Abstract
The Ponseti method is reportedly effective for treating clubfoot in children up to 9 years of age. However, whether age at the beginning of treatment influences the rate of successful correction and the rate of relapse is unknown. We therefore retrospectively reviewed 68 consecutive children with 102 idiopathic clubfeet treated by the Ponseti technique in four Portuguese hospitals. We followed patients a minimum of 30 months (mean, 41.4 months; range, 30–61 months). The patients were divided into two groups according to their age at the beginning of treatment; Group I was younger than 6 months and Group II was older than 6 months. All feet (100%) were initially corrected and no feet required extensive surgery regardless of age at the beginning of treatment. There were no differences between Groups I and II in the number of casts, tenotomies, success in terms of rate of initial correction, rate of recurrence, and rate of tibialis anterior transference. The rate of the Ponseti method in avoiding extensive surgery was 100% in Groups I and II; relapses occurred in 8% of the feet in younger and older children.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Clubfoot is a congenital deformity that historically has been difficult to correct and difficult to maintain once corrected. Its treatment has been controversial throughout the last 150 years [29]. Long-term followup showing clubfeet treated by extensive surgery led to a worse quality of life in adulthood has contributed to a decline in the enthusiasm for surgery, because repeated soft tissue releases can result in a stiff, painful, and arthritic foot and a considerably impaired quality of life [10]. In the last decade, the Ponseti method has become increasingly popular and is reportedly effective for treating clubfoot in children up to 9 years of age [23]. Although the principles of the Ponseti technique are simple, the healthcare provider must have a thorough understanding of the deformity and be highly skilled with regard to manipulation and application of plaster casts [29]. A sound knowledge of the anatomy and kinematics of the foot is extremely important [16, 24, 30]. The goal of treatment is to achieve a functional, pain-free, plantigrade foot with good mobility and without calluses able to fit into regular shoes [29, 30].
Many groups have reported their success with the technique in completely different economic, cultural, and healthcare settings [1, 3, 6, 11–13, 21–23, 26, 36, 40]. It is believed that manipulation should start as soon as possible [19, 29, 30]. However, several authors have demonstrated that even patients presenting late with clubfoot can be successfully treated by the Ponseti method [3, 23]. Whether and how much age at the beginning of treatment influences the rate of successful correction and the rate of relapse is, however, unknown.
We therefore first asked whether age at presentation and initial correction (ie, younger or older than 6 months) influenced correction rates, recurrence rates, or rate of tibialis anterior transference. We then asked if the number of casts, tenotomies, and success in terms of rate of initial correction differed by age of initial correction.
Materials and Methods
We retrospectively reviewed 68 consecutive children with 102 idiopathic clubfeet treated by the Ponseti method in four Portuguese hospitals. We included patients who presented with uncorrected clubfeet and previous tenotomy, because we considered this a previous nonoperative treatment. We excluded from this study all children with clubfeet secondary to any other cause and all children with previous posteromedial or posterior release, although we always try the Ponseti method in those cases as well. We began to use the Ponseti method at our institutions in 2003 and 2004. Treatment by this technique was recommended to every patient (age range, 1 day to 31 months) presenting from then on independent of previous nonoperative treatment or statement of need for posteromedial release. Our oldest patient in this series was 31 months old. However, none of our institutions has established an upper cutoff age limit to apply the Ponseti method. Our minimum followup was 30 months (mean, 41.4 months; range 30–60 months). We divided the patients into two groups (Table 1) depending on the age at initiation of treatment. Group I was younger than 6 months, whereas Group II was older than 6 months. Group I included 33 boys and 17 girls with 77 clubfeet treated in the first 6 months of life; of these children, 27 came from areas outside of usual encatchment areas of the institution where they would be treated because the parents were specifically seeking treatment by the Ponseti method. Eight had previous casting. Group II included 14 boys and four girls with 25 clubfeet, all of whom were treated by us after 6 months of age (12 were older than 12 months of age when the treatment was started by us). All children in Group II had previous nonoperative treatment, which also included percutaneous Achilles tenotomy in three feet. Fourteen children came from areas outside of the encatchment areas of our institutions. In Group I, the mean age at the beginning of treatment was 22.4 days (range, 1–171 days). The minimum followup for Group I was 30 months (mean, 41.3 months; range, 30–61 months). In Group II, mean age at the beginning of treatment was 402.8 days (range, 180–924 days). Minimum followup for this group was 30 months (mean, 41.6 months; range, 30–55 months). In 11 cases, the families stated the previous treating surgeon proposed posteromedial release.
