Abstract
Surgical releases for arthrogrypotic clubfeet have high recurrence rates, require further surgery, and result in short, painful feet. We asked whether a modified Ponseti technique could achieve plantigrade, braceable feet. Ten patients (mean age, 16.2 months; range, 3–40 months), with 19 arthrogrypotic clubfeet, underwent an initial percutaneous Achilles tenotomy to unlock the calcaneus from the posterior tibia followed by weekly Ponseti-style casts. A second percutaneous Achilles tenotomy was performed in 53%. Mean number of casts was 7.7 (range, 4–12). From pretreatment to completion of initial series of casts, mean scores of Dimeglio et al. improved from 16 to 5 (ranges, 12–18 and 2–9, respectively), Catterall scores (as modified by Pirani and colleagues) from 4.8 to 0.9 (ranges, 1.5–6.0 and 0.0–2.0), and maximum passive dorsiflexion from −45° (range, −75° to −20°) to 10° (range, 0° to 40°). Ankle-foot orthoses maintained correction. At the minimum followup of 13 months (mean, 38.5 months; range, 13–70 months), the mean maximum dorsiflexion was 5° (range, –20° to 20°), two patients had posterior releases and no patient’s ambulatory ability was compromised by foot shape. Arthrogrypotic clubfeet can be corrected without extensive surgery during infancy or early childhood. Limited surgery may be required as the children age.
Introduction
Arthrogryposis, or arthrogryposis multiplex congenita, is not a specific diagnosis, but rather a constellation of signs associated with various diseases or syndromes. These conditions have in common nonprogressive congenital contractures in two or more joints in multiple body areas [25]. Etiologies are often multifactorial or as yet unknown. Clubfeet are the most frequent foot deformities of arthrogryposis and tend to be more severe and rigid than idiopathic clubfeet [7, 16, 26, 33, 34, 52]. In 1970, Lloyd-Roberts and Lettin [33] described the goal of treatment of the arthrogrypotic clubfoot is “to convert a deformed rigid foot into a rigid plantigrade platform.” Earlier articles detailed the difficulty obtaining a satisfactory result, with three to four procedures performed per foot [16, 23]. Much of the recent literature still highlights the high recurrence rate, describing procedures to treat failed feet [11, 36].
Current primary treatment options for the arthrogrypotic clubfoot include manipulation and serial casting before an extensive surgical soft tissue release [7, 16, 23, 24, 30, 34, 37, 38, 41, 42, 44, 50–52] and talectomy [8, 13, 16, 17, 20, 23, 29, 31, 34, 36, 38, 41, 45]. Secondary procedures include repeat soft tissue release, talectomy, cancellectomy of the talus and cuboid (Verebelyi-Ogston procedure) [22, 46], gradual correction using an Ilizarov external fixator [6, 11, 19, 21], triple arthrodesis [16, 23, 33], and combined cuboid/cuneiform osteotomies [40]. Most of these procedures usually produce a plantigrade foot, but one with poor range of motion and recurrence of the deformity is common despite consistent orthotic wear [7, 16, 37, 44, 52]. Recurrences are difficult to treat despite the secondary procedures, and the results are often unsatisfactory [7, 8, 16, 20, 31, 37, 41, 44, 52].
In light of the frequent recurrences requiring further surgery after invasive treatment of arthrogrypotic clubfeet, we believe an important adjunct to the treatment goal of Lloyd-Roberts and Lettin [33] would be “to achieve that objective with as few procedures, of the least ablative nature, possible.” This would be similar to Turco’s goal for idiopathic clubfeet, obtaining “a cosmetically acceptable, plantigrade foot; to spare the child and parents the ordeal of multiple operations and hospitalizations” [48]. Many authors have noted nonoperative treatment, usually serial casting, cannot correct the arthrogrypotic clubfoot deformity because the joint capsules are thickened and rigid [16, 23, 33, 39]. Others, however, demonstrate a number of these feet can be corrected, without recurrences, solely through casting [5, 7, 10, 23, 38, 44].
Since 1996, the Ponseti method [39] of clubfoot treatment has gained attention and popularity for its ability to correct idiopathic clubfoot deformities. The Ponseti method consists of a series of weekly manipulations and cast changes and, in most patients, a percutaneous Achilles tenotomy before application of the last 3-week cast. The emphasis is on correcting the foot deformity through forefoot abduction, rotating both the calcaneus and the forefoot around the stationary talus. A “foot abduction brace” is used for maintenance of the correction. The technique has been reproducibly successful in treating the idiopathic clubfoot [1, 12, 28, 32, 35, 47].
Recently, the Ponseti method has been used to treat clubfeet associated with distal arthrogryposis syndromes. Boehm et al. [5] used the technique successfully in 24 clubfeet of 12 patients with distal arthrogryposis. Six feet had a relapse but were successfully treated by repeat casting. Bevan et al. [4] also had early success treating clubfeet associated with distal arthrogryposis with the method. Both these authors, as well as Dr Ponseti himself [39], did not believe the method was applicable to classic or amyoplastic clubfeet, because these are more rigid than clubfeet associated with distal arthrogryposis.
We asked whether the Ponseti method, modified by performing an initial percutaneous Achilles tenotomy before casting would: (1) correct the arthrogrypotic clubfoot; (2) result in a plantigrade foot; (3) avoid extensive surgery during infancy and early childhood despite recurrences; and (4) allow for ambulation to the best of the patient’s potential with braces if necessary.
