Abstract
Nine patients presenting during infancy were identified with clubfeet and absent anterior and lateral compartment functions. We considered these to be neurogenic clubfeet. All patients had the drop toe sign: resting posture of the toes in plantarflexion and absent active dorsiflexion movement after plantar stimulation of the foot. Two patients (three feet) underwent exploration of the peroneal nerve, which revealed anatomic abnormalities. Six patients required more casts than typical for initial correction of deformity; all but two had Achilles tenotomy. Four relapsed despite full-time bracing and eventually needed intraarticular surgery to achieve a plantigrade foot. Idiopathic absent peroneal nerve function is not a well-described entity in the clubfoot literature. All babies with clubfoot should be examined for the drop toe sign. When noted, the feet will likely be more difficult to correct initially, may need early Achilles tendon lengthening, will likely need permanent bracing, are likely to relapse and need intraarticular surgery, and may need multiple surgeries to remain plantigrade throughout growth.
Level of Evidence: Level IV, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The Ponseti method has become widely accepted as the best current practice for the treatment of children born with congenital clubfoot [1, 5, 7, 9]. Recently Ponseti et al. published a report on patients with clubfeet that did not respond to the standard treatment protocol and called these feet complex idiopathic clubfeet [10]. They described clinical features typical of complex clubfeet, referenced Turco’s 1994 description of “atypical” clubfeet [13], and presented a detailed approach to manipulations and casting that differs substantially from the classic Ponseti method [8]. The senior author (SLF) has infrequently encountered another subgroup of patients with clubfoot presenting for Ponseti method treatment who also seemed to not respond to classical treatment. These are patients who lack the ability to actively dorsiflex the toes or ankle or evert the foot.
The purpose of this report is to highlight this population of patients with apparent idiopathic congenital clubfoot who have idiopathic peroneal nerve dysfunction, lacking anterior and lateral leg compartment muscular functions. We describe the clinical findings in this group and examined whether or not the classic Ponseti method would result in correction of the foot deformities in these children.
Materials and Methods
We retrospectively reviewed 187 clubfoot patients seen during infancy between August 1998 and December 2007 and nine patients (5%) were identified (13 clubfeet) who had no active dorsiflexion of the toes or ankle and no active eversion on the affected sides. We considered these to be neurogenic clubfeet. All nine patients (13 lower extremities) had intact active plantarflexion of the toes and ankles. Calf atrophy was present on all 13 involved lower extremities. Seven were boys and two were girls, and four had bilateral clubfeet. All of the patients had a drop toe sign: resting posture of the toes in plantarflexion and no active toe extension after plantar stimulation. In contrast, the typical congenital clubfoot patient exhibits spontaneous toe dorsiflexion when moving the feet (Fig. 1) and will actively dorsiflex the ankle and toes in response to plantar foot stimulation. The patients were followed to a minimum age of 10 months (mean 3.5 years, range 10 months to 9 years).
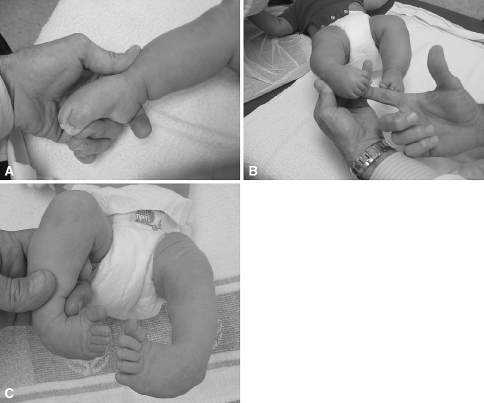
Fig. 1A–C.
(A) In the drop toe sign, the toes are held in a plantarflexed position. (B) Persistent plantarflexion of toes is noted even after plantar stimulation of the foot; no active toe dorsiflexion is noted. (C) In a typical congenital clubfoot, spontaneous dorsiflexion of the toes is noted.
Two had mild anterior bowing of the leg (Fig. 2). Six of the patients had no other discernible abnormality on physical examination. None of the patients had a family history of clubfoot, neurologic or muscle disorders. Two patients had congenital constriction band syndrome, with unilateral clubfoot but no bands on the involved lower extremity. The other seven patients were carefully examined for constriction bands on the involved and uninvolved extremities and none were found. One patient had multiple congenital anomalies (eye, palate, and heart) but no spinal abnormalities or other orthopaedic deformities. Four presented with clubfoot relapses after being treated with serial manipulations and casting elsewhere; five were diagnosed within 2 weeks of birth. Three of four with initial treatment elsewhere had not been diagnosed with a neurologic deficit by the initial treating surgeon. The neurologic investigations in our patients were not standardized but always included a thorough physical examination of the spine and other extremities for any signs of deformity or dysfunction. None of the new patients had the neurologic deficit identified by the referring pediatrician or an orthopaedic resident.
