Abstract
In the present study we found that double-stranded RNA-dependent protein kinase (PKR) regulates the protein expression level and the phosphorylation of Bcl-2 and exploits an anti-apoptotic role in human hepatocellular carcinoma cells (HepG2). Saturated free fatty acids (FFAs), e.g. palmitate, have been shown to induce cellular apoptosis in various types of cells by different mechanisms. We found palmitate down-regulates the activity of PKR, and thereby decreases the protein level of Bcl-2, mediated, in part, by the NF-κB transcription factor. In addition to the protein level of Bcl-2, the phosphorylation of Bcl-2 at different amino acid residues, such as Ser70 and Ser87, is also important in regulating cellular apoptosis. The decrease in the phosphorylation of Bcl-2 at Ser70 upon exposure to palmitate is mediated by PKR and possibly JNK, while the phosphorylation of Bcl-2 at Ser87 is not affected by palmitate or PKR. In summary, PKR mediates the regulation of the protein level and the phosphorylation status of Bcl-2, providing a novel mechanism of palmitate-induced apoptosis in HepG2 cells.
Keywords: palmitate, apoptosis, liver cell, HepG2, PKR, Bcl-2, phosphorylation of Bcl-2, NF-kappaB, JNK
Introduction
The double-stranded RNA-dependent protein kinase (PKR) is best known for triggering cell defense responses by activating cellular apoptosis during virus infection (1). Foreign double-stranded RNA (dsRNA), a by-product of viral RNA polymerases during virus replication, binds PKR, facilitates the homo-dimerization, auto-phosphorylation at Thr451 and Thr446, and thereby the activation of PKR (2, 3). The activated PKR, known as a eukaryotic initiation factor 2-alpha (eIF-2α) kinase, induces phosphorylation of eIF-2α) at Ser51 (3), which inhibits the initiation of RNA translation by the tRNA 40S ribosomal subunit. This function of PKR results in inhibition of general protein synthesis and induction of cellular apoptosis in many types of eukaryotic cells (3, 4). However, evidence is emerging, albeit controversial at this point, to suggest that PKR also has an anti-apoptotic role in mouse embryo fibroblasts and certain tumor cells (5-9).
As a Ser/Thr protein kinase, PKR is also known for its role in mediating signaling pathways (10) by interacting with proteins such as NF-κB, MAPKs, and PP2A (11-14). It is well established that PKR phosphorylates and thereby releases I-κB from NF-κB, and in so doing PKR activates NF-κB and promotes the translocation of NF-κB into the nucleus (11, 12). Upon activation of NF-κB by PKR, the transcription of a number of apoptosis-regulating genes, such as, FasL (15), p53 (16), and cIAPs (5) have been shown to be up-regulated. PKR has been reported also to play a crucial role in the phosphorylation of the 3 mitogen-activated protein kinases (MAPK) (JNK, ERK, and p38) upon ribotoxic stress (13). However, the mechanism by which PKR interacts with the major MAPKs, and whether its role is apoptotic or anti-apoptotic, is unclear. PKR also can phosphorylate the PP2A regulatory subunit B56α and thereby activate the catalytic subunit of PP2A, potentially leading to dephosphorylation of eIF-4E and arrest of translation (14).
In addition to dsRNA, PKR has been shown to be responsive to many other factors, e.g., endoplasmic reticulum (ER) stress (17, 18), cytokines such as tumor necrosis factor (TNF)-α (19) and interleukin (IL)-1 (20), deoxynivalenol (DON, or vomitoxin) (13) and lipopolysaccharide (20). In the present study, we show for the first time palmitate down-regulates the activity of PKR in HepG2 cells.
Saturated FFAs (e.g. palmitate) have been shown to induce apoptosis in many cell types, such as cardiac cells, pancreatic beta cells, breast cancer cells, and hepatocytes, and are associated with the development of a variety of diseases, such as diabetes, heart disease, and non alcoholic fatty liver disease (NAFLD) (21, 22). The mechanism by which palmitate induces apoptosis has been shown to be dependent on the cell type. For example, palmitate induces apoptosis by generating intracellular reactive oxygen species (ROS) in microvascular endothelial cells (EC) and retinal pericytes (23) but not in neonatal rat cardiomyocytes (24). Studies of palmitate-induced apoptosis in liver cells have focused predominantly on lysosomal permeabilization (25), intracellular metabolic pathways, such as beta oxidation (26), TG accumulation (27), and ceramide production (28, 29). In addition, we showed that in human hepatocellular carcinoma (HepG2/C3A) cell line, increased hydrogen peroxide (H2O2) and hydroxyl (*OH) radicals mediated the palmitate-induced lipotoxicity (30). However, the cytotoxicity, as well as apoptosis, was not completely prevented upon treating with mitochondrial complex inhibitors or free radical scavengers, suggesting that mechanisms other than ROS production in the mitochondria are contributing to the toxicity of palmitate.
More recent investigations implicated certain Bcl-2 family proteins in mediating the saturated FFA-induced apoptosis of liver cells. For example, palmitate-induced apoptosis in liver cells has been identified to be related to the activation (25, 31) of Bax and a decrease of the Bax antagonist Bcl-X(L) (25). In addition, elevated Bcl-2-interacting mediator of cell death (Bim), a pro-apoptotic Bcl-2 family protein, has been found to play a role in stearic and palmitic acid-induced apoptosis of several liver cell lines including HepG2 (31, 32), and this process has been determined to be dependent on the transcription factor, FoxO3a (31). In addition to these pro-apoptotic Bcl-2 family proteins, an anti-apoptotic member, Bcl-2, has also been identified as an important factor in regulating the apoptosis of HepG2 cells (33-35), although it has not been established whether palmitate has any effect on Bcl-2 in HepG2 cells. In pancreatic cells, the induction of apoptosis by palmitate has been shown to be associated with reduced anti-apoptotic Bcl-2 level (36). In the present study, we found a similar effect of palmitate on the level of Bcl-2 and furthermore, showed that palmitate also down-regulated the phosphorylation of Bcl-2 at Ser70, but not at Ser87, in HepG2 cells.
As one of the most important anti-apoptotic members in the Bcl-2 family, Bcl-2 protects cells against intrinsic apoptosis by maintaining the integrity of the mitochondrial membrane (37). The expression of the Bcl-2 gene has been shown to be regulated by different transcription factors, depending on the cell type (38-40). In liver tumor cell lines such as U937 and HepG2 cells, NF-κB has been identified as the central regulator of the transcription of the Bcl-2 gene (41, 42). Bcl-2 is expressed in progenitor cells in several self-renewing tissues and in certain tumor cells, including human hepatocellular carcinoma (HepG2) cells (43-46). Immunohistochemical studies indicate that Bcl-2 is not expressed in primary hepatocytes (43), although more recent study with “high-power” staining showed Bcl-2 expression in primary hepatocytes (47). In the present study, we confirm, by both RT-PCR and Western blotting, that HepG2 cells express Bcl-2, and propose a pathway through which palmitate regulates Bcl-2 protein in HepG2 cells.
Post-translational modification, e.g., phosphorylation, of Bcl-2 also plays a role in determining the anti-apoptotic role of Bcl-2 (48). Phosphorylation of Bcl-2 at the anti-apoptotic site, Ser70, sustains the anti-apoptotic role of Bcl-2 (49). On the other hand, phosphorylation of Bcl-2 at Ser87 is believed to reduce the anti-apoptotic function of Bcl-2, possibly by inhibiting the phosphorylation of Bcl-2 at Ser70 or destabilizing the Bcl-2 protein (50, 51). MAPKs have been proposed to mediate the phosphorylation of Bcl-2 (52-56), since the sequences surrounding both Ser70 and Ser87 residues of the Bcl-2 protein represent the consensus motif, X-X-S-P, recognized by MAPKs (56). PP2A, a Ser/Thr-specific protein phosphatase, has been shown to dephosphorylate Bcl-2 at both Ser70 (57) and Ser87 (51) residues.
In the present study, our data support the action of PKR as an anti-apoptotic factor and determine that PKR is involved in regulating the protein level and phosphorylation of Bcl-2 in HepG2 cells. There has been no evidence in the literature to date indicating whether palmitate has an effect on the activity of PKR. We show palmitate down-regulates the activity of PKR, which however does not alter the phosphorylation level of eIF-2α, and propose that the repression of PKR mediates apoptosis by regulating Bcl-2.
Results
Palmitate Induces Cytotoxicity and Apoptosis of HepG2 Cells
Previous work in our lab showed that palmitate induced cytotoxicity in HepG2 cells (30, 58), while unsaturated FFAs, e.g. oleate and linoleate, were not cytotoxic (30, 58). In a separate study, we found upon exposure to palmitate the HepG2 cells stained for Annexin-V (data not shown), which indicates phosphatidylserine externalization, a sign of early stage apoptosis. In the present study, we further found that palmitate increased LDH released and caspase-3 activity of HepG2 cells in a dose dependent manner, while oleate did not have a significant effect on LDH release and caspase-3 activity (Fig. 1 A and B), supporting that palmitate induces cytotoxicity and apoptosis in HepG2 cells. It has been confirmed also in the literature, that palmitate induces apoptosis of HepG2 cells (31, 32).
Figure 1. Effects of palmitate on cytotoxicity and apoptosis of HepG2 cells.
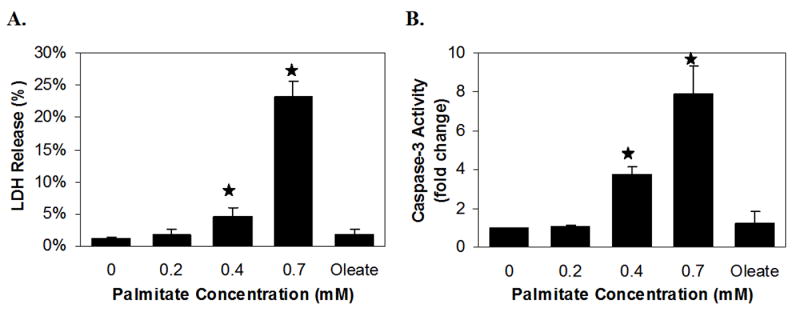
HepG2 cells were cultured in regular media until reaching approximately 90% confluency, and then exposed to different levels of palmitate or 0.7 mM oleate for 24 hours. The vehicle for the FFAs (0.7 mM BSA) was used as the control (i.e., regular media with BSA) (A, B). LDH release (A) and caspase-3 activity (B) were measured after treating with palmitate. Data expressed as averages of nine samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly higher than control, i.e., regular media with BSA, p<0.01.
Palmitate Decreases the Activity of PKR in HepG2 Cells
Palmitate decreased the phosphorylation of PKR at Thr451, which indicates the activity of PKR, in a dose-dependent manner (Fig. 2A), while unsaturated FFA, oleate, did not significantly affect the phosphorylation of PKR (Fig. 2B) in HepG2 cells. Considering the apoptotic effects of palmitate on HepG2 cells (Fig. 1B), we hypothesize that in HepG2 cells, PKR is involved in mediating the apoptosis induced by palmitate. To uncover the role of PKR in regulating apoptosis, gene silencing, and gene over-expression studies were performed.
Figure 2. Effects of palmitate and oleate on the activity of PKR.