Materials and Methods
We retrospectively reviewed the records of all arthrogrypotic patients who presented to the authors’ (WBL, HvB) office or the Ponseti Clubfoot Center with clubfeet for treatment from August 2001 to August 2006. We identified 10 patients (19 feet) presenting at a mean age of 16.2 months (range, 3–40 months). All 10 patients were treated with a modified Ponseti technique by the senior surgeons (WBL, HvB). A multidisciplinary team determined the following specific diagnoses for seven of the patients: two axonal neuropathy, two congenital myopathy, one neurogenic arthrogryposis multiplex congenital, one amyoplasia congenital, and one syndromic, renal and deformational, all of which are nonprogressive syndromes sharing the characteristic of severe fetal akinesia. The remaining three patients had an unspecified arthrogryposis considered to be amyoplasia. None of the patients could be classified as distal arthrogryposis [2, 3, 27], and most presented with an appearance of classic arthrogryposis [4] with four-extremity involvement, including the larger joints. The minimum followup from the completion of the initial series of casts was 13 months (mean, 38.5 months; range, 13–70 months). Six patients (12 feet) had more than 2 years of followup (mean, 53.6 months; range, 43.5–70 months). At last followup, the mean age was 58.2 months (range, 19–86.5 months). In this Institutional Review Board-approved retrospective study, patients’ charts were reviewed for clubfoot rating scores, age at initial Achilles tenotomy and cast application, number of casts, any further treatment of feet (recasting or surgery), maximum passive dorsiflexion, orthoses, and functional status.
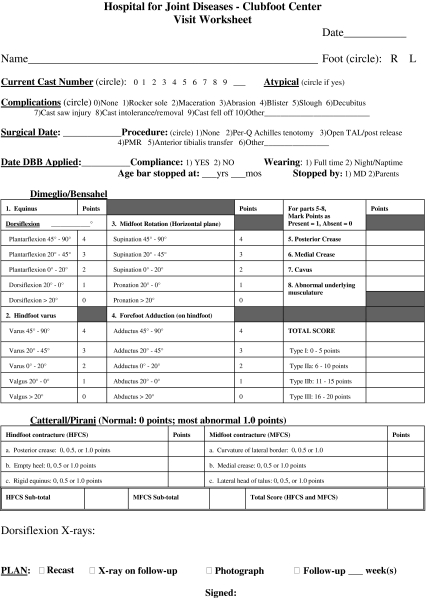
At the initial and each followup visit, each clubfoot was scored using two different clubfoot grading systems, the classification of Dimeglio et al. [14] and the Catterall scores [9] (as modified by Pirani and colleagues and as reported by Lehman et al. [18, 32]) (Appendix 1); we will refer to this system as the Catterall/Pirani score. The classification of Dimeglio et al. [14] records four parameters of positioning (ankle equinus, hindfoot varus, horizontal plane derotation of the calcaneopedal block [midfoot supination], and forefoot adduction) as well as the presence or absence of four traits (posterior and medial creases, midfoot cavus, and abnormal musculature). Each of the positioning parameters is graded on a 4-point scale, whereas the traits, if present, are worth a point apiece, for a maximum score of 20 points. Point scores of 0 to 5 coincide with a Grade I foot with a mild deformity, 90% reducible; 6 to 10 points is a Grade II or moderate deformity; 11 to 15 points is a Grade III or severe deformity; and feet that score 16 to 20 points are a Grade IV or very severe deformity. The Catterall/Pirani score consists of three hindfoot findings (presence of a posterior crease, emptiness of the heel, and extent of rigid equinus) and three midfoot findings (curvature of the lateral border, presence of a medial crease, and palpation of the lateral head of the talus). Each finding is scored as 0 (no deformity), 0.5 (mild or passively correctible deformity), or 1.0 (severe deformity) for a best possible score of 0.0 and a worst possible score of 6.0. Also, at each visit, maximum ankle dorsiflexion was measured with the knee as straight as possible given the often associated knee flexion contractures.
The first step in the modified Ponseti method was to “unlock” the calcaneus from the posterior tibia by performing a percutaneous Achilles tenotomy under local anesthesia in the clinic at the initial visit (Fig. 1A–B). This tenotomy was performed exactly as the ones routinely performed on our patients undergoing the Ponseti technique for their idiopathic clubfeet. After the tenotomy, serial weekly Ponseti-style long leg casts with manipulation were started, including changing the first posttenotomy cast after only 1 week (rather than the typical 3 weeks after a tenotomy). Ponseti–style casts are long leg casts with the knee flexed at, or as close as possible to 90°, with gradual abduction of the foot beneath the stabilized talar head [39]. No attempt is made to manipulate the calcaneus into valgus or to pronate the forefoot. The feet were re–evaluated weekly. Once the heel was in valgus and the forefoot was fully abducted (approximately 60º) and no longer supinated, the amount of ankle dorsiflexion was assessed. If the ankle could not dorsiflex above plantigrade, a second percutaneous Achilles tenotomy was performed under local anesthesia in the clinic. The last cast was molded in 10° to 20° dorsiflexion and full abduction for 3 weeks regardless of whether the second tenotomy was required. Early attempts to maintain correction with a standard foot abduction orthosis (FAO) led to recurrences, which were treated with repeat casting. Subsequently, we had the patients wear solid ankle-foot orthoses (AFOs) during the day and dorsiflexion pull-strap AFOs at night (Fig. 2). For the patients with knee contractures, knee-ankle-foot orthoses (KAFOs) with ratcheting knees were also used at night (Table 1).
Fig. 1A–B.
Photographs of Patient 3 (A) before and (B) after initial percutaneous Achilles tenotomy performed under local anesthesia in the clinic. The knee is held in maximal extension. The baby had undergone 13 casts elsewhere and was then indicated for a posteromedial release with resection of tendons before presentation.
Fig. 2.
