Abstract
Background
Laboratory-based monitoring of antiretroviral therapy is essential but adds a significant cost to HIV care. The World Health Organization 2006 guidelines support the use of CD4 lymphocyte count (CD4) to define treatment failure in resource-limited settings.
Methods
We compared CD4 obtained on replicate samples from 497 HIV-positive Ugandans (before and during ART) followed for 18 months by 2 manual bead-based assays, Dynabeads (Dynal Biotech), and Cytospheres (Beckman Coulter) with those generated by flow cytometry at the Infectious Diseases Institute in Kampala, Uganda.
Results
We tested 1671 samples (123 before ART) with Dynabeads and 1444 samples (91 before ART) with Cytospheres. Mean CD4 was 231 cells/mm3 (SD, 139) and 239 cells/mm3 (SD, 140) by Dynabeads and flow cytometry, respectively. Mean CD4 was 186 cells/mm3 (SD, 101) and 242 cells/mm3 (SD, 136) by Cytospheres and flow cytometry, respectively. The mean difference in CD4 count by flow cytometry versus Dynabeads were 8.8 cells/mm3 (SD, 76.0) and versus Cytospheres were 56.8 cells/mm3 (SD, 85.8). The limits of agreement were -140.9 to 158.4 cells/mm3 for Dynabeads and -112.2 to 225.8 cells/mm3 for Cytospheres. Linear regression analysis showed higher correlation between flow cytometry and Dynabeads (r = 0.85, r2 = 0.73, slope = 0.85, intercept = 28) compared with the correlation between flow cytometry and Cytospheres (r = 0.78, r2 = 0.60, slope = 0.58, intercept = 45). Area under the receiver operating characteristics curve to predict CD4 <200 cells/mm3 was 0.928 for Dynabeads and 0.886 for Cytospheres.
Conclusion
Although Dynabeads and Cytospheres both underestimated CD4 lymphocyte count compared with flow cytometry, in resource-limited settings with low daily throughput, manual bead-based assays may provide a less expensive alternative to flow cytometry.
Keywords: CD4 lymphocyte counts, HIV-1 viral load, monitoring and evaluation, antiretroviral therapy, resource-limited setting, Uganda
INTRODUCTION
Of the estimated 33.2 million persons infected with HIV-1 worldwide, 22.5 million live in sub-Saharan Africa.1 And antiretroviral therapy (ART) availability has expanded dramatically in sub-Saharan Africa, thus increasing the importance of laboratory methods for initiating treatment and monitoring response to therapy. Government and nongovernmental organizations have worked to increase availability and to decrease costs of laboratory tests. For example, in 2004, the Clinton Foundation HIV/AIDS Initiative leveraged an agreement with companies, including Beckman Coulter (CD4 lymphocyte count) and Roche Diagnostics (HIV viral load), to provide laboratory tests priced lower than market rates in resource-limited settings. Yet, despite efforts to reduce costs of diagnostics, HIV care programs are stretching to cover costs of personnel, medication, and laboratory tests.2 A report of treatment costs in South Africa estimated laboratory costs to comprise 50% of costs before ART and during the first month of treatment.3 Lower cost assays that do not sacrifice accuracy could have a major impact in costs of HIV/AIDS care.
HIV disease staging allows health care providers to ascertain which patients might benefit most from ART and opportunistic infection (OI) prophylaxis. The World Health Organization (WHO) has published guidelines for initiation of ART based on clinical signs and CD4 lymphocyte count.4,5 Because funds to pay laboratory fees may be unavailable in resource-limited settings, HIV disease staging is often limited to a clinical assessment of the patient for signs and symptoms of OI. And as the clinical expression of HIV-1 infection is often a late-stage event that can be fatal,6 earlier identification of persons who are at risk for morbidity and mortality but without clinical signs or symptoms requires laboratory assessment. Investigators in the United States and South Africa have shown that routine clinical markers lack sensitivity and cannot replace CD4 cell count and HIV viral load as indicators of successful HIV treatment.7,8
Although viral load testing provides the most accurate assessment of response to ART, its routine use is prohibitively expensive in resource-limited settings. For this reason, WHO supports CD4 cell count measurement to monitor response to ART. The 2006 WHO guidelines define CD4 cell failure as persistent CD4 levels below 100 cell/mm3 or fall of CD4 count to pretherapy baseline or 50% fall from the on-treatment peak value without concomitant infection to cause transient CD4 cell decrease.5 Limitations to this approach include delayed detection of treatment failure and increased risk of drug resistance due to persistence of HIV in the presence of antiretroviral drugs.
The primary laboratory-based method of HIV disease staging is measurement of CD4 lymphocytes. CD4 cell count is the most reliable indicator of the risk for OIs and is used to initiate ART and OI prophylaxis.9,10 The gold standard method for measuring CD4 lymphocytes is flow cytometry. In resource-limited settings, the FACSCount System (Becton Dickinson), a flow cytometry-based dedicated single-platform CD4 counting instrument, is often used.11 However, access to this method is limited in more remote settings, the reagents and machine are relatively expensive, and technical training is required. Therefore, we have compared 2 bead-based manual methods with flow cytometry.