Table 1.
Data from patients in Group I and Group II
| Variable | Group I (less than 6 months of age) | Group II (greater than 6 months of age) |
|---|---|---|
| Number of patients | 50 | 18 |
| Number of clubfeet | 77 | 25 |
| Age at beginning of treatment | Mean, 22.4 days (range, 1–171 ± 37.5 days) | Mean, 402.8 days (range, 180–924 ± 233.6 days) |
| Followup time | Mean, 41.3 months (range, 30–61 ± 7.1 months) | Mean, 41.6 months (range, 30–55 ± 7.5 months) |
| Male:female | 33:17 | 14:4 |
| Unilateral:bilateral clubfoot | 23:27 | 11:7 |
| Number of casts | Mean, 5.3 casts (range, 4–8 ± 0.9) | Mean, 4.3 casts (range, 3–7 ± 1.2) |
| Tenotomies | 84.4% | 80% |
| Relapses | 7.8% | 8% |
| Tibialis anterior transference | 4 | 1 |
| Posteromedial release | 0 | 0 |
The protocol followed was the same in all four institutions. The orthopaedic surgeon performed the manipulation and casting according to the Ponseti method [21, 23–25, 29, 30]. Plaster of Paris was used. Usually, the surgeon was helped by a nurse or another orthopaedic surgeon or trainee who was knowledgeable of the Ponseti method. The families were asked to soak the casts in warm water before coming to the hospital and then wrap them in plastic bags. The cast was cut with scissors or with a cast knife and removed in the hospital. We prefer not to use saws, because they disturb the child and are frightening for the family. Furthermore, the casts tended to be thin and we were concerned a saw might injure the child’s skin. We attempted to create a calm environment, in which the child could be relaxed. We try to reproduce faithfully the Ponseti technique of manipulation, casting, tenotomy, and bracing [25, 26, 29, 30]. The cavus was initially corrected by supinating and gently abducting the forefoot in proper alignment with the hindfoot. With the longitudinal arch of the foot well molded and the forefoot in slight supination, the foot was gradually abducted under the talus, which was secured against rotation in the ankle mortise by applying counterpressure with the thumb against the lateral aspect of the head of the talus. In our series, approximately 70° of abduction was accomplished with three to eight progressive serial casts, never pronating the foot or touching the heel. In some patients who came from outside our encatchment areas, we applied an “accelerated” Ponseti protocol, changing the casts every 5 days, because the reduced time between the casts does not influence the outcome [25]. If residual equinus was observed and the foot had been abducted 60° to 70°, a percutaneous tenotomy was performed under local anesthesia and the foot was immobilized in the final cast with 70° of abduction and 10° to 20° of dorsiflexion. After 3 weeks in the final cast, a foot abduction orthosis (FAO), consisting of a Dennis Browne bar and straight last shoes, was applied [30]. Bars and shoes from different companies were used in the four institutions. Nonetheless, the principles were the same. The distance between the shoe heels in the bar was adjusted to match the distance between the shoulders. The shoes were turned to 70° of external rotation in bilaterally affected children and to 70° of rotation for the clubfoot and 40° to 45° of rotation for the normal foot in unilaterally affected children. The FAO was used for 23 hours per day for the first 3 months and then at night and during naps. Initially, we recommended 3 years of bracing, but being aware of the importance of the brace in avoiding recurrences [11, 14, 24, 26, 31, 32, 38], we suggested to the families to keep the brace until the child was 4 to 5 years of age.