Photograph of a nighttime dorsiflexion pull-strap ankle-foot orthosis, which is used after completion of casting.
Table 1.
Initial series of casts
| Patient number | Foot | Initial visit | Initial series of casts | Completion of initial series of casts | |||||
|---|---|---|---|---|---|---|---|---|---|
| Age (months) | Scores* | Maximum passive DF | Number of casts | Second tenotomy | Scores* | Maximum passive DF | Initial braces | ||
| 1 | Right | 4.0 | 17, 4.0 | −45° | 4 | No | 2, 0.5 | 0º | FAO full-time |
| Left | 17, 4.0 | −45° | 4 | No | 2, 0.5 | 0º | |||
| 2 | Right | 5.0 | 17, 6.0 | −45° | 9 | Yes | 7, 1.5 | 15º | Solid AFOs day |
| Left | 17, 6.0 | −45° | 9 | Yes | 8, 1.5 | 15º | KAFOs night (ratcheting knee) | ||
| 3 | Right | 5.0 | 17, 6.0 | −25° | 4 | No | 3, 2.0 | 40º | Solid AFOs full-time |
| 4 | Right | 3.0 | 15, 6.0 | −75° | 6 | No | 3, 1.0 | 30º | Solid AFOs day |
| Left | 15, 6.0 | −75° | 6 | No | 3, 1.0 | 30º | DF AFOs night | ||
| 5 | Right | 40.0 | 18, 4.0 | −45° | 12 | Yes | 8, 1.5 | 0º | Solid AFOs full-time |
| Left | 18, 4.0 | −45° | 12 | Yes | 9, 2.0 | 0º | |||
| 6 | Right | 13.0 | 18, 6.0 | −45° | 9 | No | 5, 1.0 | 0º | Solid AFOs day |
| Left | 18, 6.0 | −45° | 9 | No | 6, 1.0 | 0º | KAFOs night | ||
| 7 | Right | 34.5 | 16, 5.5 | −30° | 11 | Yes | 7, 0.0 | 15º | Solid AFOs day |
| Left | 18, 5.0 | −30° | 11 | Yes | 6, 0.0 | 15º | KAFOs night (ratcheting knee) | ||
| 8 | Right | 10.0 | 13, 5.0 | −45° | 9 | Yes | 3, 1.0 | 0º | Solid AFOs day |
| Left | 13, 5.0 | −45° | 9 | Yes | 2, 1.0 | 20º | KAFOs night (ratcheting knee) | ||
| 9 | Right | 16.5 | 16, 5.0 | −20° | 7 | Yes | 5, 1.0 | 0º | Solid AFOs day |
| Left | 16, 5.0 | −20° | 7 | Yes | 5, 1.0 | 0º | DF AFOs night | ||
| 10 | Right | 30.5 | 12, 2.0 | −60° | 4 | No | 6, 0.5 | 0º | Solid AFOs day |
| Left | 12, 1.5 | −60° | 4 | No | 5, 0.0 | 0º | KAFOs night (ratcheting knee) | ||
| Mean | 16.2 | 16, 4.8 | −44.5° | 7.7 | 5, 0.9 | 9.5° | |||
| (range) | (3.0–40.0) | (12–18), (1.5–6.0) | (−75° to −20°) | (4–12) | (2–9), (0–2.0) | (0°–40°) | |||
* Dimeglia/Bensahel, Catterall/Pirani; DF = dorsiflexion; FAO = foot abduction orthosis; AFO = ankle–foot orthosis; KAFO = knee-ankle-foot orthosis.
Results
We were able to correct all feet. For the initial series of casts (Table 1), the mean number of casts was 7.7 (range, 4–12), with 10 of the 19 feet requiring a second percutaneous Achilles tenotomy. Patient 5, a 3 year old, had seven casts, a second tenotomy, and then five more casts. The mean score of Dimeglio et al. [14] was 16 (range, 12–18) pretreatment and five (range, 2–9) at the completion of the initial series of casts. Similarly, the mean Catterall/Pirani scores improved from 4.8 (range, 1.5–6) to 0.9 (range, 0–2). The mean maximum passive ankle dorsiflexion increased from −45° (range, −75° to −20°) pretreatment to 10° (range, 0°–40°) at completion of treatment (Fig. 3A–F).
Fig. 3A–F.
Photographs show the left foot (A–C) before treatment and (D–F) after the removal of the last cast of the initial series (seven casts and second tenotomy) of a 16.5-month-old girl (Patient 9).
Most patients achieved a plantigrade foot. At the time of latest followup, the mean maximum passive dorsiflexion was 5° (range, −20° to 20°) (Table 2). The six patients (12 feet) with more than 2 years of followup had a mean dorsiflexion of 0° (range, −20° to 20°). Five feet (26.3%) had developed a mean equinus of 10° (range, 5°–20°). All feet remained braceable, and none of the patients’ ambulatory ability was compromised by their foot shape.
Table 2.
