Abstract
Purpose: To expand knowledge concerning the significance of kin relationships in caregiving, this study assessed predictors of the timing of institutionalization for persons with dementia. The focus was on whether use of adult day care by wives and daughters holds the same implications for placement. Design and Methods: Guided by a caregiving stress process model, primary objective and subjective stressors, secondary stressors, caregiver well-being, and use of day care services were included as predictors. Cox proportional hazards models were tested using a sample of 371 community-dwelling caregivers, including 141 wives and 230 daughters and daughters-in-law. Results: The main effect of kinship was found to be significant before interactions were introduced. Adult day care use at Time 1, role captivity, role overload, and social impact were subsequently found to interact with kinship. Analyses indicated that wives who used adult day care placed their husbands to a nursing home earlier than their counterparts. Among daughters, however, those who used adult day care were more likely to postpone the placement. The influence of role overload was also stronger in wives than in daughters in predicting the timing of placement. A similar pattern was observed in the interaction between social impact and kinship. Implications: The results demonstrate that factors influencing nursing home placement may vary according to the caregiver's familial relationship to the relative. Different approaches may be needed when targeting wife vs. daughter caregivers, especially when designing adult day care programs.
Keywords: Predictors of nursing home placement, Spouse caregivers, Cognitively impaired elders, Dementia
One of the major challenges faced by family caregivers of elders with disability is the decision to institutionalize. Although placement is difficult for most caregivers, the meaning of institutionalization is likely to be different, depending on the kin relationship between caregiver and care receiver. The two most common groups of caregivers, wives and daughters, have very different relationships and obligations, and may differ as well in the resources they have available for providing care and in other demands on their time. Although one of the goals of respite programs such as adult day care services (ADSs) is to delay institutional placement, little is known about how kin relationship might affect its timing. At the program level and from a broader policy perspective, understanding how factors such as kin relationship might affect the placement decision may lead to development of better targeted services that could delay, where appropriate, the use of more expensive institutional care. The present study examines whether kin relationship affects the timing of nursing home placement for caregivers who enroll a relative into an ADS program compared with caregivers not using ADS.
Studies of predictors of nursing home placement have generally found that persons with dementia who have more functional limitations, more severe cognitive impairments and more problematic behaviors such as wandering and aggression (Gaugler, Kane, Kane, Clay, & Newcomer, 2003; Gaugler et al., 2000; Wolinsky, Callahan, Fitzgerald, & Johnson, 1993), and fewer social supports (e.g., Colerick & George, 1986; Hanley, Alecxih, Wiener, & Kennell, 1990; Pot, Deeg, & Knipscheer, 2001) are more likely to be placed. Characteristics of caregivers also play an important role in the placement decision (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995; Gaugler, Kane, Kane, Clay, & Newcomer, 2005; Hebert, Dubois, Wolfson, Chambers, & Cohen, 2001; Pot et al., 2001; Toseland, McCallion, Gerber, & Banks, 2002; Yaffe et al., 2002). Studies suggest that nursing home placement is more likely to occur when the caregivers of persons with dementia are older, have lower levels of physical functioning, and poorer self-reported health (Gaugler et al., 2000; Gaugler, Kane, et al., 2003; Herbert et al., 2001). Higher levels of caregiver burden (McFall & Miller, 1992; Schulz et al., 2004; Yaffe et al., 2002) as well as caregivers’ appraisals of caregiving stressors such as role captivity or role overload (Gaugler et al., 2000) are also associated with greater risk for nursing home placement.
From a service perspective, there has been considerable interest in whether use of programs such as ADSs can delay institutionalization. At a policy level, delay or prevention of placement can reduce overall costs for long-term care, while potentially promoting better quality of life for older people. Previous studies, however, of the effects of ADS and other respite services, such as in-home care, on placement have shown mixed results. Some studies reported no association between use of respite services and the timing of nursing home placement (Hedrick, et al., 1993; Weissert, Wan, Livieratos, & Katz, 1980). Lawton, Brody, and Saperstein (1989) and Kosloski and Montgomery (1995), however, found small but significant delays in nursing home placement when various respite services, including ADS, were used. In contrast, some studies report that respite care actually can precipitate institutionalization (Gaugler & Zarit, 2001; Gaugler et al., 2003; Montgomery & Borgatta, 1989; Zarit, Stephens, Townsend, Greene, & Leitsch, 1999). These latter studies suggest an interplay between severity of symptoms and service use. People who use ADS or other respite services are more likely to have greater cognitive and physical impairment in the first place and thus are at greater risk for nursing home placement. Zarit and his colleagues found that one reason that ADS does not reduce institutionalization is that caregivers seek out this help too late in their relative's disease (Zarit et al., 2003). It may also be that use of ADS serves as a trial placement for some caregivers, helping them take a step toward institutionalizing their relative. ADS users may also be more favorably inclined to use other services, including placement (Gaugler, Kane, et al., 2003).
Type of relationship between caregiver and care receiver may also affect placement. The most consistent finding with respect to relationship draws from the fact that the majority of family caregivers are women (Stone, Cafferata, & Sangl, 1987). The two largest groups of caregivers are wives and daughters or daughters-in-law of care receivers (Stone et al., 1987). The reasons and the resources they have for keeping their relatives in the community, or for placing them, may differ between these two groups. Wives, for example, are more likely than daughters or daughters-in-law to be in frail health and to have instrumental activities of daily living (IADLs) or activities of daily living (ADLs) impairments themselves, due to their more advanced age. Consequently wives may be more likely than daughters to relinquish caregiving due to health reasons (Burton, Zdaniuk, Schulz, Jackson, & Hirsch, 2003; Schneider, Murray, Banerjee, & Mann, 1999). Daughters or daughters-in-law, in contrast, are more likely to have competing demands between caregiving and their other social roles such as own marriages, parenting roles, and work (Baring, MacEwen, Kelloway, & Higginbottom, 1994; Reid & Hardy, 1999; Stephens, Franks, & Townsend, 1994).