We considered the foot “corrected” when it was clinically possible to achieve at least 15° of dorsiflexion, 70° of abduction, a neutral or slightly valgus heel, and a straight lateral foot border. Later loss of dorsiflexion, varus of the heel, or dynamic supination was identified as a “relapse.” Relapses in children younger than 2 years old were treated with recasting and rebracing. In older children, the family was offered recasting and rebracing or recasting and tibialis anterior transference. Before doing surgery, we obtained a radiograph to ensure the ossific nuclei of the third cuneiform were present.
We recorded the patients’ demographics and compared the number of casts needed to achieve correction, the rate of relapses, the need for posteromedial release (PMR), and the need for tibialis anterior transference (Table 1). We used Pearson’s chi square test to compare these categorical variables for Groups I (younger than 6 months) and II (older than 6 months). The primary end point for this study was the need for PMR at any stage in both groups. The secondary end point was the need for surgical treatment of a relapse by means of a tibialis anterior transfer (TAT). Patients with previous PMR or posterior releases were excluded from this study.
Results
Groups I and II were similar in terms of successful initial correction, rate of relapses, need for PMR, and the need for TAT at the time of followup for this study. Correction was achieved in every child by means of the Ponseti method. When the groups were combined, our rate of posteromedial release at 41.4 months of mean followup was 0%, our overall relapse rate was 7.8%, and our TAT rate was 4.9% (already including the patient in whom this surgery is scheduled). Although all the children were older than 2.5 years of age at followup, 76.4% of the children were still using their FAO at night.
The average number of casts, tenotomies and rate of initial correction was similar in the two groups. The average number of casts necessary to achieve correction in Group I was 5.3 (range, four to eight casts). Percutaneous Achilles tenotomy was needed in 84.4% of the cases. At a mean followup of 41.3 months, there were no PMRs in Group I and six feet (7.8%) had a relapse. In four cases, the reason for the relapse was identified as intolerance of the brace. Three children had a TAT for treatment of the relapse and one is scheduled for this surgery, whereas the other two have been treated with a new series of casting and reapplication of the brace. Forty-two patients are still using the FAO. The average number of casts necessary to achieve correction in Group II was 4.3 (range, three to seven casts). Tenotomy was performed in 80% of the cases. At a mean followup of 41.6 months, 10 patients in Group II were still using the FAO. All feet were initially corrected by the Ponseti technique and there was no need to perform PMR. We observed a relapse in two feet (8%). The reason for the relapse was identified as intolerance of the brace. Both children had a TAT.
There were no major complications with the technique, namely any bleeding problems associated with the tenotomy, but there were some minor complications. In one case in Group I, a rocker bottom deformity was observed after taking off the final cast. We decided to recast the child, in equinus, to correct the iatrogenic deformity. We applied two casts starting 1 month after the child had the last cast removed. We then repeated the tenotomy approximately 0.5 cm proximally to the site where the previous tenotomy was performed. Correction was then achieved. Other complications included a blister on one foot, which delayed tenotomy for 1 week and an extra cast, and two cases of blisters after the application of the FAO.
Discussion
The Ponseti method has become increasingly popular and is effective for treating clubfoot in children up to 9 years of age [23]. Several groups have reported success with the technique in different economic, cultural, and healthcare settings [1, 3, 6, 11–13, 21–23, 26, 36, 40]. Some authors also demonstrated patients presenting late with clubfoot can be successfully treated by the Ponseti method [3, 23]. Whether age at the beginning of treatment influences successful correction and the rate of relapse is unknown. We therefore asked whether age at presentation and initial correction (ie, younger or older than 6 months) influenced correction rates, recurrence rates, or rate of tibialis anterior transference. We then asked if the number of casts, tenotomies, and success in terms of rate of initial correction differed by age of initial correction.
