Abstract
Objectives
Little is known about the effectiveness of therapeutic massage, one of the most popular complementary medical treatments for neck pain. A randomized controlled trial was conducted to evaluate whether therapeutic massage is more beneficial than a self-care book for patients with chronic neck pain.
Methods
Sixty-four such patients were randomized to receive up to 10 massages over 10 weeks or a self-care book. Follow-up telephone interviews after 4, 10, and 26 weeks assessed outcomes including dysfunction and symptoms. Log-binomial regression was used to assess whether there were differences in the percentages of participants with clinically meaningful improvements in dysfunction and symptoms (i.e., > 5 point improvement on the Neck Disability Index (NDI); > 30% improvement from baseline on the symptom bothersomeness scale) at each time point.
Results
At 10 weeks, more participants randomized to massage experienced clinically significant improvement on the NDI (39% vs. 14% of book group; RR= 2.7; 95% confidence interval (CI) = 0.99–7.5) and on the symptom bothersomeness scale (55% vs. 25% of book group; RR=2.2; 95% CI=1.04–4.2). After 26 weeks, massage group members tended to be more likely to report improved function (RR=1.8; 95% CI=0.97–3.5), but not symptom bothersomeness (RR=1.1; 95% CI=0.6–2.0). Mean differences between groups were strongest at 4 weeks and not evident by 26 weeks. No serious adverse experiences were reported.
Conclusions
This study suggests that massage is safe and may have clinical benefits for treating chronic neck pain at least in the short term. A larger trial is warranted to confirm these results.
Introduction
Neck pain is a common health problem in the United States and other developed countries. It has been estimated that about 70% of adults are afflicted by neck pain at some time in their lives,1,2 10 to 40% of adults are bothered by neck pain each year,3 10 to 15% of adults report neck pain that has persisted more than 6 months in the past year, 2 and 5% of adults are currently experiencing disabling neck pain.1 Although a multiplicity of options are available for treating neck pain, little solid evidence exists to guide clinicians and patients regarding the most effective treatments. Standard medical practice employs rest, medication, physical medicine modalities, and education.4,5 Medications, especially non-steroidal anti-inflammatories, and referral for physiotherapy were the most common treatments used by general practitioners in a recent study of how primary care physicians diagnose and treat patients with chronic neck pain.6 Neck pain is the second most common condition for which complementary and alternative medical (CAM) therapies are used.7 In the US, chiropractic and massage are the most commonly used CAM therapies for neck pain.7 Almost 1 in 4 chiropractic visits and 1 in 5 massage visits are for neck symptoms.8–10 Although therapeutic massage is one of the most popular CAM treatments for neck pain, few studies have evaluated its effectiveness for this condition and we found no studies that actually studied massage as it is commonly practiced in the US. We therefore conducted this exploratory pragmatic clinical trial in a primary care population to evaluate the value of therapeutic massage as a treatment for chronic neck pain.
Materials and Methods
Study Design and Setting
This randomized, parallel-group trial compared the effectiveness and safety of therapeutic neck massage with a self-care book for patients whose neck pain had persisted at least 12 weeks. The study was conducted at Group Health, a nonprofit, integrated healthcare system serving approximately 500 000 enrollees in Washington State and Idaho. The institutional review board at Group Health approved the study protocol. All study participants gave informed oral consent before eligibility screening and informed written consent before the baseline interview and randomization.
Participants
Between March and July, 2004, Group Health enrollees between 20 and 64 years of age who had received primary care for neck pain at least three months prior were mailed a letter describing the study. Patients who returned statements of interest were telephoned by a research assistant who assessed their eligibility for the study. After eligible and interested patients signed consent forms, interviewers telephoned them again to collect baseline data and randomize them to treatment group.