These differences in physical ability and social roles among spouse and daughter or daughters-in-law caregivers may influence service utilization especially the ADS and nursing home placement in various ways. However, few studies have examined whether the use of services such as ADS by spouse and daughter caregivers of persons with dementia has a similar or different effect on the timing of placement. Therefore, the goal of the present study was to examine predictors of placement and, in particular, to determine whether the use of adult day care by wives and daughters or daughters-in-law holds the same significance for nursing home placement.
Methods
Procedures
The study drew upon data originally collected for the Adult Day Care Collaborative Study (ADCCS; Zarit, Stephens, Townsend, & Greene, 1998). Adult Day Care Collaborative Study was designed to evaluate the effectiveness of ADSs on family caregivers and their relatives with dementia. The study used a quasi-experimental design. The treatment group comprised caregivers who were enrolling their relative with dementia into an ADS program in a Northeastern state that has a well-developed network of ADS programs and provides subsidies to assist families in paying for it. Because random assignment was not possible, the control group consisted of caregivers of persons with dementia living in another state that had similar social and demographic characteristics but fewer available ADS for patients with dementia at the time the study was conducted. Neither group was aware of the existence of the other group.
Data were collected by means of in-person and telephone interviews. Trained interviewers conducted three in-person interviews: baseline (T1), after 3 months (T2), and after 12 months (T3). Caregivers in the treatment group began using ADSs at the baseline (T1). Phone contact was maintained with caregivers for another 12 months for a total observation period of 24 months.
Caregivers were eligible to participate in the study if (a) they had primary responsibility for the care recipient, (b) the care recipient had a diagnosis of dementia, (c) the caregiver received little or no formal (paid) help at the time of enrolling in the study, and (d) the care recipient was not bedridden. In addition, caregivers in the control group had to indicate a willingness to use ADS if a program were available and affordable. This last step was to increase the comparability of the treatment and control groups for propensity to use formal services. Detailed descriptions of the study design and procedure can be found in Zarit et al. (1998).
Sample
The current study focused on wives and daughters (including daughters-in-law). As noted, wives and daughters are the largest groups of caregivers, and there were sufficient numbers in each kin group in the ADCCS sample to examine long-term outcomes. The sample consisted of 371 caregivers, including 141 wives (76 day care users and 65 in the control group) and 230 daughters and daughters-in-law (98 day care users and 132 in the control group; Table 1). We included daughters-in-law in the sample because although the history of the relationship is different than for daughters, many of the same normative expectations and competing demands apply. During the 2-year period covered by the study, 187 caregivers (50.1% of the sample) institutionalized their relatives. Those care recipients who were institutionalized, averaged 348.14 days in the community.
Table 1.
Explanatory and Outcome Characteristics of Sample and Mean differences (N = 371)
|
M (SD) |
|||||||
| All | Relation |
No–Day Care Sample |
Day Care Sample |
||||
| Wives (n = 141) | Daughters (n = 230) | Wives (n = 65) | Daughters (n = 132) | Wives (n = 76) | Daughters (n = 98) | ||
| Caregiver age | 58.52 (12.76) | 71.36 (8.35) | 52.13 (9.36)** | 68.46 (9.06) | 52.51 (9.89)*** | 71.01 (8.43) | 51.92 (9.05)*** |
| Caregiver education | 13.17 (2.12) | 12.70 (2.41) | 13.78 (1.98) | 12.92 (1.92) | 13.74 (1.89)** | 12.28 (2.40) | 13.47 (2.02)*** |
| Days in the community before placement | 341.68 (237.85) | 318.74 (208.91) | 356.74 (252.82)** | 392.33 (186.03) | 330.00 (208.73) | 259.97 (215.31) | 388.81 (303.97)*** |
| Months of caregiving | 40.05 (38.81) | 46.92 (37.65) | 35.84 (38.98)** | 50.14 (35.57) | 40.78 (43.34) | 44.17 (39.37)** | 29.18 (31.21)** |
| ADL problems at T1 | 7.28 (2.09) | 7.17 (2.24) | 7.34 (1.99) | 6.92 (2.19) | 7.14 (2.13) | 7.38 (2.28) | 7.62 (1.76) |
| Behavior problems at T1 | 6.92 (2.76) | 6.72 (2.79) | 7.05 (2.74) | 6.35 (2.79) | 6.68 (2.74) | 7.03 (2.77) | 7.54 (2.67) |
| Role captivity at T1 | 6.85 (2.64) | 6.67 (2.77) | 6.96 (2.55) | 6.12 (2.75) | 6.64 (2.42) | 7.14 (2.72) | 7.39 (2.67) |
| Role overload at T1 | 21.63 (3.43) | 21.64 (3.43) | 21.63 (3.44) | 21.05 (3.38) | 20.92 (3.50) | 22.14 (3.42) | 22.59 (3.13) |
| Social impact at T1 | 32.21 (4.54) | 31.62 (4.44) | 32.57 (4.57)* | 30.60 (4.29) | 31.92 (4.61)* | 32.49 (4.41) | 33.44 (4.38) |
| Anger rating at T1 | 7.67 (2.9) | 7.18 (2.90) | 8.06 (2.84)*** | 6.63 (2.67) | 7.87 (2.68)*** | 7.75 (3.03) | 8.30 (3.02) |
| CES-D rating at T1 | 17.20 (11.69) | 19.79 (11.76) | 15.62 (11.39)*** | 16.63 (10.64) | 14.14 (10.11) | 22.52 (12.07) | 17.62 (12.70)* |
Notes: ADL = activities of daily living; CES-D = Center for Epidemiological Studies-Depression scale.
