Abstract
Background
Changing community norms to increase awareness of HIV status and reduce HIV-related stigma has the potential to reduce the incidence of HIV-1 infection in the developing world.
Methods
We developed and implemented a multi-level intervention providing community-based HIV mobile voluntary counseling and testing (CBVCT), community mobilization (CM), and post-test support services (PTSS). Forty-eight communities in Tanzania, Zimbabwe, South Africa and Thailand were randomized to receive the intervention or standard clinic-based VCT (SVCT), the comparison condition. We monitored utilization of CBVCT and SVCT by community of residence at 3 sites, which was used to assess differential uptake. We also developed Quality Assurance procedures to evaluate staff fidelity to the intervention.
Findings
In the first year of the study a four-fold increase in testing was observed in the intervention versus comparison communities. We also found an overall 95% adherence to intervention components. Study outcomes, including prevalence of recent HIV infection and community-level HIV stigma, will be assessed after three years of intervention.
Conclusion
The provision of mobile services, combined with appropriate support activities, may have significant effects on utilization of VCT. These findings also provide early support for community mobilization as a strategy for increasing testing rates.
Keywords: HIV prevention, HIV voluntary counseling and testing, community mobilization, post-test support services, HIV-related stigma
Introduction
There is no more compelling public health crisis in the world today than the HIV epidemic in sub-Saharan Africa and other parts of the developing world. Achieving important and meaningful reductions in HIV-1 incidence in countries impacted by the HIV/AIDS epidemic requires evidence-based approaches to prevention that mobilize communities to respond to this disease. While VCT has been recognized as a gateway to treatment1, and has been found to be safe and effective as an individual-level prevention intervention in developing countries2, 3, increasing awareness of HIV status at a community level has great potential for changing community norms.
Controlled studies of well-characterized approaches to community change are few in number4-8. Community-level approaches to prevention need to (a) tip the scale to establish as the community norm reductions in behaviors and attitudes (e.g., stigma, fears of getting tested for HIV, and subsequent disclosure) which lead to HIV transmission as well as increases in behaviors that help people maintain health (e.g., getting tested for and discussions about HIV); (b) support early adopters of behavior change so that others are encouraged to follow their lead; (c) ensure that individuals have the information and skills they need to initiate and maintain risk reduction; and (d) establish support systems to promote effective coping for those diagnosed with HIV9, 10. However, current HIV testing in many resource-constrained settings may be offered on a limited basis, often with no or inadequate counseling1.
Project Accept
Project Accept is the first international multi-site community randomized, controlled study to determine the efficacy of a multi-level structural HIV prevention intervention with HIV-incidence and stigma reduction as study endpoints. The intervention is directed at the community level, aimed at increasing knowledge of HIV status, changing community norms, and enhancing social support for people living with HIV/AIDS. By moving beyond individual behavior change to effect community-level change, we hope to address discrimination and inequities experienced in our study communities.
Methods
The intervention uses three major strategies: (1) community mobilization (CM) to enhance the uptake of VCT, thus increasing the rate of HIV testing and frequency of discussions about HIV; (2) community-based voluntary counseling and testing (CBVCT) to increase access to VCT and make awareness of HIV status more normative in community settings; and (3) comprehensive post-test support services (PTSS) that seek to improve the psychosocial wellbeing of those infected with HIV and assist HIV-negative people in maintaining their negative status.
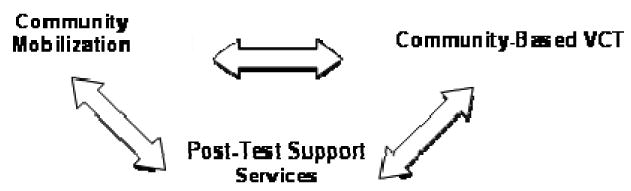
Figure 1 illustrates the synergy of these strategies to change community norms and reduce risk for HIV infection among all community members, irrespective of whether they participated directly in the intervention. Outcomes are evaluated at the community level, using community sampling methods.
Figure 1. Intervention Components.
The aims of the study are: (1) to test the hypothesis that communities receiving the Project Accept intervention, relative to those receiving the standard VCT (SVCT) services available to community members, will have significantly lower incidence of HIV infection; (2) to test the hypothesis that CBVCT communities, relative to SVCT communities, will at the end of the three-year intervention period report significantly less HIV-related stigma, fewer risk behaviors, higher rates of HIV testing, more favorable social norms regarding HIV testing, more frequent discussions about HIV, more frequent disclosure of HIV status, and fewer HIV-related negative life events; and, (3) to assess whether the Project Accept intervention is cost-effective compared to SVCT.
Project Accept utilizes an approach to community change11 based on diffusion theory12, which has been used to study social change in various settings, particularly in international development and public health. Diffusion is the process by which an innovation is communicated over time among members of a social system. Diffusion theory has been used as the rationale for many community-level interventions in the context of HIV prevention13. This model focuses on social networks, and utilizes opinion leaders as change agents. Although such elements are influenced by global cultural trends often portrayed through the media, immediate face-to-face interpersonal interactions occurring in natural social networks within communities are essential for inducing changed norms promoting and maintaining behavior change.
Research Sites
Kisarawe, Tanzania, is a rural district in the coastal region adjacent to a major transit route, approximately 100 km from Dar es Salaam; the area is largely agricultural. Mutoko, Zimbabwe is a rural district located in the Mashonaland East Province approximately 150 km from the capital, Harare; the area is also largely agricultural. Soweto, in Gauteng province, is the largest urban township in South Africa; historically, it was created to accommodate the work force for the city of Johannesburg. Vulindlela, South Africa, is a rural area located approximately 25 km from Pietermaritzburg and situated in the province of KwaZulu-Natal; employment opportunities are provided mostly through the forestry industry and in nearby towns. Chiang Mai is a province in northern Thailand; communities are located in rural areas near the border with Myanmar, largely populated by ethnic minorities.
