Abstract
Atherosclerotic vascular disease is the leading cause of ischemic stroke, resulting in occlusive or severely stenotic lesions of major intracranial or extracranial arteries and narrowing of small penetrating arteries of the brain. Atherosclerosis of the coronary arteries (ie, coronary artery disease) is an indirect cause of cardioembolic stroke secondary to myocardial infarction. Ischemic heart disease may also be complicated by atrial fibrillation and cardioembolic stroke. Prevention of recurrent stroke and other ischemic events, including myocardial infarction, is a key component of treatment for patients with symptomatic ischemic cerebrovascular disease. Prevention of recurrent stroke involves controlling those factors that promote the course of atherosclerosis, including hypertension, hyperlipidemia, diabetes mellitus, and smoking, as well as such local interventions as carotid endarterectomy and endovascular treatment. Nevertheless, administration of antiplatelet agents remains the core of management for preventing recurrent stroke and other cardiovascular events in at-risk patients.
ACE = angiotensin-converting enzyme; AHA = American Heart Association; ARB = angiotensin II receptor blocker; ASA = American Stroke Association; CAD = coronary artery disease; CEA = carotid endarterectomy; ESPRIT = European/Australasian Stroke Prevention in Reversible Ischaemia Trial; ESPS-2 = European Stroke Prevention Study 2; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; PAD = peripheral arterial disease; PRoFESS = Prevention Regimen for Effectively Avoiding Second Strokes; TIA = transient ischemic attack
Stroke is a leading cause of death and disability in the United States. The economic consequences of stroke, including health care costs and lost economic productivity, are substantial. Of the approximately 780,000 strokes that occur annually in the United States, 87% are secondary to brain ischemia.1 Although ischemic stroke and transient ischemic attack (TIA) may be secondary to a broad spectrum of underlying diseases, atherosclerosis is the leading etiologic factor, especially among those aged 50 years or older.2 Disruption of an advanced atherosclerotic plaque may lead to ischemia secondary to thromboembolic occlusions, and occlusion or severe stenosis of an atherosclerotic artery may lead to hypoperfusion of the brain.
In addition to affecting major extracranial (eg, the aorta) and intracranial arteries, atherosclerotic disease affects the smaller penetrating arteries of the brain. Atherosclerotic disease in these smaller arteries may cause lacunar infarctions. Cardiogenic embolism leading to ischemic stroke, most commonly occurring among persons with atrial fibrillation, is often the indirect result of ischemic heart disease secondary to atherosclerosis.
Because of the diffuse nature of atherosclerosis, patients with TIA or stroke often have symptomatic disease or advanced asymptomatic disease affecting the coronary or peripheral arteries. As a result, patients with ischemic neurologic symptoms are also at risk of symptomatic peripheral vascular disease, myocardial infarction, and vascular death.3,4 Thus, managing the underlying atherosclerotic vascular disease is important when treating patients with ischemic cerebrovascular disease and is crucial for preventing recurrent stroke or ischemic events in other arterial sites.5-7 In recognition of the importance of managing atherosclerotic vascular disease, evidence-based guidelines for the treatment of patients with recent stroke or TIA have been developed by the American Heart Association (AHA)/American Stroke Association (ASA) and the American College of Chest Physicians.8-11
For editorial comment, see page 3
MANAGEMENT OF RISK FACTORS FOR ADVANCED ATHEROSCLEROSIS AND ISCHEMIC VASCULAR DISEASE
Some risk factors associated with increased likelihood of advanced atherosclerosis and ischemic disease are not modifiable. These risk factors include age, sex, ethnicity, family history, and premature vascular disease. However, several conditions that augment the course of atherosclerosis can be effectively addressed across the continuum of care. Among these risk factors, hypertension, hyperlipidemia, diabetes mellitus, and smoking are especially important, and their control is fundamental to management strategies for lowering the likelihood of recurrent ischemic events among patients with ischemic heart disease, ischemic stroke, or peripheral arterial disease (PAD). Management in such cases includes lifestyle changes and use of prescription medications, to be coordinated by a primary care physician in order to achieve optimal control.
Hypertension
Arterial hypertension (ie, systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg) is the most important modifiable factor associated with increased risk of stroke. Both diastolic and isolated systolic hypertension are important predictors of primary or recurrent stroke.12 Hypertension predisposes patients to atherosclerotic disease of the intracranial and extracranial arteries, most commonly at sites of vascular bifurcation. Hypertension also contributes to disease of the small penetrating arteries that perfuse deep brain structures.13,14
Management of hypertension is important both during the acute phase of ischemic stroke and throughout the long-term course of this condition. Both low blood pressure and high blood pressure in the setting of acute stroke are associated with poor outcomes. However, the optimal treatment of patients with hypertension in the first few hours or days after stroke has not been established.15 Some research has focused on antihypertensive therapy initiated in the first few days after stroke, but additional evaluation of the safety and efficacy of such therapy is needed.15-19 In the absence of definitive clinical data, current evidence-based guidelines suggest pursuing a cautious approach to reducing blood pressure in the acute stroke setting.20 In many cases, the patient's blood pressure will decrease spontaneously during the first few hours after stroke, and no medical intervention will be needed.
An exception to the cautious approach involves aggressive management of patients who are at high risk for hemorrhagic transformation. In addition, the blood pressure of patients who are to be treated with thrombolytic agents needs to be lower than 185 mm Hg systolic and less than 110 mm Hg diastolic in order to receive this medication.20
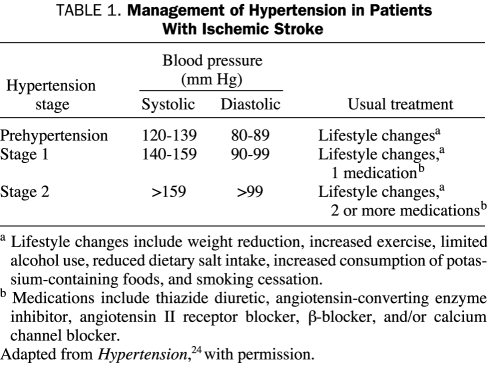
When short-term management of hypertension evolves into a strategy for longer-term treatment, the patient's condition will most likely be monitored by primary care physicians. The efficacy of antihypertensive therapy is confirmed by meta-analyses and randomized trials, which have shown that a 30% to 40% reduction in risk of recurrent stroke can be achieved by reducing blood pressure in patients.21-23 Although a major benefit may be achieved with only a 5- to 10-mm Hg reduction in blood pressure, the goal of long-term management is to reduce blood pressure to normal levels (ie, <120/80 mm Hg).24 Blood pressure is affected favorably by such lifestyle changes as reduced alcohol consumption, weight loss, increased exercise, restricted salt intake, increased consumption of fruits and vegetables, and smoking cessation. Nevertheless, most patients with high blood pressure will require treatment with antihypertensive medications (Table 1).