Fig. 2.
More severely affected feet have extreme equinus, abnormal plantar and posterior skin creases, and often an anterior bow to the tibia as the tight posterior muscles, tendons, and ligaments are not opposed by anterior compartment muscle function.
The initial Pirani rating [3] was 6 of 6 for 11 feet and 4 of 6 for two feet. All patients were treated using the Ponseti method [10], with a range of four to 11 manipulations and cast applications. All but two (the less severe feet initially) underwent percutaneous tendoachilles tenotomy. Two of the patients had recurrent slippage of casts and then developed features consistent with complex clubfoot (absent the hyperextended first toe). These patients were then managed with a short break from casting to allow swelling to resolve, early tendoachilles tenotomy, and the modified manipulation and casting technique described by Ponseti et al. [10] (Fig. 3). The two patients with initial Pirani scores of 4 both achieved 25° of dorsiflexion after four and five casts. All the remaining patients had less than 10° of ankle dorsiflexion after tenotomy and were treated with continued weekly manipulation and casting until at least 5° of dorsiflexion was obtained (Fig. 4).
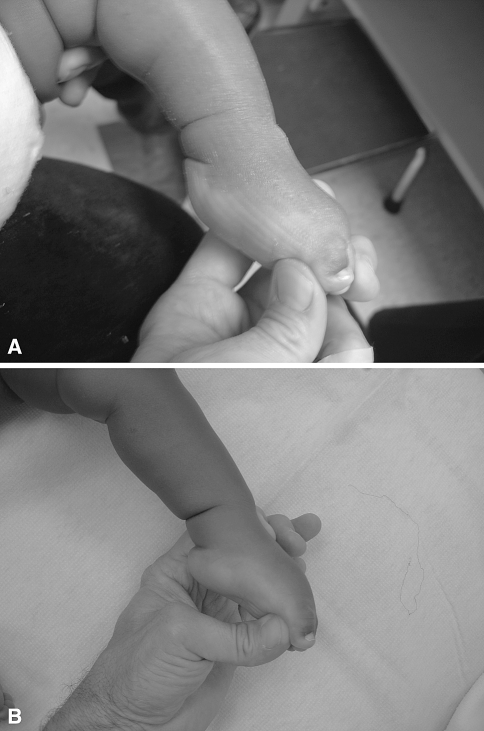
Fig. 3A–B.
(A) Drop toe sign and a swollen foot with a proximally displaced heel pad are noted after casting elsewhere and three casts slipping off. (B) After a casting “break” of 3 weeks, swelling has resolved and the heel pad is in better position, but an extreme stiff equinus position remains. Early tendoachilles tenotomy is beneficial in feet with this much plantarflexion to prevent cast slippage.
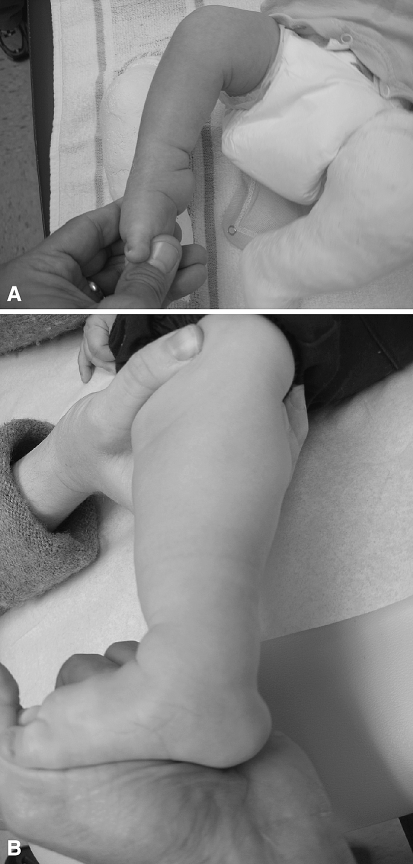
Fig. 4A–B.
(A) The initial photograph shows severe plantarflexion deformity and abnormal posterior ankle and plantar foot creases. (B) The photograph after early tenotomy, nine casts, and 3 months of solid ankle-foot orthosis at neutral in daytime and foot abduction orthosis wear at night shows dorsiflexion limited to a few degrees above neutral.
At the conclusion of casting, all but one (eight patients) were placed initially into well-molded shoes attached to a foot abduction bar in outward rotation full time for 3 months. These eight patients were then fit with a molded solid plastic ankle foot orthosis in neutral position that was worn in the daytime and the foot abduction bar was worn at night. The other patient was placed in a knee-ankle-foot orthosis full time initially.
