Abstract
Introduction
Hip fracture incidence is declining in North America, but trends in hip fracture recurrence have not been described.
Methods
All hip fracture events among Olmsted County, Minnesota, residents in 1980-2006 were identified. Secular trends were assessed using Poisson regression, and predictors of recurrence were evaluated with Andersen-Gill time-to-fracture regression models.
Results
Altogether, 2752 hip fractures (median age, 83 years; 76% female) were observed, including 311 recurrences. Between 1980 and 2006, the incidence of a first-ever hip fracture declined by 1.37%/year for women (p<0.001) and 0.06%/year for men (p=0.917). Among 2434 residents with a first-ever hip fracture, the cumulative incidence of a second hip fracture after 10 years was 11% in women and 6% in men, with death treated as a competing risk. Age and calendar year of fracture were independently associated with hip fracture recurrence. Accounting for the reduction in first-ever hip fracture rates over time, hip fracture recurrence appeared to decline after 1997.
Conclusion
A recent reduction in hip fracture recurrence is somewhat greater than expected from the declining incidence of hip fractures generally. Additional research is needed to determine the extent to which this can be attributed to improved patient management.
Mini-Abstact
The decline in hip fracture incidence is now accompanied by a further reduction in the likelihood of a recurrent hip fracture among survivors of the first fracture.
Keywords: Aging, Hip fracture, Incidence, Population-based study, Recurrence, Secular trends
Introduction
Persons suffering a hip fracture have an increased likelihood of additional fractures, including another hip fracture: There is about a 2-fold relative risk of recurrent hip fracture [1], while the absolute risk of hip fracture recurrence varies from 2% to 15% depending partly on the length of follow-up [2-14]. However, overall hip fracture incidence rates have been declining in North America [15-19]. Moreover, the average age at first-ever hip fracture has increased with general aging of the population [20], and hip replacement surgery is increasingly employed for fracture repair [21]. No studies have examined the impact of such changes on trends in the risk of a recurrent hip fracture. To address this issue, we extended an earlier population-based study of hip fractures among Rochester, Minnesota, residents in 1928-1992 [20] to include residents of the rural portion of the community, where hip fracture rates are lower [22], and updated it through 2006. This report focuses on the declining incidence of first hip fractures and trends in the risk of hip fracture recurrence among Olmsted County, Minnesota, residents over the 26-year period, 1980-2006.
Methods
Population-based research can be conducted in Olmsted County because medical care is virtually self-contained within the community and there are relatively few providers [23]. Most orthopedic care, for example, is provided by the Mayo Clinic, which has maintained a common medical record with its two affiliated hospitals (St. Marys and Rochester Methodist) for over 100 years. Recorded diagnoses and surgical procedures are indexed, including the diagnoses made for outpatients seen in office or clinic consultations, emergency room visits or nursing home care, as well as diagnoses recorded for hospital inpatients, at autopsy or on death certificates. Medical records of the other providers who serve the local population, most notably the Olmsted 4 Medical Center with its affiliated Olmsted Community Hospital, are also indexed and retrievable [23]. Thus, details of the medical care provided to community residents are available for study through this unique medical records linkage system (the Rochester Epidemiology Project).
Following approval by the Institutional Review Boards of Mayo Clinic and the Olmsted Medical Center, we used this database to identify all hip fractures that occurred among residents of the central city of Rochester during the 79-year period, 1928 through 2006, and for residents of Olmsted County in toto (including the rural areas) from 1980 through 2006. Except for four patients who declined to authorize the use of their records for research [24], detailed provider-linked inpatient and outpatient medical records were reviewed for all local residents with any diagnosis attributable to diagnostic rubric 820 in the International Classification of Diseases, Ninth Revision, Clinical Modification [25] or equivalent codes in earlier classification systems. Almost all were admitted to local hospitals, but the availability of outpatient data allowed us to identify fractures that occurred elsewhere, as well as a few nursing home residents who were not hospitalized. All hip fractures were included except uncommon isolated fractures of the greater or lesser trochanter. Subtrochanteric fractures, which account for about 5% of all proximal femur fractures [26], and those more distal on the femur were excluded. Radiographic confirmation was obtained in virtually all instances, but the original radiographs were not available for review. Designation of the fracture site as femur neck (cervical) or intertrochanteric was therefore based on radiologists’ and surgeons’ reports. Likewise, differentiation of initial from recurrent hip fractures was based on review of complete contemporary medical record documentation.