TABLE 1.
Management of Hypertension in Patients With Ischemic Stroke
The optimal medical regimen for managing hypertension after stroke has not yet been established. Clinical trials have tested, both singly and in combination, the efficacy of angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), β-blockers, calcium channel blockers, and diuretics.22,23 In addition to lowering blood pressure, evidence suggests that ACE inhibitors and ARBs may slow progression of arterial disease.25,26 This effect may partially explain the reduction in recurrent vascular events observed with the use of a perindopril-based blood pressure-lowering regimen among patients with a history of stroke or TIA but without hypertension.27 Although these data are interesting, they have not yet led to the widespread use of antihypertensive medications for prevention of recurrent stroke in patients who are not hypertensive.
On the basis of current evidence, guidelines for prevention of recurrent stroke suggest that a diuretic or the combination of a diuretic and an ACE inhibitor may be the most appropriate choice for initial antihypertensive therapy. However, guidelines also recommend consideration of the severity of arterial disease and the presence of concomitant renal disease, renal artery stenosis, heart disease, and diabetes mellitus when selecting a therapeutic antihypertensive regimen.10
Hyperlipidemia
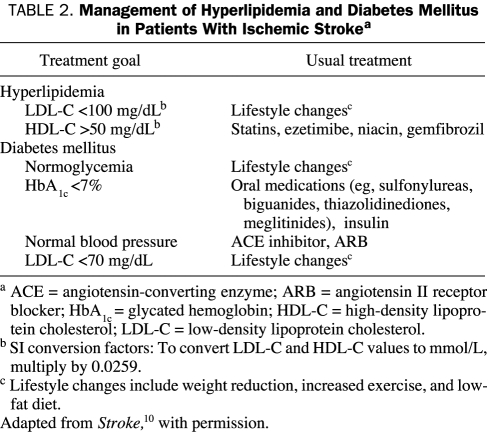
Although hyperlipidemia causes an increased risk of stroke secondary to atherosclerosis, especially among younger patients, its association with recurrent stroke is less clear. However, because hyperlipidemia is a strong predictor of myocardial ischemia, a fasting lipid profile should be obtained from all patients who have had recent ischemic stroke. If levels of low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) fall outside the target range (LDL-C <70-100 mg/dL, HDL-C >50 mg/dL; to convert to mmol/L, multiply by 0.0259), a comprehensive management program consisting of lifestyle modifications and medications should be initiated in the hospital and maintained on a long-term basis for patients with hyperlipidemia10 (Table 2).
TABLE 2.
Management of Hyperlipidemia and Diabetes Mellitus in Patients With Ischemic Strokea
Several clinical trials have shown the efficacy of statins for reducing the risk of recurrent cardiovascular events in patients with ischemic stroke.28-31 The results of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial,29 which included 4731 participants with a history of TIA or stroke but no history of coronary artery disease (CAD), indicated that, in comparison with placebo, atorvastatin reduced the relative risk of recurrent stroke by 16% during 5 years of follow-up (95% confidence interval, 1%-29%; P=.03). The recently updated AHA/ASA guidelines9 for secondary stroke prevention recommend the use of statin therapy for all patients with atherosclerotic stroke or TIA. In addition to lowering lipid levels, statins appear to stabilize the vasculature and to slow the progression of atherosclerosis.32,33
Concern has recently been expressed that statins may increase the patient's risk of hemorrhagic stroke.29,34,35 However, the observed increases in hemorrhagic stroke have been minimal, so the benefits of statins in preventing ischemia outweigh the risk of bleeding.34 Thus, statin therapy should not be withheld from patients who have had ischemic stroke.
In addition to using statins, patients with hypertriglyceridemia or low HDL-C levels may be treated with ezetimibe, niacin, or gemfibrozil.36-38 These medications also may be administered to patients who are unable to tolerate statins.
Diabetes Mellitus
Approximately 25% of patients who have had ischemic stroke also have diabetes mellitus, the presence of which is associated with an increased likelihood of recurrent stroke.39,40 Patients with metabolic syndrome, which includes lipid disturbances, insulin resistance, hypertension, and truncal obesity, also have an increased risk of stroke and other ischemic events.41 Because adequate glycemic control reduces the frequency of microvascular complications and lowers the risk of small-artery atherosclerotic disease, current secondary prevention guidelines recommend a goal of near normoglycemic levels (ie, glycated hemoglobin <7%) for patients with diabetes mellitus and recent stroke10 (Table 2).