Community Selection and Mapping
Project Accept is a randomized controlled study, in which 48 communities were randomized to either the Project Accept intervention or a clinic-based standard voluntary counseling and testing (standard VCT) control condition. The intervention design was informed by data from a community ethnography exercise which collected information about the communities through participatory mapping and transect walks. The data collected from this informative phase were used to identify appropriate sites for community-based testing and post-test support venues as well as to identify community groups or networks to collaborate with for community mobilization and for post-test support services. This community participatory phase was also instrumental in laying the groundwork for community partnerships critical to the intervention. Information from participatory mapping and transect walks was also used to identify relevant community attributes, such as, geographic location, population density, access to roads and health services, socioeconomic status, and ethnic composition. Communities that shared common attributes were matched into pairs using site-specific criteria. Communities in each pair were later randomized by the statistics center to either control or intervention.
From a social perspective, a community was defined as a group of individuals who live in proximity to one another and participate in common practices, depend on one another, make decisions together, identify themselves as part of something larger than the sum of their individual relationships, and commit themselves to the group's well-being14. Sites used both social and geographical characteristics to define and choose community pairs that would participate in the study. Community pairs were chosen to be of approximately the same population size. More community pairs were needed in sites with small community populations than in sites with larger community populations. Tanzania selected ten communities; Zimbabwe, Soweto and Vulindlela (South Africa) each selected eight communities; and Thailand selected fourteen communities. The communities chosen within each site were selected to be sufficiently distant and isolated from each other so that there would be little cross-contamination, or little possibility that individuals from a control community would benefit from the activities in intervention communities.
Community Preparedness
All Project Accept sites undertook a rigorous program of community preparedness and involvement activities, with the goals of building and maintaining long-term collaborative partnerships between health and social services, study communities, and Project Accept researchers. Staff members from all study sites were provided with training and received ongoing supervision in implementing the community preparedness and involvement protocol designed specifically for this study. Community preparedness and involvement activities included geographic and social mapping exercises, identification of key stakeholders, establishment of a multilayer community advisory structure, and ongoing community sensitization activities about the study. Community working groups were established for each site, comprised of diverse members of both intervention and comparison study communities. Community working groups play an important role in keeping researchers informed about community issues that could impact the study and keep the community informed about study-related matters. Each site has also established an external advisory committee made up of provincial and national governmental and nongovernmental policy makers who are regularly updated on study progress. The external advisory group has an important contribution to make in ensuring that the results of the research can be promptly translated into public policy should the intervention be found effective.
The intervention is being delivered over a period of three years in each community. HIV incidence will be evaluated from a single cross-sectional sample of serum specimens collected after the intervention has ended. The effect of the intervention on HIV incidence is not measured by prospectively following a cohort and administering repeated HIV tests because VCT is an integral part of both the intervention and primary endpoint assessment. A laboratory-based method will be utilized to assess the prevalence of recent infection – in essence, a measure of HIV incidence. While the intervention is offered to anyone over the age of 16, the post-intervention assessment will be conducted among a probability sample of 18-32 year olds from each community regardless of whether or not they participated in the intervention. Thus, the study will evaluate the effect of the Project Accept intervention on HIV incidence in the general population of young adults, which carries the highest relevance to public health policy.
Theoretical Foundations for Intervention
The Project Accept intervention has strong theoretical roots. While the overall community-level approach is based on diffusion theory, each of the components of the proposed intervention has its own rationale with different theoretical underpinnings. The approach is multi-leveled to maximize the potential for a number of positive behavioral outcomes as well as a reduction in HIV transmission. Table 1 outlines the relationship between theory, intervention and predicted outcomes.
Table 1. Intervention Theories.
| Theory | Intervention | Assessment |
|---|---|---|
| Tipping point for social change – maximizing the proportion of individuals who know HIV status will influence norms mediated by social networks16 | Easy Community Access to VCT to increase the percentage of the population aware of HIV status through increased availability of VCT in community settings |
|
| Diffusion of innovation – early adopters of innovative behavior influence others in their social network15 | Community outreach and mobilization using outreach coordinators and recruiting early testers as community outreach workers |
|
| Social action model – reduction in HIV transmission will be influenced by self-regulatory skills, contextual issues, and mood22 | Post-test support through post-test clubs with peer-based social support groups |
|
| Combined | Combined |
|
Diffusion of Innovation
The community mobilization component of the intervention is based on diffusion of innovation theory which contends that all communities have a small number of people who are innovators15. These innovators then influence others in their social network to adopt the innovation. Eventually, a threshold of behavioral adoption at the network level is reached which sustains the widespread uptake of a behavior. This is similar to what would be explained by the “law of the few” in tipping point theory, but puts greater emphasis on the importance of timing16. In particular, diffusion of innovation theory predicts that by enticing opinion leaders early on to adopt an innovative behavior deemed to be adaptive, the speed of uptake of the new behavior is facilitated. Such uptake effects have been documented with behaviors such as adolescent smoking, pregnancy, and sexual risk behavior17-19. Both negative and positive attitudes towards persons with stigmatized illnesses and behaviors are also influenced by these social dynamics20, 21. Thus, the community mobilization approach used in this study seeks to promote HIV testing and disclosure among early adopters, particularly if these individuals are influential and central to the larger social network. By penetrating social networks in communities, we hope to shift community norms to the extent that there is an increase in discussions about HIV and AIDS and a decrease in HIV-related stigma.
Tipping Point Theory
The community-based VCT component of the intervention is based on the theory that a “tipping point” occurs when a critical mass of adoption occurs in a social network16. It is affected by three factors: (1) the “law of the few”; (2) the “stickiness” of the behavior; and (3) the context of the innovation16. The “law of the few” refers to the role that a few core transmitters can have in the diffusion of key factors (such as microbes, behaviors, or beliefs) across a social network. Using this framework, we hope that behavior change among a core of HIV-infected individuals as well as a change in beliefs among community leaders should significantly slow the spread of the HIV epidemic in our study communities. The “stickiness” of a behavior refers to the social salience of the behavior, or how important it is deemed to be to the collective community. In this study we hope that increasing the proportion of individuals in a community who are aware of their HIV status will eventually increase the collective awareness that HIV is a real threat and that many HIV-infected people may belong to the social network. The context of the innovation refers to the physical and social context where behaviors occur; the context of innovations has a strong impact on the readiness to adopt them. We envisage that providing VCT in the context of where people live could change social norms around HIV testing, increase the frequency of discussions in communities and, ultimately decrease behavioral risk for HIV.
