Abstract
Subclinical hypothyroidism (SCH), also called mild thyroid failure, is diagnosed when peripheral thyroid hormone levels are within normal reference laboratory range but serum thyroid-stimulating hormone (TSH) levels are mildly elevated. This condition occurs in 3% to 8% of the general population. It is more common in women than men, and its prevalence increases with age. Of patients with SCH, 80% have a serum TSH of less than 10 mIU/L. The most important implication of SCH is high likelihood of progression to clinical hypothyroidism. The possibility that it is a cardiovascular risk factor has been a subject of debate. Large-scale randomized studies are needed for evidence-based recommendations regarding screening for mild thyroid failure and levothyroxine therapy for this condition. Currently, the practical approach is routine levothyroxine therapy for persons with a persistent serum TSH of more than 10.0 mIU/L and individualized therapy for those with a TSH of less than 10.0 mIU/L.
SCH = subclinical hypothyroidism; TPO = thyroperoxidase; TSH = thyroid-stimulating hormone
Subclinical hypothyroidism (SCH) is defined as a serum thyroid-stimulating hormone (TSH) level above the upper limit of normal despite normal levels of serum free thyroxine.1 Serum TSH has a log-linear relationship with circulating thyroid hormone levels (a 2-fold change in free thyroxine will produce a 100-fold change in TSH). Thus, serum TSH measurement is the necessary test for diagnosis of mild thyroid failure when the peripheral thyroid hormone levels are within normal laboratory range.1 The individual range for peripheral thyroid hormones is narrower than the population reference laboratory range; therefore, a slight reduction within the normal range will result in elevation of serum TSH above the normal range.
Subclinical hypothyroidism or mild thyroid failure is a common problem, with a prevalence of 3% to 8% in the population without known thyroid disease.2,3 The prevalence increases with age and is higher in women.2 After the sixth decade of life, the prevalence in men approaches that of women, with a combined prevalence of 10%.2 Antithyroid antibodies can be detected in 80% of patients with SCH, and 80% of patients with SCH have a serum TSH of less than 10 mIU/L.
Before diagnosis of SCH, other causes of an elevated TSH level, such as recovery from nonthyroidal illness, assay variability, presence of heterophile antibodies interfering with the TSH assay, and certain cases of central hypothyroidism with biologically inactive TSH and thyroid hormone resistance, should be excluded. However, the most common cause of elevated TSH is autoimmune thyroid disease.1 Previous radioiodine therapy, thyroid surgery, and external radiation therapy can also result in mild thyroid failure. Transient SCH may occur after episodes of postpartum, silent, and granulomatous thyroiditis.1,4
The clinical importance of and therapy for mild elevation of serum TSH (<10 mIU/L)5 and the exact upper limit of normal for the serum TSH level remain subjects of debate.6-9 When the TSH level is above 10 mIU/L, levothyroxine therapy is generally agreed to be appropriate.5,10 However, management of patients with a serum TSH level of less than 10 mIU/L is controversial.11 Some authors argue for routine10 and some for selective5 therapy. A recent 2007 meta-analysis of 14 randomized clinical trials enrolling a total of 350 patients concluded that levothyroxine replacement therapy for SCH does not result in improved survival or decreased cardiovascular morbidity. Data on health-related quality of life and symptoms did not show significant differences between intervention groups. Some evidence indicates that levothyroxine replacement improves some parameters of lipid profiles and left ventricular function.12
WHAT IS THE UPPER LIMIT OF NORMAL FOR THE SERUM TSH LEVEL?
Lowering the upper limit of normal for the serum TSH level from 5.0 to 3 .0 or even 2.5 mIU/L has been proposed,7,9 but such proposals have been met with substantial critique.6,8 The strongest argument in favor of lowering the upper limit of normal for the serum TSH level is the higher level of antithyroid antibodies detected in persons with a serum TSH level between 3.0 and 5.0 mIU/L and the higher rate of progression to clinical thyroid disease.9 After exclusion of persons with goiter, antithyroid antibodies, and a family history of thyroid disease, the mean serum TSH is 1.5 mIU/L. The serum TSH distribution curve is not Gaussian; there is a tail end at the upper limits of normal. If the distribution is extrapolated to be Gaussian, then the upper limit for the 97.5th percentile will be 2.5 mIU/L.9 The argument against lowering the upper limit of normal for TSH values is that 22 to 28 million more Americans would be diagnosed with hypothyroidism without any clinical or therapeutic benefit from this diagnosis.8 Our own data also show that decreasing the upper limit of the TSH reference range to 3.0 mIU/L results in more than a 4-fold increase in diagnosis of hypothyroidism among patients without history of thyroid disease seen in a tertiary medical center.13 No clear evidence supports a benefit for intervening at these levels of TSH. In contrast, lowering of the level of TSH from the upper limit of normal to lower normal range by adjustment of levothyroxine dose does not improve sense of well-being and nonspecific complaints.14 Recent reanalysis of the data from the National Health and Nutrition Examination Survey III study has suggested that serum TSH distribution progressively shifts toward higher concentrations with age and that the prevalence of SCH may be significantly overestimated in older age groups unless an age-specific range for TSH is used.6 In a recent study of 766 persons with negative findings on antithyroid antibody assay, normal findings on thyroid ultrasonography, and no evidence of thyroid disease, Hamilton et al15 determined a serum TSH level of 4.1 mIU/L to be the upper reference limit. This value is more compatible with clinical experience and is a reasonable compromise.
