Abstract
Recurrent dynamic and structural deformities following clubfoot surgery are commonly due to residual muscle imbalance from a strong tibialis anterior muscle and weak antagonists. We asked whether subcutaneous tibialis anterior tendon transfer effectively treated recurrent deformities following clubfoot surgery and whether the presence of structural deformities influenced the outcome. The patients were divided into two groups: Group I, dynamic supination deformity only (51 patients, 76 feet); and Group II, dynamic supination with other structural deformities (44 patients, 61 feet). The mean age at surgery was 4.3 years (range, 1.4–10.7 years); the minimum followup was 2 years (mean, 5.2 years; range, 2–12.5 years) for both groups. The results were graded according to our subjective rating system of restoration of muscle balance: good, restoration of muscle balance; fair, partial restoration of muscle balance; and poor, no improvement. The two groups had similar outcomes: in Group I, there were 65 good (87%), 11 fair (13%), and no poor results and in Group II, there were 54 good (88%), seven fair (12%), and no poor results. Our data suggest the tibialis anterior tendon transfer restores muscle balance in recurrent clubfeet; we observed no recurrences. This transfer improves function and may prevent secondary osseous changes. We believe the muscle imbalance supports, at least in part, the neuromuscular etiological aspects of congenital clubfeet.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
One of the most common sequelae of surgical treatment of congenital talipes equinovarus deformities (clubfoot) is dynamic supination from a strong tibialis anterior muscle and weak antagonists, particularly the peroneal and tibialis posterior muscles. It is also a common sequelae following otherwise successful nonoperative treatment with the Ponseti technique [1, 6, 7, 23, 42–45]. Why the tibialis anterior muscle maintains relatively normal function and strength in congenital clubfeet is unknown. Thus, when the child walks the strong tibialis anterior produces dynamic supination. It can also be a contributing factor in cavus deformities, hindfoot varus and forefoot adduction, and other structural deformities, such as rotatory dorsal subluxation of the navicular following surgical treatment [37, 52, 54].
Garceau first described the use of tibialis anterior tendon transfer in recurrent clubfoot deformities [19]. Current treatment methods include transfer of the entire tendon, either subcutaneously beneath the ankle retinaculum [10, 19–21, 31, 36, 38, 43, 45, 50], above the ankle retinaculum to the dorsum or lateral aspect of the midfoot [14] or by a split tibialis anterior tendon transfer [36, 39]. The latter technique was initially as described by Hoffer et al. [26]. In the split transfer, the most medial or cuneiform portion of the tibialis anterior tendon is transferred to the cuboid or peroneus tertius tendon. The same transfers can also be performed during treatment for more severe structural deformities in which dynamic supination or muscle imbalance is a contributing factor. At our institution we have used a technique that transfers the tibialis anterior tendon subcutaneously to the dorsum of the foot, thereby maintaining its position beneath the ankle retinaculum.
We asked whether subcutaneous tibialis anterior tendon transfer was an effective procedure for recurrent deformities following clubfoot surgery and whether the presence of structural deformities influenced the outcome. We also reviewed the current etiologic and histologic findings as a possible explanation why muscle imbalance is so common in children with clubfeet.
Materials and Methods
We retrospectively reviewed the medical records of 122 patients (173 feet) with congenital clubfeet treated by subcutaneous tibialis anterior tendon transfers following other clubfoot surgery between 1986 and 2005. We excluded 27 patients who had less than two years of followup postoperatively following tibialis anterior tendon transfer. The majority of patients were initially treated by the senior author (GHT) with a posteromedial plantar release at approximately 9 months of age [53]. The others had their initial treatment elsewhere with a complete soft tissue release between 6 and 12 months of age. We included no patients who had failed conservative treatment using the Ponseti method. Thus, there were 95 patients (137 feet) meeting our study criteria; 42 patients had bilateral transfers. The mean age at tibialis anterior tendon transfer was 4.3 years (range, 1.4–10.7 years). There were 67 male and 28 female patients. The patients were divided into two groups: Group I, dynamic supination deformity only (51 patients, 76 feet) and Group II, dynamic supination with other structural deformities requiring treatment (44 patients, 61 feet). Additional procedures were based on the preoperative clinical and radiographic assessment of the feet and included repeat posteromedial plantar release, repeat tendo Achilles lengthening, posterior release, plantar release, medial release, and midfoot osteotomy. The minimum followup for the 95 patients was 2 years (mean, 5.2 years; range, 2–12.5 years).
