Abstract
A systematic review of English-language literature was undertaken to answer the question, “Are there differences in cost or quality of inpatient medical care provided to adults by hospitalists vs nonhospitalists?” A computerized search was performed, using hospitalist and either quality, outcome, or cost as search terms. References from relevant articles were searched by hand. A standard data-extraction tool was used, and articles were included on the basis of quality and relevance. The reports that were included (N=33) show general agreement that hospitalist care leads to shorter length of stay and lower cost per stay. Three reports show improvement in outcomes for orthopedic surgery patients who had hospitalist consultation or comanagement, 3 reports show improvement in markers of quality of care for patients with pneumonia, and 2 reports show improvement in aspects of heart failure management. Further research should seek to determine why differences in care exist, whether these improvements might be generalized to other physicians, and whether hospitalists provide demonstrable benefit in other areas of care.
In the United States, general medical inpatient care is provided by both hospitalists (who provide only inpatient care) and more traditional, nonhospitalist physicians (who provide both outpatient and inpatient care). Although the hospitalist model of care is established and accepted in Canada and the United Kingdom, the first hospitalist program in the United States, the Park Nicollet program in Minnesota, was not established until 1994.1 A growing effort is being made to determine whether a difference in care exists between these 2 groups of physicians because a systematic difference would have implications for the cost and quality of care.
Reviews of hospitalist care were previously undertaken by Wachter and Goldman,2 Wachter,3 and most recently Coffman and Rundall.4 Since the 2005 review by Coffman and Rundall, a number of reports on hospitalist care (including 20 articles cited in this review) have compared hospitalists and nonhospitalists in terms of cost, length of stay (LOS), and quality measures. The previous reviews generally concluded that hospitalist care leads to lower cost per admission and shorter LOS without altering patient satisfaction.
This review collects and synthesizes all available reports of trials that help answer the question, “Are there differences in cost or quality of inpatient medical care provided to adults by hospitalists vs nonhospitalists?” The review is undertaken now because of the number of new articles since the last review and because of the importance of identifying any modifiable differences between hospitalists and other physicians that might lead to systematic improvements in cost or quality of care.
MATERIALS AND METHODS
A systematic review of the English-language literature was undertaken to answer the question, “Are there differences in cost or quality of inpatient medical care provided to adults by hospitalists vs nonhospitalists?” Articles were included if they contained data on outcomes, quality measures, or cost of care delivery from randomized trials or observational studies of adult patients cared for by hospitalists vs nonhospitalists. Articles were excluded if they pertained to pediatric or critical care hospitalists rather than general medicine hospitalists. Articles were excluded if they compared factors in addition to type of attending physician (for example, articles comparing a service with residents or a discharge planner and a service without). Poor-quality articles were also excluded (for example, if they had no comparison group, used estimated numbers of outcomes for a control group, or did not report significance or P values).
Searches for relevant articles were conducted on the National Library of Medicine Gateway (http://gateway.nlm.nih.gov/gw/Cmd) and on the Cochrane Collaboration Web site (www.cochrane.org). Search terms included hospitalist and either quality, outcome, or cost. Articles were screened by title and then by abstract. In addition, on the National Library of Medicine Web site, the Related Articles search tool was used after relevant articles were selected. References in the selected articles were searched by hand for further research reports on the topic that might not have been located in the original searches. The search included articles published up to August 1, 2008.
The selected articles were evaluated for study quality according to the methods outlined by the Cochrane Handbook for Systematic Reviews of Interventions.5 The methods included classification of articles on the basis of study type and scrutiny of articles for methodological flaws. A formal information tracking and evaluation tool was used for data extraction.
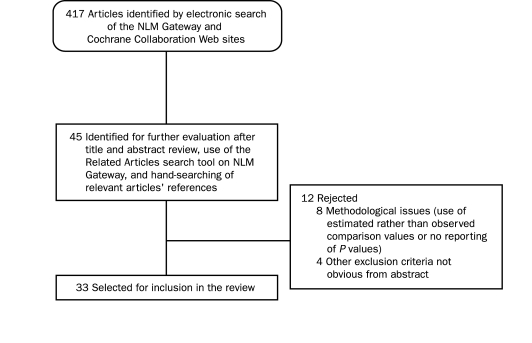
A flowchart similar to that outlined by the QUOROM (Quality of Reporting of Meta-analyses) statement6 was used to track the flow of reports through the evaluation process (Figure).
FIGURE.
Flow of information through the systematic review process. NLM = National Library of Medicine.