Incidence rates were estimated separately for the people affected by their first-ever hip fracture, as well as for all hip fracture events that occurred during the study period (including those observed among individuals whose first-ever hip fracture had occurred prior to residency in the community). In calculating hip fracture incidence rates, the entire population of Olmsted County was considered to be at risk. Denominator age- and sex-specific person-years were estimated from decennial census data with linear interpolation between census years [27] and extrapolation from 2000 to 2006. Assuming that fracture risk for any individual is approximately constant over intervals defined in the underlying rate table (e.g., 1 year), the likelihood is equivalent to a Poisson regression [28] allowing the use of standard software to estimate standard errors and calculate 95% confidence intervals (CI). Incidence rates for all hip fracture events and for first-ever hip fractures alone were directly age- and/or age-sex adjusted to the population distribution of U.S. whites in 2000; confidence intervals for the adjusted rates are based on the same assumptions as above.
To assess secular trends, the relation of crude hip fracture incidence to age, sex and year of fracture was assessed using Poisson regression [29]. Such models fit the predicted event rate as the exponential of a linear combination of gender, age-group and calendar year. Temporal changes in age and/or age-sex adjusted incidence rates were evaluated using least squares regression analysis; the slope relative to calendar year was allowed to change at the “best” potential inflection point, based on a systematic examination of all years.
Among those whose first-ever hip fracture occurred while residing in Olmsted County, the cumulative incidence of a second hip fracture was estimated for up to 20 years following the initial fracture using product-limit methods [30]. In the customary approach, patients who die are censored; when the death rate is high [31], however, this overestimates recurrent fracture risk 6 as observed by attending physicians. Therefore, we treated death as a competing event in an alternative analysis [32]. Because fracture recurrence might be reduced among persons treated with hip arthroplasty, some analyses censored follow-up when an arthroplasty was used to repair the first-ever hip fracture or was performed during follow-up. Kaplan-Meier and Hakulinen methods were also used to assess survival compared to expected death rates from the Minnesota white population. Observed and expected cumulative incidence estimates, as well as survival curves, were compared using the log-rank test [33].
In the group with a first-ever hip fracture, we also compared the number of subsequent hip fractures observed (based on the first recurrent hip fracture per person) to the number expected in this cohort during their follow-up in the community, i.e., standardized incidence ratios (SIR). Expected numbers were derived by applying calendar year-, age- and sex-specific first hip fracture incidence rates from the local population to the calendar year-, age- and sex-specific person-years of follow-up in the cohort and summing over the strata. Ninety-five percent confidence intervals for the SIRs were calculated as above [28]. Poisson regression was also used to assess the relative impact of calendar year of follow-up, adjusting for the expected number of fractures.
Finally, Andersen-Gill time-to-fracture regression models [34] were used to assess the impact of various covariates (i.e., age, gender, cause and site of the first-ever hip fracture) on the subsequent risk of another hip fracture. These models allow for the use of multiple hip fractures per subject, while appropriately accounting for the correlation. Univariate relationships between the risk of recurrent hip fractures and each clinical characteristic under consideration were first assessed. Stepwise methods with forward selection and backward elimination were then used to choose independent variables for the final models. For both univariate and multivariate models, the assumption of proportional hazards was examined for the variables considered.
Results
During the 26-year study period, 1980-2006, 2752 hip fractures occurred among Olmsted County residents (median age, 83 years; 76% female), excluding four isolated fractures of the greater or lesser trochanter. In accordance with the racial composition of the community (96% white in 1990), 97% of the patients were white. Altogether, 2441 (89%) represented a first-ever hip fracture, including 7 bilateral hip fractures, whereas the remaining 311 represented subsequent events. The overall age- and sex-adjusted (to 2000 U.S. whites) incidence of any hip fracture among Olmsted County residents during the study period was 119 per 100,000 person-years (95% CI, 114-123), including 105 per 100,000 person-years (95% CI, 101-110) for first-ever hip fractures and 13 per 100,000 person-years (95% CI, 12-15) for recurrent events. Incidence rates for all hip fractures and for first hip fractures alone are delineated in Table 1 for the 5-year period, 1998-2002, the best compromise between recent fracture numerator data and accurate population denominator estimates anchored on the 2000 census.
Table 1.