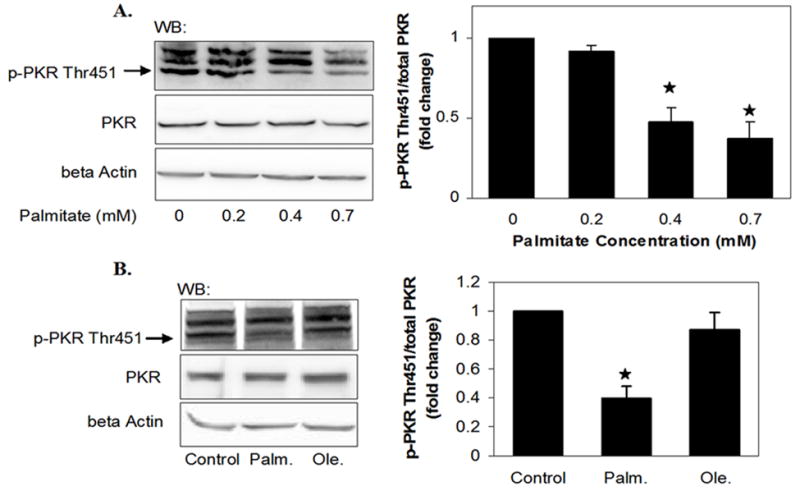
HepG2 cells were cultured in regular media until reaching 90% confluency and then exposed to different levels of palmitate (A), 0.7 mM palmitate or oleate (B) for 24 hours. The vehicle for the FFAs (0.7 mM BSA) was used as the control (i.e., regular media with BSA), in which the concentration of FFAs was 0 (A, B). After treatment, the cells were harvested, and western blot analysis was performed to detect the phosphorylated level of PKR. Quantified the level of p-PKR Thr451 by normalizing to the levels of total PKR and expressed as average of three samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly lower than control, i.e., regular media with BSA, p<0.01.
PKR is Anti-apoptotic in HepG2 Cells
The siRNA targeting PKR employed in the present study markedly inhibited the gene and protein expression of PKR, and thereby reduced the level of phosphorylated PKR (Fig. 3A). Silencing PKR with this siRNA increased the activity of caspase-3 significantly (Fig. 3B) but not the release of LDH (Fig. 3B), and induced fragmentation of chromatin DNA (Fig. 3B), suggesting that PKR has an anti-apoptotic role in HepG2 cells. To confirm the role of PKR in apoptosis, we over-expressed and rescued the PKR expression level in PKR-silenced cells and found that the caspases-3 activity was reduced to levels close to control (Fig. 3C). Taken together, these results suggest that PKR plays an anti-apoptotic role in HepG2 cells. To further confirm a catalytic role of PKR in regulating apoptosis, we inhibited the activity of PKR with a pharmaceutical inhibitor of PKR (59-61) and found that, similar to the siRNA of PKR, the PKR inhibitor also induced apoptosis in HepG2 cells, as evidenced by the caspase-3 activity and DNA fragmentation (supplementary Fig. 1). Considering the negative effect of palmitate on the activity of PKR, we therefore proposed that palmitate induces apoptosis, in part, by repressing PKR.
Figure 3. Role of PKR in cytotoxicity and apoptosis of HepG2 cells.

Reverse transfection of suspended HepG2 cells were performed with scrambled siRNA (Control) or siRNA of PKR for 24 hours and the transfected cells were cultured in regular media for another 24 hours (A, B). Cells were then harvested, and RT-PCR and western blot analysis were performed to detect the gene, protein and phosphorylation levels of PKR to confirm that the PKR gene was silenced and the activity of PKR was suppressed (A). LDH release, Caspase-3 activity, and DNA fragmentation were assayed (B). In (C), reverse transfection of scramble siRNA (■, control) or siRNA of PKR (▨, siPKR) was performed followed by forward transfection of empty vector pCMV6-XL5 (pCMV) or the plasmid containing PKR cDNA sequence (hPKR). Cells were then harvested and caspase-3 activity was assayed (C). Data expressed as average of three (A) or nine (B, C) samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly higher (B, C) or lower (A, C), than control, p<0.01. #, significantly lower than siPKR-CMV in Fig. C, p<0.01.
Palmitate Down-regulates the Protein Expression Level of Bcl-2
Palmitate decreased the protein level of Bcl-2 (Fig. 4A). Oleate did not have a significant effect on the protein level of Bcl-2 (Fig. 4B). It is unclear from the literature how palmitate would regulate the Bcl-2 protein. However, as illustrated in Figs. 2 and 4, palmitate, concomitantly, decreased the phosphorylation of PKR and the protein level of Bcl-2, suggesting a potential association between PKR and Bcl-2. To confirm this association and test the involvement of PKR in mediating the effect of palmitate on Bcl-2, gene silencing and over-expression of PKR were performed.
Figure 4. Effects of palmitate and oleate on the protein level of Bcl-2.
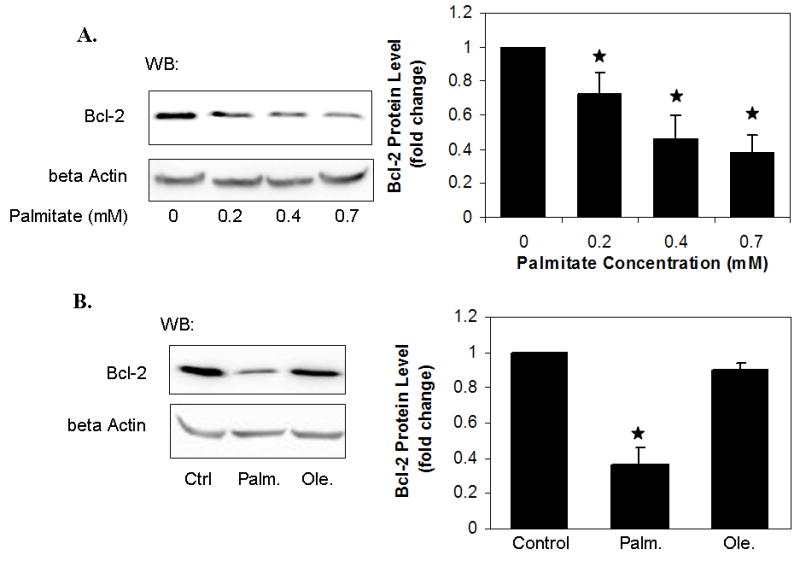
HepG2 cells were cultured in regular media until reaching 90% confluency, and then exposed to different levels of palmitate (A), 0.7 mM palmitate or 0.7 mM oleate (B) for 24 hours. The vehicle for the FFAs (0.7 mM BSA) was used as the control (i.e., regular media with BSA), in which the concentration of FFAs was 0 (A, B). After treatment, the cells were harvested, and western blot analysis was performed to detect the protein level of Bcl-2. Quantified Bcl-2 protein level by normalizing to beta actin levels and expressed as average of three samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly lower than control, i.e., regular media with BSA, p<0.01.
PKR is Involved in Mediating the Effects of Palmitate on the Protein Level of Bcl-2 in HepG2 Cells
Silencing the expression of the PKR gene with siRNA of PKR (Fig. 3A) down-regulated the mRNA and protein level of Bcl-2 (Fig. 5 A and B), suggesting that PKR positively regulates the mRNA expression (Fig. 5A), and in turn the protein level (Fig. 5B) of Bcl-2. Similarly, inhibiting the activity of PKR, with the PKR inhibitor, also suppressed the mRNA and protein level of Bcl-2 (Supplementary Fig. 2 A and B). Considering the repressive effect of palmitate on the PKR activity (Fig. 2), we hypothesize that the suppression of PKR activity mediates the negative effects of palmitate on Bcl-2 levels. To confirm our hypothesis that PKR is involved in the decrease of Bcl-2 by palmitate, we over-expressed the PKR gene in HepG2 cells (Fig. 5C) and exposed the cells to palmitate, and indeed found that the Bcl-2 level was rescued by over-expressing PKR (Fig. 5C). This suggests that the suppression of PKR activity indeed mediates the decrease of Bcl-2 induced by palmitate.
Figure 5. Involvement of PKR in regulating the protein level of Bcl-2.
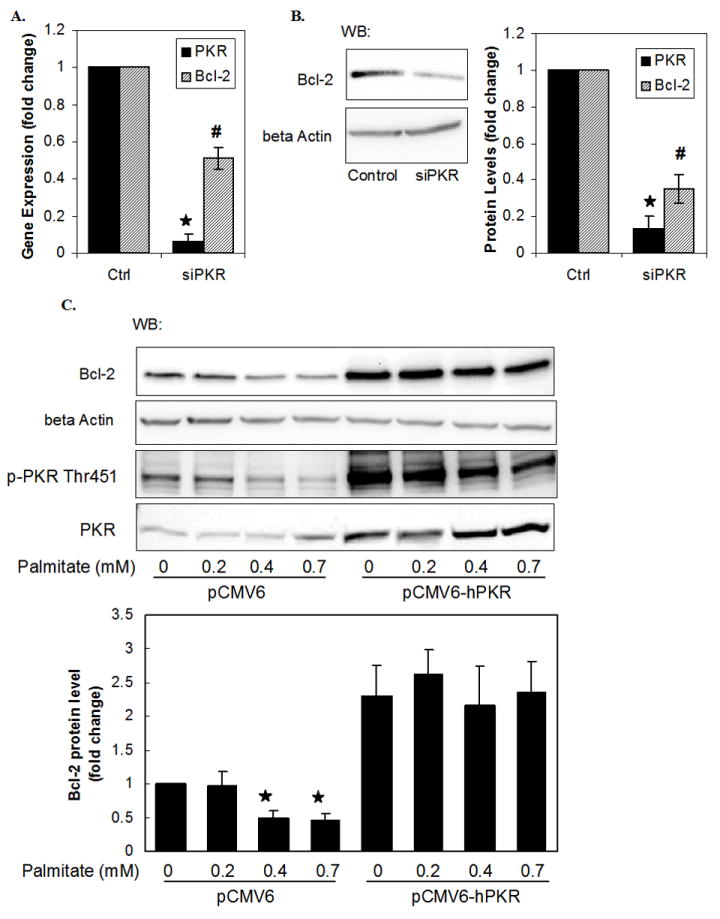
Reverse transfection of suspended HepG2 cells were performed with scrambled siRNA (Control) or siRNA of PKR for 24 hours and the transfected cells were cultured in regular media for another 24 hours (A, B). Cells were harvested, and RT-PCR (A) and western blot analysis (B) were performed to detect the gene (A) and protein (B) expression levels of PKR (■, also shown in Fig. 3C) and Bcl-2 (▨). In HepG2 cells, forward transfection of empty vector pCMV6-XL5 (pCMV6) or the plasmid containing PKR cDNA sequence (pCMV6-hPKR) was performed and the cells were then treated with different concentrations of palmitate for 24 hours (C). The vehicle for palmitate (0.7 mM BSA) was used as the control (i.e., regular media with BSA), in which the concentration of palmitate was 0 (C). Cells were then harvested, and western blot analysis was performed to detect the phosphorylation and protein level of PKR and the protein levels of Bcl-2 (C). Gene expression data expressed as average of nine samples ± SD from three independent experiments. Quantified the protein levels of Bcl-2 by normalizing to beta actin and expressed as average of three samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★ and #, PKR or Bcl-2 levels significantly lower than control, p<0.01.