Potential participants were excluded if they 1) had neck pain likely due to a non-mechanical cause (e.g., metastatic cancer, fractured vertebrae, spinal stenosis); 2) had complex neck pain or neck pain potentially inappropriate for massage (cervical radiculopathy, prior neck surgery, litigation for neck pain, motor vehicle accident within past three months); 3) had unstable serious medical or psychiatric conditions or dementia; 4) had minimal neck pain (rating of less than 3 on 0 to 10 point bothersomeness scale) or had had neck pain lasting less than 12 weeks; 5) were currently receiving other treatments for neck pain apart from medications; 6) had used massage for neck pain within the last year; or 7) could not speak or understand English.
Randomization
Using a computer program with variable block sizes of four or six, treatment assignments were randomly generated and placed in opaque, sequentially numbered envelopes by a researcher not involved in patient recruitment or randomization. The envelopes were stored in a locked filing cabinet until needed for randomization.
Treatments
Participants in the trial retained access to the medical care available as part of their insurance benefits. Those randomized to massage received up to 10 massage treatments over a 10-week period, with the exact number of visits based on each participant’s clinical progress as determined by the massage therapist, based on their findings and the comments of the participant. Massage treatments were provided without cost to the study participants. Nine licensed massage practitioners with at least 5 years of experience (median =7.5 years) who were members of a network of CAM practitioners provided the treatments in their private offices. Participants were assigned a massage therapist according to geographic location and schedule availability. The massage protocol permitted a variety of commonly used Swedish and clinical massage techniques and allowed massage therapists to make typical self-care recommendations, such as to exercise or to drink more water and is described in detail elsewhere.11
Participants randomized to the self-care group were mailed a copy of What to Do for a Pain in the Neck by Jerome Schofferman, MD.12 This book includes information on potential causes of neck pain, neck-related headaches, whiplash, recommended strengthening exercises, body mechanics and posture, conventional treatment, complementary therapies for neck pain, and first aid for intermittent flare-ups. No additional instruction about using the book was provided.
Outcome Measures
At baseline and 4, 10 and 26 weeks after randomization, participants were interviewed by telephone interviewers unaware of treatment group. Participants received $5 for completing the 10 week interview and $10 for completing the 26 week interview. In addition to assessing the primary and secondary outcomes, the baseline telephone interview asked about sociodemographic characteristics, neck pain history and the current episode, health status and knowledge of and expectations about the helpfulness of massage and self-care education.
Our primary outcomes were neck related disability and symptom bothersomeness. The Neck Disability Index (NDI), a 10-item (0 to 50 point or 0 to 100 percentage point) questionnaire that has high internal consistency and test-retest reliability,13 was used to measure neck-related disability. An eleven point (0 to 10) numerical rating scale was used to assess how bothersome participants felt their neck pain had been in the previous week. A similar measure showed good construct validity in earlier research for back pain.14 These outcomes were evaluated as both continuous and dichotomous variables. For the dichotomous variables, improvement was defined as a decrease of five or more points on the NDI or a decrease of 30 percent or more on the bothersomeness scale. The cut points for the NDI values have been previously shown to be most strongly associated with patients’ global rating of their improvement (i.e., “better or much better” compared with no improvement). 15
Secondary outcomes included a newer measure of neck pain disability, the Copenhagen Neck Functional Disability Scale,16 general health status as assessed by the Short Form-36,17 degree of restricted activity as indicated by patient responses to two questions,18 use of medications in the last week, and a one-question rating of global improvement. We assessed global improvement by asking participants: “Compared to the neck pain you felt before you began this study, is your neck pain now…” completely gone, much better, better, a little better, about the same, a little worse, or much worse. We also collected self-reported information on all treatments used for neck pain during the study period. After all other outcome data were collected at the 10-week interview, we asked participants receiving massage about adverse experiences. Specifically, we asked participants: “Do you believe there was anything about your massage treatments that caused you to feel significant discomfort, pain or harm” and if they replied yes, to explain what happened.