Annual incidence per 100,000 of first-ever hip fractures and all hip fracture events observed among Olmsted County, Minnesota, residents in 1998-2002, by gender and age-group
| All hip fractures | First hip fractures | |||
|---|---|---|---|---|
| Age-group | n | Rate | n | Rate |
| Men | ||||
| <50 | 9 | 4 | 9 | 4 |
| 50-59 | 8 | 26 | 8 | 26 |
| 60-69 | 14 | 72 | 14 | 72 |
| 70-79 | 38 | 305 | 35 | 281 |
| 80-89 | 66 | 1232 | 62 | 1158 |
| ≥90 | 18 | 2334 | 17 | 2204 |
| Subtotal (95% CI)† | 153 | 86 (72-100) | 145 | 82 (68-95) |
| Women | ||||
| <50 | 9 | 4 | 9 | 4 |
| 50-59 | 8 | 24 | 8 | 24 |
| 60-69 | 23 | 109 | 23 | 109 |
| 70-79 | 79 | 484 | 70 | 429 |
| 80-89 | 219 | 2033 | 189 | 1755 |
| ≥90 | 105 | 3495 | 85 | 2829 |
| Subtotal (95%CI)† | 443 | 134 (122-147) | 384 | 118 (105-130) |
| Total (95% CI) ‡ | 596 | 117 (108-126) | 529 | 104 (95-113) |
Rate per 100,000 person-years directly age-adjusted to the U.S. 2000 white population
Rate per 100,000 person-years directly age- and sex-adjusted to the U.S. 2000 white population
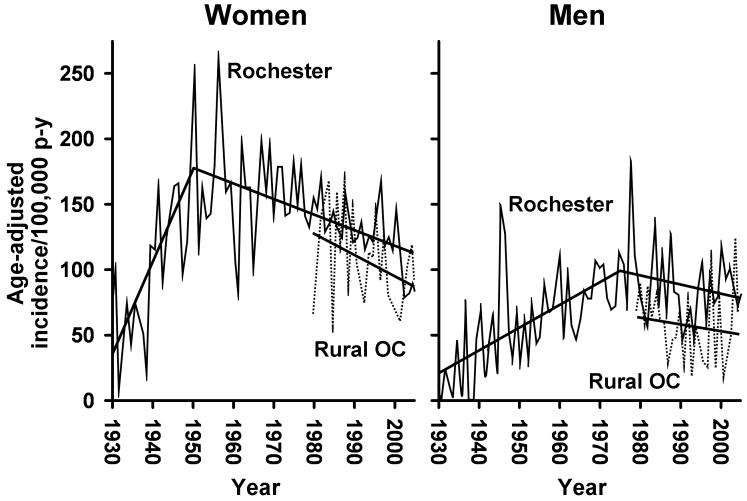
However, fracture incidence rates for Rochester residents peaked for women in 1950 and for men in 1975 (Fig. 1). Between 1980 and 2006, first-ever hip fracture incidence in Rochester declined by 1.40%/year in women and was unchanged (0.04%/year) in men, while rates for rural Olmsted County residents fell by 1.26%/year in women and 0.79%/year in men. For Olmsted County as a whole, first fracture rates declined by 1.37%/year among women (p < 0.001) and 0.06%/year among men (p = 0.917) over this period. Comparable changes for all hip fractures since 1980 were -1.42%/year (p < 0.001) and -0.44%/year (p = 0.390) for women and men, respectively. These trends were the result of hip fractures precipitated by moderate trauma (by convention, the equivalent of a fall from standing height or less), which accounted for 86% of all fractures. The overall incidence (both sexes combined) of hip fractures due to severe trauma (e.g., motor vehicle accidents and falls from greater than standing height; 13% of the total) and specific pathological processes (e.g., metastatic malignancy; 1% of the total) changed only by -1.4%/year (p = 0.071) and 5.9%/year (p = 0.302), respectively, between 1980 and 2006.
Fig. 1.
Age-adjusted incidence (per 100,000 person-years) of first-ever hip fracture among women and men residing in Rochester (1928-2006) or rural Olmsted County (1980-2006), Minnesota, by calendar year.
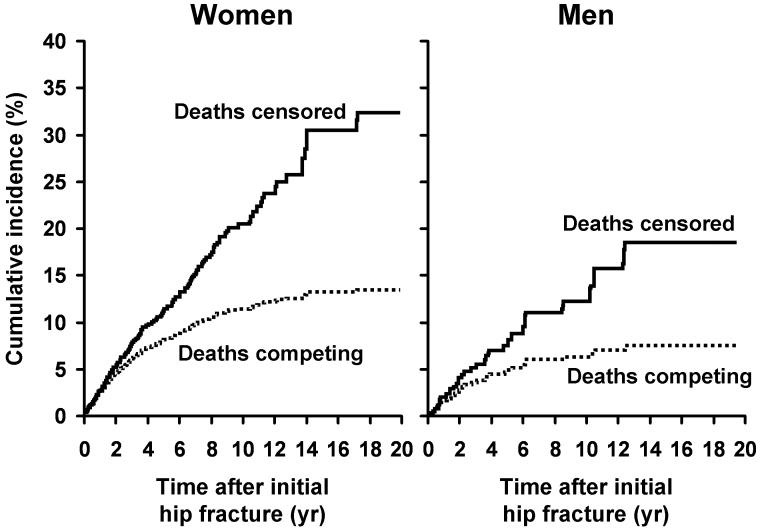
There were 2434 patients with a first-ever hip fracture (1832 women and 602 men), of whom 219 (186 women and 33 men) experienced 222 recurrent hip fractures in over 10,000 person-years of follow-up (to death in 76% of cases). The average time between the first and second hip fracture was 3.9 years (median 2.7), 4.0 years (median 2.8) in women and 3.4 years (median 2.1) in men. The cumulative incidence of a subsequent one increased steadily by time after the first-ever hip fracture event and, after 20 years, was 29% (32% in women and 18% in men) when follow-up was censored at death (Fig. 2). At 10 years, the figure was 19% (20% in women and 12% in men). However, mortality was high in this population: After one year, 22% had died compared to an expected 9%, and analogous figures after 10 years were 80% and 63%, respectively (p<0.001). Relative survival (observed versus expected) was similar in men (53%) and women (56%) at the 10-year point, and there was no significant change in mortality over calendar time after adjusting for age and sex (p=0.237). Figure 2 also shows results with death taken into account as a competing risk. In this analysis, more reflective of what would actually be observed in practice, the estimated cumulative incidence of a recurrent hip fracture was only 10% at 10 years (11% in women and 6% in men) and 12% after 20 years (13% in women and 7% in men).