*p < .05. **p < .01. ***p < .001.
Measures: Predictors of Nursing Home Placement
In selecting measures to predict the timing of placement, we were guided by the caregiving stress process model of caregiving (Pearlin, Mullan, Semple, & Skaff, 1990). This widely used framework for studying family caregivers views care-related stress as the result of an unfolding multidimensional process. The main elements of the model include background characteristics, primary stressors (objective and subjective stressors directly related to caregiving), secondary stressors (reflecting the encroachment of caregiving stressors onto other domains of life), resources, and outcomes. Primary objective stressors are the demands that are directly related to the caregiving situation such as care demands and behavioral disturbance, whereas primary subjective stressors are the caregivers’ internal responses to those demands. These primary stressors, in turn, may spill over into other areas of the caregiver's life, leading, for example, to conflict or strain in carrying out work, social network, or other family roles what Pearlin and colleagues call secondary stressors.
Both primary and secondary stressors contribute to caregiving outcomes, such as feelings of depression and emotional distress. All these factors can also contribute to longer term outcomes such as nursing home placement. The effects of stressors can be modified by resources, including social support and services that may provide relief to caregivers. Background characteristics, including the kin relationship of caregiver to care receiver, can affect how this process unfolds, including the subjective meanings caregivers give to stressors and the resources they have for containing the effects of care-related stressors.
For the current study, we selected variables from Pearlin and colleagues’ (1990) caregiver stress process model that were most likely to be related to the placement decision. All measures except for timing of placement were drawn from the initial interview when participants enrolled in the study. For ADS users, that was also the point at which they enrolled their relative into a day program.
Background and Context Variables.—
Variables assessing background and context reflect antecedent or current conditions that are hypothesized to influence the experiences of the caregiver and care recipient. For the present study, we included (a) kinship of caregiver to care receiver and (b) duration of care (months since the care recipient's symptoms began to require care, as reported by the caregiver).
Because age and education variables were confounded with kin relationship, these background characteristics were not included in the analyses.
Primary Objective Stressors.—
These stressors represent conditions of potential hardship that flow directly from the needs of the patient and demands of caregiving. Two measures of primary stressors were used: (a) the care recipient's ability to perform ADLs and (b) the care recipient's behavior problems, as reported at the baseline interview.
Activities of daily life. Caregivers rated the degree to which their relative needed assistance with 10 IADLs and personal ADLs. A 3-point Likert rating was used to indicate if the relative was able to perform the activity without help, needed some assistance, or was unable to perform the activity without help. Items were drawn from existing scales (Lawton, Brody, & Saperstein, 1989) and were selected to reflect functions appropriate to a dementia sample. A total count of ADL functioning was computed, with higher scores indicating greater impairment (α =.86).
Behavior problems. Caregivers reported the presence or absence during the past month of 14 behavior problems associated with dementia (e.g., “becoming angry or aggressive”). Items were drawn from the Revised Memory and Behavior Problems Checklist (Teri et al., 1992). A total count of reported behavior problems was computed (α = .69).
Primary Subjective Stressors.—
Primary subjective stressors reflect the perceived impact of direct care-related stressors (primary objective stressors). Two measures of appraisals of primary stressors were used.
Role captivity. This three-item scale was developed by Pearlin and colleagues (1990). The scale measures the extent to which caregivers feel trapped and constrained in the caregiving role (e.g., “I wish I were free to lead a life of my own”). Caregivers reported the extent to which they had felt this way during the past week using a 4-point Likert rating: never, just a little, somewhat, and all the time. The potential range of score was 3–12, with higher scores indicating more role captivity (α = .82).
Role overload. This seven-item scale assesses the extent to which the demands of caregiving are exhausting caregivers’ time and energy (e.g., “I have more things to do than I can handle”). It includes four items developed by Pearlin and colleagues (1990) and three items developed for the study (e.g., “I can count on a block of time to use as I like”). The range of responses was same as for role captivity. The potential range of scores was 7–28, with higher scores indicating more overload (α = .71).
Secondary Stressors.—
Only one indicator of secondary stressors, social impact, was used. This eight-item scale assesses the extent to which caregiving interrupted caregivers' social activities outside the caregiving role (e.g., visit with friends, religious activities). For each item, respondents reported the extent to which caregiving had interrupted activities during the past week: a lot more time than desired, little more time than desired, about the same, a little less than desired, and lot more less time than desired (α = .79).
Another important secondary stressor that is often mentioned in the literature is work–caregiving strain. Because many daughters in the sample worked outside the home, and most wives did not, this variable was confounded with kin relationship and therefore was not used in the analyses.
Psychological Distress.—
Two measures of psychological distress were used.
Anger. Based on previous work that suggested that caregivers score consistently higher on anger than non-caregiving controls (e.g., Anthony-Bergstone, Zarit, & Gatz, 1988), a four-item anger scale was included. The scale was adapted from the Hopkins Symptom Checklist (SCL-90; Derogatis, Lipman, & Covi, 1973) by Pearlin and colleagues (1990), and measures feelings of anger and irritation (e.g., “I had temper outbursts I could not control”). Caregivers reported how often each statement was true in the past week on a 4-point scale ranging from not at all to very much. Summary scores could range from 4 to 16, with higher scores indicating greater anger (α = .78).
Depression. Depressed mood was assessed with the Center for Epidemiological Studies-Depression scale (Radloff, 1977). This 20-item scale has been widely used with a variety of populations, including caregivers (Lawton et al., 1989). Caregivers reported how often they experienced each symptom in the past week on a 4-point Likert scale ranging from rarely or none of the time to most or all of the time. The potential range of scores was 0–60, with higher scores representing greater depressive symptomology (α = .92).