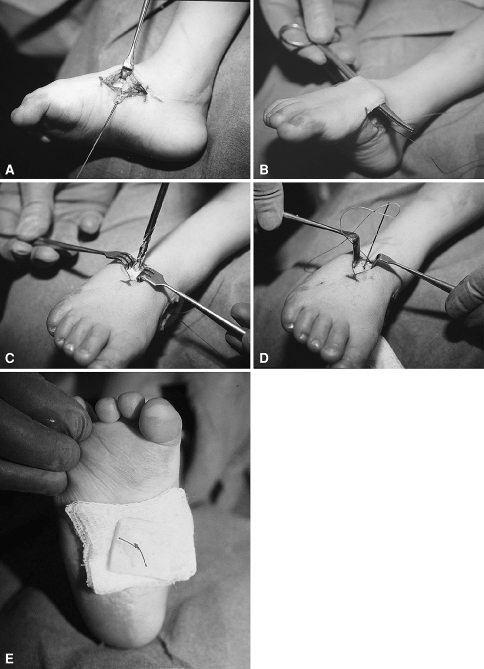
Our surgical technique is relatively simple (Fig. 1A–E). It is similar to that described by Ippolito et al. [31] except that we do not specifically transfer the tendon to the third cuneiform. We believe the ideal age is between 3 and 4 years as this allows enough time to be certain that any early mild dynamic supination will not resolve with maturation of the patient’s gait. The senior author performed all surgery. Under pneumatic tourniquet control, the insertion of the tibialis anterior tendon on the medial aspect of the foot was detached, usually through the previous medial skin incision. It is important to preserve as much length as possible by mobilizing the entire insertion of the tendon. It is also important to mobilize the entire tendon as there can be two or three slips at the insertion site [2]. The tendon was secured by a Krakow stitch using a large 0 or number 1 absorbable suture. This maintained control of the tendon and prevented it from becoming bulbous during transfer. The tendon was dissected proximally to the ankle retinaculum. In some cases there was scar tissue from the previous surgery that was divided. Next, a 2-cm longitudinal incision was made over the dorsum of the midfoot in line with the third metatarsal. Care was taken to mobilize the extensor digitorum brevis muscle and its tendons to expose the capsule of the midfoot. A 5 mm × 5 mm distally based flap of capsule and perichondrium or periosteum was made. This allowed inspection for any midfoot joints. These joints are to be avoided when making the drill hole. A large drill hole, usually 3/8-inch or 32-mm, was made vertically through the midfoot. This hole was usually the same diameter as the tendon and was typically in the second or third cuneiform. Radiographs were not obtained as we place the drill hole in the mid-dorsum at the foot in line with the third metatarsal axis rather than in a specific bone. The opening of the drill hole was widened slightly with a large curette.
Fig. 1A–E.
(A) The tibialis anterior tendon insertion is detached through a medial incision and secured with a Krakow stitch. This allows good control of the tendon for transfer and insertion into bone. (B) A subcutaneous tunnel is created between the dorsal and medial incisions. The plane is above the dorsal fascia, extensor tendons and neuromuscular structures. (C) A drill hole is made through the midfoot. Care is taken to avoid damaging adjacent joint surfaces. The drill point selected should be the same diameter as the tendon. (D) Keith needles are used to pass the sutures through the drill hole and through the plantar surface of the foot. (E) After the tendon has been pulled into the drill hole the sutures are tied over a pad consisting of antibiotic impregnated gauze, gauze sponges, felt and a plastic button. The foot is held in the neutral position as the sutures are pulled taunt and tied.
A subcutaneous tunnel was created between the two incisions. The sutures were then passed from the medial incision to the dorsal incision. The tendon should easily slide laterally to its new position. There is ample space for the tendon to slide beneath the ankle retinaculum. The tendon should have a straight line of pull. We divided any residual bands of scar tissue or vincula. The ends of the sutures were passed through individual Keith needles and then the needles passed through the drill hole. They were kept approximately 1 cm apart and brought out through the plantar surface of the foot. Each needle was passed through a antibiotic petroleum-based gauze, 2 × 2-inch gauze sponges, a felt pad, and then a plastic button. The tendon was pulled into the drill hole. It should easily pass with the foot in a neutral position. The sutures were tightened and tied. The pneumatic tourniquet was deflated, homeostasis achieved, and the two incisions closed. A below-knee weight-bearing cast was applied.
Postoperatively, patients were allowed to weight bear as tolerated. The cast was removed at approximately 6 weeks postoperatively. We used no specific physical therapy. The patients were then followed at 4-month intervals for one year, then 6-month intervals for approximately 2 years and then annually until close to skeletal maturity.