Statistical Analysis
The study was designed to have 80% power to detect an effect size of 0.75 with a two-sided α of 0.05. Intention to treat analyses were used. Baseline characteristics were compared between groups with the use of chi-square tests for binary variables, t-tests for comparing means of continuous variables, and the Mann Whitney U test for comparing distributions of ordinal variables. Continuous outcome variables were analyzed using linear regression, and dichotomous outcome variables were analyzed using log-binomial regression. We fit regression models using generalized estimating equations19 with an exchangeable correlation structure to adjust for possible correlation within patients over the three follow-up time points. We included separate treatment effects for each follow-up time point, and adjusted for the baseline value of the outcome. All P values are two sided with an α of 0.05 used to determine statistical significance.
Results
Patient Recruitment and Follow-up
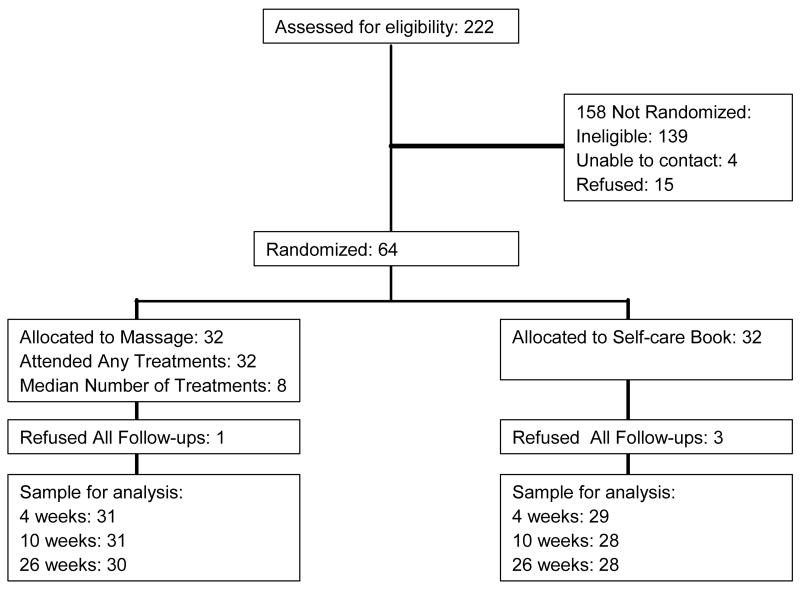
Patients were recruited for the study between March and October, 2004. Among the 222 Group Health enrollees who expressed interest before the recruitment period ended, 64 were randomized, 15 refused, 139 were ineligible and 4 could not be contacted (Figure 1). The most common reasons for ineligibility were neck pain lasting less than 12 weeks (18%), evidence of cervical radiculopathy (16%) and the use of massage for neck pain in past year (14%). Thirty-two participants were randomized to massage and 32 to the self-care book. Follow-up rates exceeded 90% at the 4, 10 and 26-week time points.
Figure 1.
Participant Flow
Baseline Characteristics
The typical study participant was white, female, between 40 and 50 years of age, married, employed, and had attended college (Table 1). The average time since first neck pain was 7.6 years and 81% had had their current episode for at least a year. Few participants reported recent work loss or restricted activity, but more than half had used medications in the previous week, primarily non-steroidal anti-inflammatory medicines. Participants had higher expectations of helpfulness for massage than for self-care.
Table 1.