Thus far, we showed that palmitate down-regulated the activity of PKR, which played an anti-apoptotic role in HepG2 cells. We identified that by suppressing the PKR activity, palmitate down-regulated the expression level of Bcl-2. Although the mechanism is not fully understood, the positive effect of PKR on the anti-apoptotic protein Bcl-2 could serve as one of the potential pathways by which PKR protects HepG2 cells from apoptosis. It is known that PKR phosphorylates I- κB, which then releases and activates NF-κB (11, 12), the key transcription factor that up-regulates the transcription of Bcl-2 in HepG2 cells (41, 42). Indeed, silencing the gene expression of PKR decreased the level of NF-κB in the nucleus (Fig. 6A, comparing lanes 1 and 3), while over-expressing PKR increased it (Fig. 6A, comparing lanes 1 and 2). Moreover, the decreased level of NF-κB in the nucleus was restored by rescuing the PKR expression in PKR-silenced cells (Fig. 6A, comparing lanes 3 and 4). Furthermore, the PKR inhibitor also decreased the level of NF-κB p65 in the nuclear extract of HepG2 cells (Supplementary Fig. 2B). These results suggest that PKR regulates the activity of NF-κB in HepG2 cells. It has been shown that NF-κB plays a key role in facilitating the transcription of the Bcl-2 gene in liver tumor cell lines, such as U937 and HepG2 cells, and the inhibition of the NF-κB results in down-regulation of the Bcl-2 gene expression (41, 42). Therefore, it is expected that the protein level of Bcl-2 modifies in correspondence with the nuclear level of NF-κB, as shown in Fig. 6A, in which the gene expression level of PKR is modulated. We further confirmed the role of NF-κB in regulating the expression level of Bcl-2 with an inhibitor of NF-κB, NF-κB SN50 (Fig. 6B). Thus, from our results and the literature data, we propose that the transcription factor, NF-κB, mediates PKR regulation of Bcl-2 expression in HepG2 cells. Indeed, we also observed that palmitate decreased the level of NF-κB in the nucleus (Fig. 6C).
Figure 6. Role of PKR in regulating the Nuclear NF-κB p65 level.

Reverse transfection of scramble siRNA (control, the first two lanes) or siRNA of PKR (siPKR, the third and fourth lane) was performed followed by forward transfection of empty vector pCMV6-XL5 (pCMV) or the plasmid containing PKR cDNA sequence (hPKR) (A). Cells were then harvested and the nuclear extract was separated from the cytoplasmic fraction, and western blot analysis was performed to detect the level of Bcl-2 in the cytoplasmic fraction and the levels of NF-kB p65 in both the nuclear extract and the cytoplasmic fraction. TBP and beta actin were also measured as loading controls for the nuclear extracts and the cytoplasmic fraction, respectively (A). 90%-confluent HepG2 cells were exposed to a cell-permeable inhibitor of NF-kB, SN50 (18 μM), or its negative control, SN50M (18 μM), in regular media for 24 hours (B). After treatment, the cells were harvested, and western blot analysis was performed to detect the protein level of Bcl-2 in the whole cell lysates (B). 90%-confluent HepG2 cells were exposed to 0.7 mM palmitate or oleate for 24 hours (C). The vehicle for the FFAs (0.7 mM BSA) was used as the control (i.e., regular media with BSA). After treatment, the cells were harvested, and western blot analysis was performed to detect the protein level of NF-kB p65 in the nuclear extracts (C).
In summary, palmitate induces apoptosis of HepG2 cells, in part, by reducing Bcl-2 level, mediated by the repression of PKR and NF-κB activities (Fig. 2-6). However, in addition to the protein level of Bcl-2, the anti-apoptotic role of Bcl-2 is regulated also by the post-translational modification of Bcl-2. The phosphorylation of Bcl-2 at Ser70 sustains the anti-apoptotic role of Bcl-2, while phosphorylation of Bcl-2 at Ser87 attenuates the anti-apoptotic role of Bcl-2 (49-51). Therefore, we further investigated the involvement of palmitate and PKR in regulating the phosphorylation of Bcl-2.
Palmitate Decreases the Phosphorylation of Bcl-2 at Ser70, while the Phosphorylation of Bcl-2 at Ser87 is Not Affected
Palmitate decreased the phosphorylation of Bcl-2 at Ser 70 in HepG2 cells (Fig. 7A). On the other hand, the phosphorylation of Bcl-2 at the pro-apoptotic amino acid residue, Ser87, was not affected by palmitate (Fig. 7B). Considering the concomitant repression of the phosphorylation of Bcl-2 and PKR activity by palmitate (Fig. 2), we propose that PKR, a protein kinase, may be involved in mediating the effects of palmitate on the phosphorylation of Bcl-2.
Figure 7. Effect of Palmitate on the phosphorylation of Bcl-2.

HepG2 cells were cultured in regular media until reaching 90% confluency, and then exposed to regular media with different levels of palmitate (A, B) for 24 hours. The vehicle for palmitate (0.7 mM BSA) was used as the control (i.e., regular media with BSA), in which the concentration of palmitate was 0 (A, B). After treatment, the cells were harvested and immunoprecipitated with anti-Bcl-2 and detected for the phosphorylation of Bcl-2 at Ser 70 (A) and Ser87 (B). Quantified the phosphorylation level of Bcl-2 by normalizing to total Bcl-2 levels and expressed as average of three samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly lower than control, i.e., regular media with BSA, p<0.01.
PKR is Involved in Mediating the Effects of Palmitate on the Phosphorylation of Bcl-2 at Ser70
Silencing the PKR gene using siRNA of PKR decreased the phosphorylation of Bcl-2 at Ser70 (Fig. 8A), indicating that PKR has a positive effect on (i.e., enhances) the phosphorylation of Bcl-2 at Ser70, while the phosphorylation of Bcl-2 at Ser87 was not affected by silencing PKR (Fig. 8A). The role of PKR in positively regulating the phosphorylation of Bcl-2 at Ser70 is also supported by an inhibition study of PKR (Supplementary Fig. 2C). The effects of silencing or inhibiting PKR on the phosphorylation of Bcl-2 at Ser70 and Ser87 are consistent with those of palmitate, and considering the negative effect of palmitate on PKR activity (Fig. 2), we propose that the suppression of the PKR activity mediates the negative effects of palmitate on the phosphorylation of Bcl-2 at Ser70, as well as, the protein level of Bcl-2. To confirm this hypothesis, we over-expressed the PKR gene in HepG2 cells and exposed the cells to palmitate (Fig. 5C) and found that the phosphorylation of Bcl-2 at Ser70 was restored by over-expressing PKR in the palmitate treatment (Fig. 8B), supporting the involvement of PKR in mediating the effect of palmitate on the phosphorylation of Bcl-2 at Ser70. However, co-immunoprecipitation study showed that PKR did not directly interact with the Bcl-2 protein (Fig. 8C); therefore other intermediate signaling molecules are involved in mediating the effect of PKR on the phosphorylation of Bcl-2. PKR has been reported to positively signal MAPKs (13), and sequence analysis of both Ser70 and Ser87 residues of Bcl-2 suggests that JNK could regulate the phosphorylation of Bcl-2 (56). Taken together, the evidence suggests that JNK may act as one of the intermediates, between PKR and Bcl-2.
Figure 8. Involvement of PKR in regulating the phosphorylation of Bcl-2 at Ser70.
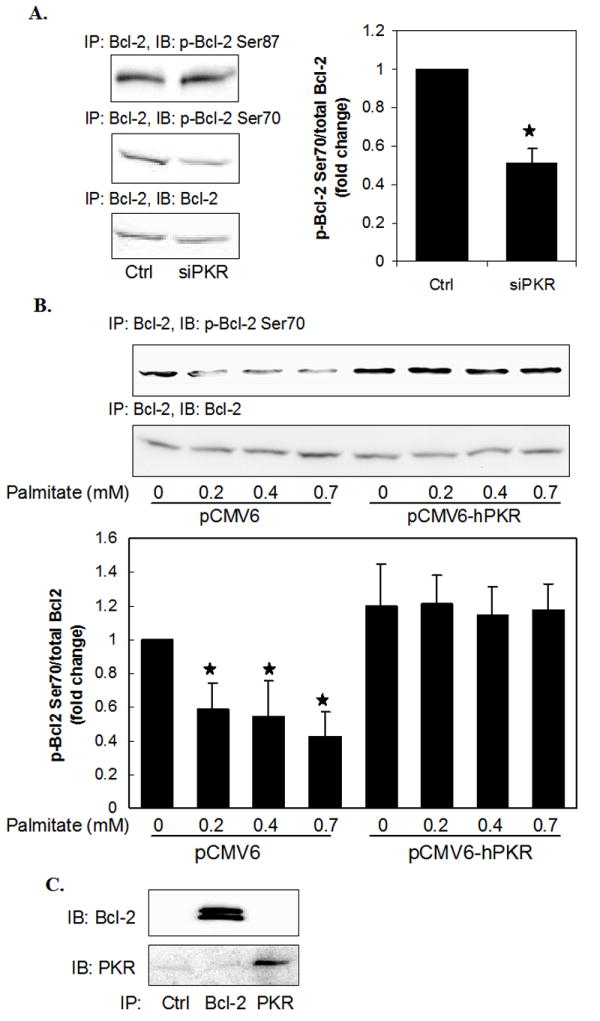
Reverse transfection of suspended HepG2 cells were performed with scrambled siRNA (Control) or siRNA of PKR for 24 hours and the transfected cells were cultured in regular media for another 24 hours (A). Cells were harvested and immunoprecipitated with anti-Bcl-2 and detected for the phosphorylation of Bcl-2 at Ser 70 and Ser87 (A). In HepG2 cells, forward transfection of empty vector pCMV6-XL5 (pCMV6) or the plasmid containing PKR cDNA sequence (pCMV6-hPKR) was performed and the cells were then treated with different concentrations of palmitate for 24 hours (B). The vehicle for palmitate (0.7 mM BSA) was used as the control (i.e., regular media with BSA), in which the concentration of palmitate was 0 (B). After the transfections and palmitate treatment, cells were harvested, and cell lysates were immunoprecipitated with anti-Bcl-2 and detected for phosphorylation of Bcl-2 at Ser 70 (B) (Please see Fig. 5C for the over-expressed PKR levels). Confluent HepG2 cells were harvested, and immunoprecipitated with anti-Bcl-2 or anti-PKR, and western blot analysis was performed to detect the coimmunoprecipitation of Bcl-2 and PKR (C). Quantified the phosphorylation level of Bcl-2 by normalizing to total Bcl-2 levels and expressed as average of three samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly different from control, p<0.01.
