 28.Gross AR, Kay TM, Hondras M, Goldsmith C, Haines T, Peloso P, et al. Manual therapy for mechanical neck disorders: a systematic review. Man Ther. 2002;7:131–49. doi: 10.1054/math.2002.0465. [DOI] [PubMed] [Google Scholar]
- 29.Evans R, Bronfort G, Nelson B, Goldsmith CH. Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine. 2002;27:2383–9. doi: 10.1097/00007632-200211010-00013. [DOI] [PubMed] [Google Scholar]
- 30.McHugh MP, Magnusson SP, Gleim GW, Nicholas JA. Viscoelastic stress relaxation in human skeletal muscle. Med Sci Sports Exerc. 1992;24:1375–82. [PubMed] [Google Scholar]
- 31.Rosário JLP, Sousa A, Cabral CMN, João SMA, Marques AP. Reeducação postural global e alongamento estático segmentar na melhora da flexibilidade, força muscular e amplitude de movimento: um estudo comparativo. Fisioter Pesq. 2008;15:12–8. [Google Scholar]
- 32.Cabral CMN, Yumi C, Sacco ICN, Casarotto RA, Marques AP. Eficácia de duas técnicas de alongamento muscular no tratamento da síndrome femoropatelar: um estudo comparativo. Fisioter Pesq. 2007;14:48–56. [Google Scholar]
- 33.Maluf SA. Efeito da reeducação postural global e do alongamento estático analítico em portadores de disfunção temporomandibular: um estudo comparativo [Tese] São Paulo: Faculdade de Medicina, Universidade de São Paulo; 2007. [Google Scholar]
- 34.Vanti C, Generali A, Ferrari S, Nava T, Dosarelli T, Pillastrini P. La rieducazione posturale globale nelle patologie muscolo-scheletriche: evidenze scientifiche e indicazioni cliniche (Rééducation Posturale Globale in musculoskeletal diseases: scientific evidence and clinical practice) Reumatismo. 2007;59:192–201. [PubMed] [Google Scholar]
- 35.Fernández-de-las-Peñas C, Alonso-Blanco C, Morales-Cabezas M, Miangolarra-Page JC. Two exercise interventions for the management of patients with ankylosing spondylitis. Am J Phys Med Rehabil. 2005;84:407–19. doi: 10.1097/01.phm.0000163862.89217.fe. [DOI] [PubMed] [Google Scholar]