Costs for laboratory assays include equipment and supply costs, reagents, technician time, and quality assurance and control programs. Although the approximate cost of reagents per test for a CD4 cell count is 3-5 USD by Dynabeads and 4-8 USD by Cytospheres compared with 5-20 USD by FACSCount, the equipment cost for Cytospheres and Dynabeads is 2000 USD, including the cost of a light microscope, which is far less than the cost of equipment for FACSCount machine (27,000 USD).12 The goals of this research were to compare 2 manual, bead-based methods, Dynabeads, and Cytospheres with flow cytometry for enumeration of CD4 lymphocytes in Kampala, Uganda. This study reports the utility of manual bead assays for CD4 cell enumeration in a large clinic population of participants treated with ART and followed over 18 months.
METHODS
Study Population
We recruited HIV-1-infected persons attending the Infectious Diseases Institute for HIV/AIDS treatment at Makerere University Faculty of Medicine in Kampala, Uganda. Participants were older than 18 years with serologic confirmation of HIV-1 infection, and either initiating ART or on ART. Five hundred fifty consecutive, eligible patients attending the clinic who provided written, informed consent were enrolled between May 2004 and February 2005. Of these, 497 participants had blood samples evaluated by flow cytometry and at least one of the manual methods according to availability of reagents. At enrollment and every 3 months for 18 months, a study physician conducted a clinical evaluation and participants completed a structured questionnaire administered by trained interviewers, as previously described.13
Laboratory Testing
At each visit, 10 mL of whole blood was drawn into tripotassium ethylene diamine tetraacetate vacutainer tubes. Blood was processed on site at the Infectious Diseases Institute laboratory and at the Makerere University-Johns Hopkins University Laboratory, which is College of American Pathologists certified. CD4 lymphocyte count, gold standard testing was conducted on a flow cytometer (FACSCount 2-color or FACSCalibur 4-color, Becton Dickinson, Franklin Lakes, NJ). CD4 lymphocyte count was determined on the same blood specimen on the same day by using Dynabeads, Dynal T4 Count (Dynal Biotech, A.S.A., Oslo, Norway), and Cytospheres, CD4 Manual Count (Beckman Coulter, Brea, CA). Both assays were done according to the manufacturer’s instructions. Our technician received up to 10 samples per day and performed both methods on each. We limited the number of samples to 10 per day to prevent technician fatigue and eyestrain.
The Dynabeads assay employs magnetic beads coated with CD14 antibody to bind monocytes that are captured before lymphocyte isolation. We processed these samples within 24 hours of collection. For monocyte depletion, 250 μL of ethylene diamine tetraacetate whole blood was added to 225 μL of dilution buffer and incubated with 25 μL of CD14 antibody-coated magnetic beads for 10 minutes. A magnet isolated the monocytes. Monocyte-depleted supernatant was divided into 2 microtubes, combined with 200 μL of dilution buffer and 25 μL of CD4 antibody-coated magnetic beads, and incubated for 10 minutes. After isolation of the CD4 lymphocytes with a magnet, cells were lysed and the CD4+ T-cell nuclei were stained with 20 μL of Sternheimer-Malbin solution and counted under light microscopy in 1 chamber of a 0.1-mm deep hemacytometer within 1 hour of lysis. The number of nuclei counted in the volume of 0.9 μL was then divided by 0.9 to determine the absolute CD4 cell count per microliter.
Cytospheres, a method approved by the US Food and Drug Administration, use anti-CD14 latex spheres to block monocytes and (Cytospheres) to bind to CD4+ T cells. We processed these samples within 6 hours of collection. Briefly, 10 μL of MY4 monoclonal antibody-labeled spheres was added to 100 μL of ethylene diamine tetraacetate whole blood and mixed for 2 minutes. Then 10 μL of CD4 monoclonal antibody-labeled spheres was added and mixed. Then 10 μL of the blood-latex spheres mixture was mixed for 10-15 seconds with 2% acetic acid and 0.025% crystal violet stain for lysing and staining. After staining, the sample is stable for 15 minutes. Under light microscopy, we counted cells that had 3 or more large latex spheres attached to them as CD4 lymphocytes in 1 chamber of a 0.2-mm deep hemacytometer. We used a conversion matrix included in the manufacturer’s instructions, which multiplied the number of cells counted by 7.3, to determine the absolute CD4 cell count per microliter.
Ethical Approval
The study protocol was approved by the Johns Hopkins Medicine Institutional Review Board, the Makerere University Faculty of Medicine Research and Ethics Committee, and the Uganda National Council of Science and Technology.