Dorsiflexion at latest followup and functional level pretreatment and at latest followup
| Patient | Latest followup | Maximum DFa | Function | ||||
|---|---|---|---|---|---|---|---|
| Length (mos) | Age (mos) | Latest followup | Pretreatment | Latest followup | Braces latest followup | ||
| 1 | Right | 48.5 | 54.0 | 10° | Only 4 months old | Independent ambulation without assistive device | Hinged AFOs day; DF AFOs night |
| Left | 10° | ||||||
| 2 | Right | 70.0 | 77.0 | −5° | Only 5 months old | Independent ambulation without assistive device; uses wheelchair long distances | KAFOs full-time |
| Left | −5° | ||||||
| 3 | Right | 15.5 | 22.0 | 0° | Preemie (corrected age 3 months); limited active movement | Standing independently with braces | Solid AFO day; KAFO night |
| 4 | Right | 14.0 | 19.0 | 10° | Only 3 months old, very limited active movement | Rolling; standing in stander with braces | KAFOs (ratcheting knee) full-time |
| Left | 10° | ||||||
| 5 | Right | 13.0 | 56.5 | 10° | Sitting independently; non-ambulatory | Independent ambulation with posterior rollator | Solid AFOs |
| Left | 10° | ||||||
| 6 | Right | 57.5 | 84.5 | 20° | Rolling, not sitting independently | Limited ambulation with posterior rollator in school only | Solid AFOs day; DF AFOs night |
| Left | 15° | ||||||
| 7 | Right | 49.0 | 86.5 | 0° | Sitting independently, standing with support | Limited ambulation with gait trainer; standing in stander | Floor reaction AFOs for ambulation; solid AFOs |
| Left | −5° | ||||||
| 8 | Right | 53.0 | 67.0 | −20° | Not rolling or sitting | Sitting independently, standing with braces for 1 minute | KAFOs |
| Left | −20° | ||||||
| 9 | Right | 20.5 | 39.5 | 10° | Rolling, sitting when propped | Sitting independently, not standing, non-ambulatory | Solid AFOs day; DF AFOs night |
| Left | 10° | ||||||
| 10 | Right | 43.5 | 75.5 | 0° | Rolling, sitting, crawling, not standing, non-ambulatory | Non-ambulatory, uses wheelchair | Solid AFOs; KAFOs (ratcheting knee) |
| Left | 0° | ||||||
| Mean | 38.5 | 58.2 | 3.2° | ||||
| (range) | (13–70) | (19–86.5) | (–20 to 20°) | ||||
aMaximum passive dorsiflexion.
We were able to avoid extensive surgery in these patients at the time of last followup. Four patients (eight of 19 feet) had early recurrences and required additional series of casts, two of which (four feet) required one additional series (Patients 7 and 9) and the other two patients (four feet) required two additional series (Patients 2 and 6) (Table 3). The mean interval between series was 12.7 months (range, 4–17.5 months) and the mean number of casts in the additional series was 4.8 (range, 2–8). An additional tenotomy was performed in three of the six series. Two patients had late recurrences that required surgery other than a percutaneous Achilles tenotomy. Patient 2 underwent bilateral percutaneous Achilles tenotomies and percutaneous posterior ankle releases for the correction of 5° equinovarus contractures concurrent with posterior knee release procedures at 6.5 years of age (4 years after completion of three series of casts). A percutaneous posterior ankle release is performed by inserting a small hemostat clamp through the stab incision used for the percutaneous Achilles tenotomy. Under fluoroscopic guidance, the clamp is used to penetrate the posterior aspects of the ankle and subtalar joint, then spreading, to disrupt the capsule. Patient 8 did not tolerate his braces and experienced recurrences of 40º of equinus. At 21 months of age, 7 months after the completion of his initial clubfoot casts, he was taken to the operating room to address his hip and knee contractures, at which time he also underwent open bilateral posterior ankle releases. At the latest followup, 3 years and 10 months after surgery, this 5.5 year old continued to refuse to wear braces consistently, and his equinus contractures recurred to 20°.
Table 3.
Patients with additional series of casts (all were bilateral)
| Patient number | Additional series | Time after previous casting (months) | Number of casts | Tenotomy |
|---|---|---|---|---|
| 2 | 2nd | 4 | 4 | Yes |
| 3rd | 11 | 8 | Yes | |
| 6 | 2nd | 16.5 | 8 | No |
| 3rd | 17.5 | 3 | Yes | |
| 7 | 2nd | 14 | 4 | No |
| 9 | 2nd | 13 | 2 | No |
| Mean | 12.7 | 4.8 | ||
| (range) | (4.0–17.5) | (2–8) |
All patients were nonambulatory pretreatment, seven of the 10 being younger than 18 months; five of the 10 patients were ambulatory at latest followup (Table 2). Only three of these five were independent ambulators with orthoses: Patient 1 with hinged AFOs without an assistive device, Patient 2 with KAFOs without an assistive device, and Patient 5 with solid AFOs and a posterior rollator. Patient 7 ambulated with floor reaction AFOs and a gait trainer, and Patient 6 ambulated in school with solid AFOs and a posterior rollator (Fig. 4A–C). Three patients (Patients 3, 4, 8) were not yet ambulatory, but showed continued progress with the potential to attain independent ambulation. The remaining two patients (Patients 9, 10) will most likely remain nonambulatory, showing no ability to kneel tall or stand with bracing and support.
Fig. 4A–C.
Photographs of Patient 6, 7-year-old boy with bilateral clubfeet at 57.5 months of followup. He had two additional series of casts and ambulates with solid ankle-foot orthoses and a posterior rollator. (A) A posterior view of the feet in standing; (B) a dorsal view of the feet in standing; and (C) dorsiflexion of the right foot measured at 20°.
Discussion
Clubfeet associated with arthrogryposis are stiffer than the idiopathic type, and correction is more difficult to obtain and maintain, even with extensive surgery. The Ponseti method of clubfoot correction has been very effective in avoiding surgery for idiopathic clubfeet [1, 15, 28]. We asked if the Ponseti method, modified by an initial percutaneous Achilles tenotomy, could correct arthrogrypotic clubfeet without the need for extensive surgery at an early age and create a foot suitable for ambulation.