RESULTS
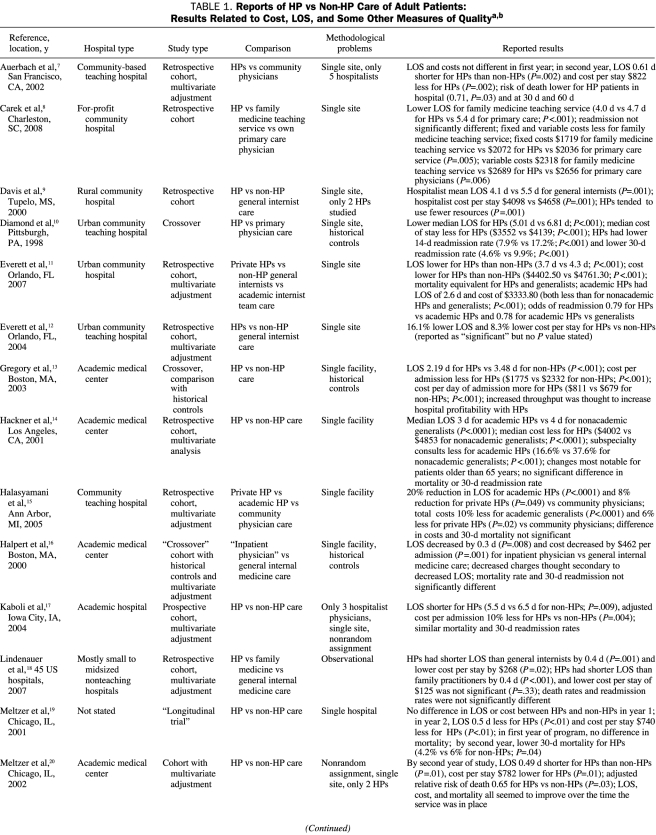
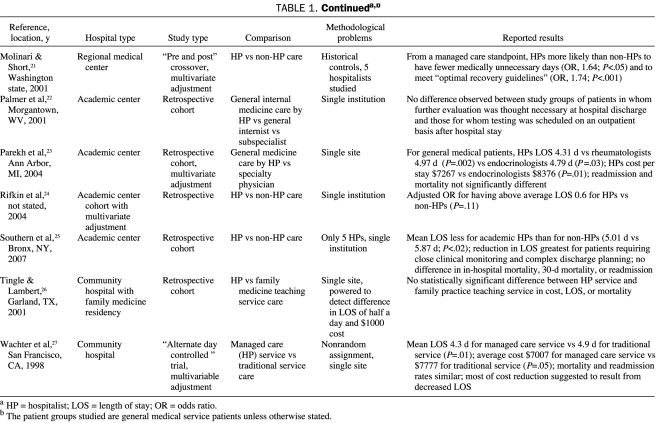
Results of this systematic review of hospitalist vs nonhospitalist care of general medical patients as they relate to cost, LOS, and other markers of quality is presented in Table 1.7-27 In general, the results show that inpatient care by hospitalist physicians leads to decreased hospital cost and LOS. Exceptions to this conclusion include 3 reports showing no significant difference in most quality measures between hospitalists and nonhospitalists26,28,29 and 2 reports showing generally better performance by either a family medicine service8 or a cardiologist-directed service30 than by hospitalist care. Three reports describe the need for fewer subspecialty consults by hospitalists than by non-hospitalists.14,31,32 A few reports describe improved survival in patients cared for by hospitalists vs nonhospitalists.7,19,20
TABLE 1.