Five patients had radiographs of the spine that were normal. Four patients had MRI of the cervical, thoracic, and lumbar spine with no abnormalities identified. Three patients had EMG and nerve conduction studies, completed between the ages of 9 and 18 months, and each demonstrated peroneal nerve dysfunction with normal tibial nerve function.
Results
Before our evaluation, only one patient had an abnormal neurologic examination documented in the medical record or communicated to the family, including three who had been treated with prior casting.
Only two of the patients had typical initial deformity correction with Ponseti method casting (four and five casts); both had less severe initial Pirani ratings. The remaining patients needed more manipulation and casting sessions than usual (7 to 11 casts), and after Achilles tenotomy had less ankle dorsiflexion (did not achieve 15–20 degrees) than usual, necessitating continued weekly manipulations and casting to achieve at least 5 degrees of dorsiflexion before beginning bracing. Because of the muscle imbalance, all patients were maintained in an ankle-foot orthosis full time after casting in an effort to prevent relapse. Thus far, only one patient older than 3 years has maintained a plantigrade foot position without intraarticular surgery.
Four of the nine patients have had relapses and underwent intraarticular surgery to obtain a plantigrade foot position after attempts to correct the deformities with further casting failed. One patient had a second recurrence treated with foot osteotomies and underwent dorsiflexion osteotomy of the distal tibia. Another patient had exploration of the peroneal nerve bilaterally while undergoing bilateral posterior ankle and subtalar releases and posterior compartment tendon lengthenings. The findings were symmetric, revealing a normal-appearing full-diameter peroneal nerve proximal to the proximal leg fascia with only a thin atrophic nerve distally.
Discussion
This series of patients illustrates the need for an initial careful, detailed neurologic examination for all clubfoot patients to document the presence or absence of peroneal nerve function. All babies with clubfoot should be examined for the drop toe sign, and when present further investigation may be warranted. Radiographs and MRI were performed in some patients, but no abnormalities to explain the neurologic deficits were found. EMGs and nerve conduction studies were performed in two patients and were abnormal. The electrodiagnostic studies did not provide information that changed treatment or altered prognosis, and the value of these studies is thus debatable. Identifying deficient anterior and lateral leg compartment functions alerts the practitioner the feet will be more difficult to correct initially and may need nonclassical Ponseti method management, including earlier-than-usual Achilles tendon lengthening.
If patients treated with casting have severe equinus that leads to the foot slipping proximally into the cast, the foot may develop features of a complex clubfoot. These features include swelling, the dorsal skin pushed distally with the toes “disappearing,” and the heel pushed against the posterior tibia and flattened (Fig. 3A). Correcting this necessitates a shift to the modified method with limited abduction, early Achilles tenotomy, dorsiflexion manipulation under the first and fifth metatarsal heads, splints behind the ankle and in front of the knee, and immobilization in 110° or more of knee flexion [10]. As in the treatment of complex clubfoot, less ankle dorsiflexion is accepted in the treatment of neurogenic clubfoot. The muscle imbalance creates the need for permanent bracing, and the feet are likely to relapse and eventually need intraarticular surgery.
Transfer of the posterior tibialis to the dorsum of the foot could be considered but we performed none in our patients. The limited ankle range of motion, especially dorsiflexion, and the lack of normal excursion of the posterior tibialis muscle in clubfoot patients may make transfer less successful. In addition, parents can be counseled intraarticular surgeries and perhaps multiple surgeries may be needed to maintain a plantigrade foot position throughout growth. This is a major departure from the principles of treatment espoused by Ponseti [8], as surgery that divides ligaments and joint capsules is believed to lead to scarring, limited motion, relapsing deformity with growth, and pain in early adulthood. We agree with this philosophy and attempt to practice according to Ponseti’s recommendations, but these patients apparently lacking either superficial or deep peroneal nerve function were unable to maintain a functional foot shape and position with manipulations, casting, and tendon surgery alone.
Idiopathic peroneal nerve palsy is not well-described in the clubfoot literature to our knowledge. Gordon and Dunn [4] described peroneal nerve palsy as a complication of clubfoot treatment in four cases treated with prolonged casting, attributing the nerve palsy to cast pressure on the peroneal nerve in the area of the fibular head. Interestingly, none of the four cases had normal peroneal nerve function explicitly documented before initiation of cast treatment, so it is possible these cases may represent congenital peroneal nerve palsies. All of the cases were resistant and recurrent, and the neurologic abnormality was discovered late. The authors noted, as the deformity seen with peroneal nerve palsy resembles that seen with congenital clubfoot, it would be easy to miss peroneal nerve palsy in clubfoot patients. We agree and thus emphasize the need to specifically look for the drop toe sign and to document the presence of active toe and ankle dorsiflexion ability during the initial assessment of children with clubfeet.