Outcome Measure: Time Until Placement
Time until placement was measured by the number of days from entry into the study until either institutionalization or completion of the 2-year period from the time of the first interview. Dates of institutionalization were identified during regular telephone contact that was maintained with participants for the 2-year period.
Analysis
Data analyses proceeded in two steps. First, descriptive statistics were examined for baseline stressors, indicators of well-being, and usage of day care. Next, a Cox proportional hazards model, one type of event history analysis, was used to analyze predictors of the timing of placement during the 2-year course of the study. A number of factors suggested the appropriateness of the Cox approach. First, not all participants in the study were institutionalized before the study period ended. The Cox approach incorporates censored cases (those who do not experience the targeted event) as well as those who experience the event. The dependent variable in an event history analysis thus is a combination of time and whether the event occurs. Censored observations were assigned a length of time representing their duration of participation in the analysis, but these cases were not coded as having experienced the event. The Cox proportional hazards model examines the product of an unknown function of time and the exponent of a linear combination of risk variables.
Caregiver characteristics, primary objective stressors, ADS use, primary subjective stressors, secondary stressor, and psychological well-being were entered, in successive steps. We hypothesized that caregivers who experience more ADL problems and behavior problems of care recipient are more likely to use the ADSs. Thus, ADS use was entered after controlling for the effects of primary objective stressors. Interactions of relationship to care recipient (wives and daughters) and other covariates were included at the last step of the analysis to investigate if kin relationship moderated the effects of ADS use and other key predictors on the timing of placement.
Results
Sample Characteristics
The demographic characteristics of the sample are shown in Table 1. When compared with caregivers who were daughters, wives on average had been providing care for more months since symptom onset (M = 46.92, SD = 37.65), reported less social interruption due to caregiving (M = 31.62, SD = 4.44), and were more depressed (M = 19.79, SD = 11.76) at baseline. In addition, when compared with daughter caregivers, wives have placed their care recipients into nursing home earlier. Additional t test and chi-squares were conducted to examine the differences between wives and daughters who accessed or did not access ADSs. Among day care users, wives were more depressed.
Predictors of Institutionalization
As a first step, we examined zero-order correlations among all the variables to identify possible problems with collinearity as well as to learn more about the association among predictors (Table 2). All the intercorrelations were in the low to moderate ranges, with none exceeding .59, and so no variables were excluded from the subsequent analysis.
Table 2.
Correlation Among Covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| 1. Caregiver relationshipa | — | −.09 | −.01 | .03 | −.06 | .15** | .10* | .09 | .14** | −.09* |
| 2. Duration of careb | — | .13** | .03 | −.10* | .01 | .07 | .06 | .02 | .04 | |
| 3. ADL problems | — | .31** | .08 | .03 | .18** | .21** | .09** | .08 | ||
| 4. Behavior problems | — | .12** | .26** | .28** | .27** | .24** | .29** | |||
| 5. Adult day care usec | — | .11** | .18** | .13** | .11* | .17** | ||||
| 6. Role captivity | — | .38** | .37** | .40** | .49** | |||||
| 7. Role overload | — | .56** | .35** | .51** | ||||||
| 8. Social impact | — | .25** | .40** | |||||||
| 9. Anger | — | .59** | ||||||||
| 10. Depression | — |
Notes: ADL = activities of daily living.
1 refers to wives and 2 refers to daughters.
Duration of care refers to the months of caregiving since the diagnosis.
1 = not enrolled in an adult day care services at Time 1; 2 = enrolled in an adult day care services at Time 1.
*p < .05. **p < .01. ***p < .001.
Table 3 shows the six steps in the Cox regression, and includes unstandardized beta coefficients, standard errors, and the relative risk of institutionalization (exp[β]). Positive coefficients are associated with decreased survival time, which in this case refers to decreased time until placement. Conversely, negative coefficients indicate an increased time until institutionalization. The relative risk refers to the estimated likelihood associated with the timing of placement.
Table 3.
Cox Regression by Models
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
Model 6 |
|||||||||||||
| B | SE | Exp(B) | B | SE | Exp(B) | B | B | Exp(B) | B | B | Exp(B) | B | B | Exp(B) | B | B | Exp(B) | |
| Caregiver characteristics | ||||||||||||||||||
| Kinshipa | −.44 | .16 | .64*** | −.53 | .16 | .59*** | −.53 | .16 | .59*** | −.53 | .16 | .59*** | −.57 | .17 | .57*** | 2.93 | 1.6 | 18.70 |
| Duration of careb | −.01 | .01 | .99 | −.01 | .01 | .99* | −.01 | .01 | .99 | −.01 | .01 | .99 | −.01 | .01 | .99 | −.01 | .01 | .99 |
| Primary objective stressor | ||||||||||||||||||
| ADL dependencies | .06 | .04 | 1.06 | .04 | .04 | 1.04 | .05 | .04 | 1.05 | .05 | .04 | 1.05 | .09 | .05 | 1.10 | |||
| Behavior problems | .09 | .03 | 1.09** | .08 | .03 | 1.08* | .06 | .03 | 1.06 | .06 | .03 | 1.07 | .09 | .04 | 1.1* | |||
| Adult day care use at T1 | .49 | .16 | 1.65** | .49 | .17 | 1.64** | .52 | .17 | 1.68** | 1.07 | .26 | 2.91*** | ||||||
| Primary subjective stressors | ||||||||||||||||||
| Role captivity at T1 | .08 | .03 | 1.09* | .09 | .04 | 1.09** | .04 | .05 | 1.04 | |||||||||
| Role overload at T1 | −.02 | .03 | .98 | −.01 | .03 | .99 | .−.06 | .05 | .94 | |||||||||
| Secondary stressor | ||||||||||||||||||
| Social impact | .02 | .02 | 1.02 | .02 | .02 | 1.02 | .07 | .03 | 1.08* | |||||||||
| Psychological distress | ||||||||||||||||||
| Anger | .01 | .03 | 1.01 | .03 | .04 | 1.04 | ||||||||||||
| Depression at T1 | −.01 | .01 | .99 | −.01 | .01 | .99 | ||||||||||||
| Interaction | ||||||||||||||||||
| Daughter × Duration of Care | −.01 | .01 | .99 | |||||||||||||||
| Daughter × ADL | −.07 | .09 | .94 | |||||||||||||||
| Daughter × Behavior Problems | −.05 | .07 | .96 | |||||||||||||||
| Daughter × Adult Day Care Use at T1 | −1.10 | .36 | .33** | |||||||||||||||
| Daughter × Role Captivity | .15 | .07 | 1.16* | |||||||||||||||
| Daughter × Role Overload | .14 | .07 | 1.16* | |||||||||||||||
| Daughter × Social Impact | −.12 | .05 | .89* | |||||||||||||||
| Daughter × Anger | −.03 | .07 | .97 | |||||||||||||||
| Daughter × Depression | −.03 | .02 | .97 | |||||||||||||||
| χ = 9.55 (2)** | Δχ = 12.67 (2)** | Δχ = 9.41 (1)** | Δχ = 7.69 (3) | Δχ = 1.28 (2) | Δχ = 26.29 (9)** | |||||||||||||
Notes: ADL = activities of daily living.