Our study included the initial patients treated with the Ponseti method in four Portuguese institutions and therefore constitutes experience with a learning curve, but that did not impair our ability to correct these feet. The study has some additional limitations. Because this was a retrospective study, Groups I and II were not matched in terms of previous treatment; we did not classify the clubfeet for severity at the beginning of the treatment; the results were not evaluated according to a standardized outcome measure. Although absence of classification of the clubfoot at the beginning of treatment may be seen as a limitation, several authors [26, 30] suggest the initial classification of severity is not related to the success of treatment, because different feet respond distinctly to the manipulation. The number of casts necessary to achieve correction can be used as a proxy for severity of the deformity [26]. We believe it is difficult to apply an outcome scale in children younger than 5 years of age or to accurately measure range of motion. The mean followup of 41.4 months is relatively short and 76.4% of the children are still using a FAO so some additional relapses may be expected in the future. Although imaging techniques have played a role in our understanding of the pathology and treatment of clubfoot [18, 20, 28, 35], data obtained from the measurement of several radiologic angles in young children might not reflect the quality of the correction obtained in a clubfoot [15]. We elected not to perform radiography on children involved in this study, except in the cases of relapse after 2 years of age. In those cases, radiographs were performed to confirm the presence of the third cuneiform ossific nucleus, so a TAT could be safely performed when needed. However, and despite these limitations, the data confirm the Ponseti method can be used with equal early results in patients younger and older than 6 months.
It is generally recognized the results provided by the Ponseti technique are superior to those accomplished with other treatments, either nonsurgical or surgical [8, 10, 17, 21, 37]. Although the Ponseti treatment is not free of complications [5, 9], we encountered no major problems. We believe the knowledge of the anatomy, pathology, and kinematics of the clubfoot and the sound understanding and strict respect for every detail in the Ponseti technique will decrease the need for extensive surgery in clubfeet and can be replicated by several groups in different settings [1, 4, 6, 12, 13, 17, 21–26, 29–34].
In our institutions, the FAO is only applied when the foot is corrected. Although we share the idea that brace intolerance is one of the main difficulties to overcome when applying this technique [2, 4, 7, 11, 14, 31, 39], we also believe the physician must be able to engage the healthcare team and the family in a synergistic way so brace intolerance and maintenance of correction may be understood as a major goal and responsibility by each person involved in the care of the child with a clubfoot. In this sense, we believe bracing “tolerance” involves continuous efforts from healthcare teams and families. Internet support groups, beyond creating awareness about the deformity and treatment [27], can also have an impact in stimulating adhesion to the bracing protocol. All our cases of relapses, in both Groups I and II, happened in children in whom brace tolerance was an issue, because the families believed the child seemed to be bothered by the brace or they simply decided to stop bracing.
Our initial enthusiasm with the Ponseti method and the active attitude of families who specifically searched for this treatment allowed us to treat patients with ages ranging from 1 day to 31 months. The Ponseti method was applied with equal success in children younger and older than 6 months (Figs. 1A–E, 2A–F, 3A–F), corroborating recent reports from other authors stating that excellent results can be achieved in older children [3, 13, 23]. Furthermore, all patients older than 6 months had previous failed nonoperative treatment, which supports prior data suggesting previously treated feet respond well to the Ponseti method [3, 26]. There was no difference between children younger and older than 6 months in terms of number of casts needed to achieve initial correction, rate of relapses, need for PMR, and the need for TAT at the time of followup for this study. In both groups, correction was achieved in every child by means of the Ponseti method. The major complication we experienced was a case, in Group I (younger than 6 months), in which a rocker bottom deformity was observed after taking off the final cast. We decided to recast the child, in equinus, to correct the iatrogenic deformity. After two casts, we repeated the tenotomy and correction was then achieved. Analyzing this case, we believe the first tenotomy was probably technically deficient and the tendon might not have been completely severed.
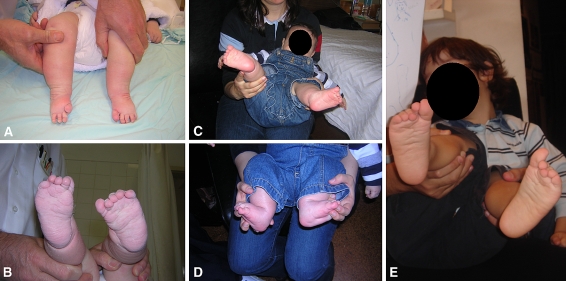
Fig. 1A–E.