PKR Positively Regulates JNK, and JNK Regulates the Phosphorylation of Bcl-2 at Ser70, but not at Ser87
Co-immunoprecipitation study indicated that JNK directly interacted with both PKR and Bcl-2 (Fig. 9A), suggesting that JNK may be a potential intermediate protein kinase that mediates the positive effect of PKR on the phosphorylation of Bcl-2 at Ser70. Indeed, silencing the PKR gene repressed the activity of JNK (Fig. 9B, comparing lanes 1 and 3), while over-expressing PKR enhanced it (Fig. 9B, comparing lanes 1 and 2). Moreover, the suppressed JNK activity was restored by rescuing the PKR expression in PKR-silenced cells (Fig. 9B, comparing lanes 3 and 4), confirming the positive connection between PKR and JNK. Considering the negative effect of palmitate on PKR activity (Fig. 2), we then propose that palmitate decreases the activity of JNK by repressing PKR. Indeed, we found that treatment of palmitate for 24 hours decreased the phosphorylation of JNK (Fig. 9C), and over-expressing PKR in the palmitate treatment restored the phosphorylation of JNK (Fig. 9D), supporting the involvement of PKR in mediating the effect of palmitate on the phosphorylation of JNK. In addition, to further assess the connection between JNK and Bcl-2, we performed a JNK inhibition study and found that the JNK inhibitor, SP600125, suppressed the phosphorylation of Bcl-2 at Ser70, but not the phosphorylation at Ser87 (Fig. 9 E and F), which is consistent with the distinct effects of palmitate as well as PKR on the phosphorylation of Bcl-2 at these two amino acid residues (Figs. 7, 8). Therefore, the results in Figure 9 suggest JNK as an intermediate protein that mediates the effects of palmitate and PKR on the phosphorylation of Bcl-2 at Ser70. We showed that PKR had an anti-apoptotic role in HepG2 cells (Fig. 3), and to further confirm the positive correlation between PKR and JNK, we investigated the role of JNK in regulating the cytotoxicity and apoptosis in HepG2 cells. Inhibiting JNK using SP600125 significantly increased LDH release (Fig. 10A) and caspase-3 activity (Fig. 10B), suggesting that similar to PKR, JNK has an anti-apoptotic role in HepG2 cells.
Figure 9. Involvement of JNK in regulating the phosphorylation of Bcl-2.
Confluent HepG2 cells were harvested, and immunoprecipitated with anti-Bcl-2 or anti-PKR, and western blot analysis was performed to detect the protein level of JNK (A). Reverse transfection of scramble siRNA (control, the first two lanes) or siRNA of PKR (siPKR, the third and fourth lane) was performed followed by forward transfection of empty vector pCMV6-XL5 (pCMV) or the plasmid containing PKR cDNA sequence (hPKR) (B). 90%-confluent HepG2 cells were exposed to 0.7 mM palmitate or oleate for 24 hours (C). The vehicle for the FFAs, 0.7 mM BSA, was used as the control (i.e., regular media with BSA) (C). In HepG2 cells, forward transfection of empty vector pCMV6-XL5 (pCMV6) or plasmid containing PKR cDNA sequence (pCMV6- hPKR) was performed and the cells were then treated with 0.7 mM palmitate for 24 hours (D). The vehicle for palmitate, 0.7 mM BSA, was used as the control (i.e., regular media with BSA) (D). After treatments, cells were then harvested and western blot analysis was performed to detect the phosphorylation and protein level of JNK1/2 After treatment (B, C, D). 90%-confluent HepG2 cells were exposed to the pharmaceutical inhibitor of JNK, SP600125 (25 μM) (E, F), or its analogue (25 μM) as a negative control of SP600125 (E) in regular media for 24 hours. The control of figure F is the vehicle of palmitate, BSA. After treatment, the cells were harvested, and western blot analysis was performed to detect the protein level of Bcl-2 and the phosphorylation of Bcl-2 at Ser70 (E), or the cell lysate was immunoprecipitated with anti-Bcl-2 and western blot analysis was performed to detect the phosphorylation level of Bcl-2 at Ser87 (F).
Figure 10. Effect of inhibiting JNK activity on cytotoxicity and apoptosis of HepG2 cells.
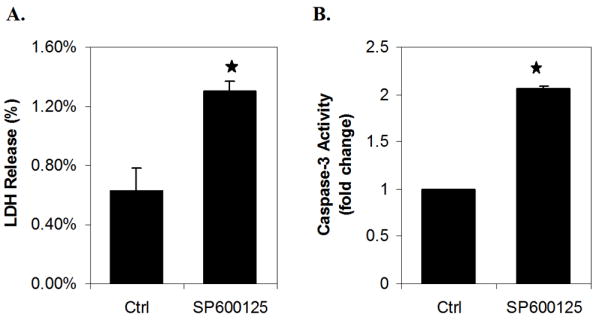
90%-confluent HepG2 cells were exposed to the pharmaceutical inhibitor of JNK, SP600125 (25 μM), or its analogue (25μM) as a negative control of SP600125 for 24 hours (A, B). LDH release (A) and caspase-3 activity (B) were measured after treatment with the JNK inhibitor. Data expressed as average of nine samples ± SD from three independent experiments. One-way ANOVA with Tukey’s post hoc method was used for analyzing the differences between treatment groups. ★, significantly higher than control, p<0.01.
In summary, palmitate inhibits the phosphorylation of Bcl-2 at the anti-apoptotic residue, Ser70, without affecting the pro-apoptotic residue, Ser87. Our data (Fig. 7-10) suggests that this effect of palmitate on the phosphorylation of Bcl-2 is mediated by the signaling of PKR and JNK. We therefore propose another anti-apoptotic pathway, which is suppressed by palmitate, consisting of PKR, JNK, and phosphorylation of Bcl-2.
Taken together, investigating the association between PKR and Bcl-2 revealed two different but complementary anti-apoptotic pathways that connect PKR and Bcl-2. First, PKR up-regulates the transcription of Bcl-2 gene, possibly through the transcription factor, NF-κB, and second, PKR up-regulates the phosphorylation of Bcl-2 at the anti-apoptotic residue, Ser70, mediated by JNK (Fig. 11B). These two pathways were down-regulated in HepG2 cells upon exposure to palmitate, and may be one of the potential mechanisms by which palmitate induces apoptosis in HepG2 cells.
Figure 11. Proposed signaling pathways from PKR to Bcl-2 induced by palmitate.

A. Reverse transfection of suspended HepG2 cells were performed with scrambled siRNA (Control) or siRNA of PKR for 24 hours and the transfected cells were cultured in regular media for another 24 hours. Cells were harvested, and western blot analysis was performed to detect the protein level of Bim. B. Summary of the signaling pathways identified in this study. First, PKR up-regulates the transcription of Bcl-2 gene through the transcription factor, likely NF-κB. Second, PKR up-regulates the phosphorylation of Bcl-2 at the anti-apoptotic residue, Ser70, mediated by JNK. By suppressing PKR and in turn these two downstream pathways, palmitate regulates the protein level and phosphorylation of Bcl-2 at Ser70 and therefore induces apoptosis in HepG2 cells. Another Bcl-2 family protein, Bim, which also mediates palmitate-induced apoptosis (31, 32) (dash lines) and the potential effect of PKR on Bim (line with the question mark) are also included.
Discussion
In the present study, PKR is anti-apoptotic in human hepatoma cells. PKR is best known for its pro-apoptotic role by phosphorylating eIF-2α and thereby inhibiting general protein synthesis (3, 4). Thus, previously it was suggested that PKR acts as a tumor suppressor by inhibiting cell growth and inducing apoptosis (62, 63). In contrast, more recent studies suggest PKR has an anti-apoptotic role in regulating tumor development and tumor cell apoptosis (6-9). Elevated PKR protein level and activity were observed in certain tumor cells, i.e., human breast cancer cells (6), melanoma cells (7, 9), and hepatitis C virus (HCV)-related hepatocellular carcinoma (8). The over-expression and elevated activity of PKR have been attributed to the development of tumor, and the proliferation of tumor cells (6-9), but the mechanism is still unclear. Research suggests that PKR may suppress apoptosis by activating the NF-κB pathway before phosphorylating eIF-2α, therefore inducing cell survival initially and cell death subsequently in NIH3T3 cells expressing PKR (5). The present study supports an anti-apoptotic role of PKR in human hepatoma cells (HepG2) and suggests potential pathways through which PKR mediates anti-apoptosis through Bcl-2, thereby further providing a potential mechanism of palmitate-induced apoptosis in HepG2 cells. Interestingly, although the phosphorylation of PKR was significantly suppressed in HepG2 cells, the phosphorylation level of eIF-2α was not altered by palmitate (Supplementary Fig. 3), suggesting that the protein synthesis arrest machinery and related apoptosis activity were not affected. Similarly, another substrate of PKR, B56α-PP2A, was also not affected by palmitate (Supplementary Fig. 3). Thus suggestive of other substrates of PKR, which we propose may be NF-κB and JNK, are mediating the effects of altered PKR activity on the regulation of Bcl-2 protein and phosphorylation levels in HepG2 cells.
PKR has been shown to activate several transcription factors such as IRF-1, p53, and NF-κB (64, 65). In the present study we show PKR is involved in controlling the transcription of Bcl-2 in HepG2 cells, mediated by the transcription factor, NF-κB. This result suggests a novel mechanism by which palmitate down-regulates the protein level of Bcl-2 (Fig. 4) in HepG2 cells. By modulating the transcription of a number of anti-apoptotic genes, such as Bcl-2 (66), Bcl-xL (67), cIAPs (68), and p53 (69), NF-κB is commonly considered an anti-apoptotic transcription factor (70, 71), which is consistent with the anti-apoptotic role of PKR in HepG2 cells. It has been shown that NF-κB is the key regulator of transcription of the Bcl-2 gene in liver tumor cell lines including HepG2 (41, 42). However, other transcription factors that may regulate the transcription of the Bcl-2 gene, for example c-Myb (38, 39) and STAT5 (40), have not been evaluated in the present study. It is not known in the literature whether these transcription factors are altered by palmitate or regulated by PKR. Therefore, it remains to be determined whether other transcription factors, in addition to NF-kB, mediate the effect of PKR on the gene expression and protein levels of Bcl-2.
Furthermore, other studies have revealed that elevated Bim, a pro-apoptotic Bcl-2 family protein, also plays an important role in stearic and palmitic acid-induced apoptosis of several liver cell lines including HepG2 (31, 32), and this process has been determined to be dependent on the transcription factor, FoxO3a (31). In the present study, we propose that the suppression of PKR mediates palmitate-induced apoptosis through Bcl-2; therefore, to test the potential connection between our results and the previous findings on Bim, we evaluated the effect of PKR on the expression of Bim. Interestingly, silencing PKR significantly increased the protein level of Bim (Fig. 11A), suggesting that PKR repressed Bim expression. As a BH3-only Bcl-2 protein, Bim promotes apoptosis by binding and inactivating anti-apoptotic proteins (72), therefore, the negative effect of PKR on Bim supports the role of PKR as an anti-apoptotic protein and could serve as another potential mechanism by which PKR inhibits apoptosis in HepG2 cell. In addition, we show in the present study that palmitate decreased PKR activity (Fig. 2), thus it is possible that the up-regulation of Bim by palmitate (31) may be, in part, due to the repression of PKR activity. However, the mechanism by which PKR down-regulates the expression of Bim is not known at this point. Future experiments will determine whether PKR has any effect on the key transcription factor of Bim, FoxO3a (31). Previously, it was shown that PP2A, which was activated by palmitate, mediated the effect of palmitate on the activity of FoxO3a and thereby the expression of Bim (31). However, in our study palmitate did not affect the activity of PP2A (data not shown), and this contradictory results may be due to the different treatment time (6 vs. 24 hours) and/or the different types of palmitate (palmitic acid dissolved in isopropyl alcohol vs. sodium palmitate complexed with BSA) used.