Social Action Theory
The Post-Test Support Services component of the intervention, which is open to both HIV negative and positive participants, is based on social action theory22, which views health-protective behavior as an interaction among three domains: (1) the self-regulatory capabilities of the individual, (2) the environmental context, and (3) responses to internal affective states. Self-regulatory factors for risk reduction include technical skills (such as appropriate and consistent condom use), social skills (such as negotiation and partner communication), and interpersonal problem solving skills. Consistent with previous research, we believe that improvements in self-regulatory capabilities of individuals can reduce the likelihood of sexual transmission acts23-26, and that support groups will help build these capabilities. Social contextual factors such as relationship status and transactional sex are likely to be linked to transmission acts. For example, injection drug users in Thailand who believe they are infected have cited a desire to protect their sexual partners as a major reason for condom use27. These contextual factors such as relationship issues are logical topics for discussion and problem solving in support groups. Negative affective and arousal states have been associated with decreased self-regulation of sexual behavior in both HIV-infected men28 and women29. Support groups, coping effectiveness training, and stigma reduction workshops should increase coping skills (self-regulatory capabilities), as well as decrease depression and stress (negative affective states) for people living with HIV, particularly if structured around issues likely to be confronted in the local environmental context 30.
Project Accept Intervention Components
Community Mobilization
CM uses community outreach to enhance the uptake of VCT, thus increasing the rate of HIV testing and frequency of discussions about HIV. This component is also designed to reduce stigma through community education and mobilization. Each site has a full time CM Coordinator who oversees three different groups of people who operate at different levels: (1) Community Working Groups consist of community leaders, gatekeepers, and community health workers identified during the preparatory phase of the study. Many of these people have been early adopters of the mobile VCT service and have influenced others in their social networks to come forward for counseling and testing. (2) Outreach workers engage in various activities, ranging from dissemination of information about HIV/AIDS, VCT and PTSS through pamphlets to one-on-one or group discussions in the community around the mobile testing locations, as well as through door-to-door organizing, or attending community meetings and social events (3). Community-based outreach volunteers (CBOVs) are groups composed of 3-5 community members active in each of the intervention communities. The volunteers are responsible for diffusing the innovation throughout their social networks and require training to do so. They are not project staff, but receive a small stipend based on local community standards. These volunteers are primarily recruited from the pool of people who have participated in VCT, regardless of HIV status. CBOVs report to the outreach workers.
Community-Based VCT (CBVCT)
This component is designed to remove structural barriers (fees, inconvenience, and waiting for results) and increases safety of VCT (anonymity, strict confidentiality and high-quality counseling) by offering VCT services at the village or community level. This easy access should increase rates of HIV testing, change social norms about testing, and increase frequency of discussions about HIV in communities. This approach also decreases behavioral risks for HIV31. VCT is provided at a variety of community locations.
Identification of suitable CBVCT locations is a joint effort of the research staff and the community mobilization groups. Locations include a variety of community settings such as marketplaces and transport venues. The four African sites offer VCT services in tents and caravans; the Thailand site uses community venues such as community centers or temples. Each site has developed a schedule for the mobile teams to visit each testing venue on a rotating basis. The fieldwork days are any combination of weekdays and weekends during the day and in the evenings to ensure that the mobile unit is accessible to community members who are employed. The schedule of visits to the mobile testing sites is distributed by the community mobilization team in advance of the mobile VCT unit visit.
Rapid testing and same-day test results are offered to all VCT participants. Participants who wish to receive their test results at a later time are given a card with the mobile team's schedule and invited to meet with the team again, either at another community venue or the same venue on a different day. In order to reduce stigma associated with seeking services from the mobile unit, the mobile VCT team emphasizes strongly, through its outreach efforts, that the mobile unit also welcomes participants who seek only information or counseling, without HIV testing. In this way, the mobile service is not simply viewed by the community as a place to get tested and receive HIV test results, but also as a place to receive personal and confidential counseling and education.
Each mobile team consists of VCT counselors, nurse phlebotomists, and community outreach workers. People in the vicinity of the van or community center are approached by an outreach worker and invited to take an HIV test. The outreach worker acts as a host, and is responsible for assigning a number to people who express interest in participating as well as giving them the study information sheet. The outreach worker answers questions and keeps people a reasonable distance away from the counseling spaces to ensure confidentiality and quiet. Those who agree to participate are invited to the testing venue (caravan, tent, room), where a study counselor administers informed consent in the participant's choice of language. Participants who agree to participate in the study are assigned a study ID number and receive pretest counseling from the study counselor before they are tested. The counselor then provides the participant with test results and post-test counseling.
The counseling session includes a condom demonstration, and participants are offered condoms to take home. The counselor assists the participants to understand the meaning of the test results, cope with the emotional impact of the result, and modify their risk-reduction plan as needed. Regardless of test results, all participants in the intervention communities are referred to Project Accept post-test support services. For participants who test positive, counselors assist in making a safe disclosure plan and provide appropriate referrals for health and social services as needed. This includes referrals to care and treatment services. Careful planning has been conducted at each site to map the current treatment and care services (including antiretroviral therapy provision), as well as other HIV prevention services available, and to ensure that those testing at Project Accept sites are appropriately referred.
Post-Test Support Services
This component is primarily designed to offer psychosocial support to improve the quality of life for individuals diagnosed with HIV, regardless of their HIV status. The expected outcomes include a reduction in social harm, an increase in social support through disclosure to those most likely to provide support, and a reduction in internalized stigma. Social support should also decrease the risk of further transmission. The objective in providing PTSS is to create a culturally appropriate support system for community members following their decision to take part in VCT. Individuals who have undergone HIV testing at Project Accept or other HIV testing venues are eligible to access the full range of PTSS services, regardless of their HIV status. Those who have undergone testing are designated as “members,” while those who have not undergone testing are “guests.” Those who have not tested can access the large information sharing group sessions offered at PTSS sites, but are not eligible to access other PTSS services until they have received HIV testing. Persons interested in testing are referred to Project Accept VCT. Five basic PTSS activities are offered:
Information-sharing group sessions are larger group meetings formed around specific age groups, serostatus, or other characteristics and topics. PTSS staff, a non-Project Accept guest lecturer, or PTSS participants may facilitate these groups. Topics include basic information on HIV/AIDS, health, nutrition, and other issues. One format makes use of formal presentations, in which participants identify a topic of interest relevant to their situation and the PTSS team leaders invite a guest speaker with expertise in that area. Another format uses group discussions, wherein participants share information, ideas, and opinions under the guidance of a facilitator.
