Abstract
Background and Purpose: Falls are a major health problem in the elderly community; however, questions regarding incidence, risk factors, and provider response to falls exist. The purpose of this study was to examine the incidence of falls, associated factors, health care costs, and provider response to falls among Medicare beneficiaries.
Participants: The participants were 12,669 respondents to the Medicare Current Beneficiaries Survey (MCBS).
Methods: Categories of number of falls (none, one, recurrent) and injury type (medically injurious versus not medically injurious) were created from the falls supplement to the MCBS. Means and proportions for the entire Medicare population were estimated using sampling weights. The association between sociodemographic variables and fall status was modeled using ordinal or binary logistic regression. Aggregate health costs by fall category were estimated from claims data.
Results: Population estimates of falls reported in 2002 ranged from 3.7 million (single fall) to 3.1 million (recurrent falls), with an estimated 2.2 million people having a medically injurious fall. Recurrent falls were more likely with increased age, being female, being nonwhite, reporting fair or poor health, and increased number of limitations in personal activities of daily living and instrumental activities of daily living and comorbidities. Although estimates of the actual costs of falls could not be determined, “fallers” consistently had larger utilization costs than “nonfallers” for the year 2002. Fewer than half (48%) of the beneficiaries reported talking to a health care provider following a fall, and 60% of those beneficiaries reported receiving fall prevention information.
Discussion and Conclusions: Falls are common and may be associated with significant health care costs. Most importantly, health care providers may be missing many opportunities to provide fall prevention information to older people.
Falls are a major health problem in the elderly community, increasing the risk for mortality, morbidity, disability, and frailty.1,2 Among older adults, falls are the leading cause of death from injury.3 Forty percent of hospital admissions of older adults were the result of fall-related injuries, resulting in an average length of stay of 11.6 days.3 Approximately one half of older adults hospitalized for fall-related injuries are discharged to nursing homes.4 Falls that do not lead to injury often begin a downward spiral of fear that leads to inactivity and decreased strength (force-generating capacity), agility, and balance and often results in loss of independence in normal activities of self-care.5
Because of the association of falls with mortality, morbidity, and disability, several studies have investigated the incidence of falls and associated risk factors among cohorts of elderly people, including those living in the community,1,6 those who are institutionalized,7 and those with specific comorbidities.8 The Centers for Disease Control and Prevention estimates that approximately one third of people 65 years of age and older fall each year.9 Although there have been several population-based studies examining the incidence of injurious falls,7–9 the incidence of falls in the general population, and among Medicare recipients specifically, has not been investigated. Given that Medicare is the largest health insurance program in the United States, with 44 million enrollees whose medical care costs $271 billion per year,10 this represents a large gap in our knowledge. In addition, Medicare has led to significant changes for elderly people in both better health and risk-reduction, thereby reducing mortality and improving care. Further examination of falls in this population could lead to changes in care that may improve health and functioning as individuals age.
Falls represent a challenge to all health care professionals, but especially to physical therapists, who provide specialized expertise in several areas, including screening high-risk populations, assessment of risk factors related physical function (eg, balance, gait, strength), and implementation of risk-reduction strategies, including development of exercise programs, selection and training in the use of assistive devices, patient education, and identification of potential risks and barriers in the home.9 A better understanding of the incidence of falls, especially medically injurious falls, among Medicare beneficiaries has health policy implications because incidence rates can be used by physical therapists and other health care professionals to justify the development of new programs designed to target older adults at risk for falls.
Clinical guidelines related to fall prevention recommend that on a yearly basis all adults over the age of 65 years should be asked by a health care provider whether they have had a fall; among those who report a fall, efforts should be directed at determining the causes of falls, and strategies to reduce future risk should be implemented.11 There is, however, limited information regarding the extent to which guidelines are being implemented, including how often older adults discuss falls with a health care provider, and the extent to which risk factors are assessed and managed.
In 2002, a 6-question supplement was added to the health and functioning questionnaire portion of the Medicare Current Beneficiary Survey (MCBS) to address issues related to falls, including incidence and provider response. The purpose of this study was to use the falls supplement to the MCBS to provide a national estimate of the incidence of falls in the Medicare population, to identify factors associated with having recurrent falls or medically injurious falls, to examine health care provider response to reported falls, and to compare aggregate health care costs as a function of fall status.
Method
Sampling Frame
The MCBS is a longitudinal survey of the Medicare population sponsored by the Centers for Medicare and Medicaid Services, which started in 1992 and is still ongoing.10 To obtain a nationally representative sample of Medicare beneficiaries, the MCBS uses a multistage, stratified sampling design. The United States is divided into 107 primary sampling units, which are further divided into clusters by postal ZIP codes. Medicare beneficiaries within each cluster are selected by systematic random sampling by age strata, with oversampling of adults aged 85 years and older. The multistage sampling scheme is used to create weights that allow estimation of means and proportions at national and regional levels. Each person in the sample is followed for up to 4 years, and every year about one third of the sample is renewed by removing people who have been in the sample for 4 years and adding a new group of older adults. Each year a person is interviewed every 4 months, with the questions about health and functioning asked only during the autumn interview. Therefore, this ongoing survey allows for certain types of longitudinal analysis. However, because the falls supplement was implemented in the health and function interview only for 2 years, we had to limit our data analysis to a cross-sectional analysis of the 2002 MCBS. A total of 12,669 beneficiaries (65 years or older) were included in the 2002 MCBS and were given the community questionnaire and falls supplement. Interviews with beneficiaries living in institutions (eg, skilled nursing facilities) are not included in the community survey data.