In the present study, we uncovered a second anti-apoptotic pathway, namely, that PKR up-regulates the phosphorylation of Bcl-2 at Ser70 (Fig. 8), mediated by JNK (Fig. 9). Although sequence analysis suggests that both Ser70 and Ser87 residues of Bcl-2 can be recognized by JNK (56), interestingly, we found that only phosphorylation at Ser70 is affected by JNK (Fig. 9). Concomitantly, palmitate (Fig. 7) and PKR silencing (Fig. 8) both decreased only the phosphorylation of Bcl-2 at Ser70, which lends support to the hypothesis that palmitate down-regulates the phosphorylation of Bcl-2 at Ser70 through PKR and JNK. In fact, all 3 MAPKs have been shown to be activated by PKR upon ribotoxic stress and the investigators proposed that MAPKs respond to PKR in the rank order of JNK>p38>ERK (13). However, we did not test the effects of PKR on the other two, less responsive, MAPK proteins, ERK and p38, which were also proposed to phosphorylate Bcl-2 at Ser70 (53-55). Thus, JNK is one of the intermediates involved in signaling the pathway from PKR to Bcl-2 phosphorylation. Further investigations of the 3 MAPKs are required to fully understand the interaction between PKR and Bcl-2.
Currently, it remains unclear how PKR interacts with MAPKs, e.g. JNK. An association between PKR and apoptosis signal-regulating kinase 1 (ASK1), one of the MAPK signaling proteins, has been previously established (73). ASK1, a MAPK kinase kinase (MAPKKK), phosphorylates SEK1/MKK4 or MKK3/MKK6, which in turn activates JNK or p38 MAPK, respectively (74). Our coimmunoprecipitation study suggests an interaction between JNK and PKR (Fig. 9). Nevertheless it must be noted that the coimmunoprecipitation of PKR and JNK does not necessarily indicate a “direct” binding of these two proteins. It is believed that the activation of MAPK cascade requires a scaffold protein that assembles the MAPKKK, MAPKK, and MAPK proteins together into a certain signaling module (75). For instance, JIP1 organizes upstream kinase HPK-1, MAPKKK MLK1, MKK7, and JNK1/2, and facilitates the activation of JNK (76). Therefore, the coimmunoprecipitation study suggests an interaction, but not necessarily a direct one, between PKR and JNK. Instead, the coimmunoprecipitation of PKR and JNK may recruit a third protein, possibly a scaffold protein that assembles JNK and facilitates the activation of JNK by PKR. In other words, the pathway we identified consisting of PKR and JNK does not preclude the possibility of other intermediates between PKR and JNK. To understand how PKR interacts with JNK, the scaffold protein and the assembly of the signaling proteins with their upstream activators need to be investigated.
It is well known that JNK is involved in many signaling pathways that control diverse cellular activities such as proliferation, differentiation, and apoptosis. Through different pathways and substrates (77), JNK has been shown to have either pro- or anti-apoptotic functions, depending on the cell type, stimulus, duration of its activation and the activity of other signaling pathways, and therefore referred to as a “double-edge sword” (78). In liver tumor cell lines such as HepG2, conflicting views on the role of JNK in regulating apoptosis have been reported in the literature. For example, JNK was shown to mediate anti-apoptotic signals in transforming growth factor-beta 1- (79) and tumor necrosis factor-induced apoptosis (80) in HepG2 cells, while others have proposed pro-apoptotic roles for JNK in HepG2 cells (32, 81). In these studies on the role of JNK in regulating apoptosis, the JNK inhibitor, SP600125, was used, and the conflicting results may be due to the different conditions the investigators applied, such as the concentrations and treatment times of SP600125, and the accompanying additives. In our study, we inhibited JNK in regular medium for 24 hours and indeed found that the JNK inhibitor (SP600125, at 25 μM) was apoptotic, as evidenced by caspases-3 activity (Fig. 10B). In Zhang et al. (79), liver tumor cell lines were treated with 20 μM SP600125 for 50 hours, resulting in significant increase of apoptosis. On the other hand, in Chen et al. (81), the authors treated the HepG2 cells with 1 μM SP600125 for 48 hours, and showed it blocked the norcantharidin-induced apoptosis. Interestingly, in their controls without norcantharidin, SP600125 or ERK inhibitor (U0126 or PD98059) slightly increased the apoptosis of HepG2 cells, which supports our finding with SP600125 in control medium. In the paper by Malhi et al. (32), the authors used SP600125 to inhibit JNK in the presence of palmitic acid for 24 hours, but the concentration of the inhibitor used was not specified. Our study suggest that JNK is involved in phosphorylating Bcl-2, an anti-apoptotic member of the Bcl-2 family, at its anti-apoptotic residue, Ser70 (Fig. 9C), suggesting that JNK may act as an anti-apoptotic factor. The anti-apoptotic role exhibited by JNK is consistent with that of PKR and therefore lends support to the hypothesis that JNK may mediate, in part, the signaling between PKR and Bcl-2. However, inhibiting JNK with SP600125 also increased the LDH release significantly (Fig. 10A), while silencing PKR did not have a significant effect on the LDH release (Fig. 3B), suggesting that JNK may be involved in other cellular activities related to cytotoxicity, in addition to the pathway from PKR to Bcl-2. On the other hand, it is also possible that the inhibitor, SP600125, itself has other non-specific effects that lead to cytotoxicity, despite its wide use as an inhibitor of JNK.
The results in the present study show for the first time that palmitate treatment decreases the activity of PKR (Fig. 2), however, the mechanism by which palmitate induces dephosphorylation of PKR is still unclear. Palmitate has been shown to induce a rise in cytosolic free Ca(2+) (82), and depletion of intracellular Ca(2+) resulted in the activation of PKR (83). These findings suggest that palmitate-induced inactivation of PKR could be mediated by a change in cytosolic Ca(2+) level. The auto-phosphorylation of PKR requires its dimerization, which depends on the hydrophobic residues on its catalytic-domain (84, 85). Therefore, a potential interaction between the free palmitate molecules and the hydrophobic residues in the catalytic-domain of PKR could disrupt the dimerization of PKR, and thereby inhibit its auto-phosphorylation. However, these proposed mechanisms require further investigation.
In summary, we identified an anti-apoptotic role of PKR and that it is involved in regulating the protein level and phosphorylation status of Bcl-2 in HepG2 cells. The transcription factor, NF-κB, and MAP kinase, JNK, appear to be involved in mediating the effects of PKR on the protein level and the phosphorylation of Bcl-2, respectively. We propose that by inhibiting PKR (Fig. 2), palmitate suppresses these two pathways (Fig. 4 and 7), and thereby attenuates the anti-apoptotic machinery (Fig. 11B).
Materials and Methods
Cell Culture and Reagent
Human hepatocellular carcinoma cell (HepG2) were cultured in Dulbecco’s Modified Eagle Medium (DMEM) (Invitrogen, Carlsbad, CA) with 10% fetal bovine serum (FBS) (Biomeda Corp, Foster City, CA) and penicillin-streptomycin (penicillin: 10,000 U/ml, streptomycin: 10,000 μg/ml) (Invitrogen, Carlsbad, CA). Freshly trypsinized HepG2 cells were suspended at 5 × 105 cells/ml in standard HepG2 culture medium and seeded at a density of 106 cells per well in standard six-well tissue culture plates. After seeding, the cells were incubated at 37°C in a 90% air/10% CO2 atmosphere, and two milliliter of fresh medium was supplied every other day to the cultures after removal of the supernatant. The HepG2 cells were cultured in standard medium for 5-6 days to achieve 90% confluent before treating with FFAs, or other additives. HepG2 cell number was assessed by trypan blue dye exclusion using a hematocytometer. Phosphate-buffered saline (PBS) were purchased from Invitrogen, poly-(I:C) and trypan blue from Sigma-Aldrich (St. Louis, MO), NF-κB SN50 and its inactive control, NF-κB SN50M, PKR inhibitor, JNK inhibitor (SP600125) and their analogues, used as negative controls, from EMD Biosciences (San Diego, CA).
Fatty Acid Salt Treatment
Sodium salts of palmitate (P9767) and oleate (O7501) were purchased from Sigma-Aldrich. Palmitate and oleate were complexed to 0.7 mM bovine serum albumin (BSA, fatty acid free) dissolved in the media, which mimics the physiological concentration of albumin in human blood (3.5-5%, (86)). Fatty acid free BSA was purchased from MP Biomedicals (Chillicothe, OH). Dose responses of palmitate at 0, 0.2, 0.4, and 0.7 mM were performed in most of the experiments. If only one concentration was reported, the concentration of palmitate or oleate would be 0.7 mM. In all the experiments, FFAs were treated for 24 hours, and the vehicle (0.7 mM BSA) was used as the control.
RNA Interference for PKR and Reverse Transfection
Silencer® Validated siRNA targeting human PKR mRNA was purchased from Ambion (Austin, TX). The synthesized oligonucleotides for siRNA are 5’-GGUGAAGGUAGAUCAAAGATT-3’ and 5’-UCUUUGAUCUACCUUCACCTT-3’. Reverse transfection of siRNA was performed. In general, the scrambled non-targeting siRNA as a negative control or the siRNA targeting PKR was diluted in serum and antibiotic free Opti-MEM (Invitrogen), and mixed with the transfection reagent, Lipofectamine RNAiMAX (Invitrogen). The mixture of siRNA and Lipofectamine RNAiMAX in Opti-MEM were then added into 6-well plates and incubated in room temperature for 20 minutes. HepG2 cells suspended in antibiotic free media were counted and plated into the 6-well plates at the same cell number per well. The cells were then incubated at 37°C for 24 hours. After transfection, the cells were incubated in regular media for another 24 hours and then collected. The mRNA and protein levels of PKR were measured by RT-PCR and Western blot analysis, respectively. Titration of the siRNA and the transfection reagent was performed (not shown), and the lowest working amounts of the siRNA and the transfection reagent were applied in the loss-of-function (LOF) experiments in the present study.
Over-expression of PKR and Forward Transfection
The PKR plasmid, pCMV6-XL5-hPKR, and the empty vector, pCMV6-XL5, were purchased from Origene (Rockville, MD). Transient transfection was performed according to the Lipofectamine 2000 (Invitrogen) method. In general, regular HepG2 cells (Fig. 5C and 8B) or the cells, in which the PKR gene was silenced by the siRNA of PKR (Fig. 3C), were washed twice with phosphate buffered saline, and the medium was replaced with 2 ml of Opti-MEM with 1% FBS. 2 μg/well of pCMV6-XL5-hPKR or the empty vector pCMV6-XL5 was then mixed with 10 ul/well of Lipofectamine 2000 in Opti-MEM, and 20 minutes later, the mixture was added to the wells. After 6 hours of transfection, the cells were then cultured in regular media for 48 hours, and harvested (Fig. 3C) or treated with palmitate (Fig. 5C and 8B) subsequently.
Cytotoxicity Measurement
HepG2 cells were cultured in different media for 24 hours and the supernatants were collected. Cells were washed with PBS and kept in 1% triton-X-100 in PBS for 24 hours at 37°C. Cell lysate was then collected, vortexed for 15 seconds, and centrifuged at 7000 rpm for 5 minutes. Cytotoxicity detection kit (Roche Applied Science, Indianapolis, IN) was used to measure the LDH levels in the supernatants and in the cell lysates. The fraction of LDH released into the medium was normalized to the total LDH (LDH released into the medium + LDH remaining in the cell lysates) (30).
DNA Fragmentation
Treated HepG2 cells were lysed and DNA was extracted using the DNA purification kit from Promega (Madison, WI). 2 μg of DNA samples were analyzed by electrophoresis on 1.5% agarose gels and visualized by SYBR gold staining for 4 hours.