(A) A child with bilateral clubfeet with previous nonoperative treatment presented at 5 months of age. (B) The parents specifically came seeking Ponseti treatment. (C) The patient was treated by the Ponseti accelerated protocol with four casts and tenotomy. (D) Both feet were corrected. (E) The same patient remained corrected at 4 years of age and the family decided to stop bracing then. The feet remain corrected at the time of this study.
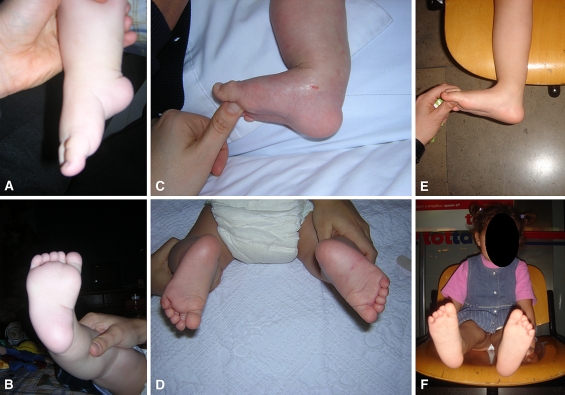
Fig. 2A–F.
(A) A 7-month-old girl presented with unilateral clubfoot with previous casting and percutaneous tenotomy of the Achilles tendon. (B) Posteromedial release was indicated in another institution. (C) The foot was corrected with four casts. (D) There was no need for another tenotomy. (E) The foot remains corrected at 4 years of age and (F) the patient is still compliant with the brace.
Fig. 3A–F.
(A) This 31-month-old child presented with a left clubfoot previously treated with physiotherapy, taping, and casting. (B) At this age, posteromedial release was indicated and the family sought a second opinion. (C) The patient was treated with four casts and a percutaneous tenotomy of the Achilles tendon. (D) Dorsiflexion of both feet is similar. (E) Both feet at 5 years of age. (F) Left foot remains corrected at 5 years of age.
When the groups were combined, our rate of PMR at 41.4 months of mean followup was 0%, our overall relapse rate was 7.8%, and our TAT rate was 4.9% (already including the patient in which this surgery is scheduled). Age at the beginning of treatment did not seem to influence the final outcome. We believe the maximum cutoff age for successful Ponseti treatment has yet to be defined and late-presenting cases should be given a trial for Ponseti treatment, because this does not preclude any subsequent options and has a high probability of success.
Acknowledgments
We thank Luis Filipe Costa Neves, MD, for his support and advice. We also thank Monica Thuesing, MD, and Filipa Monarca, MD, for their help in collecting data for this study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research and that informed consent was obtained.
References
- 1.Abdelgawad AA, Lehman WB, Bosse HJP, Scher DM, Sala DA. Treatment of idiopathic clubfoot using the Ponseti method: minimum 2-year follow-up. J Pediatr Orthop B. 2007;16:98–105. doi: 10.1097/BPB.0b013e32801048bb. [DOI] [PubMed] [Google Scholar]
- 2.Boehm S, Sinclair M. Foot abduction brace in the Ponseti method for idiopathic clubfoot deformity: torsional deformities and compliance. J Pediatr Orthop. 2007;27:712–716. doi: 10.1097/BPO.0b013e3181425508. [DOI] [PubMed] [Google Scholar]
- 3.Bor N, Herzenberg JE, Frick S. Ponseti management of clubfoot in older infants. Clin Orthop Relat Res. 2006;444:224–228. doi: 10.1097/01.blo.0000201147.12292.6b. [DOI] [PubMed] [Google Scholar]
- 4.Bouchoucha S, Smida M, Saïed W, Safi H, Ammar C, Nassib MN, Ghachem MB. Early results of the Ponseti method using the Steenbek foot abduction brace: a prospective study of 95 feet. J Pediatr Orthop B. 2008;17:134–138. doi: 10.1097/BPB.0b013e3282fa5f0d. [DOI] [PubMed] [Google Scholar]
- 5.Burghardt RD, Herzenberg JE, Ranade H. Pseudoaneurysm after Ponseti percutaneous Achilles tenotomy: a case report. J Pediatr Orthop. 2008;28:366–369. doi: 10.1097/BPO.0b013e3181653b6f. [DOI] [PubMed] [Google Scholar]
- 6.Changulani M, Garg NK, Rajagopal TS, Bass A, Nayagam SN, Sampath J, Bruce CE. Treatment of idiopathic club foot using the Ponseti method. Initial experience. J Bone Joint Surg Br. 2006;88:1385–1387. doi: 10.1302/0301-620X.88B10.17578. [DOI] [PubMed] [Google Scholar]