Reports of HP vs Non-HP Care of Adult Patients: Results Related to Cost, LOS, and Some Other Measures of Qualitya,b
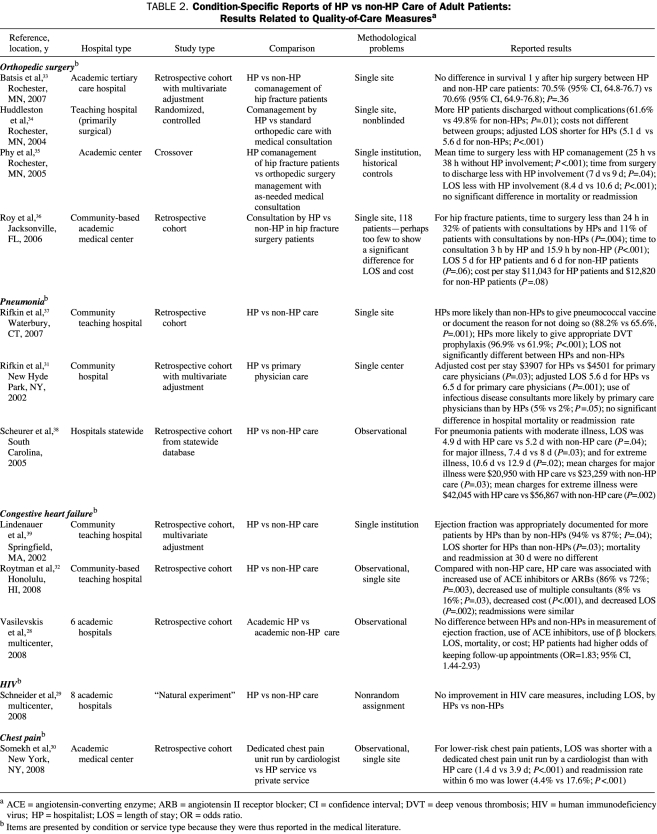
Hospitalist care was also reported to improve several measures of care for specific services or conditions, including orthopedic surgery, pneumonia, and congestive heart failure. Interestingly, improvement was not seen for patients with human immunodeficiency virus or low-risk chest pain (Table 228-39).
TABLE 2.
Condition-Specific Reports of HP vs non-HP Care of Adult Patients: Results Related to Quality-of-Care Measuresa
Orthopedic surgery patients cared for or comanaged by hospitalists had a shorter time to surgery (25 vs 38 hours; P<.001),35 a shorter time to consultation, and a shorter total LOS than those cared for by nonhospitalists.35,36 Huddleston et al34 reported fewer complications at discharge for orthopedic surgery patients comanaged by hospitalists. Rifkin et al37 found that hospitalists caring for patients with pneumonia were more likely than nonhospitalists to give appropriate prophylaxis against venous thromboembolism (96.9% vs 61.9%; P<.001) and more likely to give pneumococcal vaccine or to document the reason for not doing so (88.2% vs 65.6%; P=.001). Two studies reported decreased cost and LOS for hospitalized patients with pneumonia cared for by hospitalists vs nonhospitalists.31,38 Lindenauer et al39 reported that, for patients with congestive heart failure, hospitalists were more likely than nonhospitalists to have documented the ejection fraction (94% vs 87%; P=.04); their patients also had a shorter LOS. Another study of congestive heart failure showed improvement in use of angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and in LOS in patients cared for by hospitalists vs nonhospitalists.32 A multicenter study comparing services directed by academic hospitalists with those directed by academic generalists showed no difference in most quality measures for patients with congestive heart failure.28 Quality measures for care of patients with the human immunodeficiency virus were not improved by an academic hospitalist vs academic generalist service.29 For low-risk patients with chest pain, LOS and readmission rates were better for a chest pain unit managed by a cardiologist than for routine management by hospitalists.30
DISCUSSION
In general, the reports included in this review show that inpatient care of general medical patients by hospitalist physicians leads to decreased hospital cost and LOS.
Hospitalist programs appear to mature with time, perhaps because of adjustment by hospitalists or increased experience. Several studies have shown that hospitalist programs did not have an effect (or had lesser effect) on cost or LOS during their first year but did have notable effect during their second year.7,19,20
Several theories have been offered to explain the apparent differences between hospitalist and nonhospitalist outcomes. According to one theory, hospitalists are able to respond more rapidly to changes in a patient's condition because they tend to be in-house with no competing clinic responsibilities.40 Another theory holds that hospitalists likely have more practice or experience tending to inpatient medical problems.2 (This has been called disease-specific physician experience.20)
Several recent reports have shown that the higher daily cost per patient of hospitalists is compensated for by the more rapid discharge of patients from the hospital. One study examined the possibility that the reported decreases in costs by hospitalists are due to incomplete evaluation of patients in the hospital. In other words, the costs of any tests not completed in the hospital would be passed on to outpatient clinics after hospitalization, making hospitalists only appear more efficient. The investigators concluded that this was not the case in their study population.22 Economic analysis suggests that hospitalists increased profitability by moving patients more quickly (“higher throughput”) through hospital systems that had beds in short supply.13
Many of the research reports referenced in this review are observational studies with associated nonrandom allocation, and several of the prospective studies also had nonrandom assignment. Nonrandom assignment of patients can allow bias to occur and can also allow unequal levels of a confounding factor in different study groups, even if such bias and inequity are not readily apparent. For example, with nonrandom assignment, we might expect a larger number of acutely ill patients with pneumonia to be admitted by critical care physicians than by hospitalists and a larger number to be admitted by hospitalists than by a family medicine service, making comparisons about cost, survival, and LOS difficult. In this review, several studies had fewer than 5 hospitalists in the study group, and many studies were done at a single institution. Both of these factors may result in bias related to personal characteristics of a few physicians or to regional differences in practice. Among the articles in this review, reporting of results is nonuniform, with some articles reporting means, others medians, and some only ratios. The reports as a group are heterogeneous, making a meta-analysis inappropriate.