Psychosocial support groups consist of 8-10 participants and meet 2-4 times per month, depending on member attendance levels. Support groups provide an opportunity for participants to meet and learn from others who are coping with similar circumstances. Groups are formed around the expressed preferences of the group members and staff expertise. Selected support group members receive additional training in group facilitation, so that these groups will eventually become self-sustaining peer-led entities. Currently, in Tanzania and Zimbabwe, these peer-led groups have collaborated with other community-based organizations to provide material support to members, ranging from supplies for farming activities, to financial grants for income generating activities and children's school fees and skills training.
Crisis counseling is provided as needed by PTSS counselors to individuals and couples. Counselors focus on channeling participants to other, less resource-intense PTSS activities. Counselors also provide referrals to non-Project Accept health and social services within the community.
Coping effectiveness training (CET) workshops are 8-hour sessions for PTSS members who wish to build skills in stress management and identifying additional sources of social support after testing. The workshops have been adapted culturally by local sites based on an intervention found to be effective in the US32-34. The workshops are intended to optimize participants' mental health outcomes and to build a core of community members with effective coping skills. Some sites offer these workshops in two day sessions to minimize time commitments.
Stigma reduction workshops have two goals: (a) to help individuals better understand and cope with HIV-related stigma, and (b) to build skills to help individuals disclose their HIV status in a safe environment. These workshops have been adapted by local site based on an approach developed in Tanzania35. Graduates of stigma reduction workshops are encouraged to participate in the CM activities that address community-level stigma.
Because PTSS does not have the capacity to meet all participants' needs, counselors make referrals to non-Project Accept organizations/agencies so that members can have their immediate, practical needs addressed. PTSS staff at each site has identified a core of community-based health and social service providers to which participants with special needs are referred. The PTSS coordinator and team leaders negotiate with the relevant service organization about the nature of services to be provided to PTSS participants.
Control Communities (SVCT)
Communities randomized to the SVCT arm (the “standard-of-care” arm) receive clinic-based VCT services in existing district hospitals, community-based health care centers, or other local health delivery facilities. For the sites in Zimbabwe and Tanzania, Project Accept set up clinic-based standard VCT at the same time as CBVCT, as no local services were available at he study sites. The other three sites had existing access to clinic-based VCT in district hospitals, community-based health care centers, or other local health delivery facilities. Each of these communities has access to SVCT that reflects local access to health care. SVCT counselors received training in the risk reduction model of counseling, similar to that of CBVCT counselors. No active recruitment for participation in the SVCT services is made beyond the standard procedures of each clinic for informing patients of services (i.e., telling individual patients that VCT is available, posting of a flyer in the clinic announcing VCT availability, etc). In addition, no study-sponsored active outreach or community mobilization, mobile VCT services, or special testing support services are provided in the SVCT arm. The procedures for counseling and HIV rapid testing for SVCT are the same as those in the CBVCT communities, except that referrals are limited to existing community agencies rather than study-related testing support services.
Site-Specific Adaptations
To accommodate the various site-specific sociocultural differences at the study sites, we allowed for site-specific adaptations with the conditions that (1) sites submit their written proposals for adaptation to the Intervention Core, (2) the core group reviews the proposals, makes a decision, and forwards the proposals to the Steering Committee for further review and, (3) the Steering Committee makes the final decision on whether to approve or reject the proposed adaptations. Site-specific adaptation is essential for ensuring that the intervention meets the local needs and culture.
Intervention Development
The Intervention Core established an Intervention Working Group to implement the intervention consistent with the overall research protocol. Representatives from each site included site principal investigators, project directors, and project coordinators. This participatory process allowed each site to address site-specific issues and helped the group to reach consensus on common elements to develop standard operating procedures (SOPs). The group worked via conference calls and face-to-face meetings. An early meeting developed consensus on revisions to the previous procedures of voluntary counseling and testing as well as pilot testing of mobile VCT in Zimbabwe and Thailand31, 36. The primary change was the addition of principles for motivational interviewing, which were included in the VCT model of counseling. A three-day meeting developed the standard procedures for community mobilization based on principles from diffusion theory and prior prevention intervention trials. In order to develop procedures for PTSS, the group conducted site visits to four existing post-test clubs in Bulawayo and Chitungwiza, Zimbabwe; Nairobi, Kenya; and Kampala, Uganda. The group then developed a set of standard procedures for PTSS in a three-day workshop. Each of the SOPs underwent subsequent review at each site.
Intervention Implementation
Prior to the start of the intervention, the Intervention Core conducted monthly startup conference calls with the sites to assist in preparations for launch of the intervention. Sites also submitted a monthly startup checklist to assess readiness to start the intervention. The Thailand site was the first to launch in early January 2006, closely followed by the Zimbabwe site in late January 2006, followed by the Tanzania site in March 2006, and the two South African sites (Soweto and Vulindlela) in May 2006. CBVCT and CM components were launched at the onset of the intervention, while PTSS activities were gradually phased in by the third month at all sites.
Intervention Quality Assurance
Team leaders or coordinators monitor staff performance in the VCT, PTSS, and Community Mobilization (CM) intervention components by observing sessions conducted with participants in the field and rating their fidelity to the protocol on multiple essential components using quality assurance evaluation forms scored with a 5 point scale defined as; 5= Excellent/Very Strong (100% adherence), 4= Satisfactory/Strong (95% adherence), 3= Satisfactory (90% adherence) 2= Poor: Needs additional supervision, 1= Unacceptable: Needs intensive supervision/training. The Intervention Coordination Director visits each site twice a year to evaluate the quality and consistency of the implementation of the intervention. The goal of the assessment is to ensure a minimum of 90% adherence to the protocol and standard operating procedures. These visits allow first-hand observation of the intervention components and maintain open relations with field staff. Population-adjusted intervention field hours by component are recorded on a monthly basis and feedback on staffing adjustments necessary to equalize field hours across intervention communities is provided. Monthly feedback reports from project directors and ongoing communication with field staff are used to identify and resolve a range of day-to-day issues at each site.