The clinical results were based on our own grading system, which evaluated the restoration of muscle balance and the correction of the dynamic supination and were graded: good, restoration of muscle balance; fair, partial restoration of muscle balance; and poor, no improvement. Good results demonstrated no further dynamic supination. The foot had a smooth dorsiflexion arc of motion. Fair results had improved function but still demonstrated mild dynamic supination on dorsiflexion. A poor result had no improvement. This system has been utilized for over 20 years and is recorded on each outpatient visit. We made no attempt to correlate preoperative and postoperative ankle range of motion or foot radiographs as we were evaluating the results of the tendon transfer alone and not the other procedures; these assessment criteria might not have been affected by tibialis anterior tendon transfer.
Results
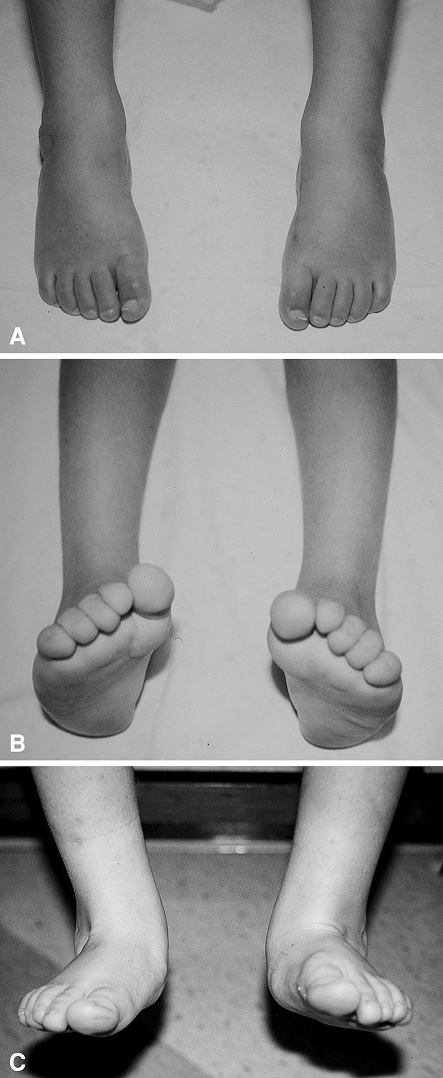
The results of our technique for performing tibialis anterior tendon transfer were similar in both groups. Improved muscle balance is usually immediately apparent following cast removal. As strength in the transferred tibialis anterior muscle is gained over the next 3 to 4 months the results improve further. At last followup 65 feet (87%) in Group I had restoration of muscle balance and were rated good (Fig. 2A–C). There were 11 feet (13%) with fair results and partial restoration of muscle balance; there were no feet with a poor result. In Group II 54 feet (88%) rated good and seven feet (12%) rated fair; there were no poor results.
Fig. 2A–C.
(A) Clinical photograph of a 4-year-old boy 3 years after bilateral posteromedial plantar releases for idiopathic clubfeet. At rest, the feet are straight and well-corrected. (B) When the feet are actively dorsiflexed there is dynamic supination of the feet. This causes him to walk on the lateral aspect of his feet. It produces no symptoms at this time but does result in asymmetrical shoe wear. (C) Two years following tibialis anterior tendon transfer active dorsiflexion procedures a smooth arc of motion without dynamic supination.
There were no postoperative complications in either group such as tendon pull-out, postoperative infections, or neurovascular injuries. There were two late complications in Group II. Two patients (two feet) developed limited plantar flexion due to progressive contracture of the tibialis anterior muscle. They were both treated by a recession of the tibialis anterior musculotendinous junction. This restored plantar flexion to 20°. Both patients and feet had a final rating of good.
Discussion
Recurrent dynamic and structural deformities commonly occur following clubfoot surgery due to residual muscle imbalance from a strong tibialis anterior muscle and weak antagonists. Several techniques have been proposed to minimize or eliminate this imbalance. We asked whether subcutaneous tibialis anterior tendon transfer was an effective treatment for recurrent deformities following clubfoot surgery and whether the presence of structural deformities influenced the outcome.
We acknowledge several limitations. We did not attempt to evaluate the feet in Group II further since they were more complex and the results of the transfer may not have affected their clinical or radiographic results, other than improved muscle balance (dynamic supination). This was only one component of their complex deformity. We evaluated our patients with our own physician-generated scoring system. This system has not been validated against any standard system and would likely be prone to interobserver variability and some recall or dependence on accurate records. However, it is simple and we believe the interobserver variability would be minimal. Finally, we had a minimum followup of two years. Recurrences could occur after that time. However, most patients were well beyond the point where recurrences would likely occur (mean 5.2 years) so we believe there would be few missed recurrences.