Although persons with a TSH level between 3.0 and 5.0 mIU/L are more likely to have positive antithyroid antibodies and future thyroid disease, the lack of evidence for a benefit from levothyroxine therapy at these levels makes keeping the upper limit of TSH at 4.0 to 5.0 (depending on the laboratory) more reasonable. For persons older than 70 years, values up to 6.0 or even 7.0 mIU/L in the absence of antithyroid antibodies should not result in diagnosis of hypothyroidism.6 Regardless of the chosen upper limit of normal, a convincing argument can be made for closer follow-up of persons with a TSH level of 3 to 5 mIU/L, in particular if antithyroid antibodies are detected.
Different normal TSH values are proposed for pregnancy. The range of serum TSH levels in the first trimester of pregnancy is 0.03 to 2.3 mIU/L; the upper limit of normal is 3.5 mIU/L in both the second and third trimesters of pregnancy.
SCREENING FOR SCH
Uniform national guidelines for screening for thyroid disease with serum TSH levels have not been established. However, because of the high prevalence of SCH and associated metabolic risk factors such as hyperlipidemia, the American Thyroid Association recommends screening by measurement of serum TSH beginning at age 35 years and every 5 years thereafter.16 The evidence in favor of screening is particularly compelling in women, but it can also be justified for men as a relatively cost-effective measure in the context of the periodic health examination. Persons with symptoms and signs potentially attributable to thyroid dysfunction and those with risk factors for its development may require more frequent serum TSH testing.16 The American College of Physicians acknowledges that treatment for subclinical thyroid dysfunction is controversial but suggests that screening to detect thyroid dysfunction may be indicated in women older than 50 years.17 Because of potential implications of SCH for adverse outcome of pregnancy18 and neuropsychiatric development of the fetus,19 aggressive case finding in pregnant women or in women anticipating pregnancy has been suggested.5 However, relying only on aggressive case finding results in missing a third of women with overt hypothyroidism or SCH.20
Before recommending routine screening of the general population, large-scale randomized trials are needed to prove that treatment will improve quality of life in otherwise healthy patients who have the mildly elevated TSH level (5-10 mIU/L) typical of most SCH cases. Meanwhile, clinicians should have a low threshold for obtaining a serum TSH level in women who have vague suggestive symptoms, who are pregnant or anticipating becoming pregnant, or who have a strong family history of autoimmune thyroid disease. Many thyroidologists advocate routine screening before and during pregnancy.20
PROPOSED ADVERSE CONSEQUENCES OF SCH
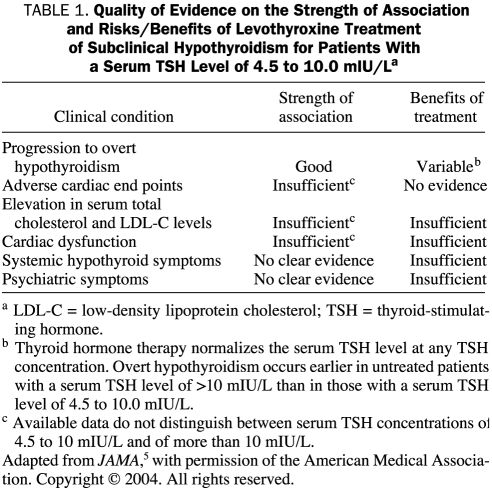
Although studies have pointed to some adverse effects of SCH, no consensus exists as to the clinical importance of the adverse effects and the benefits of levothyroxine therapy, particularly for the 80% of patients with SCH who have a TSH of less than 10 mIU/L, because of the different levels of TSH and degrees of thyroid dysfunction in these studies11,21 (Table 1). A discussion of some of the proposed adverse effects of SCH follows.
TABLE 1.