The current study has a number of limitations. It is a retrospective case series without a comparison group. In our Ponseti Clubfoot Center, all clubfeet are scored on the Dimeglio et al. and Catterall/Pirani scales each visit as standard protocol. Despite the data not being collected prospectively for this particular study, they were collected consistently in an objective and detailed fashion. The literature provides ample historical information against which we can compare our patients. Our cohort size is small, only 10 patients with 19 affected feet, reflecting a rare condition. The followup period is brief, with a minimum followup of 13 months. The time is therefore inadequate to ensure there will be no more recurrences. We plan future reports with longer followup, including intermediate to late recurrences, but our purpose in this report is to detail the success in correcting stiff arthrogrypotic clubfeet without extensive or ablative surgery during infancy or early childhood. Our study includes children with various diagnoses underlying their arthrogrypotic presentation. Most presented with an appearance of classic arthrogryposis (four-extremity involvement including the larger joints) despite subsequent further diagnostic stratification. None were classified as distal arthrogryposis, which are less rigid and more responsive to cast treatment than clubfeet associated with classic arthrogryposis and amyoplasia [4, 5, 27].
Historically, it has been difficult to correct and maintain the correction of the teratologic clubfeet associated with arthrogryposis. Early treatment is recommended, because arthrogrypotic contractures are most supple during infancy. Even then, treatment has been essentially surgical with a spectrum of progressively more extensive measures recommended, both as primary and secondary procedures. The two most common surgeries are soft tissue releases and talectomies.
Soft tissue procedures range from simple Achilles tenotomies and posterior releases to “radical” soft tissue releases [7, 16, 23, 24, 30, 33, 37, 38, 42–44, 50–52]. Satisfactory results reported for soft tissue procedures range from 100% to 21% (Table 4) with the better correction maintained in feet addressed at a younger age by more aggressive surgeries. The high recurrence rate after soft tissue releases is theoretically the result of insufficient soft tissues medially, which limits the initial correction and the lack of long-term adaptive changes of the wedged apart medial tarsal bones [34].
Table 4.
Literature review of soft tissue releases for arthrogrypotic clubfeet
| Author | Year of publication | Average age at surgery | Number of feet | Procedure | Followup time | Percent satisfactory |
|---|---|---|---|---|---|---|
| Lloyd-Robert and Lettin [33] | 1970 | NR | 14 | Soft tissue release | NR | 21 |
| Drummond and Cruess [16] | 1978 | 2.7 years | 23 | PR, TAL | NR | 26 |
| Zimbler and Craig [52] | 1983 | NR | 24 | PMR with resection of tendons, extensive capsulotomies | NR | 91 |
| Carlson et al. [7] | 1985 | 3.6 years | 26 | PMR | NR | 27 |
| Guidera and Drennan [23] | 1985 | NR | 28 | PMR | 12 years | 25 |
| Palmer et al. [38] | 1985 | 3 years | 20 | PMR | NR | 75 |
| Södergård and Ryöppy [44] | 1994 | 3 weeks | 52 | PMR | 16.3 years | 64 |
| Niki et al. [37] | 1997 | 7.3 months | 41 | PMR | 37.4 months | 27 |
| Widmann et al. [50] | 2005 | 7.4 months | 12 | PMR with resection of tendons, extensive capsulotomies | 4.3 years | 75 |
| Khan and Chinoy [30] | 2006 | 12.5 months | 5 | PMR with resection of tendons | 1 year | 100 |
NR = not reported; PMR = posterior medial release; PR = posterior release; TAL = tendo-Achilles lengthening.
Talectomies have been used both as a primary procedure [8, 16, 17, 23, 29, 34, 41] (Table 5) and as salvage procedures after recurrences [8, 13, 16, 17, 20, 23, 29, 31, 41, 45]. Removing the talus provides the hindfoot laxity needed to correct equinus and varus deformities and creates a stable neojoint between the mortise and the calcaneus [8, 17, 31, 34]. Talectomies, however, do not adequately address the forefoot deformity [13, 31]. Spontaneous tibiocalcaneal fusion occurs in some patients, although it is not clear if this is an undesirable finding [17, 29, 45], and it occasionally is performed surgically to alleviate pain after talectomy [36]. The literature is difficult to interpret, because studies often group results of primary and salvage procedures together and combine arthrogrypotic clubfeet with other kinds of teratologic clubfeet. A few authors have suggested talectomy as the primary treatment for arthrogrypotic clubfeet but base their recommendations on only one or two bilaterally treated patients without documented followup [23, 45]. Larger series of primary talectomies report satisfactory results of only 45% to 50% (Table 5).
Table 5.
Literature review of primary talectomies for arthrogrypotic clubfeet
| Author | Year of publication | Average age at surgery | Number of feet | Followup time | Percent satisfactory |
|---|---|---|---|---|---|
| Drummond and Cruess [16] | 1978 | 32 months | 11 | NR | 45 |
| Hsu et al. [29] | 1984 | NR | 1 | NR | NR |
| Guidera and Drennan [23] | 1985 | NR | 4 | NR | NR |
| Palmer et al. [38] | 1985 | NR | 33 | NR | 48 |
| Segal et al. [41] | 1989 | 46 months | 14 | 40 months | 50 |
| Sølund et al. [45] | 1991 | NR | 2 | NR | NR |
| D’Souza et al. [17] | 1998 | 26 months | 8 | 6.4 years | 50 |
| Cassis and Capdevila [8] | 2000 | NR | 16 | NR | NR |
NR = not reported.