- 7.Chen RC, Gordon JE, Luhmann S, Schoenecker PL, Dobbs MB. A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop. 2007;27:522–528. doi: 10.1097/bpo.0b013e318070cc19. [DOI] [PubMed] [Google Scholar]
- 8.Cooper DM, Dietz FR. Treatment of idiopathic clubfoot. A thirty-year follow-up note. J Bone Joint Surg Am. 1995;77:1477–1489. doi: 10.2106/00004623-199510000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Dobbs MB, Gordon JE, Walton T, Schoenecker PL. Bleeding complications following percutaneous tendoachilles tenotomy in the treatment of clubfoot deformity. J Pediatr Orthop. 2004;24:353–357. doi: 10.1097/00004694-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Dobbs MB, Nunley R, Schoenecker PL. Long-term follow-up of patients with clubfeet treated with extensive soft-tissue release. J Bone Joint Surg Am. 2006;88:986–996. doi: 10.2106/JBJS.E.00114. [DOI] [PubMed] [Google Scholar]
- 11.Dobbs MB, Rudzki DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86:22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Docker CEJ, Leuthwaite N, Kiely NT. Ponseti treatment in the management of clubfoot deformity—a continuing role for paediatric orthopaedic services in secondary care centres. Ann R Coll Surg Eng. 2007;89:510–512. doi: 10.1308/003588407X187739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Göksan SB, Bursali A, Bilgili F, Sivacioglu S, Ayanoglu S. Ponseti technique for the correction of idiopathic clubfeet presenting up to 1 year of age. A preliminary study in children with untreated or complex deformities. Arch Orthop Trauma Surg. 2006;126:15–21. doi: 10.1007/s00402-005-0070-9. [DOI] [PubMed] [Google Scholar]
- 14.Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007;89:487–493. doi: 10.2106/JBJS.F.00169. [DOI] [PubMed] [Google Scholar]
- 15.Herbsthofer B, Eckardt A, Rompe JD, Küllmer K. Significance of radiographic angle measurements in evaluation of congenital clubfoot. Arch Orthop Trauma Surg. 1998;117:324–329. doi: 10.1007/s004020050259. [DOI] [PubMed] [Google Scholar]
- 16.Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop. 2002;22:517–521. doi: 10.1097/00004694-200207000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am. 2003;85:1286–1294. doi: 10.2106/00004623-200307000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Ippolito E, Fraracci L, Farsetti P, Di Mario M, Caterini R. The influence of treatment on the pathology of club foot. CT study at maturity. J Bone Joint Surg Br. 2004;86:574–580. [PubMed] [Google Scholar]
- 19.Kite JH. Nonoperative treatment of congenital clubfoot. Clin Orthop Relat Res. 1972;84:29–38. doi: 10.1097/00003086-197205000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Kuhns LR, Koujok K, Hall JM, Craig C. Ultrasound of the navicular during the simulated Ponseti maneuver. J Pediatr Orthop. 2003;23:243–245. doi: 10.1097/00004694-200303000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am. 1980;62:23–31. [PubMed] [Google Scholar]
- 22.Lehman WB, Mohaideen A, Madan S, Scher D, Bosse HJP, Iannacone M, Bazzi JS, Feldman DS. A method for the early evaluation of the Ponseti (Iowa) technique for the treatment of idiopathic clubfoot. J Pediatr Orthop B. 2003;12:133–140. doi: 10.1097/00009957-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Lourenço AF, Morcuende JA. Correction of neglected idiopathic club foot by the Ponseti method. J Bone Joint Surg Br. 2007;89:378–381. doi: 10.1302/0301-620X.89B3.18313. [DOI] [PubMed] [Google Scholar]