Baseline Characteristics of 64 Patients with Chronic Neck Pain by Treatment Group
| Treatment Group
|
|||
|---|---|---|---|
| Characteristic | Massage (n= 32) | Book (n=32) | Total (N=64) |
| Age, mean (SD), yr | 47.4 (12.3) | 46.4 (11.3) | 46.9 (11.7) |
| Women, % | 68.8 | 68.8 | 68.8 |
| Attended some college, % | 81.3 | 81.3 | 81.3 |
| White, % | 87.1 | 81.3 | 84.3 |
| Married, % | 78.1 | 59.3 | 68.8 |
| Family income > $35,000/yr | 74.1 | 83.3 | 78.9 |
| Employed or self-employed, % | 84.4 | 84.4 | 84.4 |
| Smoker, % | 9.4 | 6.3 | 7.8 |
| SF-36 Physical Component Score, mean (SD) | 46.0 (5.6) | 44.1 (8.0) | 45.0 (6.9) |
| SF-36 Mental Health Component Score, mean (SD) | 51.9 (7.0) | 53.1 (7.6) | 52.5 (7.3) |
| Years since First Neck Pain Episode, mean (SD) | 7.3 (6.9) | 7.9 (9.4) | 7.6 (8.3) |
| Ever had neck injections, % | 9.3 | 3.1 | 6.3 |
| Pain has lasted > 1yr, % | 80.6 | 80.6 | 80.6 |
| Symptom bothersomeness during the past week (0 – 10 scale), mean, SD | 4.8 (2.3) | 4.9 (1.8) | 4.9 (2.0) |
| Copenhagen Scale (0 to 30 scale), mean (SD) | 9.3 (4.6) | 10.3 (5.7) | 9.8 (5.2) |
| Neck Disability Index (0 to 50 scale), mean (SD) | 14.2 (5.0) | 14.2 (4.7) | 14.2 (4.8) |
| > 1 Work-loss day due to neck pain in past month, % | 0 | 16.7 | 8.2 |
| > 7 days restricted activity due to neck pain in the past month, % | 12.5 | 12.5 | 12.5 |
| Used medication for neck pain in past week, % | 56.3 | 62.5 | 59.4 |
| Taking NSAIDS, % | 46.9 | 53.1 | 50 |
| Taking narcotic analgesics, % | 6.3 | 6.3 | 6.3 |
| Very satisfied with overall care for neck pain, % | 11.1 | 13 | 12 |
| Knowledge about massage, mean (SD) (1 to 5 scale) | 2.3 (1.1) | 2.3 (1.2) | 2.3 (1.1) |
| Median expectation for helpfulness of massage (0 to 10 scale) | 7 | 7.5 | 7 |
| Median expectation for helpfulness of self-care book (0 to 10 scale) | 5 | 5 | 5 |
| Confidence to manage future neck pain by oneself, % strongly agree | 10 | 14 | 12 |
Study Treatments
All participants in the massage group made at least one visit for massage (median of 8, range = 1 to 10, with 79% making 7 or more visits). Visits lasted a median of 75 minutes at the first visit and 60 minutes thereafter. In response to a question about the need for further treatments, massage therapists indicated that 87% of participants were ready to be discharged at the end of the last visit they made.
All practitioners used more than one massage technique at each visit (a median of 7 techniques, with a range of 4 to 15 per visit). The most common techniques used were: kneading (frequently used by all 9 massage therapists); friction (frequently used by 8 therapists) and clinical gliding (frequently used by 7 therapists). Swedish gliding, traction, and trigger point therapy were frequently used by 6 of the therapists. All of the massage therapists reported massaging muscles in the neck, 8 reported massage of the upper back (especially the trapezius muscle), 5 reported massage of other parts of the back, 4 reported massage to the pectoral muscles and another 3 reported massaging the rotator cuff or the arms. Massage to other areas of the body, such as the legs, feet or hands, was less commonly reported.
All the therapists made self-care suggestions to virtually all (94%) of their patients. The most common suggestions were stretching (made by 9 therapists), body awareness (made by 8 therapists) and increasing water intake (made by 7 therapists). Only one massage therapist, who often incorporated acupressure into her treatments, reported being constrained by our protocol, which proscribed acupressure.
All but one participant in the self-care group reported reading at least some of the book, with 85% reporting having read at least one-third of it.
Nonstudy Treatments
During the 10-week intervention, 13% of participants in the massage group versus 21% in the book group reported making visits to non-study healthcare providers for neck pain (p=0.49). Chiropractors (n=4) were the most common healthcare provider seen. Only one participant in the control group received massage. Over the six-month study period, 37% of the massage group and 25% of the self-care group visited a healthcare provider (p=0.40). Primary care providers (n=7), chiropractors (n=7) and massage therapists (n=10) were the most common type of provider visited. Seven participants in the massage group made a visit to a massage therapist after their treatment period had ended compared with three in the control group.
