Abstract
This Classic article is a reprint of the original work by Ignacio V. Ponseti and Jeronimo Campos, Observations on Pathogenesis and Treatment of Congenital Clubfoot. An accompanying biographical sketch on Ignacio V. Ponseti, MD, is available at DOI 10.1007/s11999-009-0719-8 and a second Classic article is available at 10.1007/s11999-009-0720-2. This article is ©1972 by Lippincott Williams and Wilkins and is reprinted with permission from Ponseti IV, Campos J. Observations on Pathogenesis and Treatment of Congenital Clubfoot. Clin Orthop Relat Res. 1972;84:50–60.
In the treatment of clubfoot, as in many other orthopedic disorders, the orthopedic surgeon is handicapped because of his ignorance of the primary causes of the deformity. Many scholarly studies blame congenital clubfoot on: abnormal leg muscle development [3], connective tissue genetic defect [22], defective cartilaginous anlage of the anterior part of the talus [16], intra-uterine compression [6], dislocation of the talonavicular joint [5], defect in peroneal muscle innervation [7], defective anterior horn cells [8], abnormal tendon insertions [14, 21], arrest of development [4], tight deltoid ligament [13], etc.
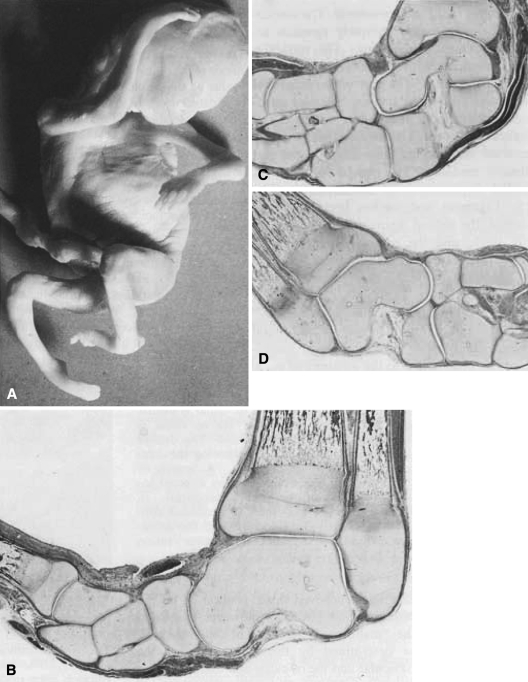
The clubfoot deformity has not been described in embryos, but it has been observed as early as the twelfth gestational week [1]. We studied 6 congenital clubfeet, 2 in a 90-mm-long (crown to rump) male fetus, 2 in a 7-month premature fetus and 2 in a 3-day-old infant. The clubfeet were the only apparent abnormalities in our specimens.
The 90-mm male fetus was thought to be in the seventeenth gestational week and had a bilateral clubfoot deformity, severe on the left and mild on the right (Fig. 1A). Hips and knees were normal. Following removal of the dermis, the leg muscles appeared to be normally developed. The talus was in normal position in the ankle mortise; the other tarsal elements were displaced medially. Serial histologic sections of both legs and feet revealed periosteal and enchondral ossification in the tibia, fibula, metatarsals, and in some phalanges. The other skeletal elements of the foot were formed by cartilage, and their shapes resembled those of normal feet in newborns. Cartilage canals were observed in these elements [10]. Normal foot joint cavities with synovial folds at their margins were apparent. The navicular articulated only with the medial aspect of the head of the talus. The calcaneocuboid joint was directed medially. The joint surfaces were congruent and no gapping was observed. No abnormalities were detected in the joint capsules and ligaments. The deltoid ligament was not unusually thick or fibrotic, and it was slightly folded and not under tension. Tendon insertions were normal. The tibialis posticus branched in the plantar aspect of the foot, sending strong insertions into the navicular, the first cuneiform and the bases of the third and fourth metatarsals. The peroneus longus tendon was also well developed and had a wide insertion into the base of the first metatarsal. The leg and foot muscles were formed by muscle fibers of variable diameter, usually small, cross-striated, with central or peripheral nuclei. All limb muscles appeared to have muscle fibers at similar stages of development (Fig. 1B–D).
Fig. 1A–D.