Our results confirmed that a subcutaneous transfer of the entire tibialis anterior tendon to the dorsum of the foot in line with the third metatarsal effectively corrects dynamic supination as well as rebalances the foot with more severe residual or recurrent deformities. We performed tibialis anterior tendon transfer in approximately 30% of feet previously treated by a posteromedial plantar release. This has ranged from 20% to 50% in other studies [1, 6, 10, 23, 38, 41, 43–46]. Cooper and Dietz [7] in their 1995 30-year followup study of patients treated by the Ponseti method reported that 38 of 71 feet (54%) underwent a tibialis anterior tendon transfer. Morcuende et al. [42] in a later study from the same institution with a minimum followup of two years reported that only four of 157 patients (3%) treated with the Ponseti technique underwent a tibialis anterior tendon transfer.
The advantages of our technique are its simplicity and that the tendon maintains its normal position beneath the ankle retinaculum. This preserves its normal mechanics and prevents the tendon from bowstringing when the foot is dorsiflexed. The other techniques of transferring the entire tendon or the split transfer involve the tendon being moved anterior to the ankle retinaculum. The tendon, as a consequence, bowstrings when the foot is dorsiflexed. This is cosmetically displeasing and may cause irritation of the overlying skin as it rubs against the shoe. Nevertheless, these transfers are also effective. Kuo et al. [36] in 2001 reviewed 55 patients (71 clubfeet) who had residual dynamic deformities and underwent tibialis anterior tendon transfer. There were 49 feet treated with a full transfer and 29 with a split transfer. Both transfers were brought anterior to the ankle retinaculum. The age of patients at surgery was 6 ± 2.5 years, which was slightly older than our patients. They also included patients who had additional procedures in both groups. This included 12 patients (13 feet) in the full tendon transfer group and five patients (five feet) in the split transfer group. Their results were based on the clinical criteria of Garceau and Palmer [20, 21] ankle and foot range of motion, muscle strength, and radiographic analysis. The clinical criteria of Garceau and Palmer demonstrated the most improvements. Their criteria were based on the presence or absence of metatarsus adductus, heel varus, and equinus. A normal-appearing foot, other than being smaller than the opposite side, was considered an excellent result (4 points), a mild deformity in one or two of the three parameters a good result (3 points), moderate deformity in all three parameters a fair result (2 points), and a severe deformity in all three parameters a poor result (1 point). Using their criteria, preoperatively in the entire tendon transfer group the mean score was 2.6 points (one excellent, 28 good, nine fair, and four poor feet). Postoperatively, this improved to a mean of 3.3 points postoperatively (13 excellent, 28 good, one fair, and no poor feet). In the split transfer group the mean preoperative score was 2.9 points (one excellent, 24 good, four fair, and no poor feet). The mean postoperative score was 3.4 points (11 excellent, 18 good and no fair or poor feet). Thus, there was no difference between the groups using the clinical criteria. The results in their other assessments showed slight improvement in range of motion (dorsiflexion, plantar flexion, inversion, and eversion), muscle strength, and radiographic results. However, there were no statistically significant differences. Kuo et al. concluded both procedures were effective but preferred the split tibialis anterior tendon transfer as they believed it was less likely to result in over connection and that it preserved some inversion function. Hui et al. [27] in 1998 performed biomechanical studies on transferring the entire tibialis anterior tendon and the split tibialis anterior tendon transfer and reported no difference in maximum dorsiflexion between either technique. They also reported the ideal axis for transferring the entire tendon was the third metatarsal axis, as in our technique, and for the split transfer the fourth metatarsal axis. It is important in a split transfer to transfer the cuneiform portion of the insertion laterally to prevent proximal twisting of the musculotendinous junction and to allow for a more direct line of pull of the muscle [17].
Our muscle balance results are similar to those of Kuo et al. [36]. Because of the complexity of the etiology and pathology of clubfeet we elected to evaluate only the muscle balance. We did not evaluate functional or radiographic results.
When our outcomes are compared with those of other studies on tibialis anterior tendon transfer of either the entire tendon above or below the ankle retinaculum or the split transfer, there appear to be no clinical differences despite a variety of assessments [7, 10, 14, 15, 29, 31, 39, 46]. This includes feet with dynamic supination and those with structural abnormalities requiring more extensive procedures performed concomitantly. This continues to raise the question of why the tibialis anterior muscle remains relatively normal while its antagonists are functionally weaker. This allows the tibialis anterior muscle to produce dynamic supination in some feet and contribute the recurrent structural deformities in others. It has been suggested that the etiology of clubfoot is neuromuscular in origin and has genetic implications [4, 8, 9, 11, 13, 40, 41, 47].