Because of the increased prevalence of hypertension and hyperlipidemia among patients with type 2 diabetes mellitus, aggressive management of these risk factors is crucial to reducing the risk of vascular events in these patients.41-47 Most patients with diabetes mellitus will need more than a single antihypertensive agent to successfully reduce their blood pressure. Because ACE inhibitors and ARBs lessen the risk of renal dysfunction, these medications may be the best choices for patients with diabetes mellitus and recent stroke.10 To reduce the high risk of ischemic events in patients with diabetes mellitus, the recommended target LDL-C level in these patients is less than 70 mg/dL.10
Smoking
Compelling evidence suggests that smoking is an important risk factor for ischemic stroke and that even passive exposure to smoking may increase stroke risk.48-50 Cessation of smoking results in rapid reduction in the likelihood of recurrent ischemia, and within 5 years after smoking cessation, the risk of stroke drops to that found among persons who have never smoked. Because patients cannot smoke while hospitalized, this is the ideal time to start a smoking cessation program. Successful programs include a combination of counseling and the use of nicotine replacement products or such medications as bupropion and varenicline.51
Other Risk Factors
Several other measures to reduce the risk of stroke also are recommended in current prevention guidelines. These measures include the consumption of a diet rich in fruits and vegetables, increased potassium intake, decreased sodium intake, weight loss, regular exercise, and avoidance of heavy alcohol consumption.10 In addition, guidelines include recommendations that women avoid postmenopausal hormone replacement therapy because such therapy may be associated with an increased risk of ischemic events, including stroke.52,53
ANTITHROMBOTIC THERAPY AND SURGICAL/ENDOVASCULAR INTERVENTIONS
Antithrombotic Therapy
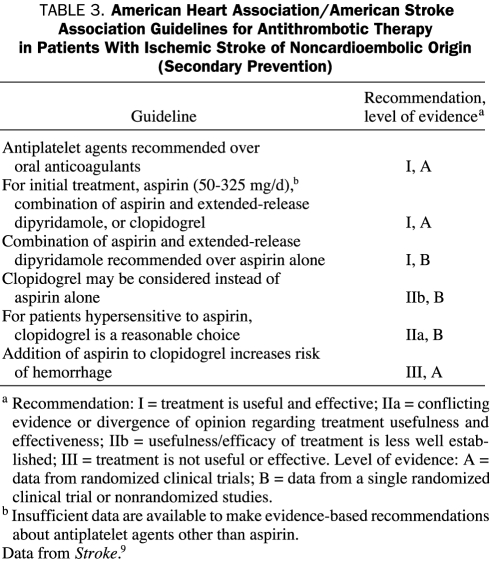
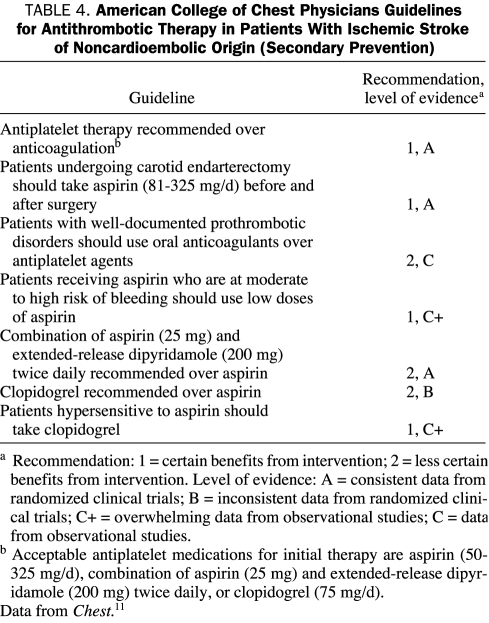
Guidelines for antithrombotic therapy for secondary prevention of stroke in patients who have had ischemic stroke of noncardioembolic origin have been developed by both the AHA/ASA (Table 3)9,10 and the American College of Chest Physicians (Table 4).11 Antithrombotic medications, including oral anticoagulants and antiplatelet agents, are key to strategies to reduce recurrent stroke risk.9-11 Oral anticoagulants are prescribed to lower the risk of cardioembolic events among patients who are at high risk for cardiac disorders, including patients with atrial fibrillation. These medications are also prescribed to many patients with prothrombotic disorders. The efficacy of oral anticoagulant therapy in preventing recurrent ischemic events in patients with stroke secondary to arterial disease has been tested in 4 clinical trials.54-57 Results of these trials demonstrate that oral anticoagulants are not superior to antiplatelet agents in preventing ischemic events, including recurrent stroke, among patients with arterial disease. Therefore, there is currently no indication for use of long-term oral anticoagulant therapy in patients with stroke secondary to atherosclerotic disease.10
TABLE 3.
American Heart Association/American Stroke Association Guidelines for Antithrombotic Therapy in Patients With Ischemic Stroke of Noncardioembolic Origin (Secondary Prevention)
TABLE 4.
American College of Chest Physicians Guidelines for Antithrombotic Therapy in Patients With Ischemic Stroke of Noncardioembolic Origin (Secondary Prevention)
Antiplatelet agents are the antithrombotic medication of choice for preventing ischemic events among persons who have symptomatic atherosclerotic disease in any vascular site. These agents can be effective regardless of patient age, sex, or concomitant diabetes mellitus or hypertension.58 In a meta-analysis of randomized clinical trials that included participants with stroke or TIA, antiplatelet therapy (vs control) was associated with significant absolute reduction in nonfatal recurrent stroke (8.3% vs 10.8%; P<.001), nonfatal myocardial infarction (1.7% vs 2.3%; P<.001), and vascular death (8.0% vs 8.7%; P=.04).58 Because of their proven efficacy, antiplatelet agents remain the standard against which other medications or surgical interventions for reducing risk of ischemic events are compared.
Aspirin, the combination of aspirin with extended-release dipyridamole, ticlopidine, and clopidogrel have been shown to provide effective secondary prevention for patients after ischemic stroke. Aspirin, in dosages from 30 mg/d to 1300 mg/d, has been found to protect patients from secondary ischemic events.58-61 Aspirin is generally tolerated well by patients; however, gastritis, peptic ulcer disease, and gastrointestinal bleeding are known complications of long-term use. These adverse effects of aspirin may be reduced by using lower doses or enteric-coated preparations.