Quality of Evidence on the Strength of Association and Risks/Benefits of Levothyroxine Treatment of Subclinical Hypothyroidism for Patients With a Serum TSH Level of 4.5 to 10.0 mIU/La
Progression to Overt Hypothyroidism
Patients with SCH have a high rate of progression to clinically overt hypothyroidism, 2.6% each year if thyroperoxidase (TPO) antibodies are absent and 4.3% if they are present.22 However, some persons do not show progression and some experience normalization. A TSH level greater than 10 mIU/L predicts a higher rate of progression, and a level of less than 6 mIU/L predicts a lower likelihood of progression. In a study in men and women older than 55 years with a mean follow-up of 32 months, the TSH level normalized in 52% of those with a serum TSH of less than 10 mIU/L.23
Systemic Symptoms of Hypothyroidism
Several randomized studies of the effect of levothyroxine therapy in patients with SCH are available. One study limited to patients with serum TSH levels from 5 to 10 mIU/L did not show any benefit.24 Some studies (range in TSH level, 3-32 mIU/L) showed improved symptom scores or improved memory in a quarter of patients. Many recent studies have not shown improvement in mood, anxiety, and cognition in older persons.25-27 In a previous scientific review in 2004,5 available data were considered insufficient to support a benefit for levothyroxine therapy in patients with SCH, in particular for the group with TSH less than 10 mIU/L, and a similar conclusion can again be drawn in 2008.
Lipid Abnormalities and Other Cardiac Risk Factors
The Colorado Health Fair study showed that the mean total cholesterol level was 216 mg/dL (to convert to mmol/L, multiply by 0.0259) for euthyroid patients and 224 mg/dL for patients with SCH.28 Several randomized studies have shown reduction of low-density lipoprotein cholesterol by levothyroxine therapy. However, most of the studies showing benefit are not categorized for serum TSH levels of 5.0 to 10.0 mIU/L. A meta-analysis of 13 studies concluded that the lipid profile improved with therapy.29 In a 2004 review, data were considered insufficient to show benefits of levothyroxine therapy on lipid levels.5 In my estimation, the possibility that lipid levels will improve with levothyroxine therapy is fair if the serum TSH level is greater than 10 mIU/L and questionable if the TSH level is less than 10 mIU/L.
In a large population-based study, emerging risk factors such as elevated C-reactive protein, homocysteines and lipoprotein(a) levels were not found to have a role in SCH.30 Improvement of endothelial dysfunction and insulin resistance after levothyroxine therapy has been suggested.31,32 In the absence of large-scale randomized trials, evidence remains inconclusive.
Adverse Cardiac End Points
The cross-sectional Rotterdam Study showed an association of SCH with myocardial infarction and aortic calcification.33 In contrast, the Wickham study34 showed no increased cardiac mortality in a 20-year follow-up. A more recent observational study also did not show any association between unrecognized SCH and cardiovascular events or mortality.35 However, several more recent meta-analyses of observational studies found an association between SCH and coronary artery disease.36-38 The risk is lower when higher-quality studies are pooled.37 A recent analysis of 7 cohort studies concluded that the relative risk of all-cause mortality was increased compared with euthyroid controls, particularly in patients with comorbid conditions.39 Another meta-analysis of 15 studies showed an increased prevalence and incidence of cardiovascular mortality only in a relatively younger population.40 Taken together, the findings of these 6 recent meta-analyses suggest that a cardiovascular risk exists for persons younger than age 70 years with no effect for those aged 70 to 80 years and a possibly protective effect for those older than 80 years.41 Thus, the cardiovascular risk issue remains controversial, and large-scale, government-sponsored, multicenter, randomized, placebo-controlled studies are needed to assess the efficacy of levothyroxine therapy in risk reduction.
Cardiac Dysfunction
Studies have shown slowed left ventricular relaxation time, increased vascular tone at rest, and left ventricular systolic dysfunction with exercise and impaired endothelial function.42 Some studies have shown improvement of cardiac contractibility and systolic time interval with levothyroxine therapy.42 No evidence exists to support an association between heart failure and a serum TSH level of less than 10.0 mIU/L. Again, most studies were not categorized for degrees of TSH elevation, and data remain insufficient for a TSH level less than 10 mIU/L but strongly suggestive for a TSH level greater than 10 mIU/L.
Adverse Fetal Effects
A seminal study by Haddow et al19 showed a 7-point reduction in intelligence quotient in children aged 7 to 9 years whose mothers had SCH at pregnancy compared with the children of euthyroid mothers. Although this was a single study, it nevertheless points to the need for screening of pregnant women and therapy for mild thyroid failure in women who are pregnant or planning on becoming pregnant.
Neuromuscular Dysfunction
It has been suggested that neuromuscular symptoms and dysfunction are common in patients with SCH and can be reversed by levothyroxine treatment.43 A definitive answer will require more studies with TSH levels stratified as less than or greater than 10 mIU/L.
Psychiatric and Cognitive Dysfunction
Data related to aggravation of depression, bipolar disorder, and effect on cognitive function have been presented.44 A recent study showed no association with anxiety, depression, or cognitive dysfunction.25 Nonetheless, it is still reasonable to have a low threshold for therapy for SCH in patients with depression, bipolar disorder, and cognitive dysfunction.