A recent publication by Song et al. [11] describes six patients with congenital clubfoot and concomitant peroneal nerve palsy similar to the patients in this report. They reported a poor prognosis for clubfoot patients with peroneal nerve palsy and noted abnormalities in electrodiagnostic studies in all six. Four of the six patients underwent corrective surgery after failing cast correction attempts, and some had multiple surgeries. Interestingly, they note one parent sued the surgeon who performed initial treatment, because peroneal nerve palsy was not mentioned when the clubfoot was first treated, and the parent assumed the palsy was caused by the use of above-knee casts.
While the etiology of congenital clubfoot is not determined, some have proposed a neurologic abnormality leading to muscle imbalance. Feldbrin et al. [2] performed electrophysiologic studies on 52 children with clubfeet and found isolated peroneal nerve damage in 27%. The clinical findings in these children were not described, so it is not known if any had the drop toe sign or clinically apparent signs of peroneal nerve dysfunction. An abnormal electrophysiologic study was a poor prognostic indicator in their study. Neuromuscular disease has been recognized by others as a risk factor for deformity recurrence [6], and we had a very high incidence of relapse (four of nine) in these patients, with short-term followup (10 months to 3.5 years) on the five patients without relapse to date. Two of the patients in this report had congenital constriction band syndrome but did not have any bands noted on the side with clubfoot and peroneal nerve palsy. We have seen cases of constriction bands in the proximal lateral leg causing a constrictive peroneal nerve lesion that leads to an equinovarus foot deformity, and this paralytic type of clubfoot associated with constriction bands has been described in the literature [12]. No bands were noted on the lower extremities of any of the cases reported here.
Patients with clubfoot and a drop toe sign signaling lack of peroneal nerve function are challenging to treat. It is more difficult initially to achieve deformity correction, and maintaining a plantigrade foot position with growth may not be possible, even with full-time bracing.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Each author certifies that his or her institution either has waived or does not require approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86:22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Feldbrin Z, Gilai AN, Ezra E, Khermosh O, Kramer U, Wientroub S. Muscle imbalance in the aetiology of idiopathic clubfoot. J Bone Joint Surg Br. 1995;77:596–601. [PubMed] [Google Scholar]
- 3.Flynn JM, Donohoe M, Mackenzie WG. An independent assessment of two clubfoot-classification systems. J Pediatr Orthop. 1998;18:237–323. doi: 10.1097/00004694-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Gordon SL, Dunn EJ. Peroneal nerve palsy as a complication of clubfoot treatment. Clin Orthop Relat Res. 1974;101:229–231. [PubMed] [Google Scholar]
- 5.Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods for idiopathic clubfoot. J Pediatr Orthop. 2002;22:517–521. doi: 10.1097/00004694-200207000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Lovell ME, Morcuende JA. Neuromuscular disease as the cause of late clubfoot relapses: a report of four cases. Iowa Orthop J. 2007;27:82–84. [PMC free article] [PubMed] [Google Scholar]
- 7.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot by using the Ponseti method. Pediatrics. 2004;113:376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 8.Ponseti IV. Congenital Clubfoot: Fundamentals of Treatment. Oxford, UK: Oxford University Press; 1996. [Google Scholar]
- 9.Ponseti IV, Smoley EN. Congenital club foot: the results of treatment. J Bone Joint Surg Am. 1963;45:261–344. [Google Scholar]
- 10.Ponseti IV, Zhivkov M, Davis N, Sinclair M, Dobbs MB, Morcuende JA. Treatment of the complex congenital idiopathic clubfoot. Clin Orthop Relat Res. 2006;451:171–176. doi: 10.1097/01.blo.0000224062.39990.48. [DOI] [PubMed] [Google Scholar]
- 11.Song KS, Kang CH, Min BW, Bae GC, Cho CH, Lee JH. Congenital clubfoot with concomitant peroneal nerve palsy in children. J Pediatr Orthop B. 2008;17:85–89. doi: 10.1097/bpb.0b013e3282f548fc. [DOI] [PubMed] [Google Scholar]
- 12.Tada K, Yonenobu K, Swanson AB. Congenital constriction band syndrome. J Pediatr Orthop. 1984;4:726–730. doi: 10.1097/01241398-198411000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Turco V. Recognition and management of the atypical idiopathic clubfoot. In: Simons GW, ed. The Clubfoot: The Present and a View of the Future. New York, NY: Springer-Verlag; 1994:76–77.