Systematic reviews may be hampered by difficulties related to publication bias, in which articles are more likely to be published if they show positive findings. This limitation is not confined to this review but is a potential problem for any review. I am unaware of any unpublished data on the topic of this review. Whether to include unpublished data should be an important consideration in conducting a systematic review. Investigators need to remember, however, that bias against negative results is not the only reason why a manuscript may be unpublished; a manuscript may have any of a number of inadequacies that disqualify it from consideration for publication.
CONCLUSION
Despite limitations in the quality of available reports, common themes emerge from this review of hospitalist care. In general, hospitalist care appears to result in lower cost per admission, largely because of shorter LOS, although use of fewer consultants has been observed by some investigators as well. A few reports show differences in other measures of quality, such as mortality, readmission rate, and performance in specific populations, such as patients with pneumonia, those with congestive heart failure, and those undergoing orthopedic surgery.
Further studies should investigate whether benefits shown for hospitalist care might be generalized to other physicians. These studies should also examine whether differences between hospitalists and nonhospitalists exist in other areas of care, with the intent again being to define the reason for any differences so that any improvements in care can be generalized to other physicians.
Acknowledgments
The thoughtful editorial comments of Kirsten Ward, PhD, Non-communicable Disease Branch, London School of Hygiene and Tropical Medicine, are appreciated.
REFERENCES
- 1.Freese RB. The Park Nicollet experience in establishing a hospitalist system. Ann Intern Med. 1999;130(4, pt 2):350-354 [DOI] [PubMed] [Google Scholar]
- 2.Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514-517 [DOI] [PubMed] [Google Scholar]
- 3.Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86(4):687-706 [DOI] [PubMed] [Google Scholar]
- 4.Coffman J, Rundall TG. The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis. Med Care Res Rev. 2005;62(4):379-406 [DOI] [PubMed] [Google Scholar]
- 5.http://www.cochrane.org/resources/handbook/index.htm. Cochrane Collaboration Web site. Accessed January 9, 2009.
- 6.Hopewell S, Clarke M, Moher D, et al. CONSORT Group CONSORT for reporting randomised trials in journal and conference abstracts. Lancet 2008;371(9609):281-283 [DOI] [PubMed] [Google Scholar]
- 7.Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficacy and patient outcomes. Ann Intern Med. 2002;137(11):859-865 [DOI] [PubMed] [Google Scholar]
- 8.Carek PJ, Boggan H, Manious AG, III, Geesey ME, Dickerson L, Laird S. Inpatient care in a community hospital: comparing length of stay and costs among teaching, hospitalists and community services. Fam Med. 2008;40(2):119-124 [PubMed] [Google Scholar]
- 9.Davis KM, Koch KE, Harvey JK, Wilson R, Engelert J, Gerard PD. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med. 2000;108(8):621-626 [DOI] [PubMed] [Google Scholar]
- 10.Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med. 1998;129(3):197-203 [DOI] [PubMed] [Google Scholar]
- 11.Everett G, Uddin N, Rudloff B. Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians. J Gen Intern Med. 2007May;22(5):662-667 Epub 2007 Mar 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Everett GD, Anton MP, Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care 2004;10(9):626-630 [PubMed] [Google Scholar]
- 13.Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38(3):905-918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hackner D, Tu G, Braunstein GD, Ault M, Weingarten S, Mohsenifar Z. The value of a hospitalist service: efficient care for the aging population? Chest 2001;119(2):580-589 [DOI] [PubMed] [Google Scholar]
- 15.Halasyamani LK, Valenstein PN, Freidlander MP, Cowen ME. A comparison of two hospitalist models with traditional care in a community teaching hospital. Am J Med. 2005;118(5):536-543 [DOI] [PubMed] [Google Scholar]
- 16.Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality, utilization, and satisfaction. Am J Manag Care 2000;6(5):549-555 [PubMed] [Google Scholar]