Caspase Analysis
For the caspase-3 substrate cleavage assay, the cells were washed with PBS, lysed, and assayed in a 96-well plate using the Caspase-3 cellular assay kit (Biomol, Plymouth Meeting, PA). Fluorescence was measured at emission and excitation settings of 360 and 460 nm, respectively, with Microplate Spectrofluorometer from Molecular Device (Sunnyvale, CA). Caspase-3 activities were normalized by relative beta-actin levels.
Nuclear Extraction and Detection of Nuclear NF-κB levels
The nuclear extracts from HepG2 cells were prepared using the Nuclear/Cytosol Fraction Kit from BioVision (Mountain View, CA). The extracted nuclear and cytoplasmic protein fractions are subjected to Western blotting analysis with anti-NF-kB p65 and anti-TBP, as a loading control for nuclear extracts, and anti-beta actin for cytoplasmic fractions.
Western Blot Analysis and Immunoprecipitation
HepG2 cells were washed twice with cold PBS and lysed in 300 μL/well of CelLytic M cell lysis buffer (Sigma-Aldrich) supplemented with protease inhibitor cocktail (Roche Applied Science, Indianapolis, IN) and Ser/Thr phosphatase inhibitor cocktail (Sigma-Aldrich). Cell lysate was clarified by centrifugation at 10,000 rpm for 15 minutes, and the supernatant was collected. Total protein levels were quantified by BCA assay kit from Pierce Inc (Rockford, IL). 20-40 μg of total protein were resolved by SDS-PAGE gels from Bio-Rad, transferred to nitrocellulose membranes, and probed with primary and secondary antibodies. Biotinylated protein ladders (Cell Signaling, Beverly, MA) were loaded to one well of each SDS-PAGE gel, and anti-biotin antibody was used to detect the protein ladders on Western blots. Antibody detection was performed using the enhanced chemiluminescence kit from Pierce Biotechnology and imaged on the Molecular Imager ChemiDoc XRS System from Bio-Rad. For immunoprecipitation, the cell lysates were incubated with appropriate primary antibodies at 4°C for 1-2 hours, and the immunocomplexes were precipitated in a mixture with protein A affinity gel (Sigma-Aldrich) by incubating overnight. Immunoprecipitates were washed three times with the cell lysis buffer and boiled in SDS-PAGE sample buffer, and the immune complexes were analyzed by western blot analysis. Phospho site-specific anti-eIF2α (Ser51) and JNK (T183/Y185), anti-eIF2α, anti-PKR, anti-NF-kB p65, and anti-JNK rabbit polyclonal antibodies were purchased from Cell Signaling (Beverly, MA), phospho site-specific anti-PP2A/C (Tyr307) from Abcam (Cambridge, MA), phospho site-specific anti-Bcl-2 (Ser70) from Upstate (Charlottesville, VA), phospho site-specific anti-phospho PKR (Thr451) and Bcl-2 (Ser87) polyclonal antibodies from EMD Biosciences, anti-Bcl-2, anti-Bim, anti-TBP, and anti-beta actin antibodies from Sigma-Aldrich. Anti-PP2A-B56α and anti-goat secondary antibody was purchased from Santa Cruze Biotechnology (Santa Cruz, CA). Secondary anti-rabbit and anti-mouse antibodies were purchased from Pierce Biotechnology Inc.
Real-time Quantitative RT-PCR Analysis
Total RNA was extracted from cells with the RNeasy mini kit (Qiagen, Valencia, CA) and depleted of contaminating DNA with RNase-free DNase (Qiagen). Equal amounts of total RNA (1 μg) were reverse-transcribed using an iScript cDNA synthesis kit (Bio-RAD). The first-strand cDNA was used as a template. The primers used for quantitative RT-PCR analyses of human PKR (5’-CCTGTCCTCTGGTTCTTTTGCT-3’ and 5’-GATGATTCAGAAGCGAGTGTGC-3’) (87), human Bcl-2 (5’-ACATCGCCCTGTGGATGACT-3’ and 5’-TCACTTGTGGCCCAGATAGG-3’), and human GAPDH (5’-AACTTTGGTATCGTGGAAGGA-3’ and 5’-CAGTAGAGGCAGGGATGATGT-3’) were synthesized by Operon Biotechnologies, Inc. (Huntsville, AL). RT-PCR was performed in 25-μl reactions using 1/10 of the cDNA produced by reverse transcription, 0.2 μM each primer, 1 X SYBR green supermix from Bio-RAD, and an annealing temperature of 60 °C for 40 cycles. Each sample was assayed in three independent RT reactions and triplicate reactions were performed and normalized to GAPDH expression levels. Negative controls included the absence of enzyme in the RT reaction and absence of template during PCR. The cycle threshold (CT) values corresponding to the PCR cycle number at which fluorescence emission in real time reaches a threshold above the base-line emission were determined using MyIQ™ Real-Time PCR Detection System (Bio-RAD).
Statistical Analysis
All experiments were performed at least three times, and representative results are shown. All data, unless specified, are shown as the mean ± S.D. for indicated number of experiments. One-way ANOVA with Tukey’s post hoc method were used to evaluate statistical significances between different treatment groups. Statistical significance was set at p<0.01.
Supplementary Material
Acknowledgments
The work was supported in part by the National Science Foundation (BES 0425821), the Environmental Protection Agency (RD83184701), the Whitaker Foundation and the National Institute of Health (R01GM079688-01, R21CA126136-01 and R21RR024439), and the MSU Foundation and the Center for Systems Biology.
Abbreviations
- PKR
double-stranded RNA-dependent protein kinase
- HepG2
human hepatocellular carcinoma cells
- Bcl-2
B-cell leukemia/lymphoma 2
- FFA
free fatty acid
- NF-κB
nuclear factor kappa B
- JNK
c-Jun N-terminal kinase
- eIF-2α
eukaryotic initiation factor 2-alpha
- MAPK
mitogen-activated protein kinase
- ERK
extracellular-signal-regulated kinase
- PP2A
protein phosphatase 2A
- IKK
I-κB kinase
- NAFLD
non alcoholic fatty liver disease
- TG
triacylglycerol
- Bim
Bcl-2-interacting mediator of cell death
- FoxO
Forkhead box-containing protein, class O
- ROS
reactive oxygen species
- RNAi
RNA interference
- LDH
lactate dehydrogenase
- HCV
hepatitis C virus
- ASK1
apoptosis signal-regulating kinase 1
References
- 1.Barber GN. The dsRNA-dependent protein kinase, PKR and cell death. Cell Death Differ. 2005 Jun;12(6):563–570. doi: 10.1038/sj.cdd.4401643. [DOI] [PubMed] [Google Scholar]
- 2.Zhang F, Romano PR, Nagamura-Inoue T, Tian B, Dever TE, Mathews MB, et al. Binding of double-stranded RNA to protein kinase PKR is required for dimerization and promotes critical autophosphorylation events in the activation loop. J Biol Chem. 2001 Jul 6;276(27):24946–24958. doi: 10.1074/jbc.M102108200. [DOI] [PubMed] [Google Scholar]
- 3.Taylor SS, Haste NM, Ghosh G. PKR and eIF2alpha: integration of kinase dimerization, activation, and substrate docking. Cell. 2005 Sep 23;122(6):823–825. doi: 10.1016/j.cell.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Stark GR, Kerr IM, Williams BR, Silverman RH, Schreiber RD. How cells respond to interferons. Annu Rev Biochem. 1998;67:227–264. doi: 10.1146/annurev.biochem.67.1.227. [DOI] [PubMed] [Google Scholar]
- 5.Donze O, Deng J, Curran J, Sladek R, Picard D, Sonenberg N. The protein kinase PKR: a molecular clock that sequentially activates survival and death programs. EMBO J. 2004 Feb 11;23(3):564–571. doi: 10.1038/sj.emboj.7600078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim SH, Forman AP, Mathews MB, Gunnery S. Human breast cancer cells contain elevated levels and activity of the protein kinase, PKR. Oncogene. 2000 Jun 22;19(27):3086–3094. doi: 10.1038/sj.onc.1203632. [DOI] [PubMed] [Google Scholar]
- 7.Kim SH, Gunnery S, Choe JK, Mathews MB. Neoplastic progression in melanoma and colon cancer is associated with increased expression and activity of the interferon-inducible protein kinase, PKR. Oncogene. 2002 Dec 12;21(57):8741–8748. doi: 10.1038/sj.onc.1205987. [DOI] [PubMed] [Google Scholar]
- 8.Hiasa Y, Kamegaya Y, Nuriya H, Onji M, Kohara M, Schmidt EV, et al. Protein kinase R is increased and is functional in hepatitis C virus-related hepatocellular carcinoma. Am J Gastroenterol. 2003 Nov;98(11):2528–2534. doi: 10.1111/j.1572-0241.2003.08663.x. [DOI] [PubMed] [Google Scholar]
- 9.Delgado Andre N, De Lucca FL. Knockdown of PKR expression by RNAi reduces pulmonary metastatic potential of B16-F10 melanoma cells in mice: Possible role of NF-kappaB. Cancer Lett. 2007 Dec 8;258(1):118–125. doi: 10.1016/j.canlet.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Williams BR. Signal integration via PKR. Sci STKE. 2001 Jul 3;2001(89):RE2. doi: 10.1126/stke.2001.89.re2. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Haque J, Lacoste J, Hiscott J, Williams BR. Double-stranded RNA-dependent protein kinase activates transcription factor NF-kappa B by phosphorylating I kappa B. Proc Natl Acad Sci U S A. 1994 Jul 5;91(14):6288–6292. doi: 10.1073/pnas.91.14.6288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gil J, Alcami J, Esteban M. Activation of NF-kappa B by the dsRNA-dependent protein kinase, PKR involves the I kappa B kinase complex. Oncogene. 2000 Mar 9;19(11):1369–1378. doi: 10.1038/sj.onc.1203448. [DOI] [PubMed] [Google Scholar]
- 13.Zhou HR, Lau AS, Pestka JJ. Role of double-stranded RNA-activated protein kinase R (PKR) in deoxynivalenol-induced ribotoxic stress response. Toxicol Sci. 2003 Aug;74(2):335–344. doi: 10.1093/toxsci/kfg148. [DOI] [PubMed] [Google Scholar]
- 14.Xu Z, Williams BR. The B56alpha regulatory subunit of protein phosphatase 2A is a target for regulation by double-stranded RNA-dependent protein kinase PKR. Mol Cell Biol. 2000 Jul;20(14):5285–5299. doi: 10.1128/mcb.20.14.5285-5299.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watanabe MA, Rodrigues Souza L, Murad JM, De Lucca FL. Antitumor activity induced by regulatory RNA: possible role of RNA-dependent protein kinase and nuclear factor-kappaB. Eur J Pharmacol. 2003 Apr 4;465(3):205–210. doi: 10.1016/s0014-2999(03)01480-8. [DOI] [PubMed] [Google Scholar]