MANAGEMENT OF SCH
Management of SCH differs depending on whether the serum TSH concentration is 3 to 5 mIU/L, 5.1 to 10 mIU/L, or higher than 10 mIU/L.
Serum TSH Concentration of 3 to 5 mIU/L
Lowering the upper limit of normal for the serum TSH level from 5.0 to 3.0 mIU/L is still controversial. Levels between 3 and 5 mIU/L are unlikely to indicate a clinically important abnormality, and levothyroxine therapy at these levels may or may not provide a benefit. Although persons with a serum TSH level of 3 to 5 mIU/L may be at higher risk of progression to hypothyroidism,22 no firm evidence of health consequences exists. In fact, in a randomized, crossover, 12-week study of patients with symptoms suggestive of hypothyroidism with serum TSH in the upper normal range, no difference in cognitive and psychological function was observed between levothyroxine-treated and control groups.14 Given these findings, intervention cannot be recommended for this group, but follow-up by serum TSH measurement in 1 year would be a reasonable approach, particularly if antithyroid antibodies are detected.
Serum TSH Concentration of 5.1 to 10 mIU/L
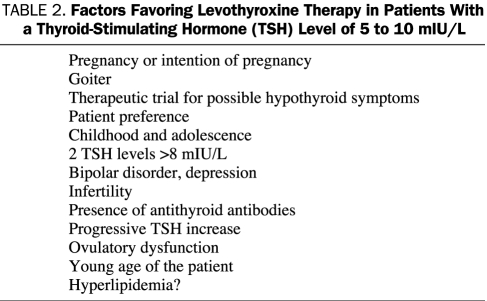
Large-scale randomized studies to conclusively show reduction of cholesterol with levothyroxine therapy in this subgroup are lacking. Most studies are not stratified for different categories of serum TSH levels, and although benefits for symptoms and lipid levels have been shown for mild thyroid failure as a group, results cannot be extended to most patients with SCH who are in this subgroup.1,45 One study of TSH levels of 5.0 to 10.0 mIU/L did not show any benefit.24 Also, cognitive, neuropsychiatric, cardiac, and muscle abnormalities described in studies including a wide spectrum of TSH levels in SCH should be confirmed by larger randomized studies. The possibility that an elevated serum TSH level is a cardiovascular risk factor is still highly controversial. Hence, decision for levothyroxine therapy for this group should be individualized and should depend on the age of the patient (favoring therapy for younger persons), associated medical conditions, degree of TSH elevation, persistence and gradual increase of TSH, presence of antithyroid antibodies, presence of goiter, and hypothyroid symptoms (Table 2).
TABLE 2.
Factors Favoring Levothyroxine Therapy in Patients With a Thyroid-Stimulating Hormone (TSH) Level of 5 to 10 mIU/L
Given both the findings of reduced intelligence quotient in the children of women who had SCH while pregnant19 and the adverse effects of mild thyroid failure on pregnancy outcome, levothyroxine therapy should be advised for pregnant women and women who anticipate becoming pregnant. Because of the effect of thyroxine on growth and development, levothyroxine therapy for children and adolescents is also reasonable. Therapy may be considered for patients with a persistent serum TSH level of more than 8 mIU/L because these levels are associated with a 70% progression to a TSH level of 10 mIU/L in 4 years (V.F. and colleagues, unpublished data, 2003).
Serum TSH Concentration Greater Than 10 mIU/L
Most thyroidologists agree that all patients with SCH and a serum TSH level above 10 mIU/L should be treated with levothyroxine.11,21 Evidence is more compelling for the adverse effects of mild thyroid failure in this group. Studies have shown that levothyroxine therapy results in an 8-mg reduction in low-density lipoprotein levels.29,45 Among the factors that predict response of lipid levels to levothyroxine therapy are higher levels of TSH, insulin resistance, higher levels of pretherapy cholesterol, and type III hyperlipidemia. Some evidence suggests that mild thyroid failure can aggravate bipolar disorder and depression46 and that it is associated with abnormalities of muscle function, nerve conduction, cardiac function,47 and cognitive and psychological function, with improvement after levothyroxine therapy.45,47-50
LEVOTHYROXINE THERAPY FOR SCH
For all patients with SCH and a serum TSH concentration above 10 mIU/L and for patients with serum TSH concentrations of 5.1 to 10.0 mIU/L in whom individualized decision for therapy is made, therapy should be started with levothyroxine. We do not currently recommend a combination of T4 plus T3 therapy. In my experience, the usual required daily levothyroxine dose is 50 to 75 μg.51 Anticipating future progression of thyroid failure, some endocrinologists recommend a full replacement dose. I prefer to start with a daily dose of 25 to 75 μg, depending on the age of the patient, the level of free thyroxine, and the serum TSH level. Serum TSH should be checked after 8 weeks, and the dose should be adjusted. Once a normal serum TSH level has been achieved, TSH should be measured again after 6 months and then annually. In younger persons, a reasonable goal for serum TSH is 0.3 to 3.0 mIU/L. For older age groups, the therapeutic goal can be higher. The benefits of fine-tuning levothyroxine therapy to achieve lower levels of serum TSH should be weighed against the possibility of adverse effects of overzealous levothyroxine therapy resulting in suppressed TSH and SCH.