Statistical Analysis
Statistical analyses were performed using SAS software (version 8.2, SAS Institute, Cary, NC). Flow cytometric testing was compared with each manual bead method. Paired data were compared by linear regression, including slopes, intercepts, and Pearson correlation coefficients. Analysis of agreement between the 2 methods was done by the Bland and Altman method, which compares the difference between paired measurements against the mean of the 2 measurements. According to Bland and Altman, limits of agreement summarize lack of agreement by calculating bias, which is estimated by the mean difference (D) and the standard deviation of the differences (S). If the differences are normally distributed, then 95% of differences will lie between D - 1.96 × S and D + 1.96 × S. In addition to analysis of agreement, we determined the number of pairs where the absolute difference between manual method and flow cytometry varied by thresholds of 50, 100, and 150 cells/mm3.
We calculated sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for all paired data and for CD4 cells counts measured before ART initiation. Receiver operating characteristics (ROCs) curves evaluated the sensitivity and specificity of Dynabeads and Cytospheres to predict CD4 cell count <100, 200, and 350 cells/mm3 by flow cytometry. We calculated the area under the ROC curve of these 3 thresholds for Dynabeads and Cytospheres.
RESULTS
Patients and Baseline Characteristics
Participant characteristics are presented in Table 1. The majority of participants (88%) were treatment naive at baseline. Median CD4 lymphocyte counts at baseline were <200 cells/mm3 by flow cytometry for both treatment naive and experienced. Four hundred ninety-seven HIV-1-infected participants completed 1 (n = 11), 2 (n = 9), 3 (n = 9), 4 (n = 15), 5 (n = 107), 6 (n = 106), or 7 (n = 240) clinic visits. Median number of visits was 7 (Interquartile range, 6-8).
TABLE 1.
Characteristics and Baseline Laboratory Data of 497 HIV-Infected Participants Treated With ART at the Infectious Diseases Institute
| Demographics | |
|---|---|
| Mean age, yrs (SD) | 36.8 (7.9) |
| Men (%) | 169 (34) |
| Women (%) | 328 (66) |
| ART naive and experienced (N = 497) | |
| CD4 cell count, median | 114 cells/mm3(IQR, 39-199) |
| HIV-1 viral load, median (N = 493) | 180.500 c/mL (IQR, 39.397-435.635) |
| ART experienced (N = 61) | |
| CD4 cell count, median | 192 (IQR, 91-262) |
| HIV-1 viral load, median | 3613 (IQR, 399-122.225) |
| ART naive (N = 436) | |
| CD4 cell count, median | 109 (IQR, 33-187) |
| HIV-1 viral load, median (N = 432) | 205.222 (IQR, 66.410-464.658) |
IQR, Interquartile range.
We tested a total of 1721 paired samples from HIV-infected Ugandans treated with ART by flow cytometry. Mean CD4 count was 240 cells/mm3 by flow cytometry. One thousand six hundred seventy-one samples were evaluated by Dynabeads (123 before ART), 1444 samples by Cytospheres (91 before ART), and 1399 samples by both manual methods. Data points for manual methods were analyzed for participants seen at 1 (n = 29), 2 (n = 68), 3 (n = 199), 4 (n = 177), 5 (n = 22), and 6 (n = 2) clinic visits. Manual methods were conducted for a median of 3 visits (IQR, 3-4).
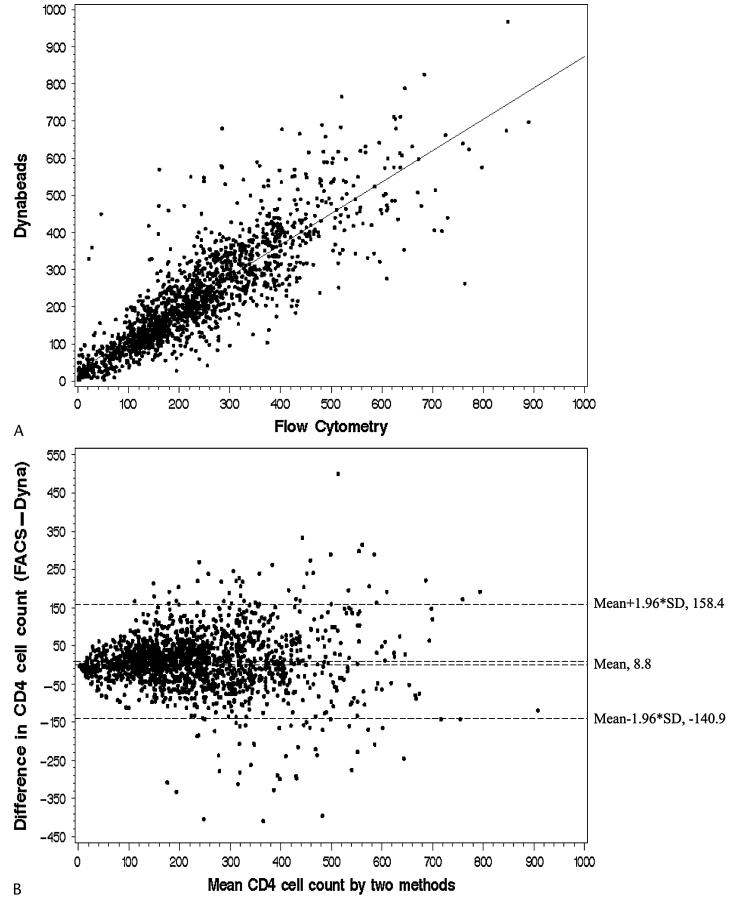
Dynabeads Versus Flow Cytometry
Mean CD4 lymphocyte count was 231 cells/mm3 (SD, 139) by Dynabeads and 239 cells/mm3 (SD, 140) by flow cytometry. The correlation between CD4 lymphocyte counts assessed by Dynabeads and flow cytometry is shown in Figure 1A, with regression slope of 0.85, intercept of 28, and Pearson correlation coefficient of 0.85. The mean difference in methods was 8.8 cells/mm3, and limits of agreement were -140.9 to 158.4 cells/mm3 (Fig. 1B). A subanalysis of 1337 samples of CD4 <350 cells/mm3 by flow cytometry compared with Dynabeads found a mean difference of 0.4 cells/mm3 and limits of agreement of -125.2 to 126.0 cells/mm3.