- 16.Yeung MC, Lau AS. Tumor suppressor p53 as a component of the tumor necrosis factor-induced, protein kinase PKR-mediated apoptotic pathway in human promonocytic U937 cells. J Biol Chem. 1998 Sep 25;273(39):25198–25202. doi: 10.1074/jbc.273.39.25198. [DOI] [PubMed] [Google Scholar]
- 17.Onuki R, Bando Y, Suyama E, Katayama T, Kawasaki H, Baba T, et al. An RNA-dependent protein kinase is involved in tunicamycin-induced apoptosis and Alzheimer’s disease. EMBO J. 2004 Feb 25;23(4):959–968. doi: 10.1038/sj.emboj.7600049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He B. Viruses, endoplasmic reticulum stress, and interferon responses. Cell Death Differ. 2006 Mar;13(3):393–403. doi: 10.1038/sj.cdd.4401833. [DOI] [PubMed] [Google Scholar]
- 19.Meusel TR, Kehoe KE, Imani F. Protein kinase R regulates double-stranded RNA induction of TNF-alpha but not IL-1 beta mRNA in human epithelial cells. J Immunol. 2002 Jun 15;168(12):6429–6435. doi: 10.4049/jimmunol.168.12.6429. [DOI] [PubMed] [Google Scholar]
- 20.Goh KC, deVeer MJ, Williams BR. The protein kinase PKR is required for p38 MAPK activation and the innate immune response to bacterial endotoxin. EMBO J. 2000 Aug 15;19(16):4292–4297. doi: 10.1093/emboj/19.16.4292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldstein AE, Werneburg NW, Canbay A, Guicciardi ME, Bronk SF, Rydzewski R, et al. Free fatty acids promote hepatic lipotoxicity by stimulating TNF-alpha expression via a lysosomal pathway. Hepatology. 2004 Jul;40(1):185–194. doi: 10.1002/hep.20283. [DOI] [PubMed] [Google Scholar]
- 22.Lu ZH, Mu YM, Wang BA, Li XL, Lu JM, Li JY, et al. Saturated free fatty acids, palmitic acid and stearic acid, induce apoptosis by stimulation of ceramide generation in rat testicular Leydig cell. Biochem Biophys Res Commun. 2003 Apr 18;303(4):1002–1007. doi: 10.1016/s0006-291x(03)00449-2. [DOI] [PubMed] [Google Scholar]
- 23.Yamagishi S, Okamoto T, Amano S, Inagaki Y, Koga K, Koga M, et al. Palmitate-induced apoptosis of microvascular endothelial cells and pericytes. Mol Med. 2002 Apr;8(4):179–184. [PMC free article] [PubMed] [Google Scholar]
- 24.Hickson-Bick DL, Sparagna GC, Buja LM, McMillin JB. Palmitate-induced apoptosis in neonatal cardiomyocytes is not dependent on the generation of ROS. Am J Physiol Heart Circ Physiol. 2002 Feb;282(2):H656–664. doi: 10.1152/ajpheart.00726.2001. [DOI] [PubMed] [Google Scholar]
- 25.Feldstein AE, Werneburg NW, Li Z, Bronk SF, Gores GJ. Bax inhibition protects against free fatty acid-induced lysosomal permeabilization. Am J Physiol Gastrointest Liver Physiol. 2006 Jun;290(6):G1339–1346. doi: 10.1152/ajpgi.00509.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giordano A, Calvani M, Petillo O, Grippo P, Tuccillo F, Melone MA, et al. tBid induces alterations of mitochondrial fatty acid oxidation flux by malonyl-CoA-independent inhibition of carnitine palmitoyltransferase-1. Cell Death Differ. 2005 Jun;12(6):603–613. doi: 10.1038/sj.cdd.4401636. [DOI] [PubMed] [Google Scholar]
- 27.Listenberger LL, Han X, Lewis SE, Cases S, Farese RV, Jr, Ory DS, et al. Triglyceride accumulation protects against fatty acid-induced lipotoxicity. Proc Natl Acad Sci U S A. 2003 Mar 18;100(6):3077–3082. doi: 10.1073/pnas.0630588100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wei Y, Wang D, Topczewski F, Pagliassotti MJ. Saturated fatty acids induce endoplasmic reticulum stress and apoptosis independently of ceramide in liver cells. Am J Physiol Endocrinol Metab. 2006 Aug;291(2):E275–281. doi: 10.1152/ajpendo.00644.2005. [DOI] [PubMed] [Google Scholar]
- 29.Assimacopoulos-Jeannet F. Fat storage in pancreas and in insulin-sensitive tissues in pathogenesis of type 2 diabetes. Int J Obes Relat Metab Disord. 2004 Dec;28 Suppl 4:S53–57. doi: 10.1038/sj.ijo.0802857. [DOI] [PubMed] [Google Scholar]
- 30.Srivastava S, Chan C. Hydrogen peroxide and hydroxyl radicals mediate palmitate-induced cytotoxicity to hepatoma cells: Relation to mitochondrial permeability transition. Free Radic Res. 2006 Jan;41(1):38–49. doi: 10.1080/10715760600943900. [DOI] [PubMed] [Google Scholar]
- 31.Barreyro FJ, Kobayashi S, Bronk SF, Werneburg NW, Malhi H, Gores GJ. Transcriptional Regulation of Bim by FoxO3A Mediates Hepatocyte Lipoapoptosis. J Biol Chem. 2007 Sep 14;282(37):27141–27154. doi: 10.1074/jbc.M704391200. [DOI] [PubMed] [Google Scholar]
- 32.Malhi H, Bronk SF, Werneburg NW, Gores GJ. Free fatty acids induce JNK-dependent hepatocyte lipoapoptosis. J Biol Chem. 2006 Apr 28;281(17):12093–12101. doi: 10.1074/jbc.M510660200. [DOI] [PubMed] [Google Scholar]
- 33.Feng LF, Zhong M, Lei XY, Zhu BY, Tang SS, Liao DF. Bcl-2 siRNA induced apoptosis and increased sensitivity to 5-fluorouracil and HCPT in HepG2 cells. J Drug Target. 2006 Jan;14(1):21–26. doi: 10.1080/10611860500527947. [DOI] [PubMed] [Google Scholar]
- 34.Handayani T, Sakinah S, Nallappan M, Pihie AH. Regulation of p53-, Bcl-2- and caspase-dependent signaling pathway in xanthorrhizol-induced apoptosis of HepG2 hepatoma cells. Anticancer Res. 2007 Mar-Apr;27(2):965–971. [PubMed] [Google Scholar]
- 35.Huang DS, Shen KZ, Wei JF, Liang TB, Zheng SS, Xie HY. Specific COX-2 inhibitor NS398 induces apoptosis in human liver cancer cell line HepG2 through BCL-2. World J Gastroenterol. 2005 Jan 14;11(2):204–207. doi: 10.3748/wjg.v11.i2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Landau Z, Forti E, Alcaly M, Birk RZ. Palmitate induced lipoapoptosis of exocrine pancreas AR42J cells. Apoptosis. 2006 May;11(5):717–724. doi: 10.1007/s10495-006-5425-3. [DOI] [PubMed] [Google Scholar]
- 37.Breckenridge DG, Xue D. Regulation of mitochondrial membrane permeabilization by BCL-2 family proteins and caspases. Curr Opin Cell Biol. 2004 Dec;16(6):647–652. doi: 10.1016/j.ceb.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Salomoni P, Perrotti D, Martinez R, Franceschi C, Calabretta B. Resistance to apoptosis in CTLL-2 cells constitutively expressing c-Myb is associated with induction of BCL-2 expression and Myb-dependent regulation of bcl-2 promoter activity. Proc Natl Acad Sci U S A. 1997 Apr 1;94(7):3296–3301. doi: 10.1073/pnas.94.7.3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taylor D, Badiani P, Weston K. A dominant interfering Myb mutant causes apoptosis in T cells. Genes Dev. 1996 Nov 1;10(21):2732–2744. doi: 10.1101/gad.10.21.2732. [DOI] [PubMed] [Google Scholar]
- 40.Weber-Nordt RM, Egen C, Wehinger J, Ludwig W, Gouilleux-Gruart V, Mertelsmann R, et al. Constitutive activation of STAT proteins in primary lymphoid and myeloid leukemia cells and in Epstein-Barr virus (EBV)-related lymphoma cell lines. Blood. 1996 Aug 1;88(3):809–816. [PubMed] [Google Scholar]
- 41.D’Alessio M, Cerella C, Amici C, Pesce C, Coppola S, Fanelli C, et al. Glutathione depletion up-regulates Bcl-2 in BSO-resistant cells. FASEB J. 2004 Oct;18(13):1609–1611. doi: 10.1096/fj.04-1813fje. [DOI] [PubMed] [Google Scholar]
- 42.Nishikawa T, Nakajima T, Moriguchi M, Jo M, Sekoguchi S, Ishii M, et al. A green tea polyphenol, epigalocatechin-3-gallate, induces apoptosis of human hepatocellular carcinoma, possibly through inhibition of Bcl-2 family proteins. J Hepatol. 2006 Jun;44(6):1074–1082. doi: 10.1016/j.jhep.2005.11.045. [DOI] [PubMed] [Google Scholar]
- 43.Charlotte F, L’Hermine A, Martin N, Geleyn Y, Nollet M, Gaulard P, et al. Immunohistochemical detection of bcl-2 protein in normal and pathological human liver. Am J Pathol. 1994 Mar;144(3):460–465. [PMC free article] [PubMed] [Google Scholar]
- 44.Terada T, Nakanuma Y. Expression of apoptosis, proliferating cell nuclear antigen, and apoptosis-related antigens (bcl-2, c-myc, Fas, Lewis(y) and p53) in human cholangiocarcinomas and hepatocellular carcinomas. Pathol Int. 1996 Oct;46(10):764–770. doi: 10.1111/j.1440-1827.1996.tb03546.x. [DOI] [PubMed] [Google Scholar]
- 45.Zeppa P, Benincasa G, Fulciniti F, Cochand-Priollet B, Troncone G, Vetrani A, et al. Apoptosis and cytologic differentiation in hepatocellular carcinoma on fine needle aspiration samples. Acta Cytol. 1996 Sep-Oct;40(5):861–866. doi: 10.1159/000333992. [DOI] [PubMed] [Google Scholar]
- 46.Zhao M, Zhang NX, Economou M, Blaha I, Laissue JA, Zimmermann A. Immunohistochemical detection of bcl-2 protein in liver lesions: bcl-2 protein is expressed in hepatocellular carcinomas but not in liver cell dysplasia. Histopathology. 1994 Sep;25(3):237–245. doi: 10.1111/j.1365-2559.1994.tb01323.x. [DOI] [PubMed] [Google Scholar]
- 47.Pianko S, Patella S, Sievert W. Alcohol consumption induces hepatocyte apoptosis in patients with chronic hepatitis C infection. J Gastroenterol Hepatol. 2000 Jul;15(7):798–805. doi: 10.1046/j.1440-1746.2000.02083.x. [DOI] [PubMed] [Google Scholar]
- 48.Blagosklonny MV. Unwinding the loop of Bcl-2 phosphorylation. Leukemia. 2001 Jun;15(6):869–874. doi: 10.1038/sj.leu.2402134. [DOI] [PubMed] [Google Scholar]
- 49.Ito T, Deng X, Carr B, May WS. Bcl-2 phosphorylation required for anti-apoptosis function. J Biol Chem. 1997 May 2;272(18):11671–11673. doi: 10.1074/jbc.272.18.11671. [DOI] [PubMed] [Google Scholar]
- 50.De Chiara G, Marcocci ME, Torcia M, Lucibello M, Rosini P, Bonini P, et al. Bcl-2 Phosphorylation by p38 MAPK: identification of target sites and biologic consequences. J Biol Chem. 2006 Jul 28;281(30):21353–21361. doi: 10.1074/jbc.M511052200. [DOI] [PubMed] [Google Scholar]