HIV Testing Algorithms and Quality Assurance
A parallel rapid HIV testing algorithm has been adopted by each site consistent with requirements approved by their Ministry of Health. Participants accessing VCT through the CBVCT and SVCT interventions receive rapid HIV testing with same-day results. For those sites using an EIA for the tiebreaker, venous blood specimens are collected, specimens labeled with a unique numeric indicator, and participants given appointments for return visits for results, with a process which maintains anonymity. All study sites are required to adhere to the standard procedures set by the HIV Prevention Trials Network (HPTN) regarding laboratory practices and biohazard containment. Quality assurance and quality control for the rapid tests in Project Accept have been performed three times per year (every 4 months) with testing of College of American Pathology proficiency panels provided and evaluated by the HPTN Laboratory Core. In brief, all staff testers are required to perform proficiency panels in field conditions using their site's rapid test kits with blinded sera. HIV testers are required to score 100% accuracy with the panels to remain certified to conduct rapid testing and retraining is offered until this proficiency is established.
Monitoring Intervention Utilization
Utilization data are reported monthly to assess uptake in all of the intervention components. Sites have developed a range of strategies designed to further increase utilization levels, including the provision of services on evenings and weekends, targeting venues with high uptake, and the provision of testing services at major local social events. Strategies developed by the sites are distributed to other sites to ensure coordination of effort. Utilization data are used to assess (1) the program-level demand for services, (2) patterns of individual service utilization, and (3) how closely the planned study operations match actual operations. Site teams receive monthly updates on their site's utilization data and can track and modify service provision for each component if necessary. These data also allow the sites and study team to monitor utilization across communities.
Results
Quality Assurance
For the first 5 months of the intervention, a random sample of 10% of VCT and PTSS sessions were selected for quality assurance evaluation, with 5% of sessions selected for evaluation thereafter. For the VCT component, VCT team leaders assess counselors' adherence and skill levels in 10 essential component areas (each with approximately 10 required activity or skill items). For the PTSS component, PTSS team leaders assess facilitators' adherence and skill levels in individual crisis counseling, group information sessions, coping-effectiveness training, and stigma reduction training (each with approximately 12 items). For the CM component, CM managers assess outreach workers' adherence and skill levels for 10 essential areas of community interaction and 6 areas of community referral and follow-up.
To evaluate fidelity to the intervention, individual item scores within an area were averaged to create a summary score and those summary scores were again averaged for an overall quality score. Team leaders and managers use the quality scores to identify strengths and weakness of individual staff and overall areas/component of the intervention and to create action plans for improvement, re-trainings, or more frequent supervision and support.
Overall quality for VCT and CM started out at 95% or greater and continued to improve as time progressed (see Figure 2) with a grand average score of 4.5 by 6 months. Quality scores for the PTSS component of the intervention were lower and experienced periodic fluctuations. Identified challenges to the fidelity of the PTSS component of the intervention trial were the wide range of activities included in the PTSS component and the novelty of the PTSS process. Often the fluctuations in quality for PTSS were associated with new staff hires or changes in responsibilities. Of note, by twelve months of the intervention, the quality score for PTSS activities had reached that of VCT and CM.
Figure 2. 12 Month Quality Assurance Scores by Intervention Component (VCT, CM and PTSS) at all 5 Study Sites.
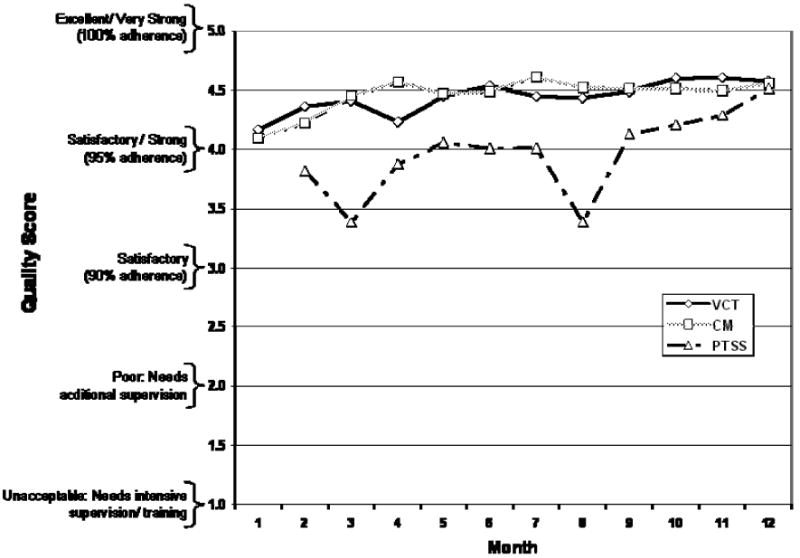
These quality assurance procedures allow for the identification of skills-training needs for VCT, PTSS and CM staff and relevant in-service skills trainings are discussed with the individual staff.
Utilization of VCT
In the three research sites (Zimbabwe, Tanzania and Thailand) where the study could monitor both CBVCT and SVCT uptake, a total of 21,391 community residents were observed to participate in HIV testing during the first 24 months of the intervention study. As seen in Figure 3, approximately a 3-fold increase is noted in HIV testing among residents of communities randomized to the intervention as opposed to the comparison communities. With regard to an estimate of the percent of community uptake among individuals 18 to 32 years of age tested, after 24 months we estimate 30 % in Tanzania, 39 % in Zimbabwe, and 33 % in Thailand. In Zimbabwe, the increase in utilization was greater than 10-fold. Figure 4 presents more detailed data on Zimbabwe, illustrating an almost even uptake of standard VCT among people from the control communities and from people in intervention communities who crossed over to control communities for testing. The standard clinic-based VCT is located in a central shopping area, and matched communities are equidistant from this center. By contrast, community-based mobile VCT, which is available only in the intervention communities, was accessed by 6,695 people from the intervention communities compared to only 17 who crossed over from the comparison communities to receive testing in the intervention community mobile testing venues.
Figure 3. Uptake of HIV Testing among Residents by Randomized Community – Thailand, Zimbabwe, Tanzania (initial 24 months).