The combination of aspirin and dipyridamole has been compared with aspirin alone in several clinical trials, most notably the European Stroke Prevention Study 2 (ESPS-2)62 and the European/Australasian Stroke Prevention in Reversible Ischaemia Trial (ESPRIT).63 Compared with the use of either aspirin or dipyridamole alone, the combination of these agents significantly reduced the relative risk of recurrent stroke among patients enrolled in ESPS-2.62 In ESPRIT, the combination of aspirin and dipyridamole was significantly more effective than aspirin alone in preventing the primary composite outcome (ie, vascular death, nonfatal myocardial infarction, nonfatal stroke, or major bleeding complication).63
In both ESPS-2 and ESPRIT, the risk of bleeding was the same with aspirin monotherapy as it was with aspirin plus dipyridamole.62,63 The primary adverse effect associated with use of dipyridamole is headache, which, in some cases, may be sufficiently severe to necessitate treatment cessation.62,63
In 3 clinical trials,64-66 the use of ticlopidine was compared with aspirin and with placebo in patients who had ischemic stroke or TIA. Ticlopidine has been found to be superior to placebo in reducing the number of ischemic events (Canadian American Ticlopidine Study [CATS]64) and superior to aspirin in reducing recurrent ischemic events (Ticlopidine Aspirin Stroke Study [TASS]65). However, in the African American Antiplatelet Stroke Prevention Study,66 no significant difference in outcome rates was observed between patients treated with aspirin and those treated with ticlopidine.
Potential complications of ticlopidine use include diarrhea, abdominal distress, skin eruptions, neutropenia, and thrombotic thrombocytopenic purpura.64-66 Although these potentially severe adverse effects, which largely occur within the first 3 months of treatment, are relatively rare, they occur frequently enough that most physicians in the United States no longer prescribe ticlopidine.
Clopidogrel has pharmacologic effects similar to ticlopidine but with an improved safety profile. Although cases of thrombotic thrombocytopenic purpura have been reported with the use of clopidogrel, the frequency of these cases is much less than with the use of ticlopidine.67,68 In the Clopidogrel Versus Aspirin in Patients at Risk of Ischaemic Events (CAPRIE) trial,69 clopidogrel significantly reduced the relative risk of major vascular events in patients with atherosclerotic vascular disease (ie, CAD, ischemic stroke, or symptomatic PAD) by 8.7% compared with aspirin (P=.043) without increasing the risk of bleeding. In the subgroup of patients who had previous stroke, the risk reduction with clopidogrel use compared with placebo was 7.3%, but this difference was not statistically significant (P=.26).69
Recently, results were reported for the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial,70 a randomized comparison of the effects of aspirin plus extended-release dipyridamole vs clopidogrel alone for secondary prevention in 20,332 patients with noncardioembolic ischemic stroke. During a mean follow-up period of 2.5 years, no significant differences were observed between the aspirin plus extended-release dipyridamole regimen and the clopidogrel regimen for rates of recurrent stroke (9.0% vs 8.8%, respectively; P=.78) or composite rates of stroke, myocardial infarction, or vascular death (13.1% vs 13.1%, respectively; P=.83).70 Although major hemorrhagic events and intracranial bleeding tended to occur more frequently among patients taking aspirin and dipyridamole than among those taking clopidogrel (4.1% vs 3.6%, respectively; P=.06), no significant difference was observed in the combined rates of recurrent stroke and major hemorrhage.71 More patients taking the combination of aspirin and dipyridamole than those taking clopidogrel had to permanently discontinue treatment, largely because of headaches (5.9% vs 0.9%, respectively).70
Overall, the results of PRoFESS70 show that monotherapy with clopidogrel and the combination of aspirin with extended-release dipyridamole are equally effective in preventing recurrent ischemic events after a stroke.
The combination of aspirin and clopidogrel has been shown to be effective for secondary prevention of recurrent ischemic events in patients with acute myocardial ischemia.71,72 This combination has also been tested in a broader range of at-risk patients, including those with ischemic stroke or TIA. In the Management of Atherothrombosis With Clopidogrel in High-Risk Patients With Recent TIA or Ischaemic Stroke (MATCH) trial,73 the combination of aspirin and clopidogrel was compared with clopidogrel alone in patients with a history of stroke or TIA. Results suggested that the combination of aspirin and clopidogrel is not more efficacious than clopidogrel monotherapy in lowering the risk of recurrent ischemic events. Furthermore, the trial found that combination therapy resulted in excess bleeding in patients with cerebrovascular disease.73
The Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) trial74 compared the combination of aspirin and clopidogrel with aspirin alone in patients who had documented ischemic cerebrovascular disease, CAD or PAD, or 3 or more atherothrombotic risk factors with no documented disease. The combination increased the risk of severe bleeding in patients and did not have a significant effect on reducing the risk of myocardial infarction, stroke, or vascular death.74 However, subgroup analysis of the enrolled population with history of myocardial infarction, stroke, or symptomatic PAD revealed that the aspirinclopidogrel combination significantly reduced the risk of recurrent ischemic events without increasing the rate of severe bleeding.75
In the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial,76 the combination of clopidogrel and aspirin was found to be superior to aspirin monotherapy in preventing microembolic signals in patients with recently diagnosed symptomatic carotid stenosis. However, the clinical meaning of this finding has yet to be determined because a clinical correlation with a reduction in ischemic events has not been shown.
A brief course of dual antiplatelet therapy with aspirin and clopidogrel, presumably after a loading dose of clopidogrel, might be a strategy for treatment of high-risk patients with recent TIA. The rationale behind such an approach is to aggressively inhibit platelet function during the period of greatest risk for stroke. Results from the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) pilot study77 suggest that dual aspirin and clopidogrel therapy may reduce the risk of stroke within 90 days of TIA. However, further research is needed to determine the clinical usefulness of this strategy for patients with recent TIA or ischemic stroke.
Current evidence-based treatment guidelines for secondary prevention of ischemic events recommend that patients with noncardioembolic stroke or TIA be treated with antiplatelet agents.9-11 Aspirin monotherapy, aspirin plus extended-release dipyridamole, and clopidogrel monotherapy are all acceptable options for initial therapy. Although clopidogrel alone and aspirin plus extended-release dipyridamole have been shown to be more effective than aspirin alone, many physicians continue to prescribe aspirin because of its established efficacy, well-known adverse-effect profile, over-the-counter availability, and low cost. Current guidelines do not recommend the use of clopidogrel over aspirin plus extended-release dipyridamole (or vice versa) for patients with noncardioembolic stroke or TIA.9,10 Guidelines further suggest that individual patient characteristics should be considered when selecting a specific medication.9,10
It should be kept in mind that the results of PRoFESS70 may have an effect on future recommendations.