Functional Status and Symptoms
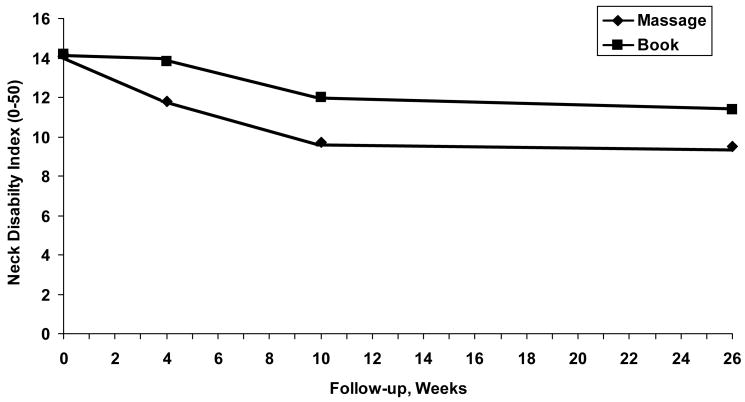
Mean scores on the Neck Disability Index declined more in the massage group than in the self-care group during the first 4 weeks of treatment (Table 2). This initial benefit of massage persisted throughout the 26-week follow-up (Figure 2), although these differences were statistically significant only at 4 weeks (Table 2). We also found that a greater proportion of the massage group than the self-care group reported a clinically meaningful improvement in the Neck Disability Index (i.e., at least 5 points) at 4, 10 and 26 weeks (Table 3). The difference between groups was most pronounced during the 10 weeks of the treatment period.
Table 2.
Mean Score Differences of Bothersomeness and Disability between Treatments at 4, 10 and 26 weeks, Controlling for Baseline Scores*
| Neck Disability Index | Symptom Bothersomeness | |||
|---|---|---|---|---|
| Follow-up Period | Mean Score Difference (95% CI) | P-value | Mean Score Difference (95% CI) | P-value |
| 4 weeks | −2.1 (−4.0 to −0.03) | 0.047 | −1.6 (−2.5 to −0.7) | 0.0006 |
| 10 weeks | −2.3 (−4.7 to 0.15) | 0.066 | −1.2 (−2.5 to 0.1) | 0.081 |
| 26 weeks | −1.9 (−4.4 to 0.63) | 0.14 | −0.14 (−1.5 to 1.2) | 0.84 |
Mean difference and 95% CI are from generalized estimating equation models
Figure 2.
Mean Neck Disability Index scores (0 to 50 points) at baseline, 4, 10, and 26 weeks by treatment group
Table 3.
Relative Risks Associated with Improvement in Disability and Pain for Massage at 4, 10, and 26 Weeks*
| Massage | Book | Relative Risk | 95% CI | P-value | |
|---|---|---|---|---|---|
| Improvement of 5+ points on Neck Disability Index, % | |||||
| 4 weeks | 35 | 7 | 5.1 | (1.2 to 21.3) | 0.023 |
| 10 weeks | 39 | 14 | 2.7 | (0.99 to 7.5) | 0.052 |
| 26 weeks | 57 | 31 | 1.8 | (0.97 to 3.5) | 0.061 |
| Improvement of bothersomeness score by ≥ 30%, % | |||||
| 4 weeks | 48 | 10 | 4.7 | (1.5 to 14.5) | 0.008 |
| 10 weeks | 55 | 25 | 2.1 | (1.04 to 4.2) | 0.038 |
| 26 weeks | 43 | 39 | 1.1 | (0.6 to 2.0) | 0.80 |
| Better or Much Better on Global Rating of Improvement, % | |||||
| 4 weeks | 58 | 7 | 8.5 | (2.0 to 35.4) | 0.003 |
| 10 weeks | 55 | 25 | 2.2 | (1.1 to 4.5) | 0.031 |
| 26 weeks | 43 | 25 | 1.8 | (0.8 to 3.8) | 0.14 |
Relative Risks are from log binomial models that incorporate all follow-up periods
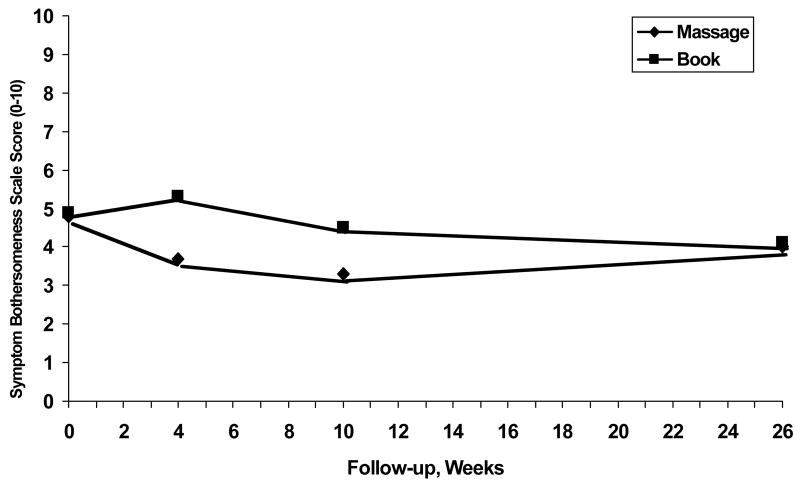
The mean scores for symptom bothersomeness also declined more quickly in the massage group than in the self-care group, but these differences were no longer statistically significant by 10 weeks and virtually disappeared by 26 weeks (Figure 3; Table 2). Similarly, a significantly higher proportion of the massage group reported a clinically meaningful change in the symptom bothersomeness score during the 10-week treatment period, but those differences were attenuated by 26 weeks (Table 3).
Figure 3.
Mean Symptom Bothersomeness scores (0 to 10 points) at baseline, 4, 10, and 26 weeks by treatment group
Secondary Outcomes