FIGURE 1.
A, Correlation analysis of Dynabeads and flow cytometry for CD4 cell counts (cells/mm3). Solid line represents regression line. Dynabeads = 28 + 0.85 × flow cytometry; r2 = 0.73; Pearson correlation coefficient = 0.85. B, Bland-Altman plot comparing the difference between flow cytometry (FACS) and Dynabeads (Dyna) versus the mean of the 2 methods for CD4 cell count (cells/mm3).
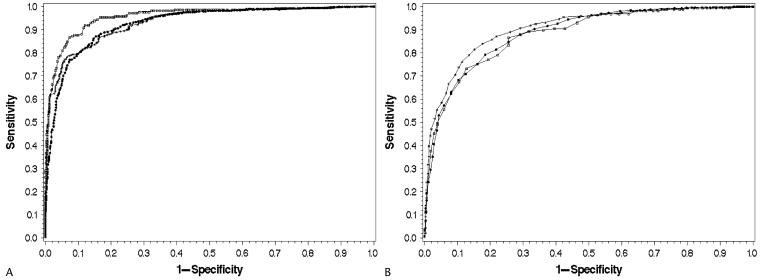
Median absolute differences by Dynabeads for those with CD4 cell count <200, 200-350, 350-500, and >500 cells/mm3 were 1, 16, 24, and 90 cells/mm3, respectively. Absolute difference was <50 cells/mm3 in 77% of cases, <100 cells/mm3 in 92% of cases, and <150 cells/mm3 in 97% of cases. For Dynabeads, sensitivity, specificity, PPV, and NPV to predict CD4 lymphocyte count <200 cells/mm3 were 87%, 84%, 82%, and 89%, respectively (Table 2). In 123 samples tested before ART initiation, both sensitivity (97%) and PPV (94%) were higher but specificity (56%) and NPV (75%) were low. Figure 3A illustrates the ROC curves for thresholds of CD4 count <100, 200, and 350 cells/mm3 by flow cytometry, and Table 2 lists the corresponding areas under the ROC curve.
TABLE 2.
Sensitivity, Specificity, PPV, NPV, and Area Under the Curve of Manual Bead Assays for CD4 Lymphocyte Count by Flow Cytometry of 497 Participants
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC | |
|---|---|---|---|---|---|
| Dynabeads (cells/mm3) | |||||
| <100 | 83 | 94 | 66 | 97 | 0.958 |
| <200 | 87 | 84 | 82 | 89 | 0.928 |
| <350 | 94 | 69 | 92 | 75 | 0.933 |
| Cytospheres (cells/mm3) | |||||
| <100 | 73 | 87 | 41 | 96 | 0.879 |
| <200 | 93 | 59 | 64 | 91 | 0.886 |
| <350 | 99 | 32 | 85 | 84 | 0.905 |
Cut-points are 100, 200, or 350 cells/mm3 for both methods concurrently. AUC, area under the curve.
FIGURE 3.
A, ROC curves for Dynabeads predicting CD4 lymphocyte count by flow cytometry. □, 100; ●, 200; *350 cells/mm3 by flow cytometry. B, ROC curves for Cytospheres predicting CD4 lymphocyte count by flow cytometry. □, 100; ●, 200; *, 350 cells/mm3 by flow cytometry.