Local Management of Large-Artery Atherosclerosis
Surgical and endovascular interventions are options for the treatment of patients with symptomatic atherosclerotic narrowing of large intracranial or extracranial arteries. Carotid endarterectomy (CEA) is an effective treatment for reducing the risk of stroke in patients with symptomatic moderate to severe stenosis (ie, > 50% narrowing) of the internal carotid artery.78,79 In general, the benefit from surgery is greatest among patients with stenosis in the range of 70% to 99%. Currently, the use of CEA, in conjunction with antiplatelet agents and with medications targeting atherosclerotic risk factors, is recommended for carefully selected patients who have stenosis of the internal carotid artery.10
In an international trial, extracranial-intracranial bypass surgery was not found to be superior to treatment with medication.80 However, some patients with symptomatic occlusion of the internal carotid artery are at high risk of recurrent stroke after surgery. Extracranial-intracranial bypass surgery is currently being assessed in the Carotid Occlusion Surgery Study (COSS) for use in patients with occlusion of the internal carotid artery who cannot be treated with CEA or endovascular interventions.81
Angioplasty, usually combined with stenting, is often used to treat patients with symptomatic arterial stenosis in either intracranial or extracranial locations of the carotid or vertebrobasilar circulations. Considerable interest has been shown in using endovascular treatments for these patients, and the number of patients who are being treated for stroke by angioplasty is increasing rapidly. Unfortunately, the clinical role of endovascular treatment needs to be better defined because much of the available information on this treatment is derived from uncontrolled series.
Published results of clinical trials comparing CEA with carotid artery angioplasty and stenting are mixed.82-84 Ongoing clinical trials, such as the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST), should help clarify the roles of CEA and carotid artery angioplasty/stenting in the treatment of patients with severe stenoses at the origin of the internal carotid artery.
The clinical usefulness of endovascular interventions for treatment of patients with stenotic lesions of the extracranial vertebral arteries or intracranial vessels is also not established. Available data on such interventions are derived from small case series.85-88 Ongoing clinical trials are addressing the role of endovascular treatment for these indications.
Carotid endarterectomy remains the preferred surgical intervention for treating symptomatic patients with severe stenosis of the origin of the internal carotid artery.10 The decision for surgery is affected by such factors as the patient's neurologic status, concomitant diseases, severity of the arterial condition, and presence of ulceration or of an intraluminal thrombus as well as by the skill of the surgeon. Carotid artery angioplasty and stenting are typically reserved for patients who have a contraindication for CEA, including recurrent stenosis after carotid surgery, previous radiation therapy, contralateral occlusion of the internal carotid artery, or for those who are poor surgical risks. Endovascular interventions may be considered as treatment for patients who have symptomatic extracranial vertebral artery stenosis or intracranial arterial lesions that have not responded to medication-based treatment.
DISCUSSION
With the aging of the US population and improved management of patients with heart disease, the number of people who are diagnosed as having atherosclerotic disease and who are at high risk of stroke is increasing. The number of patients who are at risk of both primary and recurrent ischemic stroke is also on the rise, and, as such, preventive measures are crucial for these patients.
Current guidelines delineate the importance of 3 components of care in treating patients with symptomatic atherosclerotic cerebrovascular disease: risk-factor management, antiplatelet therapy, and surgical procedures. These components are equally important in the primary prevention of stroke. Control of risk factors, particularly hypertension, hyperlipidemia, diabetes mellitus, and smoking, is fundamental to stroke prevention. Control of these risk factors can be accomplished by lifestyle modifications and pharmaceutical interventions and must be maintained throughout the continuum of care.
The goal of hypertension management should be a normal blood pressure for the patient. No specific antihypertensive regimen is ideal for all patients. Therefore, pending the results of ongoing and future studies, physicians should consider a patient's history when prescribing a blood pressure-lowering treatment plan. Although some evidence suggests that aggressive reduction of cholesterol levels may be associated with a modest increase in the risk of hemorrhagic stroke, the benefits of statins in reducing the risk of recurrent ischemic stroke and other ischemic vascular events outweigh the risk of bleeding. Aggressive management of blood pressure and lipid levels complements the control of blood glucose levels in patients with diabetes mellitus.
Virtually all patients who have had ischemic stroke should be treated with antiplatelet agents, such as aspirin, aspirin plus extended-release dipyridamole, or clopidogrel. In selecting medications, physicians should consider the patient's previous treatment and history of ischemic events, as well as potential contraindications, such as allergies. In appropriate cases, CEA should be considered as complementary to use of medications, including antiplatelet agents. Pending the results of ongoing clinical trials, extracranial-intracranial bypass surgery and carotid artery stenting may be options for certain patients with atherosclerotic cerebrovascular disease.
CONCLUSION
Use of an integrated treatment approach (involving risk-factor management, antiplatelet therapy, and surgical procedures, when indicated) presents the opportunity to lower the risk of recurrent stroke and other ischemic events in patients with recent ischemic stroke or TIA. Future research may provide support for using new medications, clarify the role of currently available medications, and better define the appropriate role of surgery, particularly endovascular treatments.
Footnotes
Editorial support for this study was funded by the Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership. The author did not receive any compensation for this study.