The Copenhagen Neck Functional Disability Scale was relatively insensitive to change and showed only modest differences between groups at 4 and 10 weeks (4 weeks: mean score difference (95% confidence interval (CI)) = −1.6 (−3.4 to 0.24); p=0.089; 10 weeks: mean score difference (95% CI) = −0.7 (−2.8 to 0.15); p=0.55). The SF-36 physical and mental health component scores did not differ significantly between groups. Few individuals reported neck -related work loss or restricted activity during the study. Participants in the massage group were more likely to report they were “better” or “much better” on the patient global rating of improvement at all follow-up times, with the greatest between group difference at 4 weeks (Table 3). Medication usage, which was similar at baseline, did not change in the massage group but increased by 14 percentage points in the book group at 26 weeks.
Adverse Experiences
No moderate or severe adverse experiences were reported. Nine patients reported mild adverse experiences, which did not result in disruption of daily activities, that were likely attributable to massage: Five participants reported discomfort or pain during one or more of their massage treatments, three participants reported increased soreness after treatment and one participant, who suffered from migraines, reported nausea for a day after each treatment. One of these participants discontinued treatments because of pain after the first treatment.
Discussion
This study suggests that therapeutic massage has clinically important benefits at least in the short term for persons with chronic neck pain. Our findings are unlikely to be due to other treatments for neck pain, as other treatments were used infrequently in both groups. Nor can the results be attributed to greater medication use in the massage group, because this did not occur. Furthermore, these findings are unlikely due to baseline differences between the groups as the groups were quite similar across a broad range of measures. In this study, the Neck Disability Index was more sensitive to change than the Copenhagen Scale, a finding that has been reported previously.20
Recently, Ezzo21 published a systematic review of 19 trials of massage for mechanical neck disorders. However, 13 of these included massage as part of a multimodal physiotherapy intervention and were unable to tease apart the relative contribution of massage. Moreover, these trials did not describe how much massage was actually administered. Of the 6 “massage-only” trials reviewed, 2 involved only one treatment session and 1 each studied self-administered massage, persons with headache of “cervicogenic origin,” Chinese massage, and Swedish massage. In this last trial, Irnich22 found that compared to acupuncture or sham laser treatment, massage was less likely to result in improvements in motion-related pain. Dysfunction due to neck pain was not measured. The “dose” of massage used in that study (five 30-minute treatments) was substantially less than in the present study. Furthermore, the massage given in the Irnich study does not resemble conventional massage practice in the US, where therapy sessions would be twice as long, provided by a licensed massage therapist, and include a wider range of massage techniques as well as self-care recommendations.10 Thus, none of these previous studies of massage shed light on the usefulness of the type and dose of massage used in this study or included the type of massage received by the general public seeking therapeutic massage for neck pain.