The second purpose of our study was to review the literature regarding the current etiologic and histologic data that may help explain why muscle imbalance, especially the tibialis anterior muscle, is so common in congenital clubfeet. Recent biopsy studies of the extrinsic muscles of the calf during clubfoot surgery have demonstrated fiber type disproportion, reduction in the number of muscle fibers, increased neuromuscular junctions, and electron microscopic abnormalities [22, 24, 33]. The normal ratio of type I to type II fibers is 1:2 but in clubfeet the relationship is approximately 7:1. There are also collagen [12, 18], myoblast [18], and occasionally arterial abnormalities [51] in children with clubfeet. These findings are in contrast to previous etiological theories suggesting malformation of the talus was the primary abnormality [32, 48, 49]. These observations help explain the physical findings in older children such as calf atrophy, smaller foot, and lower extremity length discrepancy. The documented muscle weakness, especially of the peroneals, tibialis posterior, and the foot dorsiflexors clinically support these histopathologic changes [45]. Feldbrin et al. [16] in 1995 performed electrophysiological studies on both legs of 52 children from 3 months to 15 years of age with idiopathic clubfeet. The studies included electromyography (EMG), nerve conduction studies (NCT), and spinal monosynaptic reflex (H-reflex). They reported numerous pathological findings in feet treated both conservatively and surgically. They believed their data supported the theory of muscle imbalance as an etiological factor. Ezra et al. [14] in 2000 reported evidence of peroneal muscle weakness by electrophysiological testing in 37 feet (25 patients) treated by tibialis anterior tendon transfer. They believed dynamic supination was due to muscle imbalance. However, Bill and Versfeld [5] were not able to demonstrate naturopathic or myopathic changes in the extrinsic muscles in 25 children with untreated clubfeet undergoing conventional EMG.
Herceg et al. [25] in 2006 in a study of 95 feet (68 patients) reported no evidence of a neuromuscular etiology in idiopathic clubfeet: biopsies of numerous muscles, with the major exception being the peroneal muscles, revealed only four feet with fiber type disproportion and 55 with muscle fiber atrophy. The importance of the peroneal muscles, especially the peroneus brevis, in clubfeet was documented in the study by Loren et al. [41] in 1998. They performed biopsies of the peroneus brevis in 64 feet. Fifty percent of their specimens demonstrated abnormal muscle histology (fiber size variation and fiber type disproportion). There was an increase in recurrent deformities in these feet compared to those with normal histology. It is interesting that this evidence is within the range of recurrence for initial operative and nonoperative treatment (Ponseti method). Karol et al. [34] studied gait analysis and muscle strength in 23 children (23 feet) with surgically treated unilateral clubfeet at a mean of 10 years postoperatively. They reported no clinically important weakness of the tibialis anterior muscle in 15 patients (65%), while in five patients it was rated weak and was unknown or inconclusive in two patients. The other muscles tested included the gastrosoleus, quadriceps, and hamstrings. The peroneal muscle strength was not analyzed but there were EMG abnormalities in the peroneus longus, brevis, or both in 21 feet (91%). None of these patients were reported to have dynamic supination.
Ippolito and Ponseti [30] in 1980 proposed a theory of retraction fibrosis of the distal muscles of the calf and the supporting connective tissue. In their study of five clubfeet and three normal feet from aborted fetuses they observed decrease in size and number of muscle fibers in the distal third of the muscles on the posteromedial aspect of the leg; increased fibrous connective tissue within the muscles, tendon sheaths, and adjacent fascia; and shortening of the triceps surae. They also serially sectioned the spinal cord from a 17-week old fetus with clubfoot and reported it histologically normal. They concluded clubfeet were not secondary to neuromuscular defects. These findings were not confirmed in a later study by Khan et al. [35].
Zimny et al. [54] in 1985 performed an electron microscopic study of the fascia from the medial and lateral sides of clubfeet and found myofibroblast cells in the medial side which they suggested may have contributed to the soft tissue contractures. Ionasescu et al. [28] reported a correlation between the pattern of protein synthesis and the severity of the contractures. Collagen synthesis was higher in the more severe clubfeet.
Arterial abnormalities can also occur in clubfeet. Sodre et al. [51] in 1990 demonstrated abnormal vascular patterns with hypoplasia or premature termination of the anterior tibial artery. These vascular abnormalities may have a relationship to the associated dysplasia since these vessels supply the talus and dorsal lateral part of the foot. Dietz et al. [12] performed a morphometric study of the tendon sheaths of the anterior and posterior tibial tendons of four clubfeet and two normal feet. They found the clubfeet had fewer cells and cytoplasmic volume in its posterior tibial tendon sheath when compared to its anterior tibial tendon sheath. This was reversed in the normal foot. They presumed this was evidence of a regional growth disturbance.