CONCLUSION
Subclinical hypothyroidism occurs in the clinical setting of a serum TSH level above the upper limit of normal despite a normal serum free thyroxine concentration. Initiating levothyroxine replacement therapy is recommended for all patients with a TSH greater than 10 mIU/L, even if the free thyroxine concentration is within normal laboratory range. However, treatment of patients with a serum TSH level between 5 and 10 mIU/L remains controversial. The strongest arguments for levothyroxine therapy are the high risk of progression to overt hypothyroidism, the possible improvement of quality of life, and the possibility that SCH is a cardiovascular risk factor. Recent evidence shows that any possible increased cardiovascular risk would be to persons younger than 70 years; those aged 70 and 80 years have no additional risk, and those older than 80 years may actually enjoy a protective benefit. Large-scale, government-sponsored, multicenter, randomized, placebo-controlled studies are urgently needed to assess the efficacy of levothyroxine therapy in the subgroup with TSH levels of less than 10 mIU/L. Meanwhile, therapy of this subgroup should be individualized by taking into account patient preference, presence of symptoms, age, and associated medical conditions.
Supplementary Material
On completion of this article you should be able to: (1) diagnose and interpret the meaning and clinical importance of subclinical hypothyroidism, (2) assess possible adverse effects of mild thyroid failure and describe the current knowledge about the effect of levothyroxine therapy in mild thyroid failure, and (3) select patients with subclinical hypothyroidism who are more likely to benefit from therapy.
CME Questions About SCH
-
An 81-year-old man has symptoms of fatigue but is otherwise healthy. His thyroid is normal on palpitation. He is overweight with a body mass index of 38. Laboratory tests yield the following results: total cholesterol, 270 mg/dL (to convert to mmol/L, multiply by 0.0259); elevated serum homocysteine levels; lipoprotein(a) level, 60 mg/dL (to convert to μmol/L, multiply by 0.0357); serum thyroid-stimulating hormone (TSH) level, 7 mIU/L; serum free thyroxine, 1.1 ng/dL (to convert to pmol/L, multiply by 12.871); and elevated levels of C-reactive protein. Which one of the following statements is true regarding the management of this patient?
Levothyroxine therapy will reduce cardiovascular risk
Overnight oximetry will be helpful
Hyperlipidemia is caused by subclinical hypothyroidism (SCH)
Levothyroxine therapy will lower homocysteine levels
Levothyroxine therapy will reduce lipoprotein(a) levels
-
A 30-year-old woman presents with fatigue and a weight gain of 9.1 kg in the past 6 months. She has a sister who is receiving levothyroxine therapy for hypothyroidism. On examination, a diffuse 35-g thyroid is palpable. Laboratory tests are unremarkable except for a serum free thyroxine level of 1.3 ng/dL and a serum TSH level of 7 mIU/L. Thyroperoxidase (TPO) antibodies are detected. Which one of the following statements is least applicable to this patient?
Levothyroxine therapy will result in substantial weight loss
Levothyroxine therapy has a 25% chance of improving her quality of life
Levothyroxine therapy will reduce the size of the goiter
The likelihood of progression to clinical hypothyroidism in 10 years is 50%
Therapy is semiurgent if she plans pregnancy
-
A 32-year-old woman is 8 weeks pregnant. Laboratory studies ordered by her obstetrician show a normal blood cell count and serum glucose level, a serum free thyroxine level of 1.2 ng/dL, a serum TSH level of 5.0 mIU/L, and the presence of TPO antibodies. Which one of the following statements is least applicable to the management of this patient?
Normal serum TSH values in the first trimester of pregnancy differ from nonpregnant values
Levothyroxine therapy is strongly recommended
Risk of miscarriage may be increased
Risk of postpartum hyperthyroidism may be increased
Increased thyroxin-binding globulin in the first trimester can result in TSH elevation to stabilize free thyroxine levels
-
Which one of the following patients is most likely to benefit from levothyroxine therapy?