(A) 90-mm (crown to rump) male fetus with bilateral clubfoot. (B) Frontal section of the left foot showing the talus in the ankle mortise, and the navicular, cuneiforms, and first and second metatarsals displaced medially. The anterior tibial tendon is seen above the navicular. Endochondral ossification is seen in the tibia, fibula and first metatarsal (×15). (C) Frontal section of the left foot taken about 3 mm behind section (B). The anterior and posterior portions of the os calcis are underneath the talus. The navicular articulates with the medial aspect of the head of the talus. The three cuneiforms are to the left and the cuboid is underneath the navicular. The medial ankle ligament is folded (×15). (D) Frontal section of the left foot. The talus is in the ankle mortise. The navicular is medial and the anterior portion of the os calcis is underneath the head of the talus. The deltoid ligament is slightly folded following the contour of the head of the talus. A branch of the posterior tibial tendon is seen directed toward the base of the fourth metatarsal. In (C) and (D) there is a cellular connection between the calcaneus and the navicular suggesting a calcaneonavicular fusion (×15).
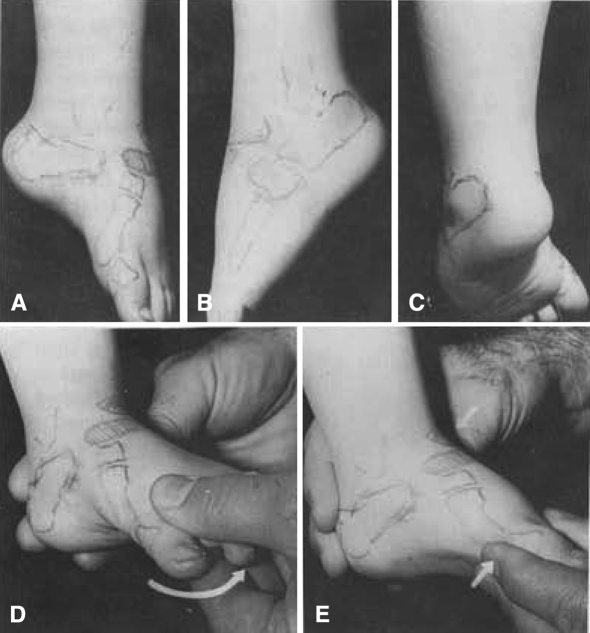
The feet of the 7-month-old fetus and of the 3-day-old infant had similar clubfoot deformities. The body of the talus, although in equinus, was otherwise in normal relationship with the tibia and fibula. The other tarsal bones were in equinus and displaced medially. The neck of the talus angled medially an average of 20° above normal. The navicular tuberosity turned obliquely upwards toward the medial malted us. The navicular articulated only with the medial aspect of the head of the talus. The part of the head that remained uncovered had no articular cartilage and formed a prominence on the dorsal aspect of the foot. The os calcis was severely inverted and the calcaneocuboid joint was directly medially. The cuboid followed the medial displacement of the navicular (Fig. 2). Ligament and tendon insertions were normal, the deltoid ligament was not unusually thick, and the muscles appeared well developed. No abnormalities were observed in the histologic sections obtained only in the 7-month-old fetus.
Fig. 2.

Clubfoot of a 3-day-old infant. The navicular is medially displaced and articulates only with the medial aspect of the head of the talus. The cuneiforms are seen to the right of the navicular and the cuboid is underneath it. The calcaneocuboid joint is directed postero-medially. The anterior two-thirds of the os calcis is seen underneath the talus. The tendons of the arterial tibial, extensor hallucis longus, and extensor digitorum longus are medially displaced.
We found in our dissections what Scarpa [20], Adams [1], and many other authors had found before us. Possibly no fundamental knowledge has been added to the anatomy of club-foot in the past 100 years, and it appears that the cause of this deformity cannot be determined from anatomic observations. Adams in 1866 emphasized the medial angulation of the neck of the talus which he observed in all dissected clubfeet. Recently Irani and Mary Sherman [16] believed this deviation to be the primary fault. Adams, however, regarded the “malformed condition of the astragalus as determined by the malposition of the navicular and the os calcis and that its altered form is evident adaptation to the altered position of these bones.” Scarpa, early in the nineteenth century, asserted that in infants who have not begun to walk “this obliquity of the body of the astragalus is very trifling when compared with that of the other bones of the tarsus.” Together with Adams most authors regard “the altered form of the astragalus as the result rather than the cause of the deformity.” In the same way, changes in muscles, tendons and ligaments observed at birth and believed to cause the deformity are most likely secondary. Not much can be added, to Scarpa’s assertion “that the essence of this congenital deformity of the feet consists in the twisting of the os naviculare, of the cuboids, and of the os calcis, around their smaller axis, into which morbid direction any drawn the cuneiform bones, those of the metatarsus, and of the phalanges of the toes, and that comparatively, the astragalus is the least displaced of all the other bones of the tarsus.” We do not know the cause of these displacements although it has been established that it is partly genetic [23].