Our findings raise the question of the most clinically useful way to present a study’s results. Typically, studies of treatments for spine pain display results as mean differences between groups (or from baseline). However, such data do not always highlight important clinical differences between groups.23 For example, our dichotomized results for the primary outcomes measures showed stronger benefit for massage than the mean change between groups. Clinicians often characterize patients as having benefited or not from the treatments. Displaying study outcomes as the proportion receiving each treatment who have benefited to a clinically meaningful extent will make the study results easier for clinicians to interpret. One downside of this approach is that if the main study outcomes are dichotomized as improved (to an important extent) or not, the required sample sizes to detect a 10 – 20% difference in the proportion who have improved would usually be larger than that required to detect a mean change equal to the minimum clinically important difference.
Our trial evaluating massage for neck pain was not designed to tease apart the specific effects of soft-tissue manipulation from those attributable to the patient-provider interaction, the home practice recommendations, or expectations of the patient. Thus, our trial cannot shed light on which aspects of the massage experience might have been responsible for the benefits seen. Rather we conducted a more pragmatic trial to evaluate massage for neck pain. There were clearly differences between the two groups regarding patient provider interactions as everyone in the massage group, but only about 1 in 5 persons in the self-care group visited at least one type of health care provider during the intervention period. However, this design is most appropriate for answering clinical questions regarding the benefits of massage therapy for patients with chronic neck pain seen by primary care providers. Reassuringly, the mean scores on the Neck Disability Index were comparable to those of primary care neck pain patients in other therapeutic trials.15,24,25
Nevertheless, our study includes some important methodological strengths, notably a treatment protocol that reflected common practice, a rigorous randomization procedure, good adherence to treatment recommendations, high follow-up rates, and the use of recommended outcome measures administered by interviewers unaware of treatment group. Limitations of this study include modest size, the impossibility of masking people to study treatment (as is generally true of studies of physical treatments), follow-up of less than one year, and the absence of participants with severe neck pain. Despite these limitations, our data suggest that therapeutic massage is helpful in relieving neck pain and dysfunction for a substantial fraction of individuals, at least in the short term. Because some of the exclusion criteria for this study (e.g. exclusion of participants with cervical radiculopathy, prior neck surgery, litigation for neck pain, motor vehicle accident within the past three months, and currently receiving treatments for neck pain apart from medications) may well have eliminated some people who would seek massage therapy for their neck pain in the community, future studies would be required to evaluate the effectiveness of massage in such individuals.
Future studies should investigate the optimal dose of massage including the number of treatments, the frequency of treatments and the length of the treatment period as well as the usefulness of “booster” sessions or self-massaging devices, in extending the time frame for these benefits. Once the treatment is optimized, larger studies should be conducted that include at least one year or longer follow-up period and patients with more severe neck pain. Such studies should include multiple outcome measures, including global rating of improvement, which we found to show an important difference between treatment groups at all follow-up interviews.
Acknowledgments
The authors gratefully thank Marian Wolf Dixon, Diana Thompson and the members of the Massage Therapy Research Consortium for development of the massage protocol, John Ewing, Erica Holden and Christel Kratohvil for assistance in conducting the study and Kristin Delaney for help with data management and analyses. Grant Number R21 AT 001584 from the National Center for Complementary and Alternative Medicine supported this study. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of NCCAM or the NIH.
Sources of Support: This study was supported by Grant Number R21 AT 001584 from the National Center for Complementary and Alternative Medicine.