An 85-year-old man with a serum TSH level of 7.0 mIU/L and cognitive changes
A woman in the first trimester of pregnancy with a serum TSH level of 4.0 mIU/L who tests positive for TPO antibodies
A 65-year-old man who has just been released from the hospital after a prolonged recovery from myocardial infarction whose laboratory study now shows a serum TSH level of 12 mIU/L
A 55-year-old woman with a serum TSH level of 5.1 mIU/L and a serum cholesterol level of 260 mg/dL (to convert to mmol/L, multiply by 0.0259)
A 40-year-old woman who had an upper respiratory infection 2 months earlier followed by several weeks of sore neck and who now has a serum TSH level of 12 mIU/L and serum free thyroxine level of 0.8 ng/dL
-
Which one of the following statements about mild thyroid failure (SCH) is true?
All cases of mild thyroid failure of autoimmune origin are associated with the presence of TPO antibodies
Almost all patients with a serum TSH level greater than 10.0 mIU/L need levothyroxine therapy
Women older than 60 years are 4 times more likely to have an elevated serum TSH level than men in the same age group
The best therapy for SCH is a combination of levothyroxine (T4) and T3
All experts would agree that levothyroxine therapy is indicated in a patient with a serum TSH of 8.0 mIU/L and a mildly elevated total cholesterol level
This activity was designated for 1 AMA PRA Category 1 Credit(s).™
Because the Concise Review for Clinicians contributions are now a CME activity, the answers to the questions will no longer be published in the print journal. For CME credit and the answers, see the link on our Web site at mayoclinicproceedings.com.
REFERENCES
- 1.Cooper DS. Subclinical hypothyroidism. N Engl J Med. 2001;345(4):260-265 [DOI] [PubMed] [Google Scholar]
- 2.Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489-499 [DOI] [PubMed] [Google Scholar]
- 3.Karmisholt J, Andersen S, Laurberg P. Variation in thyroid function tests in patients with stable untreated subclinical hypothyroidism. Thyroid 2008;18(3):303-308 [DOI] [PubMed] [Google Scholar]
- 4.Fatourechi V. Subclinical hypothyroidism: when to treat, when to watch? Consultant 2004;44(4):533-539 [Google Scholar]
- 5.Surks MI, Ortiz E, Daniels GH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA 2004;291(2):228-238 [DOI] [PubMed] [Google Scholar]
- 6.Surks MI, Hollowell JG. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J Clin Endocrinol Metab. 2007December;92(12):4575-4582 Epub 2007 Oct 2 [DOI] [PubMed] [Google Scholar]
- 7.Spencer CA, Hollowell JG, Kazarosyan M, Braverman LE. National Health and Nutrition Examination Survey III thyroid-stimulating hormone (TSH)-thyroperoxidase antibody relationships demonstrate that TSH upper reference limits may be skewed by occult thyroid dysfunction. J Clin Endocrinol Metab. 2007November;92(11):4236-4240 Epub 2007 Aug 7 [DOI] [PubMed] [Google Scholar]
- 8.Surks MI, Goswami G, Daniels GH. The thyrotropin reference range should remain unchanged. J Clin Endocrinol Metab. 2005;90(9):5489-5496 [DOI] [PubMed] [Google Scholar]
- 9.Wartofsky L, Dickey RA. The evidence for a narrower thyrotropin reference range is compelling. J Clin Endocrinol Metab. 2005;90(9):5483-5488 [DOI] [PubMed] [Google Scholar]
- 10.Gharib H, Tuttle RM, Baskin HJ, Fish LH, Singer PA, McDermott MT. Subclinical thyroid dysfunction: a joint statement on management from the American Association of Clinical Endocrinologists, the American Thyroid Association, and the Endocrine Society. Thyroid 2005;15(1):24-28 [DOI] [PubMed] [Google Scholar]
- 11.Chu JW, Crapo LM. The treatment of subclinical hypothyroidism is seldom necessary. J Clin Endocrinol Metab. 2001;86(10):4591-4599 [DOI] [PubMed] [Google Scholar]
- 12.Villar HC, Saconato H, Valente O, Atallah AN. Thyroid hormone replacement for subclinical hypothyroidism. Cochrane Database Syst Rev. 2007;(3):CD003419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fatourechi V, Klee GG, Grebe SK, et al. Effects of reducing the upper limit of normal TSH values [letter]. JAMA 2003;290(24):3195-3196 [DOI] [PubMed] [Google Scholar]