The following hypothesis fits most known facts: Eversion of the foot is among the last movements acquired during a normal child’s development [11]. An equinovarus position could possibly develop in a fetus with retarded or weak contractions of the peronei and foot dorsiflexors; since the plantar flexors and invertors are stronger muscles, once established the malposition will not correct spontaneously. It may become fixed if some abnormality in the connective tissue maturation occurs [22]; it will be unyielding at birth in disorders of muscle development (i.e., arthrogryposis) or of innervation (i.e., spina bifida).
In the treatment of clubfoot the orthopedist endeavors to align the tarsal and metatarsal bones in proper position with the leg. The aim is a supple, well-corrected foot; a normal foot is hardly ever obtained. Conservative treatment can only succeed when all foot and leg muscles are well developed and the infant can actively move the foot although tarsal joint motion range is very restricted. Rigid feet in infants with defective or absent muscles will need surgical correction.
Treatment entails correction of the position of the bones and of the curvature profiles of joint surfaces as well as the stretching of ligaments and tendons in the medial and posterior aspects of the foot. The younger the infant, the easier these corrections are. Success requires a thorough knowledge of the deformity and of the functional anatomy of the foot. The following observations bear on treatment:
Movements of the 3 tarsal joints occur simultaneously; therefore, adduction and inversion must be corrected together. Plaster cast wedgings delay correction [17].
There is no fixed axis of rotation for the tarsal joints; rather, these joints with their ligaments are suited for a complex movement around a moving axis [15]. Attempts to tilt the os calcis under the talus on a hypothetical anteroposterior axis of motion [12] fail to correct heel inversion since the articular surfaces and ligaments of the talocalcaneal prevent this motion.
Inversion and adduction of the tarsus is corrected when the os calcis is shifted and turned laterally underneath the talus at the same time that the navicular and cuboid are shifted laterally. The deltoid, the calcaneotalar, and calcaneonavicular ligaments must he stretched. The spring ligament must be lengthened sufficiently to provide room between the sustentaculum tali and the navicular for the head of the talus.
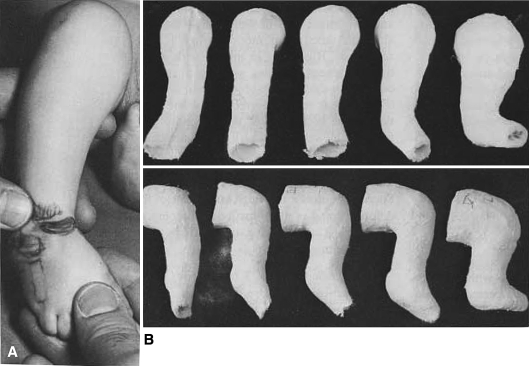
Although the clubfoot is in severe supination, the front part of the foot is everted in relation to the heel (the first metatarsal is plantarflexed to a greater degree than the fifth metatarsal) and this relationship causes the cavus deformity [19]. The cavus is corrected by inverting the forefoot (Fig. 3). The navicular, cuneiforms and metatarsals will thus be placed in straight alignment to form the lever arm needed for the correction of heel inversion (Fig. 4A).
Attempts to correct heel inversion by forcibly everting the forefoot fail, and the cavus deformity increases as the first metatarsal is further plantarflexed [19]. This common maneuver causes false corrections [23].
The lateral shift of the os calcis, navicular, and cuboid in relation to the talus can only be accomplished if the talus is stabilized against rotation. Casts extending to below the knee will allow the leg, and therefore the talus, to rotate and heel inversion will not correct. Plaster casts will have to extend from toe to groin with the knee bent 90° (Fig. 4B).