Fig. 2.
Cumulative incidence of a recurrent hip fracture among 2434 Olmsted County, Minnesota, women and men who had a first-ever hip fracture in 1980-2006, with follow-up censored at death or with deaths treated as a competing risk.
Compared to age, sex- and calendar year-specific first hip fracture rates for the population generally, the overall relative risk of a recurrent hip fracture among the 2434 with a first-ever hip fracture was 1.7 (95% CI, 1.5-2.0) and was similar for residents of urban Rochester (SIR, 1.7; 95% CI, 1.5-2.0) and rural Olmsted County (SIR, 1.7; 95% CI, 1.2-2.3). The influence of selected characteristics at baseline (time of the first-ever hip fracture) on recurrent hip fracture risk is delineated in Table 2. There it can be seen that the relative risk of another fracture, adjusting for the expected risk of fracture, was lowest in those with a first-ever hip fracture in 2000-2006 in contrast to earlier decades, although this trend was not statistically significant (p=0.080). In addition, recurrent hip fracture risk differed by age (p<0.001) and gender (p=0.011). There seemed to be little effect related to the etiology of the initial fracture (p=0.606), except for a trend toward increased risk in the small number with a pathologic hip fracture at baseline. Finally, the relative risk of a subsequent hip fracture, adjusting for expected hip fractures, seemed equivalent regardless of the type (femur neck, intertrochanteric) of first hip fracture (p=0.244) or the side that was affected (p=0.839). All results were similar when each patient’s individual hips were followed separately (data not shown).
Table 2.
Observed versus expected recurrent hip fractures and standardized incidence ratios (SIR, with 95% confidence interval) among 2434 Olmsted County, Minnesota, residents with a first-ever hip fracture in 1980-2006, by nature of the first hip fracture
| Baseline characteristic | n | Observed | Expected | SIR (95% CI) |
|---|---|---|---|---|
| Calendar time | ||||
| 1980-89 | 797 | 100 | 56.2 | 1.8 (1.4-2.2) |
| 1990-99 | 951 | 98 | 52.6 | 1.9 (1.5-2.3) |
| 2000-06 | 686 | 21 | 18.6 | 1.1 (0.7-1.7) |
| Age, years | ||||
| <60 | 178 | 2 | 0.9 | 2.3 (0.3-8.1) |
| 60-69 | 191 | 23 | 4.1 | 5.7 (3.6-8.5) |
| 70-79 | 531 | 58 | 25.8 | 2.2 (1.7-2.9) |
| 80-89 | 1106 | 102 | 75.6 | 1.4 (1.1-1.6) |
| ≥90 | 428 | 34 | 21.1 | 1.6 (1.1-2.3) |
| Gender | ||||
| Women | 1832 | 186 | 115.2 | 1.6 (1.4-1.9) |
| Men | 602 | 33 | 12.3 | 2.7 (1.8-3.8) |
| Etiology | ||||
| Moderate trauma | 2082 | 193 | 112.1 | 1.7 (1.5-2.0) |
| Severe trauma | 323 | 25 | 15.1 | 1.6 (1.1-2.4) |
| Pathological | 29 | 1 | 0.2 | 5.6 (0.1-31) |
| Type | ||||
| Femoral neck | 1327 | 124 | 67.3 | 1.8 (1.5-2.2) |
| Intertrochanteric | 1103 | 94 | 59.8 | 1.6 (1.3-1.9) |
| Unknown | 4 | - | - | - |
| Side | ||||
| Right | 1205 | 106 | 62.6 | 1.7 (1.4-2.0) |
| Left | 1229 | 113 | 64.9 | 1.7 (1.4-2.1) |
However, this analysis obscures important information evident when the first-ever hip fracture type and side are considered together (Table 3). Thus, compared to site-specific Olmsted County first fracture rates, it is clear that patients with an initial femur neck fracture are at much greater relative risk of a recurrent femoral neck fracture in the opposite hip than they are of a contralateral intertrochanteric fracture or any recurrent fracture in the same hip. In part, the low risk of an ipsilateral fracture could have been due to the fact that 65% of patients with a first-ever femoral neck fracture had a hip arthroplasty at some point (90% within 3 months of fracture). However, when hips were followed separately and censored at arthroplasty, the result was similar, with an overall relative risk of recurrence in the same hip of just 0.6 (95% CI, 0.2-1.2). Likewise, the patients with an initial intertrochanteric hip fracture were at greatest risk of a recurrent contralateral intertrochanteric fracture (Table 3). They also were not at increased risk of any ipsilateral hip fracture recurrence. Only 14% of this group ever had a hip arthroplasty (60% within 3 months of fracture) but, again, when follow-up was censored at arthroplasty, the relative risk of a recurrent fracture in the same hip was only 0.2 (95% CI, 0.1-0.5). For all patients combined, the relative risk of a recurrent hip fracture in the same hip (censored at arthroplasty) was 0.3 (95% CI, 0.2-0.5), and in the opposite hip was 3.2 (95% CI, 2.8-3.7).
