In a recent study (1), it was shown that anastomoses of small arteries with continuous suture can yield comparable results to those with the interrupted suture method. We report herein a technical detail of the continuous technique which has been useful for veins and arteries of all sizes. It has been particularly valuable in reconstructing the small vascular structures at the hepatic hilum during transplantation of the liver in children.
The technique is applicable only with monofilament polypropolene (Prolene), a suture material which has little adventitial pull and which slides easily through vessel walls. Suture materials, such as silk, which lack these qualities cannot be used.
Prolene sutures which evenly divide the vessels are placed and tied (Fig. 1). Half of the circumference is sewed with one of the end sutures. Its mate is used to construct the other half of the circumference (Fig. 2), and the two ends are tied together where they meet (Fig. 3). Arteries which can be rotated are sutured with the conventional external method. However, with some arteries and more commonly with veins, short vessel lengths may make it necessary to fashion the posterior anastomotic wall from inside the lumen (Fig. 1), using the last needle penetration to bring the suture to the outside. The intraluminal suturing is easily done (Fig. 1) with a previously described continuous everting technique (2) that has been used in preference to the Blalock continuous horizontal mattress suture method.
Fig. 1.
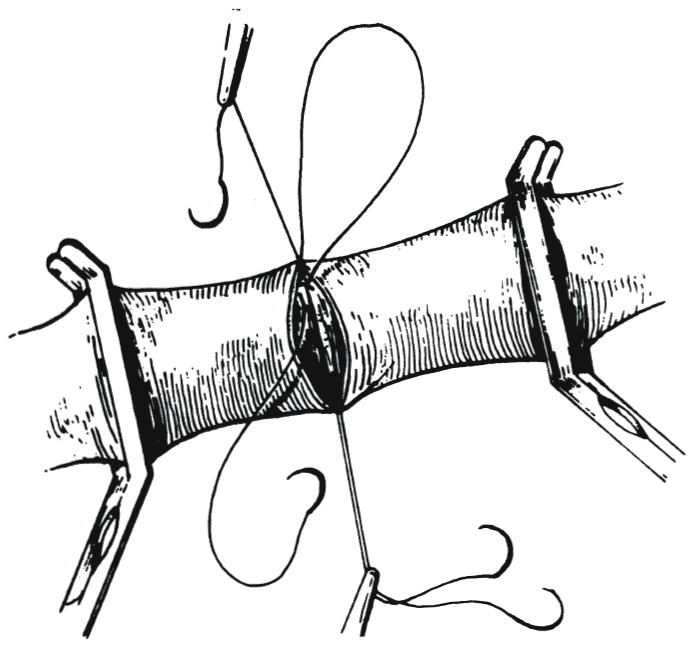
Intraluminal performance of posterior wall anastomosis after placement and tying of sutures.
Fig. 2.
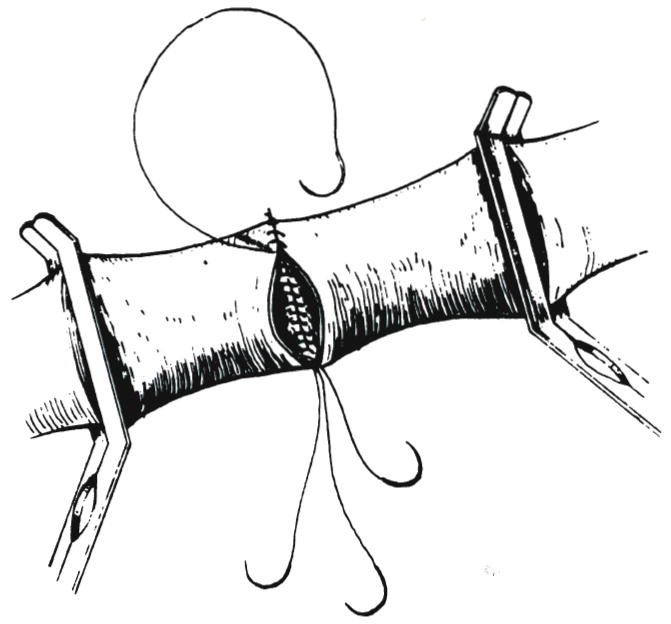
The mate of one end suture is used to construct the other half of the circumference.
Fig. 3.