The equinus is corrected last by dorsiflexing the foot in full valgus. To prevent recurrence of cavus and false correction of heel inversion the metatarsal heads must always be in a plane perpendicular to the leg (Fig. 4B) Correction of a severe equinus is radically shortened by subcutaneous heel-cord sectioning; a rockerbottom deformity and flattening of the superior articular surface of the talus are thus prevented [19].
Fig. 3A–E.
(A–C) Relapsed clubfoot of a 3-year-old boy. The foot is supinated, but the forefoot is too everted in relation with the heel. The first metatarsal is severely plantarflexed while the fifth is in proper relationship with the cuboid and calcaneus. This abnormal relationship between the forefoot and hindfoot causes the cavus deformity. (D) Wrong maneuver to correct the clubfoot. The forefoot is everted, and by plantarflexing the first metatarsal and dorsiflexing the fifth the cavus deformity increases and the heel inversion does not correct. (E) The cavus is corrected by dorsiflexing the inner forefoot, thereby placing it in proper alignment with the hindfoot.
Fig. 4A–B.
(A) Manipulation to correct the right clubfoot of a 6-week-old baby boy. Outward pressure is exerted on the forefoot and counter pressure on the lateral aspect of the head of the talus. The forefoot is never everted; rather, it is displaced laterally as a unit with the midfoot. Heel inversion will correct when the anterior aspect of the os calcis, together with the cuboid and scaphoid, are shifted and turned laterally in relation with the talus. (B) Antero-posterior and lateral views of the toe-to-groin plaster casts used to maintain the corrections obtained by manipulating the left foot of the baby in (A). The plaster casts were changed weekly except for the last one which was left on for 3 weeks. Observe that the forefoot was never everted. No anesthesia was used except to section the heelcords before the application of the fifth plaster cast. The right foot was treated similarly. Well fitting, high-topped shoes attached in 75 degree outward rotation on a 9- inch long steel bar then worn full-time for 3 months, and at night for 6 years.
The bones will remain well aligned when normal curvature profiles of joint surfaces have developed and when normal balance is reached in the pattern and strength of ligaments, tendons, and muscles in the leg and foot. This can be accomplished only gradually through many months of treatment. Denis Browne splints [6] or plaster casts are usually applied following weekly manipulative corrections. In our experience with severe cases false corrections and rockerbottom deformities are more common complications with splints than with casts, probably because the tarsometatarsal joints are much less rigid than the tarsal arid ankle joints. We prefer to control the correction obtained after gentle manipulation with well-molded, thinly padded toe-to-groin plaster casts which are changed every 4–7 days. If the heelcord is sectioned, the last cast is left on for 3 weeks. With proper manipulations and plaster cast technic the initial stage of treatment need not last much longer than 2 months. Joint molding and muscle development can then be accomplished by controlling the corrected position of the feet with a Denis Browne splint with well-fitted high-topped shoes attached in 75° outward rotation. In unilateral cases the shoe on the normal foot is attached in neutral rotation. The splints are left on full time for several months and then are discarded gradually, several hours a day, but remain applied at night for at least 5 or 6 years.
It is difficult to be certain when all components of clubfoot deformity are completely corrected. Although the position of the bones of the foot and their relationship to one another can be identified by palpation, false corrections can go undetected. Roentgenograms are useful to record the initial degree of deformity and to follow its correction. Only the central part of the tarsal elements, however, are ossified in infancy except for the navicular which does not ossify until the second or third year of age. Heel inversion can be estimated by measuring the talocalcaneal angle in anteroposterior roentgenograms [18] but the all-important relationship between the navicular and the head of the talus cannot be determined in the infant. One cannot be sure, therefore, that the correction is adequate. We consider the deformity corrected when the foot can be fully pronated and dorsiflexed. If this is no longer possible in a subsequent visit we believe that the deformity has relapsed.
Relapses, or incomplete correction, of the deformity are common in rigid feet with poor leg muscle development. The orthopedic surgeon cannot influence rigidity of connective tissue, but he can change muscle balance by transferring tendon insertions when necessary and thereby obtain correction in many cases.
The peroneal muscles are of necessity stretched by the deformed position of the foot and appear weaker than the supinators. Following the initial treatment, strength of the peronei and of foot dorsiflexors improve to normal in some children and maintain the foot well corrected. In some cases, however, the peronei remain weak and with a slight recurrence of heel inversion deformity the anterior tibial ceases to be a dorsiflexor and becomes purely a supinator [9]. We treat the first recurrence with manipulation and toe-to-groin plaster casts changed each week for an average of 6 weeks. In most recurrences heel inversion is more resistant to conservative treatment than is equinus. We treat the second recurrence by another series of manipulations and plaster cast applications followed by anterior tibial transfer to the third cuneiform. The Achilles tendon is lengthened when necessary to correct equinus.