Table 3.
Observed versus expected recurrent hip fractures and standardized incidence ratios (SIR, with 95% confidence interval) among 2434 Olmsted County, Minnesota, residents with a first-ever hip fracture in 1980-2006, by hip fracture type and laterality
| Sites of first and second* | Observed | Expected | SIR (95% CI) |
|---|---|---|---|
| Initial femoral neck | 122 | 73.2 | 1.7 (1.4-2.0) |
| All ipsilateral recurrences | 7 | 37.5 | 0.2 (0.1-0.4) |
| Ipsilateral femoral neck | 3 | 18.9 | 0.2 (0.03-0.5) |
| Ipsilateral trochanteric | 4 | 18.6 | 0.2 (0.1-0.6) |
| All contralateral recurrences | 115 | 35.7 | 3.2 (2.7-3.9) |
| Contralateral femoral neck | 79 | 17.6 | 4.5 (3.6-5.6) |
| Contralateral trochanteric | 36 | 18.1 | 2.0 (1.4-2.8) |
| Initial trochanteric | 94 | 63.5 | 1.5 (1.2-1.8) |
| All ipsilateral recurrences | 6 | 32.4 | 0.2 (0.1-0.4) |
| Ipsilateral trochanteric | 5 | 16.3 | 0.3 (0.1-0.7) |
| Ipsilateral femoral neck | 1 | 16.1 | 0.1 (0.01-0.3) |
| All contralateral recurrences | 88 | 31.1 | 2.8 (2.3-3.5) |
| Contralateral trochanteric | 64 | 15.3 | 4.2 (3.2-5.3) |
| Contralateral femoral neck | 24 | 15.8 | 1.5 (0.97-2.3) |
Excluded from the overall figure for femoral neck fractures are two subsequent hip fractures of unknown site. Also, one initial hip fracture of uncertain site was excluded from this analysis.
In a multivariate Andersen-Gill analysis, the only independent predictors of higher hip fracture recurrence were greater age (hazard ratio [HR] per 10-year increase, 1.5; 95% CI, 1.4-1.7) and more recent calendar year of the first-ever hip fracture, which was protective (HR per 10-year increase, 0.8; 95% CI, 0.6-0.9).
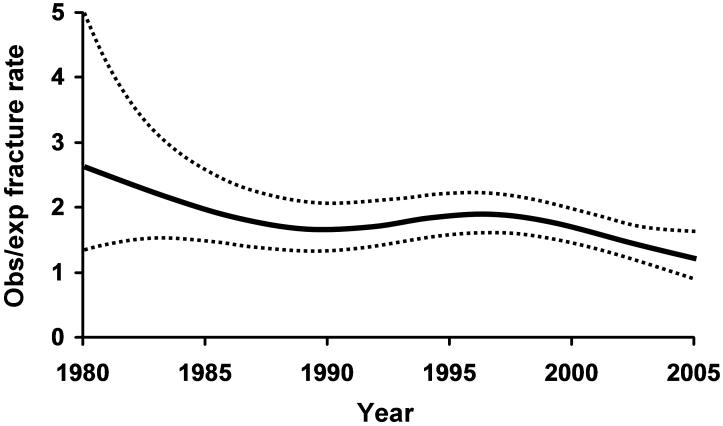
In order to determine if the trend to reduced hip fracture recurrence was related to the decline in hip fracture incidence generally, we described the temporal trend in hip fracture recurrence relative to expected hip fractures based on first-ever hip fracture incidence rates in the community (Fig. 3). While the relative risk of recurrence beyond expected seemed to decline after 1997, the overall downward trend did not achieve statistical significance in this analysis (p=0.105).
Fig. 3.