- 51.Simizu S, Tamura Y, Osada H. Dephosphorylation of Bcl-2 by protein phosphatase 2A results in apoptosis resistance. Cancer Sci. 2004 Mar;95(3):266–270. doi: 10.1111/j.1349-7006.2004.tb02214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Srivastava RK, Mi QS, Hardwick JM, Longo DL. Deletion of the loop region of Bcl-2 completely blocks paclitaxel-induced apoptosis. Proc Natl Acad Sci U S A. 1999 Mar 30;96(7):3775–3780. doi: 10.1073/pnas.96.7.3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Deng X, Xiao L, Lang W, Gao F, Ruvolo P, May WS., Jr Novel role for JNK as a stress-activated Bcl2 kinase. J Biol Chem. 2001 Jun 29;276(26):23681–23688. doi: 10.1074/jbc.M100279200. [DOI] [PubMed] [Google Scholar]
- 54.Deng X, Ruvolo P, Carr B, May WS., Jr Survival function of ERK1/2 as IL-3-activated, staurosporine-resistant Bcl2 kinases. Proc Natl Acad Sci U S A. 2000 Feb 15;97(4):1578–1583. doi: 10.1073/pnas.97.4.1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mai H, May WS, Gao F, Jin Z, Deng X. A functional role for nicotine in Bcl2 phosphorylation and suppression of apoptosis. J Biol Chem. 2003 Jan 17;278(3):1886–1891. doi: 10.1074/jbc.M209044200. [DOI] [PubMed] [Google Scholar]
- 56.Basu A, You SA, Haldar S. Regulation of Bcl2 phosphorylation by stress response kinase pathway. Int J Oncol. 2000 Mar;16(3):497–500. doi: 10.3892/ijo.16.3.497. [DOI] [PubMed] [Google Scholar]
- 57.Ruvolo PP, Deng X, Ito T, Carr BK, May WS. Ceramide induces Bcl2 dephosphorylation via a mechanism involving mitochondrial PP2A. J Biol Chem. 1999 Jul 16;274(29):20296–20300. doi: 10.1074/jbc.274.29.20296. [DOI] [PubMed] [Google Scholar]
- 58.Li Z, Srivastava S, Yang X, Mittal S, Norton P, Resau J, et al. A hierarchical approach employing metabolic and gene expression profiles to identify the pathways that confer cytotoxicity in HepG2 cells. BMC Syst Biol. 2007;1:21. doi: 10.1186/1752-0509-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jammi NV, Whitby LR, Beal PA. Small molecule inhibitors of the RNA-dependent protein kinase. Biochem Biophys Res Commun. 2003 Aug 15;308(1):50–57. doi: 10.1016/s0006-291x(03)01318-4. [DOI] [PubMed] [Google Scholar]
- 60.Eley HL, Tisdale MJ. Skeletal muscle atrophy, a link between depression of protein synthesis and increase in degradation. J Biol Chem. 2007 Mar 9;282(10):7087–7097. doi: 10.1074/jbc.M610378200. [DOI] [PubMed] [Google Scholar]
- 61.Gilfoy FD, Mason PW. West Nile virus-induced interferon production is mediated by the double-stranded RNA-dependent protein kinase PKR. J Virol. 2007 Oct;81(20):11148–11158. doi: 10.1128/JVI.00446-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Koromilas AE, Roy S, Barber GN, Katze MG, Sonenberg N. Malignant transformation by a mutant of the IFN-inducible dsRNA-dependent protein kinase. Science (New York, NY) 1992 Sep 18;257(5077):1685–1689. doi: 10.1126/science.1382315. [DOI] [PubMed] [Google Scholar]
- 63.Meurs EF, Galabru J, Barber GN, Katze MG, Hovanessian AG. Tumor suppressor function of the interferon-induced double-stranded RNA-activated protein kinase. Proceedings of the National Academy of Sciences of the United States of America. 1993 Jan 1;90(1):232–236. doi: 10.1073/pnas.90.1.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumar A, Yang YL, Flati V, Der S, Kadereit S, Deb A, et al. Deficient cytokine signaling in mouse embryo fibroblasts with a targeted deletion in the PKR gene: role of IRF-1 and NF-kappaB. Embo J. 1997 Jan 15;16(2):406–416. doi: 10.1093/emboj/16.2.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cuddihy AR, Li S, Tam NW, Wong AH, Taya Y, Abraham N, et al. Double-stranded-RNA-activated protein kinase PKR enhances transcriptional activation by tumor suppressor p53. Mol Cell Biol. 1999 Apr;19(4):2475–2484. doi: 10.1128/mcb.19.4.2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tamatani M, Che YH, Matsuzaki H, Ogawa S, Okado H, Miyake S, et al. Tumor necrosis factor induces Bcl-2 and Bcl-x expression through NFkappaB activation in primary hippocampal neurons. J Biol Chem. 1999 Mar 26;274(13):8531–8538. doi: 10.1074/jbc.274.13.8531. [DOI] [PubMed] [Google Scholar]
- 67.Chen C, Edelstein LC, Gelinas C. The Rel/NF-kappaB family directly activates expression of the apoptosis inhibitor Bcl-x(L) Mol Cell Biol. 2000 Apr;20(8):2687–2695. doi: 10.1128/mcb.20.8.2687-2695.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang CY, Mayo MW, Korneluk RG, Goeddel DV, Baldwin AS., Jr NF-kappaB antiapoptosis: induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science. 1998 Sep 11;281(5383):1680–1683. doi: 10.1126/science.281.5383.1680. [DOI] [PubMed] [Google Scholar]
- 69.Wu H, Lozano G. NF-kappa B activation of p53 A potential mechanism for suppressing cell growth in response to stress. J Biol Chem. 1994 Aug 5;269(31):20067–20074. [PubMed] [Google Scholar]
- 70.Kucharczak J, Simmons MJ, Fan Y, Gelinas C. To be, or not to be: NF-kappaB is the answer--role of Rel/NF-kappaB in the regulation of apoptosis. Oncogene. 2003 Dec 8;22(56):8961–8982. doi: 10.1038/sj.onc.1207230. [DOI] [PubMed] [Google Scholar]
- 71.Li M, Shillinglaw W, Henzel WJ, Beg AA. The Rela(p65) subunit of NF-kappaB is essential for inhibiting double-stranded RNA-induced cytotoxicity. J Biol Chem. 2001 Jan 12;276(2):1185–1194. doi: 10.1074/jbc.M006647200. [DOI] [PubMed] [Google Scholar]
- 72.Willis SN, Adams JM. Life in the balance: how BH3-only proteins induce apoptosis. Curr Opin Cell Biol. 2005 Dec;17(6):617–625. doi: 10.1016/j.ceb.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Takizawa T, Tatematsu C, Nakanishi Y. Double-stranded RNA-activated protein kinase interacts with apoptosis signal-regulating kinase 1. Implications for apoptosis signaling pathways. Eur J Biochem. 2002 Dec;269(24):6126–6132. doi: 10.1046/j.1432-1033.2002.03325.x. [DOI] [PubMed] [Google Scholar]
- 74.Ichijo H, Nishida E, Irie K, ten Dijke P, Saitoh M, Moriguchi T, et al. Induction of apoptosis by ASK1, a mammalian MAPKKK that activates SAPK/JNK and p38 signaling pathways. Science. 1997 Jan 3;275(5296):90–94. doi: 10.1126/science.275.5296.90. [DOI] [PubMed] [Google Scholar]
- 75.Chang L, Karin M. Mammalian MAP kinase signalling cascades. Nature. 2001 Mar 1;410(6824):37–40. doi: 10.1038/35065000. [DOI] [PubMed] [Google Scholar]
- 76.Whitmarsh AJ, Cavanagh J, Tournier C, Yasuda J, Davis RJ. A mammalian scaffold complex that selectively mediates MAP kinase activation. Science. 1998 Sep 11;281(5383):1671–1674. doi: 10.1126/science.281.5383.1671. [DOI] [PubMed] [Google Scholar]
- 77.Davis RJ. Signal transduction by the JNK group of MAP kinases. Cell. 2000 Oct 13;103(2):239–252. doi: 10.1016/s0092-8674(00)00116-1. [DOI] [PubMed] [Google Scholar]
- 78.Liu J, Lin A. Role of JNK activation in apoptosis: a double-edged sword. Cell Res. 2005 Jan;15(1):36–42. doi: 10.1038/sj.cr.7290262. [DOI] [PubMed] [Google Scholar]
- 79.Zhang H, Ozaki I, Mizuta T, Yoshimura T, Matsuhashi S, Eguchi Y, et al. Transforming growth factor-beta 1-induced apoptosis is blocked by beta 1-integrin-mediated mitogen-activated protein kinase activation in human hepatoma cells. Cancer Sci. 2004 Nov;95(11):878–886. doi: 10.1111/j.1349-7006.2004.tb02197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Liedtke C, Plumpe J, Kubicka S, Bradham CA, Manns MP, Brenner DA, et al. Jun kinase modulates tumor necrosis factor-dependent apoptosis in liver cells. Hepatology. 2002 Aug;36(2):315–325. doi: 10.1053/jhep.2002.34615. [DOI] [PubMed] [Google Scholar]
- 81.Chen YN, Cheng CC, Chen JC, Tsauer W, Hsu SL. Norcantharidin-induced apoptosis is via the extracellular signal-regulated kinase and c-Jun-NH2-terminal kinase signaling pathways in human hepatoma HepG2 cells. Br J Pharmacol. 2003 Oct;140(3):461–470. doi: 10.1038/sj.bjp.0705461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Remizov O, Jakubov R, Dufer M, Krippeit Drews P, Drews G, Waring M, et al. Palmitate-induced Ca2+-signaling in pancreatic beta-cells. Mol Cell Endocrinol. 2003 Dec 30;212(1-2):1–9. doi: 10.1016/j.mce.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 83.Aktas H, Fluckiger R, Acosta JA, Savage JM, Palakurthi SS, Halperin JA. Depletion of intracellular Ca2+ stores, phosphorylation of eIF2alpha, and sustained inhibition of translation initiation mediate the anticancer effects of clotrimazole. Proc Natl Acad Sci U S A. 1998 Jul 7;95(14):8280–8285. doi: 10.1073/pnas.95.14.8280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dey M, Cao C, Dar AC, Tamura T, Ozato K, Sicheri F, et al. Mechanistic link between PKR dimerization, autophosphorylation, and eIF2alpha substrate recognition. Cell. 2005 Sep 23;122(6):901–913. doi: 10.1016/j.cell.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 85.Lemaire PA, Lary J, Cole JL. Mechanism of PKR activation: dimerization and kinase activation in the absence of double-stranded RNA. J Mol Biol. 2005 Jan 7;345(1):81–90. doi: 10.1016/j.jmb.2004.10.031. [DOI] [PubMed] [Google Scholar]
- 86.Peters T. All about albumin : biochemistry, genetics, and medical applications. Academic Press; San Diego: 1996. pp. xx–432. [Google Scholar]
- 87.Pataer A, Vorburger SA, Chada S, Balachandran S, Barber GN, Roth JA, et al. Melanoma differentiation-associated gene-7 protein physically associates with the double-stranded RNA-activated protein kinase PKR. Mol Ther. 2005 May;11(5):717–723. doi: 10.1016/j.ymthe.2005.01.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