Until about 1948 a release of the soft tissues in the medial aspect of the foot [5] was the most commonly performed operation in this clinic for treatment of recurrences or incomplete corrections in severe clubfeet. In a review of the results of treatment in 1963 [19] it was observed that medial release operations often leave extensive scarring and stiffness in the midtarsal joints and that early transfer of the anterior tibial tendon reduced greatly the need for this operation. During the past 20 years anterior tibial transfer has been the preferred operation for the treatment of relapsed foot supination. Bone and joint surgery has been rarely required for the correction of obstinate cases.
The results of anterior tibial transfers to the dorsum of the foot done in this clinic from 1950 to 1960 have been recently evaluated. Four hundred and ninety-one feet in 338 patients were treated during this period. Of these, 73 feet in 42 patients had an anterior tibial transfer. During the past year we have been able to see 34 of these patients with a total of 58 feet operated on. The operations were performed at ages ranging from 6 months to 10 years with an average of 5 years. The follow-up period ranged from 9 to 20 years with an average of 16 years.
The tendon was transferred to the third cuneiform in 43 cases and to the cuboid in 15. The tendon was transferred to its new attachment without changing its position underneath the ankle retinaculum except to provide a straight line of pull. In all cases the tendon was attached to the bone through a drill hole using a Bunnell pull-out suture. The foot was immobilized for 4 weeks in a toe-to-groin plaster cast. In addition to the anterior tibial transfer the Achilles tendon was lengthened in 11 feet; the extensor hallucis longus was recessed to the neck of the first metatarsal in 5 feet; and a medial release operation was done in 4 feet (one of these had already had a medial release operation 4 years earlier). The anterior tibial transferred in 2 feet with persistent supination following astragalectomy done 2 years before. Triple arthrodesis and anterior tibial transfer were done in 2 feet with relapse following medial release operations done 7 years previously.
Persistent or relapsed supination was treated with medial soft-tissue release in 4 feet 1–3 years following the tendon transfer, and one foot had a triple arthrodesis 10 years later. The last foot and one foot of the preceding group had medial release operations at the time of the transfer. The Achilles tendon was lengthened in 11 feet 1–10 years following the transfer. In 2 feet severe planovalgus following transfer of the anterior tibial tendon to the cuboid was treated by retransferring the tendon to the second cuneiform and Grice bone block.
The results were assessed by clinical and roentgenographic examination. We obtained AP and lateral roentgenograms of the feet with the patient standing and lateral roentgenograms with the feet in maximal dorsiflexion and in maximal plantarflexion. All patients are carrying on active lives and have no pain nor complaints referable to their feet. Most of them are or have participated in high school athletics. Clinically the heel was well aligned in 33 feet; it was in 10° of inversion or less in 15 feet and in slight eversion in 10 feet (4 feet of the last group had transfers to the cuboid; 2 of these 4 had retransfers to the second cuneiform and Grice bone block). In all cases the forefoot was well corrected except for 3 feet with 10–20° of adduction. A slight tendency of cock-up deformity in the metatarsophalangeal joint of the big toe was observed in 12 feet. The strength of the transferred anterior tibial was normal in 53, 4+ in 3 feet, and 3+ in the 2 feet with the retransferred tendon. Active ankle dorsiflexion was possible to more than 10° in 32 feet, from 10° to neutral in 21 feet, to 5° of equinus in 3 feet, and to 10° of equinus in 2 feet. Active ankle plantarflexion to more than 20° was seen in 48 patients. Plantarflexion was limited to 15° in 5 patients and to 10° in 5 patients. Subtalar motion was within normal limits in 30 feet, limited to about 50 per cent of normal in 18 feet, and absent in 10 feet.