REFERENCES
- 1.Rosamond W, Flegal K, Furie K, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008January29;117(4):e25-e146 Epub 2007 Dec 17 [DOI] [PubMed] [Google Scholar]
- 2.Albers GW, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke. Chest 1998;114(5)(suppl):683S-698S [DOI] [PubMed] [Google Scholar]
- 3.Steg PG, Bhatt DL, Wilson PWF, et al. REACH Registry Investigators One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA 2007;297(11):1197-1206 [DOI] [PubMed] [Google Scholar]
- 4.Bravata DM, Ho SY, Meehan TP, Brass LM, Concato J. Readmission and death after hospitalization for acute ischemic stroke: 5-year follow-up in the Medicare population. Stroke 2007June;38(6):1899-1904 Epub 2007 May 17 [DOI] [PubMed] [Google Scholar]
- 5.Rothwell PM. The interrelation between carotid, femoral and coronary artery disease [editorial]. Eur Heart J. 2001;22(1):11-14 [DOI] [PubMed] [Google Scholar]
- 6.Adams RJ, Chimowitz MI, Alpert JS, et al. Coronary risk evaluation in patients with transient ischemic attack and ischemic stroke: a scientific statement for healthcare professionals from the Stroke Council and the Council on Clinical Cardiology of the American Heart Association/American Stroke Association. Circulation 2003;108(10):1278-1290 [DOI] [PubMed] [Google Scholar]
- 7.Fayad P. Secondary prevention measures after a stroke—should they target stroke or heart disease? Nat Clin Pract Neurol. 2006;2(12):646-647 [DOI] [PubMed] [Google Scholar]
- 8.Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006;47(10):2130-2139 [DOI] [PubMed] [Google Scholar]
- 9.Adams RJ, Albers G, Alberts MJ, et al. Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke 2008May;39(5):1647-1652 Epub 2008 Mar 5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention. Stroke 2006;37(2):577-617 [DOI] [PubMed] [Google Scholar]
- 11.Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thombolytic Therapy. Chest 2004;126(3)(suppl):483S-512S [DOI] [PubMed] [Google Scholar]
- 12.Bornstein N, Silvestrelli G, Caso V, Parnetti L. Arterial hypertension and stroke prevention: an update. Clin Exp Hypertens 2006;28(3-4):317-326 [DOI] [PubMed] [Google Scholar]
- 13.MacMahon S, Rodgers A. Blood pressure, antihypertensive treatment and stroke risk. J Hypertens Suppl. 1994;12(10):S5-S14 [PubMed] [Google Scholar]
- 14.Alexander RW. Hypertension and the pathogenesis of atherosclerosis: oxidative stress and the mediation of arterial inflammatory response: a new perspective. Hypertension 1995;25(2):155-161 [DOI] [PubMed] [Google Scholar]
- 15.Castillo J, Leira R, García MM, Serena J, Blanco M, Dávalos A. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke 2004February;35(2):520-526 Epub 2004 Jan 15 [DOI] [PubMed] [Google Scholar]
- 16.Chalmers J. The management of blood pressure in acute stroke. Lancet Neurol. 2003;2(10):593 [DOI] [PubMed] [Google Scholar]
- 17.Goldstein LB. Blood pressure management in patients with acute ischemic stroke [published correction appears in Hypertension. 2004;43(5):e35] Hypertension 2004February;43(2):137-141 Epub 2004 Jan 12 [DOI] [PubMed] [Google Scholar]
- 18.CHHIPS Trial Group CHHIPS (Controlling Hypertension and Hypotension Immediately Post-Stroke) pilot trial: rationale and design. J Hypertens 2005;23(3):649-655 [DOI] [PubMed] [Google Scholar]
- 19.Schrader J, Lüders S, Kulschewski A, et al. ACCESS Study Group The ACCESS Study: evaluation of Acute Candesartan Cilexetil Therapy in Stroke Survivors. Stroke 2003July;34(7):1699-1703 Epub 2003 Jun 19 [DOI] [PubMed] [Google Scholar]
- 20.Adams HP, Jr, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke Association. Stroke 2003;34(4):1056-1083 [DOI] [PubMed] [Google Scholar]
- 21.Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews [published correction appears in Stroke. 2004;35(3):776-785] Stroke 2004;35(4):1024 [PubMed] [Google Scholar]
- 22.Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke 2003November;34(11):2741-2748 Epub 2003 Oct 23 [DOI] [PubMed] [Google Scholar]
- 23.Blood Pressure Lowering Treatment Trialists' Collaboration Effects of different blood-pressure lowering regiments on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362(9395):1527-1535 [DOI] [PubMed] [Google Scholar]
- 24.Chobanian AV, Bakris GL, Black HR, et al. National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003December;42(6):1206-1252 Epub 2003 Dec 1 [DOI] [PubMed] [Google Scholar]
- 25.Enseleit F, Hürlimann D, Lüscher TF. Vascular protective effects of angiotensin converting enzyme inhibitors and their relation to clinical events. J Cardiovasc Pharmacol. 2001;37(suppl 1):S21-S30 [DOI] [PubMed] [Google Scholar]
- 26.Iadecola C, Gorelick PB. Hypertension, angiotensin, and stroke: beyond blood pressure. Stroke 2004;35(2):348-350 [DOI] [PubMed] [Google Scholar]
- 27.PROGRESS Collaborative Group Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack [published corrections appear in Lancet. 2001;358(9292):1556 and 2002;359(9323):2120] Lancet 2001;358(9287):1033-1041 [DOI] [PubMed] [Google Scholar]
- 28.Henyan NN, Riche DM, East HE, Gann PN. Impact of statins on risk of stroke: a meta-analysis. Ann Pharmacother. 2007December;41(12):1937-1945 Epub 2007 Nov 6 [DOI] [PubMed] [Google Scholar]
- 29.Amarenco P, Bogousslavsky J, Callahan A, III, et al. Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549-559 [DOI] [PubMed] [Google Scholar]
- 30.Collins R, Armitage J, Parish S, Sleight P, Peto R, Heart Protection Study Collaborative Group Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet 2004;363(9411):757-767 [DOI] [PubMed] [Google Scholar]
- 31.Crouse JR, III, Byington RP, Furberg CD. HMG-CoA reductase inhibitor therapy and stroke risk reduction: an analysis of clinical trials data [published correction appears in Atherosclerosis. 1998;140(1):193-194] Atherosclerosis 1998;138(1):11-24 [DOI] [PubMed] [Google Scholar]