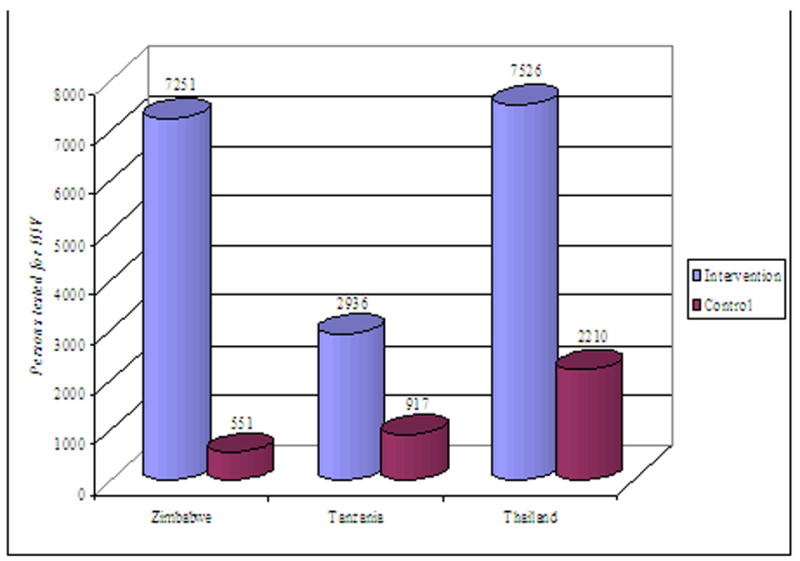
Figure 4. Zimbabwe – CBVCT and SVCT Utilization by Community of Origin (initial 24 months).
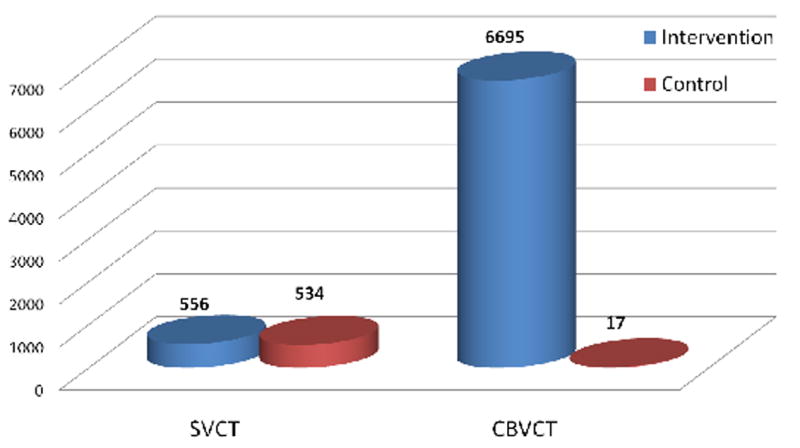
Overwhelmingly, communities randomized to the intervention utilized the mobile testing services provided by the intervention with very few testing at standard VCT sites in other communities. Thailand was the exception to this rule with 2,548 persons from communities randomized to the intervention testing at standard VCT sites in addition to the 4,978 intervention community persons participating in mobile HIV Testing. This is likely due to the fact that standard clinic-based HIV testing sites are available and located close to the participating Thai communities randomized to the intervention. Very few individuals in communities randomized to the control condition sought out HIV testing in neighboring communities randomized to the intervention and offering mobile HIV testing (17 in Zimbabwe, 7 in Tanzania, and 23 in Thailand).
Discussion
From a scientific perspective, community-level approaches have the potential to alter the course of the HIV epidemic—to have epidemic impact—in developing countries. This is the first international multi-site randomized, controlled, Phase III trial to determine the efficacy of a behavioral/social science intervention with an HIV incidence endpoint. Project Accept is being conducted in sites selected because they will allow for assessing HIV incidence as an endpoint. Individual-level behavioral or biological interventions, such as clinic-based VCT or pre-exposure prophylaxis, are strategies largely designed to respond to the epidemic one person at a time. A community-level intervention based on changing community norms can change the environmental context in which people make decisions about HIV risk.
Analysis of the process data collected in the first year of the study has been informative. A significant difference in the uptake of VCT in the intervention versus control communities was observed across all three countries providing early validation of the intervention's theoretical model. In addition, the utilization of standard clinic-based VCT available in the Thai communities by the residents of intervention communities in addition to mobile VCT suggests that diffusion of the idea of the importance of knowing one's HIV status is occurring. It is also reassuring to see that there is little contamination of residents from control communities resulting from crossing over to intervention communities to take advantage of free mobile HIV testing. This will ensure an accurate representation of the true effect of the intervention when the study is fully evaluated.
The major effort into developing and implementing the in-depth quality-assurance methodology has been rewarded with a wealth of information on the successes and challenges of implementing this complex intervention. The overall 95% adherence to essential intervention delivery components indicates that the wide range of activities contained within the intervention can be successfully and faithfully instituted in resource limited settings. The QA process has also been able to identify challenges to implementation, especially around PTSS activities, and has provided solutions to those challenges, primarily in early identification of enhanced training needs.
The community working groups have played an active role in disseminating information about the study to community members, including hosting public events to improve the visibility of the study and in advising our teams on how to improve communication with stakeholders. Community working group members contributed to community mobilization activities by helping to recruit community-based outreach volunteers, participated in the intervention, and subsequently referred others to our services. Finally, community working group members have been instrumental in assisting the study teams to troubleshoot problems that have arisen, as they are often the first to hear of rumors or misconceptions about the study.
Perhaps the most important lesson learned this far in the project has been the role of stigma in complicating the response to the epidemic, as evidenced by some people's initial reluctance to access PTSS for fear of being identified as HIV positive. However, through post-test support activities, stigma has been addressed by helping people talk about these fears. The fear of a positive test-result was also expressed as a fear of losing one's social support. The experience of individuals who had tested positive prior to introduction of the pilot phase of the intervention encouraged this fear. Many study participants described experiences of HIV-infected individuals being shunned by their friends and family. One young man said, “When you are sick there are very few relatives who will support you. Most will not want anything to do with you and they will tell you to go where you got the disease from.” However, participants in the pilot were linked to a local post-test club that helped them to overcome this fear. These services provided psychosocial support exactly when individuals who tested HIV-positive were most vulnerable to the effects of stigmatization by friends, family, and other community members. It was through these services that individuals learned to accept their HIV status, and experienced acceptance by others.