Initially, we were unsuccessful using the Ponseti method for children with arthrogryposis and clubfeet, because the severe equinus prevented the heel from rotating under the talus. We then modified the technique by performing an initial percutaneous Achilles tenotomy before any casting. This “unlocked” the heel from the posterior tibia and allowed the foot to respond to the manipulation of the Ponseti method. Casts were then changed weekly until the forefoot adduction/supination and hindfoot varus were corrected. Fifty-three percent of the feet required a second percutaneous Achilles tenotomy before the last cast, because the ankle could not be dorsiflexed above plantigrade. We found recurrences first manifested as ankle equinus and hindfoot varus, and therefore believe it important to gain full correction of the hindfoot initially with a goal of attaining 20° of dorsiflexion. Repeating the tenotomy does not appear to cause future foot shape or function difficulties, because the feet tend to be stiff with little active plantar/dorsiflexion regardless of treatment. Other authors have reported on Achilles tendon resection without compromising function [50, 52]. A final cast was worn for 3 weeks followed by bracing to maintain the correction. After recurrences occurred in our first few patients when the typical FAO was used, we changed to solid AFOs during the day and dorsiflexion pull-strapped AFOs at night. We hypothesized the FAOs were not effective in this patient group, because most arthrogrypotics with extensive lower extremity involvement do not kick their legs, unlike the children with idiopathic clubfeet. Likely, that kicking motion helps to stretch out the ankle musculature.
The earlier the feet can be addressed, the more flexible they are and easier they are to correct. Patient 1 needed four casts to correct stiff deformities (Dimeglio et al. [14] score of 17, Catterall/Pirani score of 4.0) at 4 months of age compared with seven casts for Patient 9 with similarly stiff feet (Dimeglio et al. [14] score of 16, Catterall/Pirani score of 5.0) at 13 months of age. Patient 6 required nine casts at 13 months of age compared with 12 casts for Patient 5 at 40 months of age for equally stiff feet (Catterall/Pirani scores of 6.0 and 4.0, respectively, Dimeglio et al. [14] score of 18 for both). Patient 5 was the oldest patient treated in this series, presenting with bilaterally untreated feet at nearly 3½ years of age. Even at that late age, we were able to bring her feet to a plantigrade position, which allowed her to become ambulatory with a posterior rolling walker and AFOs.
Our algorithm for a child with multilevel lower extremity involvement is to treat the feet at initial presentation, when they are at their most flexible. In those patients with knee extension contractures, the casts are molded to gradually increase knee flexion. Once the feet are corrected, KAFOs are fabricated to both maintain the foot correction and stretch knee flexion or extension contractures with ratcheting step-lock hinges. At approximately 1 year of age, the hip positional deformities or dislocations are addressed either by proximal femoral osteotomies or open reductions. Once the child demonstrates the hip, head, and trunk control necessary for a standing program, any severe knee flexion contractures are addressed by posterior releases alone or, for contractures greater than 40°, together with an Ilizarov frame for gradual contracture correction [49].
All feet in this study were corrected to at least neutral dorsiflexion (plantigrade) after completion of the first series of casts. In our experience, the average number of casts per foot was greater in the arthrogrypotic clubfoot than the idiopathic clubfoot [1] (7.7 versus 5.5). Twenty-one percent of the feet had one additional series of casts and 21% had two additional series of casts to treat recurrences. Two patients had more than Achilles tenotomies; both had bilateral posterior releases, open in one case and percutaneous in the other. Therefore, recurrence requiring surgical treatment is 21% for our series. This rate is likely to gradually rise as the cohort ages, but the treatment is appreciably milder than those for failed talectomies and extensive soft tissue releases. At latest followup, all patients continued to have braceable feet. Functionally, 50% of patients were ambulatory, 30% were perambulatory, and 20% did not have the capacity to ambulate.
A different standard of rating treatment results should be applied to the arthrogrypotic clubfoot compared with the idiopathic clubfoot. The goals are to avoid surgery in the infant and young child and to reduce the extent of any surgery that may be required as the child matures. We found a modified Ponseti method provided initial correction of the arthrogrypotic clubfoot and could be also be used to address most recurrences. Additional limited surgery was performed in only four of the 19 feet. We expect any salvage procedures, if needed, will be much less extensive than those required for feet historically treated with more extensive surgical procedures. We have been able to achieve and maintain braceable feet, creating a stable platform for weightbearing with the extent of surgery, in most cases, being only an Achilles tenotomy.
Appendix 1
Footnotes
Study conducted at NYU Hospital for Joint Diseases, New York, NY.