- 32.Tsuchiya A, Nagotani S, Hayashi T, et al. Macrophage infiltration, lectin-like oxidized-LDL receptor-1, and monoctye chemoattractant protein-1 are reduced by chronic HMG-CoA reductase inhibition. Curr Neurovasc Res. 2007;4(4):268-273 [DOI] [PubMed] [Google Scholar]
- 33.Corsini A, Pazzucconi F, Arnaboldi L, et al. Direct effects of statins on the vascular wall. J Cardiovasc Pharmacol. 1998;31(5):773-778 [DOI] [PubMed] [Google Scholar]
- 34.Bang OY, Saver JL, Liebeskind DS, et al. Cholesterol level and symptomatic hemorrhagic transformation after ischemic stroke thrombolysis [published correction appears in Neurology. 2007;68(18):1547] Neurology 2007March;68(10):737-742 Epub 2006 Dec 20 [DOI] [PubMed] [Google Scholar]
- 35.Goldstein LB. Low LDL cholesterol, statins, and brain hemorrhage: should we worry [editorial]? Neurology 2007;68(10):719-720 [DOI] [PubMed] [Google Scholar]
- 36.Bloomfield Rubins H, Davenport J, Babikian V, et al. VA-HIT Study Group Reduction in stroke with gemfibrozil in men with coronary heart disease and low HDL cholesterol: the Veterans Affairs HDL Intervention Trial (VA-HIT). Circulation 2001;103(23):2828-2833 [DOI] [PubMed] [Google Scholar]
- 37.Gagné C, Bays HE, Weiss SR, et al. Ezetimibe Study Group Efficacy and safety of ezetimibe added to ongoing statin therapy for treatment of patients with primary hypercholesterolemia. Am J Cardiol. 2002;90(10):1084-1091 [DOI] [PubMed] [Google Scholar]
- 38.Miller M. Niacin as a component of combination therapy for dyslipidemia. Mayo Clin Proc. 2003;78(6):735-742 [DOI] [PubMed] [Google Scholar]
- 39.Hillen T, Coshall C, Tilling K, Rudd AG, McGovern R, Wolfe CD, South London Stroke Register Cause of stroke recurrence is multifactorial: patterns, risk factors, and outcomes of stroke recurrence in the South London Stroke Register. Stroke 2003June;34(6):1457-1463 Epub 2003 May 15 [DOI] [PubMed] [Google Scholar]
- 40.Petty GW, Brown RD, Jr, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Survival and recurrence after first cerebral infarction: a population-based study in Rochester, Minnesota, 1975 through 1989. Neurology 1998;50(1):208-216 [DOI] [PubMed] [Google Scholar]
- 41.Kernan WN, Inzucchi SE, Viscoli CM, Brass LM, Bravata DM, Horwitz RI. Insulin resistance and risk for stroke. Neurology 2002;59(6):809-815 [DOI] [PubMed] [Google Scholar]
- 42.Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339(19):1349-1357 [DOI] [PubMed] [Google Scholar]
- 43.Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993;329(5):304-309 [DOI] [PubMed] [Google Scholar]
- 44.Heart Protection Study Collaborative Group MRC/BHF heart protection study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003;361(9374):2005-2016 [DOI] [PubMed] [Google Scholar]
- 45.Pyŏrälä K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) [published correction appears in Diabetes Care. 1997;20(6):1048] Diabetes Care 1997;20(4):614-620 [DOI] [PubMed] [Google Scholar]
- 46.Curb JD, Pressel SL, Cutler JA, et al. Systolic Hypertension in the Elderly Program Cooperative Research Group Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension [published correction appears in JAMA. 1997;277(17):1356] JAMA 1996;276(23):1886-1892 [PubMed] [Google Scholar]
- 47.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383-393 [DOI] [PubMed] [Google Scholar]
- 48.Kawachi I, Colditz GA, Stampfer MJ, et al. Smoking cessation and decreased risk of stroke in women. JAMA 1993;269(2):232-236 [PubMed] [Google Scholar]
- 49.Wolf PA, D'Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke: the Framingham Study. JAMA 1988;259(7):1025-1029 [PubMed] [Google Scholar]
- 50.You RX, Thrift AG, McNeil JJ, Davis SM, Donnan GA, Melbourne Stroke Risk Factor Study (MERFS) Group Ischemic stroke risk and passive exposure to spouses' cigarette smoking. Am J Public Health 1999;89(4):572-575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nides M, Leischow S, Sarna L, Evans SE. Maximizing smoking cessation in clinical practice: pharmacologic and behavioral interventions. Prev Cardiol. 2007;10(2)(suppl 1):23-30 [DOI] [PubMed] [Google Scholar]
- 52.Writing Group for the Women's Health Initiative Investigators Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288(3):321-333 [DOI] [PubMed] [Google Scholar]
- 53.Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen-replacement therapy after ischemic stroke. N Engl J Med. 2001;345(17):1243-1249 [DOI] [PubMed] [Google Scholar]
- 54.ESPRIT Study Group Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial. Lancet Neurol. 2007;6(2):115-124 [DOI] [PubMed] [Google Scholar]
- 55.Algra A, De Schryver EL, van Gijn J, Kappelle LJ, Koudstaal PJ. Oral anticoagulants versus antiplatelet therapy for preventing further vascular events after transient ischemic attack or minor stroke of presumed arterial origin. Stroke 2003;34(1):234-235 [DOI] [PubMed] [Google Scholar]
- 56.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Warfarin-Aspirin Symptomatic Intracranial Disease Trial Investigators Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005;352(13):1305-1316 [DOI] [PubMed] [Google Scholar]
- 57.Mohr JP, Thompson JLP, Lazar RM, et al. Warfarin-Aspirin Recurrent Stroke Study Group A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001;345(20):1444-1451 [DOI] [PubMed] [Google Scholar]
- 58.Antithrombotic Trialists' Collaboration Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002;324(7329):71-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dutch TIA Trial Study Group A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991;325(18):1261-1266 [DOI] [PubMed] [Google Scholar]
- 60.SALT Collaborative Group Swedish Aspirin Low-Dose Trial (SALT) of 75 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet 1991;338(8779):1345-1349 [PubMed] [Google Scholar]