The neuropathic abnormalities of fiber type disproportion, increased neuromuscular junctions, electron microscopic abnormalities combined with abnormal collagen synthesis, and increased connective tissue in adjacent tendon sheaths, capsules, and ligaments are similar to the changes reported in arthrogryposis multiplex congenita [3]. Although the work by Ippolito and Ponseti [30] demonstrated anterior horn cells were present in the lower portion of the spinal cord of a single aborted human fetus with a clubfoot, this does not conclusively prove that some form of an anterior horn cell defect is not present. Banker [3] feels that all the anterior horn cells must be counted and compared to a normal spinal cord of the same age in order to rule out this possibility. Most likely, there will be a small percentage diminution in the number of cells. It will not be as simple as the gross presence or absence of anterior horn cells.
The neuromuscular etiological concepts in congenital clubfeet yield important information regarding recurrent deformities, especially dynamic supination with or without other structural deformities. For unknown reasons the tibialis anterior muscle appears generally spared while its antagonists, particularly the peroneal muscles, are abnormal in 30% to 50% of patients with clubfeet. This appears to be a major factor leading to dynamic supination. Thus, tibialis anterior tendon transfer by a variety of techniques can be anticipated in a substantial number of children and based on the literature is an effective method of treatment. Our technique is simple, biomechanically advantageous, and effective in restoring muscle balance.
Acknowledgments
We thank PariAnne Fatica in her transcription and correspondence regarding this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abdelgawad AA, Lehman WB, Bosse HJ, Scher DM, Sala DA. Treatment of idiopathic clubfoot using the Ponseti method: minimum 2-year follow-up. J Pediatr Orthop B. 2007;16:98–105. doi: 10.1097/BPB.0b013e32801048bb. [DOI] [PubMed] [Google Scholar]
- 2.Arthornthurasook A, Gew IK. Anterior tibial tendon insertion: an anatomical study. J Med Assoc. Thailand. 1990;73:692–696. [PubMed] [Google Scholar]
- 3.Banker BQ. Neuropathic aspects of arthrogryposis multiplex congenita. Clin Orthop Relat Res. 1972;84:71–78. doi: 10.1097/00003086-197205000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Barker S, Chesney D, Miedzybrodzka Z, Maffulli N. Genetics and epidemiology of idiopathic congenital talipes equinovarus. J Pediatr Orthop. 2003;23:265–272. doi: 10.1097/00004694-200303000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Bill PL, Versfeld GA. Congenital clubfoot. An electromyographic study. J Pediatr Orthop. 1982;2:139–142. doi: 10.1097/01241398-198202020-00004. [DOI] [PubMed] [Google Scholar]
- 6.Changulani M, Garg NK, Rajagopal TS, Bass A, Nayagam SN, Sampath J, Bruce CE. Treatment of idiopathic club foot using the Ponseti method. Initial experience. J Bone Joint Surg Br. 2006;88:1385–1387. doi: 10.1302/0301-620X.88B10.17578. [DOI] [PubMed] [Google Scholar]
- 7.Cooper DM, Dietz F. Treatment of idiopathic clubfoot. A thirty-year follow-up note. J Bone Joint Surg Am. 1995;77:1477–1489. doi: 10.2106/00004623-199510000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Cowell HR, Wein BK. Current concepts review Genetic aspects of clubfoot. J Bone Joint Surg Am. 1980;62:1381–1384. [PubMed] [Google Scholar]
- 9.Dietz F. The genetics of idiopathic clubfoot. Clin Orthop Relat Res. 2002;401:39–48. doi: 10.1097/00003086-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Dietz FR. Treatment of a recurrent clubfoot deformity after initial correction with the Ponseti technique. Instr Course Lect. 2006;55:625–629. [PubMed] [Google Scholar]
- 11.Dietz FR, Cole WG, Tosi LL, Carroll NC, Wemer RD, Comstock D. A search for the gene(s) predisposing to idiopathic clubfoot. Clin Genet. 2005;67:361–362. doi: 10.1111/j.1399-0004.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dietz FR, Ponseti IV, Buckwater JA. Morphometric study of clubfoot tendon sheaths. J Pediatr Orthop. 1983;3:311–318. doi: 10.1097/01241398-198307000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Ester AR, Tyerman G, Wise CA, Blanton SH, Hecht JT. Apoptotic gene analysis in idiopathic talipes equinovarus (clubfoot) Clin Orthop Relat Res. 2007;462:32–37. doi: 10.1097/BLO.0b013e318073c2d9. [DOI] [PubMed] [Google Scholar]