1 refers to wives and 2 refers to daughters.
Duration of caregiving refers to the months of caregiving since the diagnosis.
*p < .05. **p < .01. ***p < .001.
In the first model, relationship to the care recipient was significant. Compared with daughters or daughters-in-law, wives placed their husbands into a nursing home at an earlier point in time. The second model introduced the set of primary objective stressors. With the primary objective stressors introduced, relationship to the care recipient still remained significant and duration of care also became significant. Behavior problems, one of the two primary objective stressors, was significantly associated with placement. Caregivers who had provided care to their relatives for longer periods of time actually kept their relatives in the community longer. Caregivers who reported that the care recipient had higher rates of behavior problems placed their relatives into the nursing home earlier.
When ADS use was added in Model 3, duration of care was no longer significant but relationship to the care recipient, behavior problems, and adult day care use at Time 1 were all significant. Caregivers who used ADS were more likely to place their relatives into nursing homes earlier. The fourth model added primary subjective stressors and secondary stressors. Although kin relationship and adult day care use at Time 1 were still significant, only the role captivity stressor made a significant contribution. Caregivers who felt greater role captivity at baseline placed their relatives into the nursing home earlier.
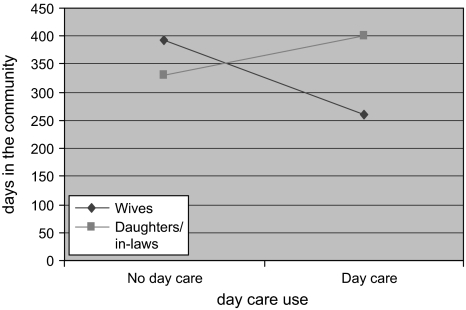
Inclusion of the two indicators of caregiver distress in Model 5 did not contribute significantly to the prediction of timing. In the last step (Model 6), we added interaction terms. With these interactions in the model, the main effect for kin relationship on timing of placement was no longer significant but several interactions reached statistical significance. For example, kin relationship by day care interaction was significant. As shown in Figure 1, wives who used day care placed their husbands into a nursing home sooner than wives who did not use day care. For daughters and daughters-in-law, however, the opposite was true. Daughters who used day care delayed placement longer than did daughters not using day care.
Figure 1.
Interaction: types of relationship and day care use to placement.
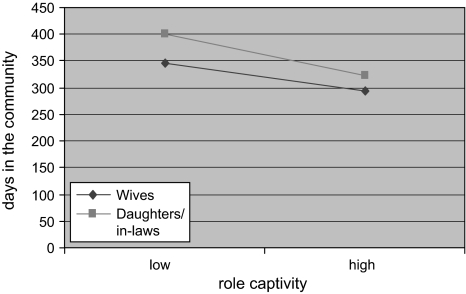
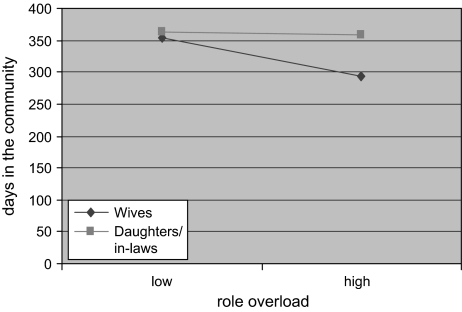
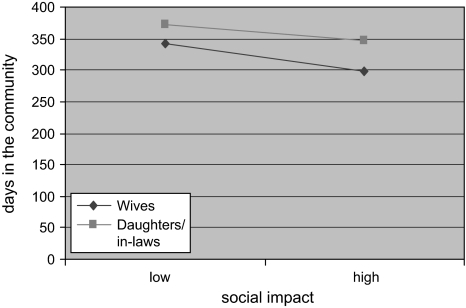
There were also significant interactions for relationship and role captivity and overload. When role captivity level was high, both wives and daughters put their care recipient into nursing home earlier, but when role captivity was low, daughters were likely to keep their parent in the community longer (Figure 2). In contrast to the findings for role captivity, when role overload was high, only wives placed their husbands earlier (Figure 3). There were no differences between wives and daughters when overload was low: Both kept their care recipients in their homes longer. Finally, the interaction of social impact and caregiver relationship was similar to that found for role overload. Both wives and daughters kept their care recipient in the community longer when social interruption was low. However, wives who reported more interruption in social activities placed their husbands into nursing home sooner (Figure 4).