- 61.Sze PC, Reitman D, Pincus MM, Sacks HS, Chalmers TC. Antiplatelet agents in the secondary prevention of stroke: meta-analysis of the randomized control trials. Stroke 1988;19(4):436-442 [DOI] [PubMed] [Google Scholar]
- 62.Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study 2: dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143(1-2):1-13 [DOI] [PubMed] [Google Scholar]
- 63.ESPRIT Study Group Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet 2006;367(9523):1665-1673 [DOI] [PubMed] [Google Scholar]
- 64.Gent M, Blakely JA, Easton JD, et al. The Canadian American Ticlopidine Study (CATS) in thromboembolic stroke. Lancet 1989;1(8649):1215-1220 [DOI] [PubMed] [Google Scholar]
- 65.Hass WK, Easton JD, Adams HP, et al. Ticlopidine Aspirin Stroke Study Group A randomized trial comparing ticlopidine hydrochloride with aspirin for the prevention of stroke in high-risk patients. N Engl J Med. 1989;321(8):501-507 [DOI] [PubMed] [Google Scholar]
- 66.Gorelick PB, Richardson D, Kelly M, et al. African American Antiplatelet Stroke Prevention Study (AAASPS) Investigators Aspirin and ticlopidine for prevention of recurrent stroke in black patients: a randomized trial. JAMA 2003;289(22):2947-2957 [DOI] [PubMed] [Google Scholar]
- 67.Harker LA, Boissel J-P, Pilgrim AJ, Gent M, CAPRIE Steering Committee and Investigators Comparative safety and tolerability of clopidogrel and aspirin: results from CAPRIE. Drug Saf. 1999;21(4):325-335 [DOI] [PubMed] [Google Scholar]
- 68.Zakarija A, Bandarenko N, Pandey DK, et al. Clopidogrel-associated TTP: an update of pharmacovigilance efforts conducted by independent researchers, pharmaceutical suppliers, and the Food and Drug Administration. Stroke 2004February;35(2):533-537 Epub 2004 Jan 5 [DOI] [PubMed] [Google Scholar]
- 69.CAPRIE Steering Committee A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996;348(9038):1329-1339 [DOI] [PubMed] [Google Scholar]
- 70.Sacco RL, Diener HC, Yusuf S, et al. PRoFESS Study Group Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359(12):1238-1251 Epub 2008 Aug 27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) [published correction appears in Circulation. 2008;117(9):e180] Circulation 2007August14;116(7):e148-e304 Epub 2007 Aug 6 [DOI] [PubMed] [Google Scholar]
- 72.Antman EM, Hand M, Armstrong PW, et al. 2007 Focused update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, writing on behalf of the 2004 Writing Committee [published correction appears in Circulation. 2008;117(6):e162] Circulation 2008January15;117(2):296-329 Epub 2007 Dec 10 [DOI] [PubMed] [Google Scholar]
- 73.Diener H-C, Bogousslavsky J, Brass LM, et al. MATCH Investigators Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet 2004;364(9431):331-337 [DOI] [PubMed] [Google Scholar]
- 74.Bhatt DL, Fox KA, Hacke W, et al. CHARISMA Investigators Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006April20;354(16):1706-1717 Epub 2006 Mar 12 [DOI] [PubMed] [Google Scholar]
- 75.Bhatt DL, Flather MD, Hacke W, et al. CHARISMA Investigators Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol. 2007May15;49(19):1982-1988 Epub 2007 Apr 11 [DOI] [PubMed] [Google Scholar]
- 76.Markus HS, Droste DW, Kaps M, et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using Doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation 2005May3;111(17):2233-2240 Epub 2005 Apr 25 [DOI] [PubMed] [Google Scholar]
- 77.Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM, FASTER Investigators Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol. 2007November;6(11):961-969 Epub 2007 Oct 10 [DOI] [PubMed] [Google Scholar]
- 78.North American Symptomatic Carotid Endarterectomy Trial Collaborators Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325(7):445-453 [DOI] [PubMed] [Google Scholar]
- 79.European Carotid Surgery Trialists' Collaborative Group Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998;351(9113):1379-1387 [PubMed] [Google Scholar]
- 80.EC/IC Bypass Study Group Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke: results of an international randomized trial. N Engl J Med. 1985;313(19):1191-1200 [DOI] [PubMed] [Google Scholar]
- 81.Grubb RL., Jr Extracranial-intracranial arterial bypass for treatment of occlusion of the internal carotid artery. Curr Neurol Neurosci Rep. 2004;4(1):23-30 [DOI] [PubMed] [Google Scholar]
- 82.SPACE Collaborative Group 30 Day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised non-inferiority trial [published correction appears in Lancet. 2006;368(9543):1238] Lancet 2006;368(9543):1239-1247 [DOI] [PubMed] [Google Scholar]
- 83.Mas J-L, Chatellier G, Beyssen B, et al. EVA-3S Investigators Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355(16):1660-1671 [DOI] [PubMed] [Google Scholar]
- 84.Yadav JS, Wholey MH, Kuntz RE, et al. Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Investigators Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351(15):1493-1501 [DOI] [PubMed] [Google Scholar]
- 85.Chastain HD, II, Campbell MS, Iyer S, et al. Extracranial vertebral artery stent placement: in-hospital and follow-up results. J Neurosurg. 1999;91(4):547-552 [DOI] [PubMed] [Google Scholar]
- 86.de Rochemont Rdu M, Turowski B, Buchkremer M, Sitzer M, Zanella FE, Berkfeld J. Recurrent symptomatic high-grade intracranial stenoses: safety and efficacy of undersized stents—initial experience. Radiology 2004;231(1):45-49 [DOI] [PubMed] [Google Scholar]
- 87.Malek AM, Higashida RT, Phatouros CC, et al. Treatment of posterior circulation ischemia with extracranial percutaneous balloon angioplasty and stent placement. Stroke 1999;30(10):2073-2085 [DOI] [PubMed] [Google Scholar]
- 88.Mori T, Kazita K, Mori K. Cerebral angioplasty and stenting for intracranial vertebral atherosclerotic stenosis. AJNR Am J Neuroradiol. 1999;20(5):787-789 [PMC free article] [PubMed] [Google Scholar]