Observed compared to expected recurrent hip fractures over time among 2434 Olmsted County, Minnesota, residents with a first-ever hip fracture in 1980-2006. (Dotted lines indicate the 95% confidence interval.)
Conclusions
Altogether, 9% of the subjects in this cohort who experienced a first-ever hip fracture in 1980-2006 have experienced a recurrent hip fracture (10% in women and 5% in men), which is consistent with the 6-9% figure in most previous reports [3, 5-10, 13]. Of these, 23% occurred within one year following a first-ever hip fracture, and 70% within the first five years. However, the absolute risk of recurrence is better estimated by cumulative incidence. In the usual approach, the cumulative incidence of a second hip fracture is conditional upon survival to that point and, at 10 years, was 19%. By 10 years, however, 80% of the hip fracture patients had already died. Taking death into account as a competing risk, the cumulative incidence of a second hip fracture at 10 years was only 10%. Although death rates following the first hip fracture were greater in men than women as seen in other studies [31], the relative discrepancy in 10-year cumulative incidence of hip fracture recurrence, with and without taking death into account, in men (6% versus 12%) was comparable to the figures in women (11% versus 20%).
It has long been known that hip fracture incidence increases with age [35], and relative growth of the elderly population has been accompanied by a shift to older average age at the time of hip fracture [20]. Consistent with aging of the population nationally, the proportion of individuals in the Olmsted County population ≥ 65 years of age rose from 6% in 1930 to 11% in 2005, while the proportion ≥ 85 years old changed from 0.4 to 1.6%. Correspondingly, the mean age at hip fracture increased from 65.2 years in 1929-1942 to 78.9 years in 1983-1992 [20] and to 81.8 years in 2001-2006. This might suggest some “compression of morbidity” from a shorter duration of post-fracture disability preceding death [36]. However, like others [20, 37], we found no secular trend to reduced relative survival following a first-ever hip fracture, and in the multivariate Andersen-Gill analysis, greater age was an independent predictor of hip fracture recurrence as reported also by others [12]. Adjusting for age, there was no effect on hip fracture recurrence of gender, urban versus rural residence or etiology (i.e., severe versus moderate trauma as a cause of the first-ever hip fracture). Other recent studies have shown that high-energy fractures are as strongly associated with subsequent fracture risk as are the moderate trauma fractures traditionally attributed to osteoporosis [38].
The only other independent risk factor in the multivariate analysis was a protective effect of calendar time, with lower recurrence rates following the first-ever hip fractures in 2000-2006 compared to those occurring in the preceding two decades. The explanation for this is not readily apparent. Certainly, the overall hip fracture rates themselves were declining with time, but the improvement in hip fracture recurrence in recent years was seen even after taking the background changes in first-ever hip fracture incidence into account. Moreover, our analysis was somewhat conservative in that expected hip fracture recurrences were estimated from first-ever hip fracture rates that assumed the entire Olmsted County population to be at risk. These rates would be 2%, 7% and 17% higher in women age 65-74, 75-84 and ≥ 85 years, respectively, if hip fracture prevalence (i.e., the population not at risk of a first-ever hip fracture) were taken into account [20]; first-ever hip fracture rates for Olmsted County men would be 1%, 3% and 6% higher, respectively, in those age groups. Trends in hip fracture recurrence did not appear to reflect greater use of total or hemiarthroplasty for hip fracture repair since there was no association of age, gender or calendar time with the use of hip arthroplasty: 44%, 39%, and 43% of the patients with a hip fracture in 1980-1989, 1990-1999 and 2000-2006, respectively, underwent hip arthroplasty either at the time of surgery or during subsequent follow-up. Moreover, arthroplasty is used mostly for femoral neck fractures [13], and the trend to decreasing recurrence was similar following an initial intertrochanteric fracture (-2%/year) and an initial femoral neck fracture (-3%/year).
The downward deflection in hip fracture recurrence after 1997 that is seen in Figure 3 does coincide with the introduction of potent bisphosphonate therapy, and others have speculated that more aggressive osteoporosis treatment strategies could be responsible for the secular decline in hip fracture rates generally [18, 19]. Although pharmacologic intervention could also13 be efficacious in reducing hip fracture recurrence [14], it appears that only a minority of hip fracture patients are so treated [13, 39]. Moreover, we are unaware of specific, systematic changes in osteoporosis management among hip fracture patients in the community during this interval.