- 14.Pollock MA, Sturrock A, Marshall K, et al. Thyroxine treatment in patients with symptoms of hypothyroidism but thyroid function tests within the reference range: randomised double blind placebo controlled crossover trial. BMJ 2001;323(7318):891-895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton TE, Davis S, Onstad L, Kopecky KJ. Thyrotropin levels in a population with no clinical, autoantibody, or ultrasonographic evidence of thyroid disease: implications for the diagnosis of subclinical hypothyroidism. J Clin Endocrinol Metab. 2008April;93(4):1224-1230 Epub 2008 Jan 29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ladenson PW, Singer PA, Ain KB, et al. American Thyroid Association guidelines for detection of thyroid dysfunction. [published correction appears in Arch Intern Med. 2001;161(2):284] Arch Intern Med. 2000;160(11):1573-1575 [DOI] [PubMed] [Google Scholar]
- 17.Helfand M, Redfern CC American College of Physicains Clinical guideline, part 2: screening for thyroid disease: an update [published correction appears in Ann Intern Med. 1999;130(3):246] Ann Intern Med. 1998;129(2):144-158 [DOI] [PubMed] [Google Scholar]
- 18.Hollowell JG, LaFranchi S, Smallridge RC, Spong CY, Haddow JE, Boyle CA. 2004 Where do we go from here?—summary of working group discussions on thyroid function and gestational outcomes. Thyroid 2005;15(1):72-76 [DOI] [PubMed] [Google Scholar]
- 19.Haddow JE, Palomaki GE, Allan WC, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999;341(8):549-555 [DOI] [PubMed] [Google Scholar]
- 20.Vaidya B, Anthony S, Bilous M, et al. Detection of thyroid dysfunction in early pregnancy: universal screening or targeted high-risk case finding? J Clin Endocrinol Metab. 2007January;92(1):203-207 Epub 2006 Oct 10 [DOI] [PubMed] [Google Scholar]
- 21.McDermott MT, Ridgway EC. Subclinical hypothyroidism is mild thyroid failure and should be treated. J Clin Endocrinol Metab. 2001;86(10):4585-4590 [DOI] [PubMed] [Google Scholar]
- 22.Vanderpump MP, Tunbridge WM, French JM, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf) 1995;43(1):55-68 [DOI] [PubMed] [Google Scholar]
- 23.Díez JJ, Iglesias P. Spontaneous subclinical hypothyroidism in patients older than 55 years: an analysis of natural course and risk factors for the development of overt thyroid failure. J Clin Endocrinol Metab. 2004;89(10):4890-4897 [DOI] [PubMed] [Google Scholar]
- 24.Kong WM, Sheikh MH, Lumb PJ, et al. A 6-month randomized trial of thyroxine treatment in women with mild subclinical hypothyroidism [published correction appears in Am J Med. 2002;113(3):264] Am J Med. 2002;112(5):348-354 [DOI] [PubMed] [Google Scholar]
- 25.Roberts LM, Pattison H, Roalfe A, et al. Is subclinical thyroid dysfunction in the elderly associated with depression or cognitive dysfunction? Ann Intern Med. 2006;145(8):573-581 [DOI] [PubMed] [Google Scholar]
- 26.Gussekloo J, van Exel E, de Craen AJ, Meinders AE, Frölich M, Westendorp RG. Thyroid status, disability and cognitive function, and survival in old age. JAMA 2004;292(21):2591-2599 [DOI] [PubMed] [Google Scholar]
- 27.Jorde R, Waterloo K, Storhaug H, Nyrnes A, Sundsfjord J, Jenssen TG. Neuropsychological function and symptoms in subjects with subclinical hypothyroidism and the effect of thyroxine treatment. J Clin Endocrinol Metab. 2006January;91(1):145-153 Epub 2005 Nov 1 [DOI] [PubMed] [Google Scholar]
- 28.Canaris G, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160(4):526-534 [DOI] [PubMed] [Google Scholar]
- 29.Danese MD, Ladenson PW, Meinert CL, Powe NR. Effect of thyroxine therapy on serum lipoproteins in patients with mild thyroid failure: a quantitative review of the literature. J Clin Endocrinol Metab. 2000;85(9):2993-3001 [DOI] [PubMed] [Google Scholar]
- 30.Hueston WJ, King DE, Geesey ME. Serum biomarkers for cardiovascular inflammation in subclinical hypothyroidism. Clin Endocrinol. 2005;63(5):582-587 [DOI] [PubMed] [Google Scholar]
- 31.Duntas LH, Wartofsky L. Cardiovascular risk and subclinical hypothyroidism: focus on lipids and new emerging risk factors: what is the evidence? Thyroid 2007;17(11):1075-1084 [DOI] [PubMed] [Google Scholar]
- 32.Razvi S, Ingoe L, Keeka G, Oates C, McMillan C, Weaver JU. The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial. J Clin Endocrinol Metab. 2007May;92(5):1715-1723 Epub 2007 Feb 13 [DOI] [PubMed] [Google Scholar]