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
The authors certify that their institution (NYU Medical Center) has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Abdelgawad AA, Lehman WB, Bosse HJP, Scher DM, Sala DA. Treatment of idiopathic clubfoot using the Ponseti method: minimum 2-year follow-up. J Pediatr Orthop B. 2007;16:98–105. doi: 10.1097/BPB.0b013e32801048bb. [DOI] [PubMed] [Google Scholar]
- 2.Bamshad M, Jorde LB, Carey JC. A revised and extended classification of the distal arthrogryposes. Am J Med Genet. 1996;65:277–281. doi: 10.1002/(SICI)1096-8628(19961111)65:4<277::AID-AJMG6>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 3.Beals RK. The distal arthrogryposes: a new classification of peripheral contractures. Clin Orthop Relat Res. 2005;435:203–210. doi: 10.1097/01.blo.0000157540.75191.1d. [DOI] [PubMed] [Google Scholar]
- 4.Bevan WP, Hall JG, Bamshad M, Staheli LT, Jaffe KM, Song K. Arthrogryposis multiplex congenita (amyoplasia): an orthopaedic perspective. J Pediatr Orthop. 2007;27:594–600. doi: 10.1097/BPO.0b013e318070cc76. [DOI] [PubMed] [Google Scholar]
- 5.Boehm S, Limpaphayom N, Alaee F, Sinclair MF, Dobbs MB. Early results of the Ponseti method for the treatment of clubfoot in distal arthrogryposis. J Bone Joint Surg Am. 2008;90:1501–1507. doi: 10.2106/JBJS.G.00563. [DOI] [PubMed] [Google Scholar]
- 6.Brunner R, Hefti F, Tgetgel JD. Arthrogrypotic joint contracture at the knee and the foot: correction with a circular frame. J Pediatr Orthop B. 1997;6:192–197. doi: 10.1097/01202412-199707000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Carlson WO, Speck GJ, Vicari V, Wenger DR. Arthrogryposis multiplex congenita: a long-term follow-up study. Clin Orthop Relat Res. 1985;194:115–123. [PubMed] [Google Scholar]
- 8.Cassis N, Capdevila R. Talectomy for clubfoot in arthrogryposis. J Pediatr Orthop. 2000;20:652–655. doi: 10.1097/00004694-200009000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Catterall A. A method of assessment of the clubfoot deformity. Clin Orthop Relat Res. 1991;264:48–53. [PubMed] [Google Scholar]
- 10.Chen RC, Gordon JE, Luhmann SJ, Schoenecker PL, Dobbs MB. A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop. 2007;27:522–528. doi: 10.1097/bpo.0b013e318070cc19. [DOI] [PubMed] [Google Scholar]
- 11.Choi IH, Yang MS, Chung CY, Cho TJ, Sohn YJ. The treatment of recurrent arthrogrypotic clubfeet in children by the Ilizarov method: a preliminary report. J Bone Joint Surg Br. 2001;83:731–737. doi: 10.1302/0301-620X.83B5.11019. [DOI] [PubMed] [Google Scholar]
- 12.Colburn M, Williams M. Evaluation of the treatment of idiopathic clubfoot by using the Ponseti method. J Foot Ankle Surg. 2003;42:259–267. doi: 10.1016/S1067-2516(03)00312-0. [DOI] [PubMed] [Google Scholar]
- 13.Dias LS, Stern LS. Talectomy in the treatment of resistant talipes equinovarus deformity in myelomeningocele and arthrogryposis. J Pediatr Orthop. 1987;7:39–41. doi: 10.1097/01241398-198701000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B. 1995;4:129–136. doi: 10.1097/01202412-199504020-00002. [DOI] [PubMed] [Google Scholar]
- 15.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86:22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Drummond DS, Cruess RL. The management of the foot and ankle in arthrogryposis multiplex congenita. J Bone Joint Surg Br. 1978;60:96–99. doi: 10.1302/0301-620X.60B1.627587. [DOI] [PubMed] [Google Scholar]
- 17.D’Souza H, Aroojis A, Chawara GS. Talectomy in arthrogryposis: analysis of results. J Pediatr Orthop. 1998;18:760–764. doi: 10.1097/00004694-199811000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Flynn JM, Donohoe M, Mackenzie WG. An independent assessment of two clubfoot-classification systems. J Pediatr Orthop. 1998;18:323–327. doi: 10.1097/00004694-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Grant AD, Lehman WB. Clubfoot correction using the Ilizarov technique. Bull Hosp Jt Dis Orthop Inst. 1991;51:84–87. [PubMed] [Google Scholar]
- 20.Green AD, Fixsen JA, Lloyd-Roberts GC. Talectomy for arthrogryposis multiplex congenita. J Bone Joint Surg Br. 1984;66:697–699. doi: 10.1302/0301-620X.66B5.6389557. [DOI] [PubMed] [Google Scholar]
- 21.Grill F, Franke J. The Ilizarov distractor for the correction of relapsed or neglected clubfoot. J Bone Joint Surg Br. 1987;69:593–597. doi: 10.1302/0301-620X.69B4.3611163. [DOI] [PubMed] [Google Scholar]
- 22.Gross RH. The role of the Verebelyi-Ogston procedure in the management of the arthrogrypotic foot. Clin Orthop Relat Res. 1985;194:99–103. [PubMed] [Google Scholar]
- 23.Guidera KJ, Drennan JC. Foot and ankle deformities in arthrogryposis multiplex congenita. Clin Orthop Relat Res. 1985;194:93–98. [PubMed] [Google Scholar]
- 24.Hahn G. Arthrogryposis: pediatric review and habilitative aspects. Clin Orthop Relat Res. 1985;194:104–114. [PubMed] [Google Scholar]
- 25.Hall JG. Arthrogryposis multiplex congenita: etiology, genetics, classification, diagnostic approach, and general aspects. J Pediatr Orthop B. 1997;6:159–166. [PubMed] [Google Scholar]
- 26.Hall JG, Reed SD, Driscoll EP. Part I Amyoplasia: a common, sporadic condition with congenital contractures. Am J Med Genet. 1983;15:571–590. doi: 10.1002/ajmg.1320150407. [DOI] [PubMed] [Google Scholar]