Although one might question the generalizability of these data from a small Midwestern community that is predominantly white and better educated than the white population of the United States as a whole [23], the overall annual incidence of hip fractures among persons ≥ 50 years of age in Olmsted County in 1999-2001 (386 per 100,000) is very close to the 391 per 100,000 figure for United States whites generally in 2001 [40]. Nonetheless, interpretation of these data is significantly limited by the lack of information on trends in hip fracture risk factors (e.g., bone density, bone turnover and falls). It also was not possible in the present study to determine if the recent decline in hip fracture recurrence could be attributed directly to improved management of hip fracture patients or, instead, to a reduction in underlying comorbid factors [4, 9] or an increase in obesity [41] among the survivors of a first-ever hip fracture. This is an important matter to resolve since substantial further improvement should be possible if better pharmacologic [14] and rehabilitation [42] regimens are responsible, although evidence for their effectiveness in preventing hip fracture recurrence is equivocal [43-45]. In addition, most recurrent hip fractures mirror the anatomic type (femoral neck or intertrochanteric) of the initial one [3, 5, 6, 9], and this may provide a basis for more focused interventions.
Acknowledgements
The authors would like to thank Leona Bellrichard, R.N., Marcia Erickson, R.N., Wendy Gay, R.N., Joan LaPlante, R.N., and Barbara Nolte, R.N. for assistance with data collection and Mary Roberts for help in preparing the manuscript.
Financial support This project was supported in part by grants AG-04875 and AR-30582 from the National Institutes of Health, U.S. Public Health Service.
Footnotes
Statement regarding potential conflict of interest/disclosure: The authors have no conflicts of interest to declare.
References
- 1.Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 2.Stewart IM. Fracture of neck of femur; survival and contralateral fracture. Br Med J. 1957;2:922–924. doi: 10.1136/bmj.2.5050.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melton LJ, III, Ilstrup DM, Beckenbaugh RD, et al. Hip fracture recurrence: a population-based study. Clin Orthop. 1982;167:131–138. [PubMed] [Google Scholar]
- 4.Chiu KY, Pun WK, Luk KD, et al. Sequential fractures of both hips in elderly patients--a prospective study. J Trauma. 1992;32:584–587. doi: 10.1097/00005373-199205000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Schroder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the second hip fracture. Clin Orthop. 1993:166–169. [PubMed] [Google Scholar]
- 6.Dretakis KE, Dretakis EK, Papakitsou EF, et al. Possible predisposing factors for the second hip fracture. Calcif Tissue Int. 1998;62:366–369. doi: 10.1007/s002239900446. [DOI] [PubMed] [Google Scholar]
- 7.Chapurlat RD, Bauer DC, Nevitt M, et al. Incidence and risk factors for a second hip fracture in elderly women. The Study of Osteoporotic Fractures. Osteoporos Int. 2003;14:130–136. doi: 10.1007/s00198-002-1327-6. [DOI] [PubMed] [Google Scholar]
- 8.Johnell O, Kanis JA, Oden A, et al. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004;15:175–179. doi: 10.1007/s00198-003-1514-0. [DOI] [PubMed] [Google Scholar]
- 9.Yamanashi A, Yamazaki K, Kanamori M, et al. Assessment of risk factors for second hip fractures in Japanese elderly. Osteoporos Int. 2005;16:1239–1246. doi: 10.1007/s00198-005-1835-2. [DOI] [PubMed] [Google Scholar]
- 10.Nymark T, Lauritsen JM, Ovesen O, et al. Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int. 2006;17:1353–1357. doi: 10.1007/s00198-006-0125-y. [DOI] [PubMed] [Google Scholar]
- 11.van Helden S, Cals J, Kessels F, et al. Risk of new clinical fractures within 2 years following a fracture. Osteoporos Int. 2006;17:348–354. doi: 10.1007/s00198-005-2026-x. [DOI] [PubMed] [Google Scholar]
- 12.Berry SD, Samelson EJ, Hannan MT, et al. Second hip fracture in older men and women: the Framingham Study. Arch Intern Med. 2007;167:1971–1976. doi: 10.1001/archinte.167.18.1971. [DOI] [PubMed] [Google Scholar]
- 13.Lonnroos E, Kautiainen H, Karppi P, et al. Incidence of second hip fractures. A population-based study. Osteoporos Int. 2007;18:1279–1285. doi: 10.1007/s00198-007-0375-3. [DOI] [PubMed] [Google Scholar]
- 14.Morin S, Rahme E, Behlouli H, et al. Effectiveness of antiresorptive agents in the prevention of recurrent hip fractures. Osteoporos Int. 2007;18:1625–1632. doi: 10.1007/s00198-007-0421-1. [DOI] [PubMed] [Google Scholar]
- 15.Melton LJ, III, Atkinson EJ, Madhok R. Downturn in hip fracture incidence. Public Health Rep. 1996;111:146–150. discussion 151. [PMC free article] [PubMed] [Google Scholar]
- 16.Zingmond DS, Melton LJ, III, Silverman SL. Increasing hip fracture incidence in California Hispanics, 1983 to 2000. Osteoporos Int. 2004;15:603–610. doi: 10.1007/s00198-004-1592-7. [DOI] [PubMed] [Google Scholar]