- 17.Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and cost on an academic hospitalist service. Am J Manag Care 2004;10(8):561-568 [PubMed] [Google Scholar]
- 18.Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357(25):2589-2600 [DOI] [PubMed] [Google Scholar]
- 19.Meltzer DO, Shah MN, Morrison J, Jin L, Levinson W. Decreased length of stay, costs and mortality in a randomized trial of academic hospitalists [abstract]. JGIM 2001;16(suppl 1):208-209 11318919 [Google Scholar]
- 20.Meltzer DO, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866-874 [DOI] [PubMed] [Google Scholar]
- 21.Molinari C, Short R. Effects of an HMO hospitalist program on inpatient utilization. Am J Manag Care 2001;7(11):1051-1057 [PubMed] [Google Scholar]
- 22.Palmer H, Delamata M, McBride C, Dunsworth T, Evans K, Hobbs G. After discharge effects of a hospitalist service [abstract]. JGIM 2001;16(suppl 1):211 11318921 [Google Scholar]
- 23.Parekh V, Saint S, Furney S, Kaufman S, McMahon L. What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medical service? J Gen Intern Med. 2004;19(5, pt 1):395-401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rifkin WD, Holmboe E, Scherer H, Sierra H. Comparison of hospitalists and nonhospitalists in inpatient length of stay adjusting for patient and physician characteristics. J Gen Intern Med. 2004;19(11):1127-1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Southern WN, Berger MA, Bellin EY, Hailpern SM, Arnsten JH. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167(17):1869-1874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tingle LE, Lambert CT. Comparison of a family practice teaching service and a hospitalist model: costs, charges, length of stay, and mortality. Fam Med. 2001;33(7):511-515 [PubMed] [Google Scholar]
- 27.Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA 1998;279(19):1560-1565 [DOI] [PubMed] [Google Scholar]
- 28.Vasilevskis EE, Meltzer D, Schnipper J, et al. Quality of care for decompensated heart failure: comparable performance between academic hospitalists and non-hospitalists. J Gen Intern Med. 2008September;23(9):1399-1406 Epub 2008 Jul 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider JA, Zhang Q, Auerbach A, et al. Do hospitalists or physicians with greater inpatient HIV experience improve HIV care in the era of highly active antiretroviral therapy? results from a multicenter trial of academic hospitalists. Clin Infect Dis. 2008;46(7):1085-1092 [DOI] [PubMed] [Google Scholar]
- 30.Somekh NN, Rachko M, Husk G, Friedmann P, Bergmann SR. Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186-192 [DOI] [PubMed] [Google Scholar]
- 31.Rifkin WD, Conner D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77(10):1053-1058 [DOI] [PubMed] [Google Scholar]
- 32.Roytman MM, Thomas SM, Jiang CS. Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure. J Hosp Med. 2008:3(1):35-41 [DOI] [PubMed] [Google Scholar]
- 33.Batsis JA, Phy MP, Melton LJ, III, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219-225 [DOI] [PubMed] [Google Scholar]
- 34.Huddleston JM, Long KH, Naessens JM, et al. Hospitalist-Orthopedic Team Trial Investigators Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38 [DOI] [PubMed] [Google Scholar]
- 35.Phy MP, Vanness DJ, Melton LJ, III, et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165(7):796-801 [DOI] [PubMed] [Google Scholar]
- 36.Roy A, Heckman MG, Roy V. Associations between the hospitalist model of care and quality-of-care-related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28-31 [DOI] [PubMed] [Google Scholar]
- 37.Rifkin WD, Burger A, Holmboe ES, Sturdevant B. Comparison of hospitalists and nonhospitalists regarding core measures of pneumonia care. Am J Manag Care 2007;13(3):129-132 [PubMed] [Google Scholar]
- 38.Scheurer DB, Miller JG, Blair DI, Pride PJ, Walker GM, Cawley PJ. Hospitalists and improved cost savings in patients with bacterial pneumonia at a state level. South Med J. 2005;98(6):607-610 [DOI] [PubMed] [Google Scholar]
- 39.Lindenauer PK, Chehabeddine R, Pekow P, Fitzgerald J, Bengamin EM. Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists. Arch Intern Med. 2002;162(11):1251-1256 [DOI] [PubMed] [Google Scholar]
- 40.Sox HC. The hospitalist model: perspectives of the patient, the internist, and internal medicine. Ann Intern Med. 1999;130(4, pt 2):368-372 [DOI] [PubMed] [Google Scholar]