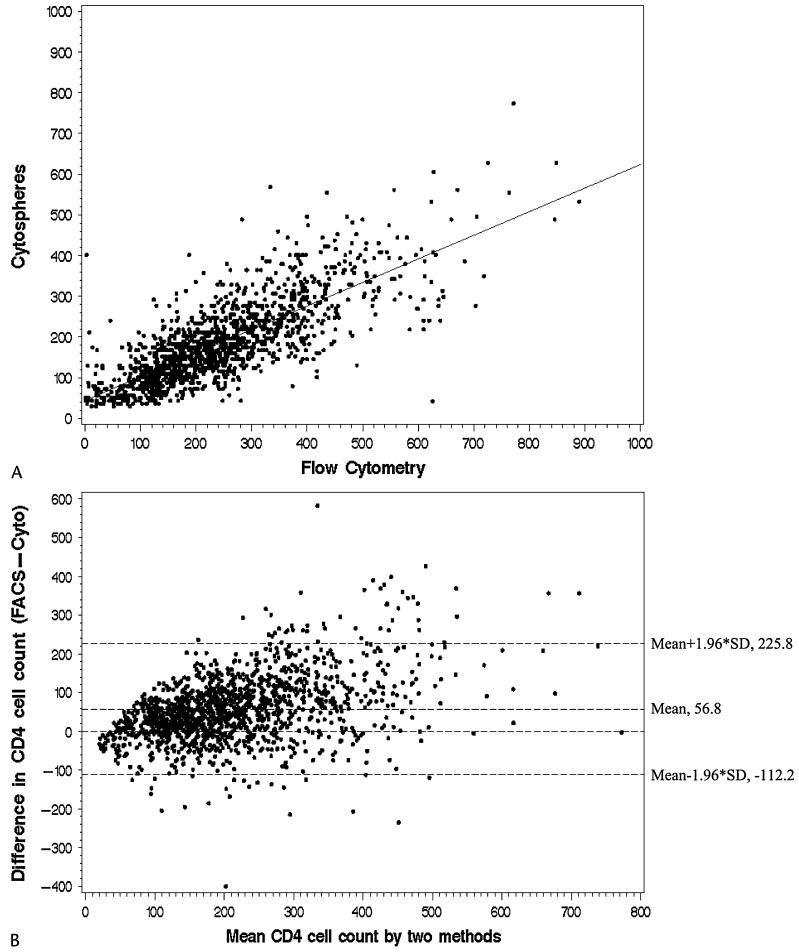
Cytospheres Versus Flow Cytometry
Mean CD4 was 186 cells/mm3 (SD, 101) by Cytospheres and 242 cells/mm3 (SD, 136) by flow cytometry. The correlation between CD4 lymphocyte counts assessed by Cytospheres and flow cytometry is shown in Figure 2A, with a regression slope of 0.58, intercept of 45, and Pearson correlation coefficient of 0.78. The mean difference in methods was 56.8 cells/mm3, and limits of agreement were -112.2 to 225.8 cells/mm3 (Fig. 2B). A subanalysis of 1156 samples of CD4 <350 cells/mm3 by flow cytometry compared with Cytospheres found a mean difference of 35.2 cells/mm3 and limits of agreement of -94.6 to 164.9 cells/mm3.
FIGURE 2.
A, Correlation analysis of Cytospheres and flow cytometry for CD4 cell counts (cells/mm3). Solid line represents regression line. Cytospheres = 45 + 0.58 × flow cytometry; r2 = 0.60; Pearson correlation coefficient = 0.78. B, Bland-Altman plot comparing the difference between flow cytometry (FACS) and Cytospheres (Cyto) versus the mean of the 2 methods for CD4 cell count (cells/mm3).
Median absolute differences by Cytospheres for those with CD4 cell count <200, 200-350, 350-500, and >500 cells/mm3 were 15, 71, 111, and 210 cells/mm3, respectively. Absolute difference was <50 cells/mm3 in 50% of cases, <100 cells/mm3 in 75% of cases, and <150 cells/mm3 in 89% of cases. For Cytospheres, sensitivity, specificity, PPV, and NPV to predict CD4 <200 cells/mm3 were 93%, 59%, 64%, and 91%, respectively (Table 2). In 91 samples tested before ART initiation, sensitivity (92%) and PPV (90%) were high but specificity (47%) and NPV (54%) were low. Figure 3B illustrates the ROC curves for thresholds of CD4 count <100, 200, and 350 cells/mm3 by flow cytometry, and Table 2 lists the corresponding areas under the ROC curve.
DISCUSSION
Although Dynabeads and Cytospheres both underestimated CD4 lymphocyte count compared with flow cytometry, in resource-limited settings with low daily throughput, manual bead-based assays may provide a less expensive alternative to flow cytometry. According to regression slopes of 0.85 for Dynabeads and 0.58 for Cytospheres (slope of 1 indicates perfect agreement), Cytospheres underestimated flow cytometry to a greater degree than Dynabeads.
According to Bland-Altman analysis of bias, limits of agreement were -140.9 to 158.4 cells/mm3 for Dynabeads and -112.2 to 225.8 cells/mm3 for Cytospheres. This indicates that Dynabeads results may be as many as 140.9 cells/mm3 greater or 158.4 cells/mm3 lesser than flow cytometry results. For clinical purposes, this amount of variation is acceptable so far as the manual methods are far less expensive than flow cytometry, and limited infrastructure in remote regions may prevent the use of more accurate methods.