References
- 1.Cote P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine. 98;23:1689–98. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Makela M, Heliovaara M, Sievers K, Impivaara O, Knekt P, Aromaa A. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 91;134:1356–67. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 3.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine. 94;19:1307–9. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Aker PD, Gross AR, Goldsmith CH, Peloso P. Conservative management of mechanical neck pain: systematic overview and meta-analysis. BMJ. 96;313:1291–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Borenstein DG. Management of neck pain: a primary care approach. Hosp Pract. 98;33:147–50. 153–4, 160. doi: 10.3810/hp.1998.10.113. [DOI] [PubMed] [Google Scholar]
- 6.Borghouts J, Janssen H, Koes B, Muris J, Metsemakers J, Bouter L. The management of chronic neck pain in general practice. A retrospective study. Scand J Prim Health Care. 9917:215–20. doi: 10.1080/028134399750002430. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 98;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 8.Cherkin DC, Deyo RA, Sherman KJ, et al. Characteristics of visits to licensed acupuncturists, chiropractors, massage therapists, and naturopathic physicians. J Am Board Fam Pract. 2002;15 :463–72. [PubMed] [Google Scholar]
- 9.Coulter ID, Hurwitz EL, Adams AH, Genovese BJ, Hays R, Shekelle PG. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine. 2002;27:291–6. 297–8. doi: 10.1097/00007632-200202010-00018. [DOI] [PubMed] [Google Scholar]
- 10.Sherman KJ, Cherkin DC, Kahn J, et al. A survey of training and practice patterns of massage therapists in two US states. BMC Complement Altern Med. 2005;5:13. doi: 10.1186/1472-6882-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherman KJ, Dixon MW, Thompson D, Cherkin DC. Development of a taxonomy to describe massage treatments for musculoskeletal pain. BMC Complement Altern Med. 2006;6:24. doi: 10.1186/1472-6882-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schofferman J. What to do for a Pain in the Neck: The complete program for Neck Pain Relief. New York, NY: Simon and Schuster; 2001. [Google Scholar]
- 13.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–15. [PubMed] [Google Scholar]
- 14.Dunn KM, Croft PR. Classification of low back pain in primary care: using “bothersomeness” to identify the most severe cases. Spine. 2005;30:1887–92. doi: 10.1097/01.brs.0000173900.46863.02. [DOI] [PubMed] [Google Scholar]
- 15.Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck-pain study. Am J Public Health. 2002;92:1634–41. doi: 10.2105/ajph.92.10.1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jordan A, Manniche C, Mosdal C, Hindsberger C. The Copenhagen Neck Functional Disability Scale: a study of reliability and validity. J Manipulative Physiol Ther. 98;21:520–7. [PubMed] [Google Scholar]
- 17.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 18.Riess P. Current estimates from the national health interview survey: United States, 1984. Hyattsville, MD: National Center for Health Statistics; 1986. DHHS publication PHS 86–1584. Vital and health statistics; series 10; no 156. [PubMed] [Google Scholar]
- 19.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 20.Bolton JE. Sensitivity and specificity of outcome measures in patients with neck pain: detecting clinically significant improvement. Spine. 2004;29:2410–7. 2418. doi: 10.1097/01.brs.0000143080.74061.25. [DOI] [PubMed] [Google Scholar]
- 21.Ezzo J, Haraldsson BG, Gross AR, et al. Massage for mechanical neck disorders: a systematic review. Spine. 2007;32:353–62. doi: 10.1097/01.brs.0000254099.07294.21. [DOI] [PubMed] [Google Scholar]
- 22.Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. 2001;322:1574–8. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. BMJ. 1998;316:690–3. doi: 10.1136/bmj.316.7132.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26:788–97. 798–9. doi: 10.1097/00007632-200104010-00020. [DOI] [PubMed] [Google Scholar]
- 25.Hoving JL, Koes BW, de Vet HC, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med. 2002;136:713–22. doi: 10.7326/0003-4819-136-10-200205210-00006. [DOI] [PubMed] [Google Scholar]