Figure 2.
Interaction: types of relationship and role captivity to placement.
Figure 3.
Interaction: types of relationship and role overload to placement.
Figure 4.
Interaction: types of relationship and social impact to placement.
Discussion
The current study investigated whether kin relationship and ADS use affected the timing of nursing home placement of persons with dementia. Past research on placement of older adults with dementia had found social characteristics and caregiver stressors as potential predictors of institutionalization (Gaugler et al., 2003, 2005). Prior work also found little or no delay in nursing home placement due to use of ADS or other respite services (Gaugler et al., 2003; McCann et al., 2005). Little attention, however, has been given to the question of whether the risk factors differ according to the caregiver's relationship to the care recipient, the use of respite services such as ADS, or their interaction.
As might be expected, the analysis revealed that nursing home placement is a complex process involving multiple predictors from different domains. Several variables had the expected direct effects on the timing of placement. For example, caring for someone with more behavior problems was associated with shorter trajectories to nursing home placement. Some of the most interesting findings, however, emerged from interactions of predictor variables and relationship. Of particular relevance for this investigation were the results of the kin relationship by ADS interaction. For wives, ADS use shortened the time to placement. These results suggest that ADS may serve as a stepping-stone to institutionalization, at least for wives. For daughters, in contrast, the effect of ADS use was to delay institutionalization. It is also noteworthy that prior to entering the interaction terms, ADS use was associated with earlier placement. One reason for the mixed implications of ADS use for nursing home placement in prior studies may be that caregivers were analyzed as a single group. As seen in the present study, the effects of the delay of placement among daughters would likely be offset by the shorter time to placement among wife caregivers. Only by considering wives and daughters separately do the effects of ADS use on placement become apparent.
One important consideration in interpreting these findings is that wives and daughters enrolled their relative into ADS at different points in their own caregiving careers. This difference was statistically controlled in the analyses because the duration of care variable was entered into the analyses prior to the interaction terms. At the same time, it may be that, as suggested earlier, wives who select to use ADS view it as a trial institutionalization, which then allows them to take a more permanent step to place their husband in a nursing home. They may feel they have fulfilled their obligation and are ready to let go. Daughters selecting to use ADS, in contrast, may be more likely to be looking for ways to free up time for addressing competing obligations, including work, and other family and social obligations.
The other interactions of stressors and kin relationship also suggest the complexity of the decision to place a relative in a nursing home. The social impact of caregiving had both a direct effect on timing of placement and a significant interaction with kin relationship. Surprisingly, it was wives, and not daughters, who were more likely to place their husbands into nursing home sooner when they reported that the impact of caregiving on social activities was greater. This last finding bears additional scrutiny. Despite the longstanding finding that women in general maintain larger social network than do men (e.g., Antonucci & Akiyama, 1987; Gottlieb & Green, 1984; Shye, Mullooly, Freeborn, & Pope, 1995), there is extensive evidence that dementia brings with it an increasing social isolation for both caregivers and care recipients (Bass, Noelker, & Rechlin, 1996; Drentea, Clay, Roth, & Mittelman, 2006). This may be particularly problematic for wives, who may have already experienced other social losses as part of the normal process of aging. For example, in one study of loneliness in spousal caregivers, Beeson (2003) found that wife caregivers reported greater loneliness than husband caregivers. This finding suggests that their social network may no longer adequately meet their needs for contact and support. Daughters, in contrast, may be more socially engaged, if not overengaged. Brody (1981) speaks of the “sandwich” generation of middle-aged caregivers who are caught in multiple social demands. Another consideration is that for older adults, their spouse often has a primary role in their social network and in social activities. Hence, it is possible that wives in the sample, faced with their husband's inability to maintain many social and leisure activities, may have a more daunting task than daughters to sustain an adequate level of social activity. Although daughters report slightly more disruption of their social activities than do wives, they may still have more opportunities for satisfying social contact, including, for those daughters who are married, activities they share with their husbands.
The role of the two primary subjective stressors—role captivity and role overload—is also interesting. As in past research (e.g., Aneshensel et al., 1995), role captivity was a strong predictor of the timing of placement. With high levels of role captivity, both wives and daughters were more likely to place their relative sooner, but the effects of kin relationship were apparent with low captivity. In that case, daughters were less likely to place their parent than wives were to place their husbands. The results for role overload were somewhat different. There were no relationship differences in the timing of placement with low role overload, but wives were more likely to place sooner with high role overload. Role overload assesses the subjective impact that daily care tasks have on caregivers. This interaction of kin relationship placement and high role overload may reflect that wives may be wearing down physically and emotionally under the constant pressure of these tasks. These findings also address a larger issue that the stress process in caregiving is multidimensional and the effects of stressors on specific outcomes such as the timing of placement can differ. Although role overload and role captivity are moderately correlated (r = .18), high role overload is a stronger risk factor for wives, whereas low role captivity can be viewed as a protective factor for daughters.
There are some limitations to this study. The measures used in the study to predict the timing of nursing home placement were obtained up to 2 years prior to when placement might have occurred. Any changes in the caregiver's or care recipient's circumstances that occurred between the baseline and nursing home placement are not accounted for in the analyses. Another limitation is that the study only looked whether the persons with dementia were enrolling in an ADS program at the start of the study. Participants used the ADS programs for varying lengths of time and did not necessarily make transition to a nursing home when they discontinued ADS use (see Zarit et al., 1999). We do know, however, that no one in the control group had used ADS during the full period of observation. We also did not take into account the caregiver's experience of ADS use, including how helpful they felt it was for their relative and for themselves.