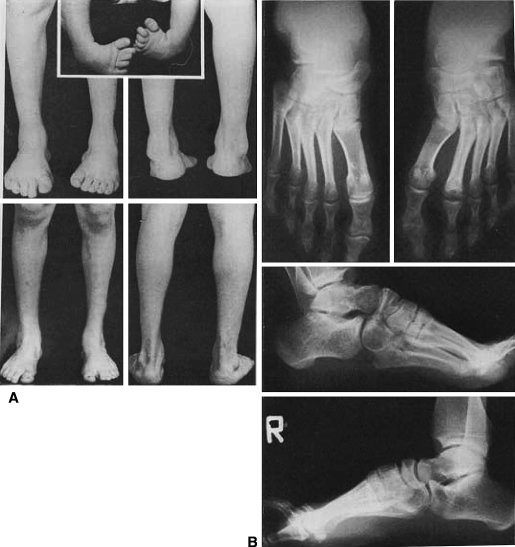
Roentgenograms of these feet rarely show a completely normal foot. Some flattening of the superior articular surface of the talus was observed in 18 cases, and in nearly all there was mild dorso-lateral wedging of the navicular. The navicular was normally aligned with the head of the talus in 33 feet; it was displaced slightly medially in 18 feet and laterally in 7. The talocalcaneal index (the sum of the talocalcaneal angles in the AP and lateral roentgenograms [2]) was within normal limits, from 40 to 85°, in 46 feet and was less than 40° in 12 feet (Figs. 5 and 6).
Fig. 5A–B.
(A) Boy with bilateral clubfoot treated at 2 weeks of age with manipulations and toe-to-groin plaster cast applications weekly until 3 months of age. The left Achilles tendon was sectioned subcutaneously to correct equinus. After the casts the patient wore Denis Browne splints on shoes full-time for 2 months and only at night until 3 years of age when they were discontinued against our advice. The clubfeet at that time were fully corrected. The patient returned at 8 years of age with relapse in both feet, worse on the left than on the right. On the right foot the anterior tibial tendon was transferred to the third cuneiform and the extensor hallucis longus was transferred to the neck of the first metatarsal. On the left foot the anterior tibial tendon was transferred to the third cuneiform following medial soft tissue release and lengthening of the posterior tibial tendon. The Achilles tendon was lengthened bilaterally. At 19 years of age the patient has no complaints and the feet are well aligned. The strength of the transferred anterior tibial is 5 + bilaterally. Subtalar motion is normal on the right and limited to 25 per cent of normal on the left. Ankle dorsiflexion is limited to 10 degrees bilaterally and plantar flexion is free to 25 degrees bilaterally. (B) Standing anteroposterior and lateral roentgenograms. The talocaneal angle is within normal limits on both sides. The naviculars are slightly wedge-shaped bilaterally and the right is medially displaced. The talonavicular joint is slightly narrower on the left than on the right. The left second metatarsal is dense and its head is flat. In the anteroposterior roentgenograms the talco-calcaneal angle is 18 degrees on the right and 20 degrees on the left.
Fig. 6A–C.
(A, top), Boy with right clubfoot treated in infancy by plaster cast applications and tendo-Achillis lengthening in another hospital and first seen by us at 5 years of age. Following manipulation and 3 plaster cast applications, the heel-cord was lengthened again and the anterior tibialis was transferred to the cuboid and the extensor hallucis longus was recessed to the neck of the first metatarsal. (B, bottom), At 19 years of age the right foot is well aligned with normal range of motion in all its joints except for limited ankle dorsiflexion to 10 degrees. The strength of the transferred anterior tibial is 5 +. The circumference of the right calf measures 2 inches less than the left. (C) Standing anteroposterior and lateral roentgenograms show mild supination in both feet. The right navicular is slightly wedge shaped.
This survey suggests that anterior tibial tendon transfer to the third cuneiform is a useful operation for the treatment of severe clubfeet which relapse following conservative treatment. Of the 58 feet surveyed, severe, foot supination recurred in only 5 and in 2 the deformity became grossly overcorrected. Heel inversion was completely corrected in three-fourths of the cases. Half of the cases had normal talar motions. Severe joint stiffness was seen in feet with medial soft-tissue releases. The 2 feet without tali gained good balance. As in all previous studies, for un-known reasons, difficult cases were encountered which yielded only to bone and joint surgery.
Summary
Morphological studies of 6 clubfeet (2 in a 90-mm crown to rump fetus, 2 in a 7-month-old fetus and 2 in a 3-day-old infant) gave no clues to the pathogenesis of this deformity. Anterior tibial tendon transfer to the third cuneiform is a useful operation for the treatment of cases of severe, relapsing clubfoot.