Variability of CD4 enumeration has been shown to be large; investigators for the Multicenter AIDS Cohort Study reported a 95% confidence range of 118 to 337 cells/mm3 for a count of 200 cells/mm3.14 Giorgi et al15 reported coefficient of variations ranging from 20% to 30%, indicating substantial measurement error. Measurement error may occur in either the flow cytometric or hematologic determinations because flow cytometry-based estimates of CD4 cell count are determined by multiplying the percentage of CD4 lymphocytes by the absolute lymphocyte count (ie, total leukocyte count × percentage lymphocytes). This study did not evaluate reproducibility, and the results of manual methods may be more variable with greater intraoperator differences when compared with automated methods. Yet, the extent to which these differences occur may be less with low lymphocyte counts compared with high lymphocyte counts.
Clinically, the CD4 count is used as a biomarker of immune function and at low levels predicts vulnerability to OIs. The rate of decline is most critical to predict development of OIs or mortality and would represent the difference between 2 measurements. In resource-limited areas without access to more accurate methods, manual methods could be used frequently to test those with relatively low CD4 cell counts who are not yet on ART.
Due to heteroscedasticity or increased variance at greater values of CD4 cell count, Bland-Altman plots shown in Figures 1B, 2B illustrate larger differences between methods as the CD4 cell count increases. And in contrast to Dynabeads, the mean difference between Cytospheres and flow cytometry increases as CD4 count increases (Fig. 2B). However, in a subanalysis limited to 1337 samples with flow cytometry-determined CD4 cell count <350 cells/mm3, there was minimal mean difference (0.4 cells/mm3) between Dynabeads and flow cytometry, and limits of agreement were -125.2 to 126.0 cells/mm3. And the mean difference was less (35.2 versus 56.8 cells/mm3) in a similar subanalysis for Cytospheres where the limits of agreement were -94.6 to 164.9 cells/mm3. These findings illustrate reduced bias between flow cytometry and manual methods at lower cell counts.
The true positive rate or sensitivity was high for both methods at cutoffs of 200 and 350 cells/mm3. This is an anticipated effect because manual method results were on average lower than flow cytometry results, the median baseline CD4 count before ARTwas 109 cells/mm3, and this population included those presenting for ART initiation or monitoring. Higher test sensitivity translates into fewer false-negative results and would limit the numbers of patients who merited ART but were not treated for HIV disease. The true negative rate or specificity of Dynabeads (84%) and Cytospheres (59%) at 200 cells/mm3 was relatively low and, if used in clinical practice, may overestimate the need for ART initiation. However, as the range in CD4 cell count of 200-350 cells/mm3 is routinely used to initiate ART, the individual may benefit from earlier ART initiation while the society paying for ART would be burdened with increased use of ART.
The PPV ranged widely for both methods and at best was 92% for Dynabeads and 85% for Cytospheres at the highest cutoff of 350 cells/mm3. This suggests that the underestimation by manual methods may compromise the clinical utility of these tests by leading the clinician to begin treatment when the flow cytometry results would have been higher. However, at the lower thresholds of 100 and 200 cells/mm3, treatment initiation would be appropriate even if the cell count was as much as 150 cells/mm3 higher by flow cytometry due to the high risk for OIs in these individuals. NPV was relatively high for both methods and may be used clinically as a confirmation that those individuals with counts measured above 200 cells/mm3 could be monitored for clinical signs and symptoms until the next CD4 enumeration is done.
The ROC curve analysis showed higher values of area under the curve for Dynabeads (0.93-0.96) than for Cytospheres (0.88-0.91) to predict CD4 <100, 200, or 350 cells/mm3.16,17 The ROC analysis may be more relevant for the purpose of classification at clinically important thresholds than the Bland-Altman analysis of bias, which evaluates each set of paired values. Although the manual methods did not agree with flow cytometry for CD4 enumeration, they performed reasonably well as the curves are in the upper left corner of Figures 3A, B. Overall, Dynabeads outperformed Cytospheres as area under the curve values were higher for all cutoffs (Table 2).
The results of our study are comparable to those reported for Dynabeads in West Africa. Diagbouga et al18 compared Dynabeads and flow cytometry in 657 samples from 301 HIV-infected patients not on ART at laboratory sites in Côte d’Ivoire, Mali, Burkina Faso, Senegal, and Togo. The correlation coefficient was 0.89. The median difference of 7.5 cells/mm3 was insignificant for CD4 <200 cells/mm3 and increased with CD4 levels. Smaller studies have also shown a close correlation.19,20 Cross-sectional comparison of Dynabeads versus flow cytometry in Paris, France (n = 46), found a correlation coefficient of 0.91 and median difference of 56 cells/mm3.21
Results for Cytospheres are less consistent than those reported for Dynabeads.21,22 This inconsistency may be due to the relatively short period of stability (approximately 15 minutes) after addition of the lysis/stain reagent. Crowe et al20 reported a correlation coefficient of 0.69 for Cytospheres (n = 27) and attributed this to misclassifying and counting monocytes. In Western Uganda, investigators found that Cytospheres overestimated CD4 counts in a cross-sectional study including 131 samples (r = 0.725, median difference = 28 cells/mm3).23 However, results of a cross-sectional analysis that compared Cytospheres with flow cytometry in 122 samples from HIV-infected participants in Chennai, India, showed high correlation (r = 0.97, mean difference = 10 cells/mm3)24 despite a mean CD4 count of 356 cells/mm3. Other investigators have noted high correlation coefficients but did not conduct analysis of bias.25-27
The choice of CD4 enumeration technology is determined by issues such as the available personnel and equipment, technical resources, daily volume of samples, and need for CD4 percentage in pediatric HIV care. The WHO has compared the different available methods that include double- and single-platform flow cytometry, dedicated cytometers (FACSCount, CyFlow Counter, PointCare), and manual bead-based methods.12 The bead-based methods are simple, rapid tests that rely on basic technology (light microscope) and direct observation (visual counting) to enumerate CD4 lymphocytes. Five to ten samples per day may meet the requirements for smaller laboratories. However, the bead-based methods are too labor intensive for a high-volume laboratory and do not provide CD4 percentage. To reduce technician fatigue and eyestrain and to avoid inaccuracies noted with higher cell counts, we agree with Crowe et al20 that documentation of >500 cells/μL is acceptable from a technical and clinical standpoint.