From the perspective of national AIDS control planners in these countries, evidence-based strategies that have maximum epidemic impact are critically needed. Country planners want interventions that are sustainable and can be adapted to the context of their local cultures. In this prevention trial, we not only test the efficacy of this intervention, but also the incremental cost-effectiveness of implementing such an approach in resource-poor countries. Project Accept is designed so that it can be used in resource-poor communities. Resources needed for the full implementation of Project Accept are relatively inexpensive, especially because the intervention relies on volunteer and peer support. Thus, we anticipate that these results will generalize to other resource-poor settings.
Acknowledgments
This research was sponsored by the U.S. National Institute of Mental Health as a cooperative agreement, through contracts U01MH066687 (Johns Hopkins University), U01MH066688 (Medical University of South Carolina), U01MH066701 (University of California, Los Angeles), and U01MH066702 (University of California, San Francisco). In addition, this work was supported by the HIV Prevention Trials Network (HPTN Protocol 043) of the Division of AIDS of the U.S. National Institute of Allergy and Infectious Diseases, and by the Office of AIDS Research of the U.S. National Institutes of Health. Views expressed are those of the authors, and not necessarily those of sponsoring agencies. We thank the communities that partnered with us in conducting this research, and all study participants for their contributions. We also thank study staff and volunteers at all participating institutions for their work and dedication.
Project Accept Study Group
Laurie Abler, MPH2
Christopher Bamanyisa, MA, AD1
Chris Beyrer, MD, MPH2
Adam W. Carrico, PhD7
David Celentano, ScD, MHS2
Suwat Chariyalertsak, MD, DrPH3
Alfred Chingono, MSc4
Lilliane Chovenye1
Kathryn Curran, MHS2
Thomas J. Coates, PhD5
Deborah Donnell, PhD6
Agnès Fiamma, MIPH5
Katherine Fritz, PhD, MPH2
Janet Frohlich, Dcur8
Becky Genberg, MPH2
Glenda Gray, MBBCH, FCPaeds(SA)9
Amy Gregowski, MHS2
Harry Hausler, MD, MPH10
Nora Margaret Hogan, PsyD1
Salim Abdool Karim, MBChB, PhD8
Sebastian Kevany, MPH7
Gertrude Khumalo-Sakutukwa, MSW, MMSc7
G.P. Kilonzo, MD, FRCP, Mmed, MBChB, BA1
Michal Kulich, PhD11
Tim Lane, PhD, MPH
Benjamin Link, MPH, MSW2
Tserayi Machinda, BSC Admin ACCA, MBA(wip)4
Suzanne Maman, PhD12
Jessie Mbwambo, MD1
James McIntyre, MBChB, MRCOG9
Joanne Mickalian, MA7
Precious Modiba, MA(SW)9
Simon Morfit, MPH, BA7
Stephen F. Morin, PhDr7
Audrey Pettifor, PhD, MPH12
Linda Richter, PhD8
Memory Sendah, MSc4
Basant Singh, Bsc, Msc2
Michael Sweat, PhD13
Greg Szekeres5
Andrew Timbe, MEd4
Heidi Van Rooyen, MA8
Surasing Visrutaratna, PhD3
Godfrey Woelk, PhD, MCOMMH, BSc4
Footnotes
Muhimbili University, College of Health Sciences
Johns Hopkins University, Bloomberg School of Public Health
Chiang Mai University, Research Institute for Health Sciences
University of Zimbabwe
University of California, Los Angeles
Statistical Center for HIV/AIDS Research & Prevention, Fred Hutchinson Cancer Research Center
University of California, San Francisco
Human Sciences Research Council
University of the Witwatersrand/Chris Hani Baragwanath Hospital
London School of Hygiene and Tropical Medicine
Charles University, Department of Probability and Statistics
University of North Carolina at Chapel Hill
Medical University of South Carolina
References
- 1.Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. Am J Public Health Oct. 2007;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grinstead OA, Gregorich SE, Choi K, Coates TJ Group TVH-CaTE. Positive and negative life events after counselling and testing: the Voluntary HIV-1 Counselling and Testing Efficacy Study. AIDS. 2001;15:1045–1052. doi: 10.1097/00002030-200105250-00013. [DOI] [PubMed] [Google Scholar]
- 3.Sweat M, Gregorich S, Sangiwa G, et al. Cost-effectiveness of voluntary HIV-1 counselling and testing in reducing sexual transmission of HIV-1 in Kenya and Tanzania. Lancet. 2000;356(9224):113–121. doi: 10.1016/S0140-6736(00)02447-8. [DOI] [PubMed] [Google Scholar]
- 4.O'Reilly KR, Piot P. International perspectives on individual and community approaches to the prevention of sexually transmitted disease and human immunodeficiency virus infection. J Infect Dis. 1996;174 Suppl 2:S214–222. doi: 10.1093/infdis/174.supplement_2.s214. [DOI] [PubMed] [Google Scholar]
- 5.Oakley A, Fullerton D, Holland J. Behavioural interventions for HIV/AIDS prevention. AIDS. 1995;9(5):479–486. [PubMed] [Google Scholar]
- 6.Farmer P, Leandre F, Mukherjee JS, et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet. 2001;358(9279):404–409. doi: 10.1016/s0140-6736(01)05550-7. [DOI] [PubMed] [Google Scholar]
- 7.Waldo CR, Coates TJ. Multiple levels of analysis and intervention in HIV prevention science: exemplars and directions for new research. AIDS. 2000;14 Suppl 2:S18–26. [PubMed] [Google Scholar]
- 8.Gregson S, Adamson S, Papaya S, et al. Impact and process evaluation of integrated community and clinic-based HIV-1 control: a cluster-randomised trial in eastern Zimbabwe. PLoS Med. 2007 Mar 27;4(3):e102. doi: 10.1371/journal.pmed.0040102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sweat MD, Denison JA. Reducing HIV incidence in developing countries with structural and environmental interventions. AIDS. 1995;9(Suppl A):S251–257. [PubMed] [Google Scholar]