- 24.Morcuende JA. Congenital idiopathic clubfoot: prevention of late deformity and disability by conservative treatment with the Ponseti technique. Pediatr Ann. 2006;35:128–136. doi: 10.3928/0090-4481-20060201-13. [DOI] [PubMed] [Google Scholar]
- 25.Morcuende JA, Abbasi D, Dolan LA, Ponseti IV. Results of an accelerated Ponseti protocol for clubfoot. J Pediatr Orthop. 2005;25:623–626. doi: 10.1097/01.bpo.0000162015.44865.5e. [DOI] [PubMed] [Google Scholar]
- 26.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113:376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 27.Morcuende JA, Egbert M, Ponseti IV. The effect of the Internet in the treatment of congenital idiopathic clubfoot. Iowa Orthop J. 2003;23:83–86. [PMC free article] [PubMed] [Google Scholar]
- 28.Pirani S, Zeznik L, Hodges D. Magnetic resonance imaging study of the congenital clubfoot treated with the Ponseti method. J Pediatr Orthop. 2001;21:719–726. doi: 10.1097/00004694-200111000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Ponseti IV. Treatment of congenital clubfoot. J Bone Joint Surg Am. 1992;74:448–454. [PubMed] [Google Scholar]
- 30.Ponseti IV. Congenital Clubfoot: Fundamentals of Treatment. Oxford, UK: Oxford University Press; 1996. [Google Scholar]
- 31.Ponseti IV. Common errors in the treatment of congenital clubfoot. Int Orthop. 1997;21:137–141. doi: 10.1007/s002640050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ponseti IV. Relapsing clubfoot: causes, prevention, and treatment. Iowa Orthop J. 2002;22:55–56. [PMC free article] [PubMed] [Google Scholar]
- 33.Ponseti IV, Smoley EN. Congenital clubfoot: the results of treatment. J Bone Joint Surg Am. 1963;45:261–275. [Google Scholar]
- 34.Ponseti IV, Zhivkov M, Davis N, Sinclair M, Dobbs MB, Morcuende JA. Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res. 2006;451:171–176. doi: 10.1097/01.blo.0000224062.39990.48. [DOI] [PubMed] [Google Scholar]
- 35.Radler C, Manner HM, Suda R, Burghardt R, Herzenberg JE, Ganger R, Grill F. Radiographic evaluation of idiopathic clubfeet undergoing Ponseti treatment. J Bone Joint Surg Am. 2007;89:1177–1183. doi: 10.2106/JBJS.F.00438. [DOI] [PubMed] [Google Scholar]
- 36.Segev E, Keret D, Lokiec F, Yavor R, Wientroub S, Ezra E, Hayek S. Early experience with the Ponseti method for the treatment of congenital idiopathic clubfoot. Isr Med Assoc J. 2005;7:307–310. [PubMed] [Google Scholar]
- 37.Singh BI, Vaishnavi AJ. Modified Turco procedure for treatment of idiopathic clubfoot. Clin Orthop Relat Res. 2005;438:209–214. doi: 10.1097/01.blo.0000173251.77826.05. [DOI] [PubMed] [Google Scholar]
- 38.Sud A, Tiwari A, Sharma D, Kapoor S. Ponseti’s vs Kite’s method in the treatment of clubfoot—a prospective randomised study. Int Orthop. 2008;32:409–413. doi: 10.1007/s00264-007-0332-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thacker M, Scher D, Sala DA, Bosse HJP, Feldman DS, Lehman WB. Use of the foot abduction orthosis following Ponseti casts: is it essential? J Pediatr Orthop. 2005;25:225–228. doi: 10.1097/01.bpo.0000150814.56790.f9. [DOI] [PubMed] [Google Scholar]
- 40.Tindall AJ, Steinlechner CWB, Lavy CBD, Mannion S, Mkandawire N. Results of manipulation of idiopathic clubfoot deformity in Malawi by orthopaedic clinical officers using the Ponseti method: a realistic alternative for the developing world? J Pediatr Orthop. 2005;25:627–629. doi: 10.1097/01.bpo.0000164876.97949.6b. [DOI] [PubMed] [Google Scholar]