- 33.Hak AE, Pols HAP, Visser TJ, Drexhage HA, Hofman A, Witteman JCM. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000;132(4):270-278 [DOI] [PubMed] [Google Scholar]
- 34.Vanderpump MP, Tunbridge WM, French JM, et al. The development of ischemic heart disease in relation to autoimmune thyroid disease in a 20-year follow-up study of an English community. Thyroid 1996;6(3):155-160 [DOI] [PubMed] [Google Scholar]
- 35.Cappola AR, Fried LP, Arnold AM, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA 2006;295(9):1033-1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rodondi N, Aujesky D, Vittinghoff E, Cornuz J, Bauer DC. Subclinical hypothyroidism and the risk of coronary heart disease: a meta-analysis. Am J Med. 2006;119(7):541-551 [DOI] [PubMed] [Google Scholar]
- 37.Ochs N, Auer R, Bauer D, et al. Meta-analysis: subclinical thyroid dysfunction and the risk for coronary heart disease and mortality. Ann Intern Med. 2008June3;148(11):832-845 Epub 2008 May 19 [DOI] [PubMed] [Google Scholar]
- 38.Singh S, Duggal J, Molnar J, Maldonado F, Barsano CP, Arora R. Impact of subclinical thyroid disorders on coronary heart disease, cardiovascular and all-cause mortality: a meta-analysis. Int J Cardiol. 2008March28;125(1):41-48 Epub 2007 Apr 16 [DOI] [PubMed] [Google Scholar]
- 39.Haentjens P, Van Meerhaeghe A, Poppe K, Velkeniers B. Subclinical thyroid dysfunction and mortality: an estimate of relative and absolute excess all-cause mortality based on time-to-event data from cohort studies. Eur J Endocrinol. 2008September;159(3):329-341 Epub 2008 May 29 [DOI] [PubMed] [Google Scholar]
- 40.Razvi S, Shakoor A, Vanderpump M, Weaver JU, Pearce SH. The influence of age on the relationship between subclinical hypothyroidism and ischemic heart disease: a metaanalysis. J Clin Endocrinol Metab. 2008August;93(8):2998-3007 Epub 2008 May 27 [DOI] [PubMed] [Google Scholar]
- 41.Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008February;29(1):76-131 Epub 2007 Nov 8 [DOI] [PubMed] [Google Scholar]
- 42.Biondi B. Cardiovascular effects of mild hypothyroidism. Thyroid 2007;17(7):625-630 [DOI] [PubMed] [Google Scholar]
- 43.Christ-Crain M, Meier C, Huber PR, Staub J-J, Muller B. Effect of l-thyroxine replacement therapy on surrogate markers of skeletal and cardiac function in subclinical hypothyroidism. Endocrinologist 2004;14(3):161-166 [Google Scholar]
- 44.Haggerty JJ, Jr, Garbutt JC, Evans DL, et al. Subclinical hypothyroidism: a review of neuropsychiatric aspects. Int J Psychiatry Med. 1990;20(2):193-208 [DOI] [PubMed] [Google Scholar]
- 45.Meier C, Staub JJ, Roth CB, et al. TSH-controlled L-thyroxine therapy reduces cholesterol levels and clinical symptoms in subclinical hypothyroidism: a double blind, placebo-controlled trial (Basel Thyroid Study). J Clin Endocrinol Metab. 2001;86(10):4860-4866 [DOI] [PubMed] [Google Scholar]
- 46.Haggerty JJ, Jr, Prange AJ., Jr Borderline hypothyroidism and depression. Annu Rev Med. 1995;46:37-46 [DOI] [PubMed] [Google Scholar]
- 47.Biondi B, Palmieri EA, Lombardi G, Fazio S. Effects of subclinical thyroid dysfunction on the heart. Ann Intern Med. 2002;137(11):904-914 [DOI] [PubMed] [Google Scholar]
- 48.Jaeschke R, Guyatt G, Gerstein H, et al. Does treatment with L-thyroxine influence health status in middle-aged and older adults with subclinical hypothyroidism? J Gen Intern Med. 1996;11(12):744-749 [DOI] [PubMed] [Google Scholar]
- 49.Cooper DS, Halpern R, Wood LC, Levin AA, Ridgway EC. L-thyroxine therapy in subclinical hypothyroidism: a double-blind, placebo-controlled trial. Ann Intern Med. 1984;101(1):18-24 [DOI] [PubMed] [Google Scholar]
- 50.Nyström E, Caidahl K, Fager G, Wikkelsö C, Lundberg PA, Lindstedt G. A double-blind cross-over 12-month study of L-thyroxine treatment of women with ‘subclinical’ hypothyroidism. Clin Endocrinol (Oxf) 1988;29(1):63-75 [DOI] [PubMed] [Google Scholar]
- 51.Fatourechi V, Lankarani M, Schryver PG, Vanness DJ, Long KH, Klee GG. Factors influencing clinical decisions to initiate thyroxine therapy for patients with mildly increased serum thyrotropin (5.1-10.0 mIU/L). Mayo Clin Proc. 2003;78(5):554-560 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.