- 14.Ezra E, Hayek S, Gilai AN, Khermosh O, Weintraub S. Tibialis anterior tendon transfer for residual dynamic supination deformity in treated clubfeet. J Pediatr Orthop B. 2000;9:207–211. doi: 10.1097/01202412-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Farsetti P, Caterini R, Mancini F, Potenza V, Ippolito E. Anterior tibial tendon transfer in relapsing congenital clubfoot: long-term follow-up study of two series treated with a different protocol. J Pediatr Orthop. 2006;26:83–90. doi: 10.1097/01.bpo.0000188999.21427.fb. [DOI] [PubMed] [Google Scholar]
- 16.Feldbrin Z, Gilai AN, Erza E, Khermosh O, Kramer U, Weintroub S. Muscle imbalance in the aetiology of idiopathic club foot: an electromyographic study. J Bone Joint Surg Br. 1995;77:596–601. [PubMed] [Google Scholar]
- 17.Fennell CW, Phillips P., III Redefining the anatomy of the anterior tibial tendon. Foot Ankle. 1994;15:396–399. doi: 10.1177/107110079401500709. [DOI] [PubMed] [Google Scholar]
- 18.Fukuhara K, Schollmeier G, Uhthoff HK. The pathogenesis of club foot. A histomorphometric and immuno-chemical study of fetuses. J Bone Joint Surg Br. 1994;76:450–457. [PubMed] [Google Scholar]
- 19.Garceau GJ. Anterior tibial tendon transposition in recurrent congenital club-foot. J Bone Joint Surg Am. 1940;22:932–936. [PubMed] [Google Scholar]
- 20.Garceau GJ. Anterior tibial tendon transfer for recurrent clubfoot. Clin Orthop Relat Res. 1972;84:61–65. doi: 10.1097/00003086-197205000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Garceau GJ, Palmer RM. Transfer of the anterior tibial tendon for recurrent club foot. A long-term follow-up. J Bone Joint Surg Am. 1967;49:207–231. [PubMed] [Google Scholar]
- 22.Gray DH, Katz JM. A histochemical study of muscle in clubfoot. J Bone Joint Surg Br. 1981;63:417–423. doi: 10.1302/0301-620X.63B3.7263758. [DOI] [PubMed] [Google Scholar]
- 23.Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007;89:487–493. doi: 10.2106/JBJS.F.00169. [DOI] [PubMed] [Google Scholar]
- 24.Handelsman J, Badalamente MA. Neuromuscular studies in clubfoot. J Pediatr Orthop. 1981;1:23–31. doi: 10.1097/01241398-198101010-00004. [DOI] [PubMed] [Google Scholar]
- 25.Herceg MB, Weiner DS, Agamanolis DP, Hawk D. Histologic and histochemical analysis of muscle specimens in idiopathic talipes equinovarus. J Pediatr Orthop. 2006;26:91–93. doi: 10.1097/01.bpo.0000188994.90931.e8. [DOI] [PubMed] [Google Scholar]
- 26.Hoffer MM, Reiswig JA, Garrett AM, Perry J. The split anterior tibial tendon transfer in the treatment of spastic varus hindfoot of childhood. Orthop Clin North Am. 1974;5:31–38. [PubMed] [Google Scholar]
- 27.Hui JHP, Goh JHC, Lee EH. Biomechanical study of tibialis anterior tendon transfer. Clin Orthop Relat Res. 1998;349:249–255. doi: 10.1097/00003086-199804000-00031. [DOI] [PubMed] [Google Scholar]
- 28.Ionasescu V, Maynard JA, Ponseti IV, Zelleweger H. The role of collagen in the pathogenesis of idiopathic club foot. Biochemical and electron microscopic correlations. Helv Paediatr Acta. 1974;29:305. [PubMed] [Google Scholar]
- 29.Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am. 2003;85:1286–1294. doi: 10.2106/00004623-200307000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Ippolito E, Ponseti IV. Congenital clubfoot in the human fetus. A histological study. J Bone Joint Surg Am. 1980;62:8–22. [PubMed] [Google Scholar]
- 31.Ippolito E, Ricciardi-Pollini PT, Tudisco C, Ronconi P. The treatment of relapsing clubfoot by tibialis anterior transfer underneath the extensor retinaculum. Ital J Orthop Traumatol. 1985;11:171–177. [PubMed] [Google Scholar]
- 32.Irani RN, Sherman MS. The pathological anatomy of idiopathic clubfoot. Clin Orthop Relat Res. 1972;84:14–20. doi: 10.1097/00003086-197205000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Isaacs H, Handelsman JE, Badenhorst M, Pickering A. The muscles in club foot–a histological, histochemical and electron microscopy study. J Bone Joint Surg Br. 1977;59:465–472. doi: 10.1302/0301-620X.59B4.925057. [DOI] [PubMed] [Google Scholar]