Finally, the study used a quasi-experimental design to evaluate the role of ADS on the timing of placement. Random assignment into a program such as ADS is generally not possible. Although quasi-experimental designs can be a valid alternative to traditional randomized trials, there are potential threats to internal validity. The main concern, therefore in this case, is that the interaction of kin relationship and ADS use may reflect the fact that different factors may lead wives and daughters to use ADS in the first place. As noted earlier, wives who choose to use ADS may be seeking to relinquish the care role or may be resorting to ADS only at a point where conditions have exceeded their ability to cope, whereas daughters may be seeking to maintain.
Despite these caveats, the current study has practical implication from a policy perspective. The finding that many daughters caring for a parent with dementia were able to delay placement suggests that ADS use, at least among daughters, had the potential to reduce the costs of more expensive institutional care. The different response of wives indicates that ADS programs may need to take a different approach with them to delay placement. One such approach has been described by Gitlin, Reever, Dennis, Mathieu, and Hauck (2006), who compared an enhanced ADS program that included counseling for the primary caregiver and other supportive services in addition to traditional ADS. The results indicated that spouse caregivers in the enhanced program had greater relief of stress and were more likely to use ADS for a longer period of time than caregivers in the control program.
The study highlighted the importance of relationship differences when studying caregiving, which in turn raise some issues to be considered in future studies. For example, other groups such as husband caregivers and son caregivers also need to be studied to examine how these groups might differ from wife and daughter caregivers. Indeed, although men are significantly less likely than women to become primary caregivers, from 25% to 30% of caregivers are men and relatively little is known about them in general, let alone about factors such as relationship differences. More importantly, although the current study showed that ADS use clearly had different implications for wives and daughters, the reason why wives and daughters use ADSs remains unclear. Identifying differences in the reasons for use of services such as ADSs may allow policy makers and providers to more appropriately target the needs of caregivers.
Funding
This project was supported by the National Institute on Aging Research Grant Program (1R03 AG 26332-01).
References
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. San Diego: Academic Press; 1995. [Google Scholar]
- Anthony-Bergstone CR, Zarit SH, Gatz M. Symptoms of psychological distress among caregivers of dementia patients. Psychology and Aging. 1988;3:245–248. doi: 10.1037//0882-7974.3.3.245. [DOI] [PubMed] [Google Scholar]
- Antonucci TC, Akiyama H. An examination of sex differences in social support among older men and women. Sex Roles. 1987;17:737–749. [Google Scholar]
- Baring J, MacEwen KE, Kelloway EK, Higginbottom SF. Predictors and outcomes of elder-care-based interrole conflict. Psychology and Aging. 1994;9:391–397. doi: 10.1037//0882-7974.9.3.391. [DOI] [PubMed] [Google Scholar]
- Bass DM, Noelker LS, Rechlin LR. The moderating influence of service use on negative caregiving consequences. Journals of Gerontology: Social Sciences. 1996;51:S121–S131. doi: 10.1093/geronb/51b.3.s121. [DOI] [PubMed] [Google Scholar]
- Beeson R. Loneliness and depression in spousal caregivers of those with Alzheimer's disease versus non-caregiving spouses. Archives of Psychiatric Nursing. 2003;17:135–143. doi: 10.1016/s0883-9417(03)00057-8. [DOI] [PubMed] [Google Scholar]
- Brody EM. Women in the middle and family help to older people. Gerontologist. 1981;21:471–480. doi: 10.1093/geront/21.5.471. [DOI] [PubMed] [Google Scholar]
- Burton L, Zdaniuk B, Schulz R, Jackson S, Hirsch C. Transitions in spousal caregiving. Gerontologist. 2003;43:230–241. doi: 10.1093/geront/43.2.230. [DOI] [PubMed] [Google Scholar]
- Colerick EJ, George LK. Predictors of institutionalization among caregivers of patients with Alzheimer's disease. Clinical Pharmacology and Therapeutics. 1986;58:228–236. doi: 10.1111/j.1532-5415.1986.tb04239.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale—Preliminary report. Psychopharmacological Bulletin. 1983;9:13–28. [PubMed] [Google Scholar]
- Drentea P, Clay OJ, Roth DL, Mittelman MS. Predictors of improvement in social support: Five-year effects of a structured intervention for caregivers of spouses with Alzheimer's disease. Social Science & Medicine. 2006;63:957–967. doi: 10.1016/j.socscimed.2006.02.020. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Edwards AB, Femia EE, Zarit SH, Stephens MA, Townsend A. Predictors of institutionalization of cognitively impaired elders: Family help and the timing of placement. Journals of Gerontology: Psychological Sciences. 2000;55:P247–P255. doi: 10.1093/geronb/55.4.p247. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Jarrott SE, Zarit SH, Stephens MAP, Townsend A, Greene R. Respite for dementia caregivers: The effects of adult day service on caregiving hours and care demands. International Psychogeriatrics. 2003;15:37–58. doi: 10.1017/s1041610203008743. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, Clay T, Newcomer R. Predicting institutionalization of cognitively impaired older people: Utilizing dynamic predictors of change. Gerontologist. 2003;43:219–229. doi: 10.1093/geront/43.2.219. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, Clay T, Newcomer R. The effects of duration of caregiving on institutionalization. Gerontologist. 2005;45:78–89. doi: 10.1093/geront/45.1.78. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Zarit SH. The effectiveness of adult day services for disabled older people. Journal of Aging and Social Policy. 2001;12:23–47. doi: 10.1300/J031v12n02_03. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Reever K, Dennis MP, Mathieu E, Hauck WW. Enhancing quality of life of families who use adult day services: Short- and long-term effects of the Adult Day Services Plus Program. Gerontologist. 2006;46:630–639. doi: 10.1093/geront/46.5.630. [DOI] [PubMed] [Google Scholar]