- 27.Hall JG, Reed SD, Greene G. The distal arthrogryposes: delineation of new entities—review and nosologic discussion. Am J Med Genet. 1982;11:185–239. doi: 10.1002/ajmg.1320110208. [DOI] [PubMed] [Google Scholar]
- 28.Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting idiopathic clubfoot. J Pediatr Orthop. 2002;22:517–521. doi: 10.1097/00004694-200207000-00019. [DOI] [PubMed] [Google Scholar]
- 29.Hsu LC, Jaffray D, Leong JC. Talectomy for club foot in arthrogryposis. J Bone Joint Surg Br. 1984;66:694–696. doi: 10.1302/0301-620X.66B5.6501362. [DOI] [PubMed] [Google Scholar]
- 30.Khan MA, Chinoy MA. Treatment of severe and neglected clubfoot with a double zigzag incision: outcome of 21 feet in 15 patients followed up between 1 and 5 years. J Foot Ankle Surg. 2006;45:177–181. doi: 10.1053/j.jfas.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Legaspi J, Li YH, Chow W, Leong JC. Talectomy in patients with recurrent deformity in club foot: a long-term follow-up study. J Bone Joint Surg Br. 2001;83:384–387. doi: 10.1302/0301-620X.83B3.11051. [DOI] [PubMed] [Google Scholar]
- 32.Lehman WB, Mohaideen A, Madan S, Scher DM, Bosse HJ, Iannacone M, Bazzi JS, Feldman DS. A method for the early evaluation of the Ponseti (Iowa) technique for the treatment of idiopathic clubfoot. J Pediatr Orthop B. 2003;12:133–140. doi: 10.1097/00009957-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Lloyd-Roberts GC, Lettin AW. Arthrogryposis multiplex congenita. J Bone Joint Surg Br. 1970;52:494–508. [Google Scholar]
- 34.Menelaus MB. Talectomy for equinovarus deformity in arthrogryposis and spina bifida. J Bone Joint Surg Br. 1971;53:468–473. [PubMed] [Google Scholar]
- 35.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113:376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 36.Nicomedez FP, Li YH, Leong JC. Tibiocalcaneal fusion after talectomy in arthrogrypotic patients. J Pediatr Orthop. 2003;23:654–657. doi: 10.1097/00004694-200309000-00015. [DOI] [PubMed] [Google Scholar]
- 37.Niki H, Staheli LT, Mosca VS. Management of clubfoot deformity in amyoplasia. J Pediatr Orthop. 1997;17:803–807. doi: 10.1097/00004694-199711000-00020. [DOI] [PubMed] [Google Scholar]
- 38.Palmer PM, MacEwen GD, Bowen JR, Mathews PA. Passive motion therapy for infants with arthrogryposis. Clin Orthop Relat Res. 1985;194:54–59. [PubMed] [Google Scholar]
- 39.Ponseti IV. Congenital Clubfoot: Fundamentals of Treatment. Oxford, UK: Oxford University Press; 1996. [Google Scholar]
- 40.Schaefer D, Hefti F. Combined cuboid/cuneiform osteotomy for correction of residual adductus deformity in idiopathic and secondary club feet. J Bone Joint Surg Br. 2000;82:881–884. doi: 10.1302/0301-620X.82B6.10845. [DOI] [PubMed] [Google Scholar]
- 41.Segal LS, Mann DC, Feiwell E, Hoffer MM. Equinovarus deformity in arthrogryposis and myelomeningocele: evaluation of primary talectomy. Foot Ankle. 1989;10:12–16. doi: 10.1177/107110078901000103. [DOI] [PubMed] [Google Scholar]
- 42.Sells JM, Jaffe KM, Hall JG. Amyoplasia, the most common type of arthrogryposis: the potential for good outcome. Pediatrics. 1996;97:225–231. [PubMed] [Google Scholar]
- 43.Simons GW. Complete subtalar release in club feet. Part I: a preliminary report. J Bone Joint Surg Am. 1985;67:1044–1055. [PubMed] [Google Scholar]
- 44.Södergård J, Ryöppy S. Foot deformities in arthrogryposis multiplex congenital. J Pediatr Orthop. 1994;14:768–772. doi: 10.1097/01241398-199414060-00015. [DOI] [PubMed] [Google Scholar]
- 45.Sølund K, Sonne-Holm S, Kjølbye JE. Talectomy for equinovarus deformity in arthrogryposis: a 13 (2–20) year review of 17 feet. Acta Orthop Scand. 1991;62:372–374. doi: 10.3109/17453679108994473. [DOI] [PubMed] [Google Scholar]
- 46.Spires TD, Gross RH, Low W, Barringer W. Management of the resistant myelodysplastic or arthrogrypotic clubfoot with the Verebelyi-Ogston procedure. J Pediatr Orthop. 1984;4:705–710. doi: 10.1097/01241398-198411000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Tindall AJ, Steinlechner CW, Lavy CB, Mannion S, Mkandawire N. Results of manipulation of idiopathic clubfoot deformity in Malawi by orthopaedic clinical officers using the Ponseti method: a realistic alternative for the developing world? J Pediatr Orthop. 2005;25:627–629. doi: 10.1097/01.bpo.0000164876.97949.6b. [DOI] [PubMed] [Google Scholar]
- 48.Turco VJ. Resistant congenital clubfoot: one-stage posteromedial release with internal fixation: a follow-up report of a fifteen-year experience. J Bone Joint Surg Am. 1979;61:805–814. [PubMed] [Google Scholar]
- 49.Bosse HJP, Feldman DS, Anavian J, Sala DA. Treatment of severe knee flexion contractures in children with arthrogryposis. J Pediatr Orthop. 2007;27:930–937. doi: 10.1097/bpo.0b013e3181594cd0. [DOI] [PubMed] [Google Scholar]
- 50.Widmann RF, Do TT, Burke SW. Radical soft-tissue release of the arthrogrypotic clubfoot. J Pediatr Orthop B. 2005;14:111–115. doi: 10.1097/01202412-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 51.Williams P. The management of arthrogryposis. Orthop Clin North Am. 1978;9:67–88. [PubMed] [Google Scholar]
- 52.Zimbler S, Craig CL. The arthrogrypotic foot plan of management and results of treatment. Foot Ankle. 1983;3:211–219. doi: 10.1177/107110078300300406. [DOI] [PubMed] [Google Scholar]