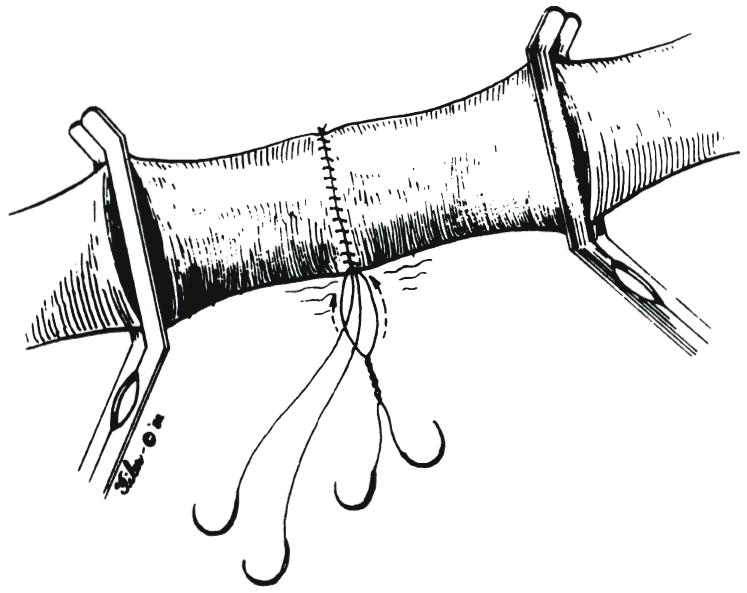
The two ends are tied together away from the wall.
No matter how the suturing has been done, the knot is deliberately placed away from the vessel wall (Fig. 3) at a distance of about one-third of the circumference or one diameter. The resulting large loop has been called the “growth factor” (Fig. 3). After blood flow is established through the anastomosis, the migration of this extra material into the suture line is stopped by the knot (Fig. 4). Gentle kneading of the suture line can expedite the process. Expansion and bulging of the suture line are immediately evident as the extra Prolene suture is taken up (Fig. 4).
Fig. 4.
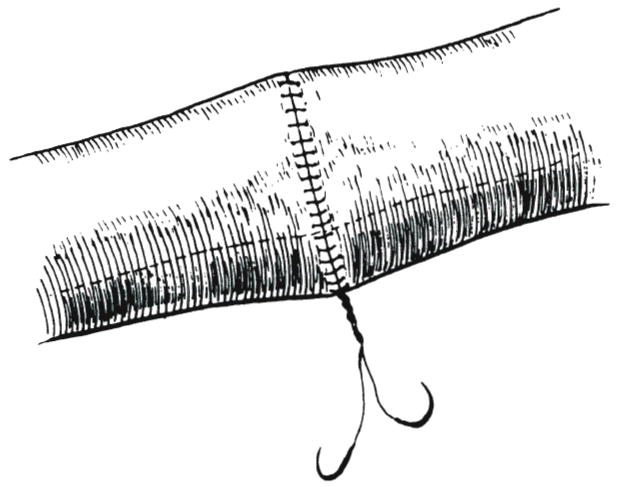
Expansion and bulging of the suture line are evident as the extra Prolene is taken up.
Observers of this seemingly heretical technique often have been aghast until they realized the advantages. Severe suture line bleeding is not common, but if present, it is apt to occur promptly and to be located near the knot, since the even distribution of the extra Prolene throughout the suture line requires time. If bleeding persists, the distracted lips of the vessels near the knot are coapted with simple sutures that do not include the original continuous suture. Otherwise, the Prolene would be restricted in its gradual self-adjusting movement.
Our greatest experience with this technique has been for liver transplantation, but the method has been valuable for arterial and venous anastomoses in many other circumstances. Particularly noteworthy has been a zero incidence of anastomotic failure in performing portacaval shunts in infants and small children whose age and size have been far below the standards cited (3) as minimal for a reasonable expectation of success.
SUMMARY
A technique of fine vascular anastomosis is described which allows expansion of the suture line.
Acknowledgments
Supported by research grants from the Veterans Administration; by project grant No. Am-29961 from the National Institutes of Health, and by grant No. RR-00084 from the General Clinical Research Centers Program of the Division of Research Resources, National Institutes of Health.
References
- 1.Lee BY, Thoden WR, Brancato RF, et al. Comparison of continuous and interrupted suture techniques in microvascular anastomosis. Surg Gynecol Obstet. 1982;155:353–357. [PubMed] [Google Scholar]
- 2.Starzl TE, Groth CG, Brettschneider L. An everting technique for intraluminal vascular suturing. Surg Gynecol Obstet. 1968;127:125–126. [PMC free article] [PubMed] [Google Scholar]
- 3.Clatworthy HW., Jr . Extrahepatic portal hypertension. In: Child CG, editor. Portal Hypertension. Philadelphia: W. B. Saunders Co.; 1974. pp. 257–261. [Google Scholar]