Footnotes
Richard A. Brand MD ✉ Clinical Orthopaedics and Related Research, 1600 Spruce Street, Philadelphia, PA 19103, USA e-mail: dick.brand@clinorthop.org
References
- 1.Adams, W.: Club-foot: Its Causes, Pathology, and Treatment. London, J. and A. Churchill, 1866.
- 2.Beatson TR, Pearson JR. A method of assessing correction in clubfeet. J. Bone Joint Surg. 1966;48B:40. [PubMed] [Google Scholar]
- 3.Bechtol CO, Mossman HW. Club-foot. An embryological study of associated muscle abnormalities. J. Bone Joint Surg. 1950;32A:827. [PubMed] [Google Scholar]
- 4.Böhm, Max: Das menschliche Bein. Deutsche Orthopaedie, Band 9. Stuttgart, Ferdinand Enke, 1935; pp. 56–59, 61–64, 137.
- 5.Brockman EP. Congenital Club-foot (Talipes Equinovarus) New York: William Wood and Co; 1930. pp. 1–59. [Google Scholar]
- 6.Browne D. Talipes equonovarus. Lancet. 1934;ii:969. doi: 10.1016/S0140-6736(00)43841-9. [DOI] [Google Scholar]
- 7.Dittrich RJ. Pathogenesis of congenital club-foot. J. Bone Joint Surg. 1930;12:373. [Google Scholar]
- 8.Durante G, Courtillier L. Atrophic musculaire par regression embryonnaire totale chez un enfant atteint de pied bot paralytique congenital. Bull. Soc. Obst. paris. 1899;2:366. [Google Scholar]
- 9.Garceau GJ, Manning KR. Transposition of the anterior tibial tendon in the treatment of recurrent congenital club-foot. J.Bone Joint Surg. 1947;29:1044. [PubMed] [Google Scholar]
- 10.Gardner E, Gray DJ, O’Rahilly R. The prenatal development of the skeleton and joints of the human foot. J. Bone Joint Surg. 1959;41A:847. [PubMed] [Google Scholar]
- 11.Harris HA. Posture in industry. Lancet. 1942;ii:56. [Google Scholar]
- 12.Hicks, J. H.: The mechanics of the foot. J. Anat. Part I, 87:345; Part II, 88:25, 1953–54.
- 13.Hirsch C. Observations on early operative treatment of congenital club-foot. Bull. Hosp. Joint Dis. 1960;31:173. [PubMed] [Google Scholar]
- 14.Hoffa Albert. Lehrbuch der orthopaedischen Chirurgie. 5. Stuttgart: Ferdinand Enke; 1905. p. 734. [Google Scholar]
- 15.Huson A. Een Ontleedkundin-Functioneel Onderzoek van de Voetwortel. Leiden: Proefschrift; 1961. [Google Scholar]
- 16.Irani RN, Sherman Mary S. The pathological anatomy of clubfoot. J. Bone Joint Surg. 1963;45A:1. [Google Scholar]
- 17.Kite JH. The treatment of congenital club-feet. Surg. Gynecol. Obstet. 1935;61:190. [Google Scholar]
- 18.Kite JH. Principles involved in the treatment of congenital club foot. J. Bone Joint Surg. 1939;21:595. doi: 10.2106/00004623-200309000-00032. [DOI] [PubMed] [Google Scholar]
- 19.Ponseti IV, Smoley EN. Congenital club foot: The results of treatment. J. Bone Joint Surg. 1963;45A:261. [Google Scholar]
- 20.Scarpa, Antonius: A Memoir on the Congenital Club Feet of Children, and on the Mode of Correcting that Deformity. Translated from Italian by J. H. Wishart, Edinburgh, A. Constable and Co., 1818.
- 21.Stewart SF. Club foot: Its incidence, cause and treatment. An anatomical-physiological study. J. Bone Joint Surg. 1951;33A:577. [PubMed] [Google Scholar]
- 22.Wynne-Davies Ruth. Family studies and the cause of congenital club foot. J. Bone Joint Surg. 1964;46B:445. [PubMed] [Google Scholar]
- 23.Wynne-Davies Ruth. Talipes equinovarus. A review of eighty-four cases after completion of treatment. J. Bone Joint Surg. 1964;46B:464. [PubMed] [Google Scholar]