- Gottlieb NH, Green LW. Life events, social network, life-style, and health: An analysis of the 1979 National Survey of Personal Health Practices and Consequences. Health Education & Behavior. 1984;11:91–105. doi: 10.1177/109019818401100105. [DOI] [PubMed] [Google Scholar]
- Hanley RJ, Alecxih LM, Wiener JM, Kennell DL. Predicting elderly nursing home admissions. Results from the 1982-1984 National Long-Term Care Survey. Research on Aging. 1990;12:199–228. doi: 10.1177/0164027590122004. [DOI] [PubMed] [Google Scholar]
- Hebert R, Dubois MF, Wolfson C, Chambers L, Cohen C. Factors associated with long-term institutionalization of older people with dementia: Data from the Canadian Study of Health and Aging. Journals of Gerontology: Medical Sciences. 2001;56:M693–M699. doi: 10.1093/gerona/56.11.m693. [DOI] [PubMed] [Google Scholar]
- Hedrick SC, Rothman ML, Chapko M, Ehreth J, Diehr P, Inui TS, et al. Summary and discussion of methods and results of the Adult Day Health Care Evaluation Study. Medical Care. 1993;31:SS94–SS103. [PubMed] [Google Scholar]
- Kosloski K, Montgomery RJ. The impact of respite use on nursing home placement. Gerontologist. 1995;35:67–74. doi: 10.1093/geront/35.1.67. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM, Saperstein AR. A controlled study of respite service for caregivers of Alzheimer's patients. Gerontologist. 1989;29:8–16. doi: 10.1093/geront/29.1.8. [DOI] [PubMed] [Google Scholar]
- McCann JJ, Hebert LE, Li YL, Wolinsky FD, Gilley DW, Aggarwal NT, et al. The effect of adult day care services on time to nursing home placement in older adults with Alzheimer's disease. Gerontologist. 2005;45:754–763. doi: 10.1093/geront/45.6.754. [DOI] [PubMed] [Google Scholar]
- McFall S, Miller BH. Caregiver burden and nursing home admission of frail elderly persons. Journals of Gerontology: Social Sciences. 1992;47:S73–S79. doi: 10.1093/geronj/47.2.s73. [DOI] [PubMed] [Google Scholar]
- Montgomery RJV, Borgatta EF. The effectives of alternative support strategies on family caregiving. Gerontologist. 1989;29:457–464. doi: 10.1093/geront/29.4.457. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pot AM, Deeg DJ, Knipscheer CP. Institutionalization of demented elderly: The role of caregiver characteristics. International Journal of Geriatric Psychiatry. 2001;16:273–280. doi: 10.1002/gps.331. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385. [Google Scholar]
- Reid J, Hardy M. Multiple roles and well-being among midlife women: Testing role strain and role enhancement theories. Journals of Gerontology: Social Sciences. 1999;54:S329–S338. doi: 10.1093/geronb/54b.6.s329. [DOI] [PubMed] [Google Scholar]
- Schneider J, Murray J, Banerjee S, Mann A. EUROCARE: A cross-national study of co-resident spouse caregivers for people with Alzheimer's disease: I—Factors associated with carer burden. International Journal of Geriatric Psychiatry. 1999;14:651–661. [PubMed] [Google Scholar]
- Schulz R, Belle SH, Czaja SH, McGinnis KA, Stevens A, Zhang S. Long-term care placement of dementia patients and caregivers health and well-being. Journal of the American Medical Association. 2004;292:961–967. doi: 10.1001/jama.292.8.961. [DOI] [PubMed] [Google Scholar]
- Shye D, Mullooly JP, Freeborn DK, Pope CR. Gender differences in the relationship between social network support and mortality: A longitudinal study of an elderly cohort. Social Science & Medicine. 1995;41:935–947. doi: 10.1016/0277-9536(94)00404-h. [DOI] [PubMed] [Google Scholar]
- Stephens MAP, Franks MA, Townsend AL. Stress and rewards in women's multiple roles: The case of women in the middle. Psychology and Aging. 1994;9:45–52. doi: 10.1037//0882-7974.9.1.45. [DOI] [PubMed] [Google Scholar]
- Stone R, Cafferata G, Sangl J. Caregivers of the frail elderly: A national profile. Gerontologist. 1987;27:616–626. doi: 10.1093/geront/27.5.616. [DOI] [PubMed] [Google Scholar]
- Teri L, Truax P, Logsdon R, Uomoto J, Zarit SH, Vitaliano PP. Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychology and Aging. 1992;7:622–31. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- Toseland RW, McCallion P, Gerber T, Banks S. Predictors of health and human services use by persons with dementia and their family caregivers. Social Science & Medicine. 2002;55:1255–1266. doi: 10.1016/s0277-9536(01)00240-4. [DOI] [PubMed] [Google Scholar]
- Weissert W, Wan T, Livieratos B, Katz S. Effects and costs of day-care services for the chronically ill: A randomized experiment. Medical Care. 1980;18:567–584. doi: 10.1097/00005650-198006000-00001. [DOI] [PubMed] [Google Scholar]
- Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. Changes in functional status and the risk of subsequent nursing home. Journals of Gerontology: Social Sciences. 1993;48:S94–S101. [PubMed] [Google Scholar]
- Yaffe K, Fox P, Newcomer R, Sands L, Lindquist K, Dane K, et al. Patient and caregiver characteristics and nursing home placement in patients with dementia. Journal of the American Medical Association. 2002;287:2090–2097. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Stephens MAP, Townsend A, Greene R. Stress reduction for family caregivers: Effects of adult day care use. Journals of Gerontology: Social Sciences. 1998;53:S267–S278. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Stephens MAP, Townsend A, Greene R, Leitsch SA. Patterns of adult day service use by family caregivers: A comparison of brief versus sustained use. Family Relations. 1999;48:335–361. [Google Scholar]