Due to the relatively higher cost of viral load testing, for now, CD4 enumeration is the primary method used to assess response to ART and predict viral failure in resource-limited settings. Furthermore, evaluation of CD4 monitoring for 429 previously antiretroviral-naive participants treated for 6 months in Gaborone, Botswana, found that an increase of >50 cells/mm3 in patients with baseline of <100 cells/mm3 would detect 93% of patients with viral suppression.28 Until costs for viral load testing are reduced or less expensive technologies become available, CD4 enumeration will remain the primary method used to monitor HIV-infected individuals and their response to ART.
ACKNOWLEDGMENTS
Support for this project was provided by the Academic Alliance for AIDS Care and Prevention in Africa, the Infectious Diseases Institute, the Bill and Melinda Gates Foundation, the Division of Intramural Research of the National Institute of Allergy and Infectious Diseases, and from a National Institutes of Health, K-23 AI060384 research training award. Special thanks to Dr Joseph Margolick for his comments and Dr Merle Sande for his leadership.
REFERENCES
- 1.UNAIDS. WHO . AIDS Epidemic Update: Special Report on HIV/AIDS, December 2007. WHO; Geneva, Switzerland: 2007. [Accessed January 6, 2008]. 1-6-0008. Available at: http://data.unaids.org/pub/EPISlides/2007/2007_epiupdate_en.pdf. [Google Scholar]
- 2.Deghaye N, Pawinski RA, Desmond C. Financial and economic costs of scaling up the provision of HAART to HIV-infected health care workers in KwaZulu-Natal. S Afr Med J. 2006;96:140–143. [PubMed] [Google Scholar]
- 3.Cost of ARVs makes up less than one third of treatment cost in South African study. [Accessed May 15, 2008];Aidsmap News. 2006 11-30-2006. Available at http://www.nam.org.uk/en/news/385FF3E4-19E1-4015-9BCE-2EACE67E9FBB.asp.
- 4.World Health Organization . Scaling up Antiretroviral Therapy in Resource-Limited Settings: Treatment Guidelines for a Public Health Approach, 2003 Revision. World Health Organization; Geneva, Switzerland: 2004. [Accessed July 17, 2007]. 7-17-0007. Available at: http://www.who.int/hiv/pub/prev-care/en/arvrevision2003en.pdf. [Google Scholar]
- 5.World Health Organization . Antiretroviral Therapy for HIV Infection in Adults and Adolescents: Recommendations for a Public Health Approach. 2006 Revision. World Health Organization; Geneva, Switzerland: 2006. [Accessed July 17, 2007]. 7-17-0007. Available at: http://www.who.int/hiv/pub/guidelines/artadultguidelines.pdf. [PubMed] [Google Scholar]
- 6.Mayanja-Kizza H, Kikawa C, Lutwama F, et al. Very low CD4 T cell counts and low total lymphocyte counts at initiation of HAART are associated with a poor outcome in the first 6 months of antiretroviral treatment; Paper presented at: XVI International AIDS Conference; Toronto, Ontario, Canada. 2006. [Google Scholar]
- 7.Bagchi S, Kempf MC, Westfall AO, et al. Can routine clinical markers be used longitudinally to monitor antiretroviral therapy success in resource-limited settings? Clin Infect Dis. 2007;44:135–138. doi: 10.1086/510072. [DOI] [PubMed] [Google Scholar]
- 8.Lawn SD, Myer L, Wood R. Efficacy of antiretroviral therapy in resource-poor settings: are outcomes comparable to those in the developed world? Clin Infect Dis. 2005;41:1683–1684. doi: 10.1086/498030. [DOI] [PubMed] [Google Scholar]
- 9.Mellors JW, Munoz A, Giorgi JV, et al. Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med. 1997;126:946–54. doi: 10.7326/0003-4819-126-12-199706150-00003. [DOI] [PubMed] [Google Scholar]
- 10.Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360:119–129. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 11.Strauss K, Hannet I, Engels S, et al. Performance evaluation of the FACSCount System: a dedicated system for clinical cellular analysis. Cytometry. 1996;26:52–59. doi: 10.1002/(SICI)1097-0320(19960315)26:1<52::AID-CYTO8>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization . CD4+ T-cell Enumeration Technologies. WHO, UNAIDS; Geneva, Switzerland: 2005. [Accessed June 22, 2007]. 6-22-2007. Available at: http://www.who.int/diagnostics_laboratory/CD4_Technical_Advice_ENG.pdf. [Google Scholar]