- 17.Hiebert R, Aharonoff GB, Capla EL, et al. Temporal and geographic variation in hip fracture rates for people aged 65 or older, New York State, 1985-1996. Am J Orthop. 2005;34:252–255. [PubMed] [Google Scholar]
- 18.Jaglal SB, Weller I, Mamdani M, et al. Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong? J Bone Miner Res. 2005;20:898–905. doi: 10.1359/JBMR.041231. [DOI] [PubMed] [Google Scholar]
- 19.Gehlbach SH, Avrunin JS, Puleo E. Trends in hospital care for hip fractures. Osteoporos Int. 2007;18:585–591. doi: 10.1007/s00198-006-0281-0. [DOI] [PubMed] [Google Scholar]
- 20.Melton LJ, III, Therneau TM, Larson DR. Long-term trends in hip fracture prevalence: the influence of hip fracture incidence and survival. Osteoporos Int. 1998;8:68–74. doi: 10.1007/s001980050050. [DOI] [PubMed] [Google Scholar]
- 21.Macaulay W, Pagnotto MR, Iorio R, et al. Displaced femoral neck fractures in the elderly: hemiarthroplasty versus total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:287–293. doi: 10.5435/00124635-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Madhok R, Melton LJ, III, Atkinson EJ, et al. Urban vs rural increase in hip fracture incidence. Age and sex of 901 cases 1980-89 in Olmsted County, U.S.A. Acta Orthop Scand. 1993;64:543–548. doi: 10.3109/17453679308993689. [DOI] [PubMed] [Google Scholar]
- 23.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 24.Melton LJ., III The threat to medical-records research. N Engl J Med. 1997;337:1466–1470. doi: 10.1056/NEJM199711133372012. [DOI] [PubMed] [Google Scholar]
- 25.Commission on Professional and Hospital Activities . International Classification of Diseases, 9th Revision, Clinical Modification, Volume 1, Diseases Tabular List. Commission on Professional and Hospital Activities; Ann Arbor, MI: 1978. [Google Scholar]
- 26.Arneson TJ, Melton LJ, III, Lewallen DG, et al. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop. 1988:188–194. [PubMed] [Google Scholar]
- 27.Bergstralh EJ, Offord KP, Chu CP, et al. Calculating Incidence, Prevalence and Mortality Rates for Olmsted County, Minnesota: An Update. Division of Biostatistics, Mayo Clinic; Rochester, MN: 1992. Technical Report No. 49. [Google Scholar]
- 28.Berry G. The analysis of mortality by the subject-years method. Biometrics. 1983;39:173–184. [PubMed] [Google Scholar]
- 29.Hastie TJ, Tibshirani RJ. Generalized Additive Models. Chapman and Hall; London: 1990. [Google Scholar]
- 30.Kaplan EL, Meier P. Non-parametic estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 31.Tosteson AN, Gottlieb DJ, Radley DC, et al. Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–1472. doi: 10.1007/s00198-007-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gooley TA, Leisenring W, Crowley J, et al. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706. doi: 10.1002/(sici)1097-0258(19990330)18:6<695::aid-sim60>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 33.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. John Wiley and Sons; New York, NY: 1980. [Google Scholar]
- 34.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. Springer-Verlag; New York, NY: 2000. [Google Scholar]
- 35.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 36.Fries J. The compression of morbidity: progress and potential. J Insur Med. 1990;22:93–97. [Google Scholar]
- 37.Giversen IM. Time trends of mortality after first hip fractures. Osteoporos Int. 2007;18:721–732. doi: 10.1007/s00198-006-0300-1. [DOI] [PubMed] [Google Scholar]
- 38.Mackey DC, Lui LY, Cawthon PM, et al. High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007;298:2381–2388. doi: 10.1001/jama.298.20.2381. [DOI] [PubMed] [Google Scholar]
- 39.Elliot-Gibson V, Bogoch ER, Jamal SA, et al. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int. 2004;15:767–778. doi: 10.1007/s00198-004-1675-5. [DOI] [PubMed] [Google Scholar]
- 40.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 41.Kannus P, Niemi S, Parkkari J, et al. Nationwide decline in incidence of hip fracture. J Bone Miner Res. 2006;21:1836–1838. doi: 10.1359/jbmr.060815. [DOI] [PubMed] [Google Scholar]
- 42.Stenvall M, Olofsson B, Lundstrom M, et al. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporos Int. 2007;18:167–175. doi: 10.1007/s00198-006-0226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cree MW, Juby AG, Carriere KC. Mortality and morbidity associated with osteoporosis drug treatment following hip fracture. Osteoporos Int. 2003;14:722–727. doi: 10.1007/s00198-003-1430-3. [DOI] [PubMed] [Google Scholar]
- 44.Berggren M, Stenvall M, Olofsson B, et al. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporos Int. 2008;19:801–809. doi: 10.1007/s00198-007-0507-9. [DOI] [PubMed] [Google Scholar]
- 45.Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–1809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]