- 34.Karol LA, Concha MC, Johnston CE., 2nd Gait analysis and muscle strength in children with surgically treated clubfeet. J Pediatr Orthop. 1997;17:790–795. doi: 10.1097/00004694-199711000-00018. [DOI] [PubMed] [Google Scholar]
- 35.Khan AM, Ryan MG, Gruber MM, Haralabatos SP, Badalamente MA. Connective tissue structures in clubfoot: a morphologic study. J Pediatr Orthop. 2001;21:708–712. doi: 10.1097/00004694-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Kuo KN, Hennigan SP, Hastings ME. Anterior tibial transfer in residual dynamic clubfoot deformity. J Pediatr Orthop. 2001;21:35–41. doi: 10.1097/00004694-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Kuo KN, Jansen LD. Rotatory dorsal subluxation of the navicular: a complication of clubfoot surgery. J Pediatr Orthop. 1998;18:770–774. doi: 10.1097/00004694-199811000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am. 1980;62:23–31. [PubMed] [Google Scholar]
- 39.Laville JM, Bussieres F. Role of Cahuzac’s operation in clubfoot varus equina revision surgery [in French] Rev Chir Orthop Reparatrice Appar Mot. 1998;84:638–645. [PubMed] [Google Scholar]
- 40.Lochmiller C, Johnston D, Scott A, Risman M, Hecht JT. Genetic epidemiology study of idiopathic talipes equinovarus. Am J Med Genet. 1998;79:90–96. doi: 10.1002/(SICI)1096-8628(19980901)79:2<90::AID-AJMG3>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 41.Loren GJ, Karpinski NC, Mubarak SJ. Clinical implications of clubfoot histopathology. J Pediatr Orthop. 1998;18:765–769. doi: 10.1097/00004694-199811000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113:376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 43.Ponseti IV. Current concepts review. Treatment of congenital club foot. J Bone Joint Surg Am. 1992;74:448–454. [PubMed] [Google Scholar]
- 44.Ponseti IV. Congenital clubfoot: fundamentals of treatment. New York, NY: Oxford Medical Publications; 1996. p. 84. [Google Scholar]
- 45.Ponseti IV, Campos J. Observations on pathogenesis and treatment of congenital club foot. Clin Orthop Relat Res. 1972;84:50–60. doi: 10.1097/00003086-197205000-00011. [DOI] [PubMed] [Google Scholar]
- 46.Ricciardi-Pollini PT, Ippolito E, Tudisco C, Farsetti P. Congenital clubfoot: results of treatment of 54 cases. Foot Ankle. 1984;5:107–117. doi: 10.1177/107110078400500303. [DOI] [PubMed] [Google Scholar]
- 47.Roye DP, Jr, Roye BD. Idiopathic congenital talipes equinovarus. J Am Acad Orthop Surg. 2002;10:239–248. doi: 10.5435/00124635-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Settle GW. The anatomy of congenital talipes equinovarus. Sixteen dissected specimens. J Bone Joint Surg Am. 1963;45:1341–1354. [PubMed] [Google Scholar]
- 49.Shapiro F, Glimcher MJ. Gross and histological abnormalities of the talus in congenital Clubfoot. J Bone Joint Surg Am. 1979;61:522–530. [PubMed] [Google Scholar]
- 50.Singer M, Fripp AT. Tibialis anterior transfer in congenital club foot. J Bone Joint Surg Br. 1958;40:252–255. doi: 10.1302/0301-620X.40B2.252. [DOI] [PubMed] [Google Scholar]
- 51.Sodre H, Bruschini S, Mestriner LA, Miranda F, Jr, Levinsohn EM, Packard DS, Jr, Crider RI, Jr, Schwartz R, Hootnick DR. Arterial abnormalities in talipes equinovarus as assessed by angiography and the doppler technique. J Pediatr Orthop. 1990;10:101–104. [PubMed] [Google Scholar]
- 52.Tarraf YN, Carroll NC. Analysis of the components of residual deformity in clubfeet presenting for reoperation. J Pediatr Orthop. 1992;12:207–216. doi: 10.1097/01241398-199203000-00011. [DOI] [PubMed] [Google Scholar]
- 53.Thompson GH, Richardson AB, Westin GW. Surgical management of resistant congenital talipes equinovarus deformities. J Bone Joint Surg Am. 1982;64:652–665. [PubMed] [Google Scholar]
- 54.Zimny ML, Willig SJ, Roberts JM, D’Ambrosia RD. An electron microscopic study of the fascia from the medial and lateral sides of clubfoot. J Pediatr Orthop. 1985;5:577–581. doi: 10.1097/01241398-198509000-00014. [DOI] [PubMed] [Google Scholar]