- 13.Spacek LA, Shihab HM, Kamya MR, et al. Response to antiretroviral therapy in HIV-infected patients attending a public, urban clinic in Kampala, Uganda. Clin Infect Dis. 2006;42:252–259. doi: 10.1086/499044. [DOI] [PubMed] [Google Scholar]
- 14.Hoover DR, Graham NM, Chen B, et al. Effect of CD4+ cell count measurement variability on staging HIV-1 infection. J Acquir Immune Defic Syndr. 1992;5:794–802. [PubMed] [Google Scholar]
- 15.Giorgi JV, Cheng HL, Margolick JB, et al. The Multicenter AIDS Cohort Study Group Quality control in the flow cytometric measurement of T-lymphocyte subsets: the multicenter AIDS cohort study experience. Clin Immunol Immunopathol. 1990;55:173–186. doi: 10.1016/0090-1229(90)90096-9. [DOI] [PubMed] [Google Scholar]
- 16.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115:928–935. doi: 10.1161/CIRCULATIONAHA.106.672402. [DOI] [PubMed] [Google Scholar]
- 17.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 18.Diagbouga S, Chazallon C, Kazatchkine MD, et al. Successful implementation of a low-cost method for enumerating CD4+ T lymphocytes in resource-limited settings: the ANRS 12-26 study. AIDS. 2003;17:2201–2208. doi: 10.1097/00002030-200310170-00008. [DOI] [PubMed] [Google Scholar]
- 19.Bi X, Gatanaga H, Tanaka M, et al. Modified Dynabeads method for enumerating CD4+ T-lymphocyte count for widespread use in resource-limited situations. J Acquir Immune Defic Syndr. 2005;38:1–4. doi: 10.1097/00126334-200501010-00001. [DOI] [PubMed] [Google Scholar]
- 20.Crowe S, Turnbull S, Oelrichs R, et al. Monitoring of human immunodeficiency virus infection in resource-constrained countries. Clin Infect Dis. 2003;37:S25–S35. doi: 10.1086/375369. [DOI] [PubMed] [Google Scholar]
- 21.Didier JM, Kazatchkine MD, Demouchy C, et al. Comparative assessment of five alternative methods for CD4+ T-lymphocyte enumeration for implementation in developing countries. J Acquir Immune Defic Syndr. 2001;26:193–195. doi: 10.1097/00042560-200102010-00017. [DOI] [PubMed] [Google Scholar]
- 22.Johnson D, Hirschkorn D, Busch MP. Evaluation of four alternative methodologies for determination of absolute CD4+ lymphocyte counts. The National Heart, Lung, and Blood Institute Retrovirus Epidemiology Donor Study. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;10:522–530. [PubMed] [Google Scholar]
- 23.Karcher H, Bohning D, Downing R, et al. Comparison of two alternative methods for CD4+ T-cell determination (Coulter manual CD4 count and CyFlow) against standard dual platform flow cytometry in Uganda. Cytometry B Clin Cytom. 2006;70:163–169. doi: 10.1002/cyto.b.20093. [DOI] [PubMed] [Google Scholar]
- 24.Balakrishnan P, Dunne M, Kumarasamy N, et al. An inexpensive, simple, and manual method of CD4 T-cell quantitation in HIV-infected individuals for use in developing countries. J Acquir Immune Defic Syndr. 2004;36:1006–1010. doi: 10.1097/00126334-200408150-00002. [DOI] [PubMed] [Google Scholar]
- 25.Carella AV, Moss MW, Provost V, et al. A manual bead assay for the determination of absolute CD4+ and CD8+ lymphocyte counts in human immunodeficiency virus-infected individuals. Clin Diagn Lab Immunol. 1995;2:623–625. doi: 10.1128/cdli.2.5.623-625.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferreira OC, Jr, Suleiman G, Brites C, et al. A rapid and reliable assay to enumerate CD4+ T lymphocytes in whole blood. J Acquir Immune Defic Syndr. 1994;7:1224–1227. [PubMed] [Google Scholar]
- 27.Landay A, Ho JL, Hom D, et al. A rapid manual method for CD4+ T-cell quantitation for use in developing countries. AIDS. 1993;7:1565–1568. doi: 10.1097/00002030-199312000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Bisson GP, Gross R, Strom JB, et al. Diagnostic accuracy of CD4 cell count increase for virologic response after initiating highly active antiretroviral therapy. AIDS. 2006;20:1613–1619. doi: 10.1097/01.aids.0000238407.00874.dc. [DOI] [PubMed] [Google Scholar]