- 10.Nelson KE, Celentano DD, Eiumtrakol S, et al. Changes in sexual behavior and a decline in HIV infection among young men in Thailand. N Engl J Med. 1996;335(5):297–303. doi: 10.1056/NEJM199608013350501. [DOI] [PubMed] [Google Scholar]
- 11.De Zoysa I, Phillips KA, Kamenga MC, et al. Role of HIV counseling and testing in changing risk behavior in developing countries. AIDS. 1995;9(Suppl A):S95–101. [PubMed] [Google Scholar]
- 12.Rogers EM. Diffusion of innovations. New York: Free Press; 1983. [Google Scholar]
- 13.Dearing JW, Meyer G, Rogers EM. Diffusion theory and HIV risk behavior change. In: DiClemente RJ, Peterson JL, editors. Prevention AIDS: Theories and methods of behavioral interventions. New York: Plenum Press; 1994. [Google Scholar]
- 14.Schaffer CR, Amundsen K. Creating Community Anywhere: Finding Support and Connection in a Fragmented World. New York: Tarcher/Perigee; 1993. [Google Scholar]
- 15.Valente TW. Social network thresholds in the diffusion of innovations. Social Networks. 1996;18(1):69–89. [Google Scholar]
- 16.Gladwell M. The tipping point: how little things can make a big difference. 1st. Boston: Little Brown; 2000. [Google Scholar]
- 17.Rodgers JL, Rowe DC, Buster M. Social contagion, adolescent sexual behavior, and pregnancy: a nonlinear dynamic EMOSA model. Dev Psychol. 1998;34(5):1096–1113. doi: 10.1037//0012-1649.34.5.1096. [DOI] [PubMed] [Google Scholar]
- 18.Rowe DC, Rodgers JL, Gilson M. Multivariate applications in substance use research: New methods for new questions. In: Rose JS, editor. Epidemics of smoking: Modeling tobacco use among adolescents. Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc.; 2000. pp. 238–258. [Google Scholar]
- 19.Rodgers JL, Rowe DC. Social contagion and adolescent sexual behavior: a developmental EMOSA model. Psychol Rev. 1993;100(3):479–510. doi: 10.1037/0033-295x.100.3.479. [DOI] [PubMed] [Google Scholar]
- 20.Doherty RW. Emotional contagion and social judgment. Dissertation Abstracts International: Section B: The Sciences and Engineering. 1996;56(10B):5831. [Google Scholar]
- 21.Rozin P, Markwith M, McCauley C. Sensitivity to indirect contacts with other persons: AIDS aversion as a composite of aversion to strangers, infection, moral taint, and misfortune. J Abnorm Psychol. 1994;103(3):495–504. doi: 10.1037//0021-843x.103.3.495. [DOI] [PubMed] [Google Scholar]
- 22.Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–946. doi: 10.1037//0003-066x.46.9.931. [DOI] [PubMed] [Google Scholar]
- 23.Barth RJ, Kinder BN. The mislabeling of sexual impulsivity. J Sex Marital Ther. 1987;13(1):15–23. doi: 10.1080/00926238708403875. [DOI] [PubMed] [Google Scholar]
- 24.Exner TM, Meyer-Bahlburg HF, Ehrhardt AA. Sexual self control as a mediator of high risk sexual behavior in a New York City cohort of HIV+ and HIV̂ gay men. J Sex Res. 1992;29(3):389–406. [Google Scholar]
- 25.Coates TJ, Aggleton P, Gutzwiller F, et al. HIV prevention in developed countries. Lancet. 1996;348(9035):1143–1148. doi: 10.1016/s0140-6736(96)02307-0. [DOI] [PubMed] [Google Scholar]
- 26.Quadland MC, Shattls WD. AIDS, sexuality, and sexual control. J Homosex. 1987;14(12):277–298. doi: 10.1300/J082v14n01_20. [DOI] [PubMed] [Google Scholar]
- 27.Vanichseni S, Des Jarlais DC, Choopanya K, et al. Condom use with primary partners among injecting drug users in Bangkok, Thailand and New York City, United States. AIDS. 1993;7(6):887–891. doi: 10.1097/00002030-199306000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Kalichman SC, Roffman RA, Picciano JF, Bolan M. Sexual relationships, sexual behavior, and HIV infection: HIV-seropositive gay and bisexual men seeking prevention services. Professional Psychology: Research & Practice. 1997;28(4):355–360. [Google Scholar]
- 29.Mellins CA, Ehrhardt AA. Families affected by pediatric acquired immunodeficiency syndrome: sources of stress and coping. J Dev Behav Pediatr. 1994;15(3):S54–60. [PubMed] [Google Scholar]
- 30.Feldman R, Manchester J, Maposhere C. Positive Women: Voices and Choices -- Zimbabwe Report. London: International Community of Women Living with HIV/AIDS; 2002. [Google Scholar]
- 31.Morin SF, Khumalo-Sakutukwa G, Charlebois ED, et al. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. J Acquir Immune Defic Syndr. 2006 Feb 1;41(2):218–224. doi: 10.1097/01.qai.0000179455.01068.ab. [DOI] [PubMed] [Google Scholar]
- 32.Rose CS, Ress B. HIV transmission risk behaviors among HIV-positive individuals: stress and coping in the aftermath of 9/11. J Assoc Nurses AIDS Care. 2002 Sep-Oct;13(5):25–31. doi: 10.1177/105532902236778. [DOI] [PubMed] [Google Scholar]
- 33.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Spring; 1984. [Google Scholar]
- 34.Center for AIDS Prevention Studies. Coping Effectiveness Training: Facilitator's Manual. San Francisco: University of California; 1997. [Google Scholar]
- 35.Parker R, Aggleton P, Attawell K, Pulerwitz J, Brown L. HIV/AIDS-related Stigma and Discrimination: A Conceptual Framework and an Agenda for Action. Washington, DC: Population Council, Horizons Program; 2002. May, [Google Scholar]
- 36.Kawichai S, Celentano DD, Chariyalertsak S, et al. Community-based Voluntary Counseling and Testing Services in Rural Communities of Chiang Mai Province, Northern Thailand. AIDS Behav. 2007 Sep;11(5):770–777. doi: 10.1007/s10461-007-9242-7. [DOI] [PubMed] [Google Scholar]