Beneficiaries participating in the community survey were interviewed in person or by proxy. Data were collected on a wide variety of items, including use of health services, medical care expenditures, sources of payment, and health status and functioning. Demographic and behavioral information such as income, education level, and living arrangements also was collected.
MCBS Falls Supplement
The MCBS 2002 falls supplement was used to determine the self-reported incidence of falls and health care provider response to those falls. Responses to 2 questions—“In the past 12 months have you fallen down?” and “How many times in the last year have you fallen down?”—were used to estimate incidence of fall category: none, one, and recurrent falls (>1). Responses to the question “In that fall(s), did you hurt yourself badly enough to get medical help?” were used to establish incidence of medically injurious falls. Responses to 3 questions—“Did you talk to a doctor/medical professional about that fall(s)?” “Did the health care provider talk with you to understand why you fell?” and “Did the health care provider talk with you about how to prevent falls?”—were used to characterize health care provider response to falls.
Cost and Use Data
Cost data were used to determine total annual cost and cost by type of use as a function of fall category. Summary data from Medicare health care claims for 2002 were used to estimate average annual costs in dollars for home health, inpatient, outpatient, medical provider, and prescription medicine events.
Sociodemographic and Clinical Characteristics
Variables of interest, other than age and sex, were divided into binary categories and included race (white of non-Hispanic origin versus nonwhite), marital status (currently married versus not married), socioeconomic status (SES, annual income of $25,000 or more versus less), education (less than high school versus high school or more),12 living status (alone versus living with others), self-report of general health (endorsing fair or poor health versus good to excellent health), and smoking status (currently a smoker versus not currently a smoker).
The number of comorbidities was determined by a simple count of the respondent's endorsements of 18 clinical conditions, such as cancer, hypertension, diabetes, acute myocardial infarction, coronary heart disease, stroke, rheumatoid arthritis or osteoarthritis, Alzheimer disease, Parkinson disease, emphysema, and hip fracture. A nonresponse to a comorbidity item was classified as not having that comorbidity. Body mass index (BMI) was calculated using the individual's self-reported height and weight and was grouped into 3 categories: overweight (BMI≥30), underweight (BMI≤18), or in the normal range (18<BMI<30).
Personal activities of daily living (ADLs) included in the survey were bathing, dressing, eating, getting in and out of chairs, walking, and using the toilet. Instrumental activities of daily living (IADLs) included in the survey were use of the telephone, light housework, heavy housework, meal preparation, shopping, and money management. Limitations in ADLs and IADLs were determined using beneficiary responses to the question “Because of a health or physical problem, do you have any difficulty _______?” Possible responses were “yes,” “no,” or “doesn’t do.” A response of “doesn’t do” triggered a follow-up question as to whether the respondent did not do the activity for health or physical reasons. If the response was “yes,” the respondent was classified as having difficulty with that activity. The number of ADLs or IADLs in which a person had difficulties was categorized into 3 groups: no ADL or IADL difficulties, 1 to 3 ADL or IADL difficulties, and 4 to 6 ADL or IADL difficulties.
Data Analysis
Incidence of falls during the year prior to the interviews was estimated using the weights provided by the multistage sampling scheme used in the MCBS.10 These estimates were calculated for the entire Medicare population, as well as for subgroups defined by sociodemographic and clinical variables. For the subgroup of “fallers,” simple means and proportions were used because this subsample did not contain individuals in all primary sampling units, precluding us from using the weighted estimation. The t test was used to compare age in the groups with and without medically injurious falls. The chi-square test was used for all other categorical variables.
Ordinal logistic regression,13 using the weights provided by the MCBS sampling scheme, was used to study associations between the categories of falls (no falls, 1 fall, or 2 or more falls) and the sociodemographic and clinical factors. This analysis was not an analysis of risk factors since the data were collected in a cross-sectional fashion. Instead, it was a means of finding variables that should be studied in future longitudinal studies. Simple binary logistic regression (without weights) was used to model medically injurious falls (“yes” versus “no”) in order to identify potentially important variables for future longitudinal studies of injurious falls. Although the logistic regressions were an exploratory analysis as opposed to a confirmatory analysis, we considered variables to be statistically significant at the .05 level. Analyses were performed using SPSS version 15* and Intercooled Stata 10.0† software.
Results
Incidence and Sociodemographic and Clinical Characteristics by Fall Category
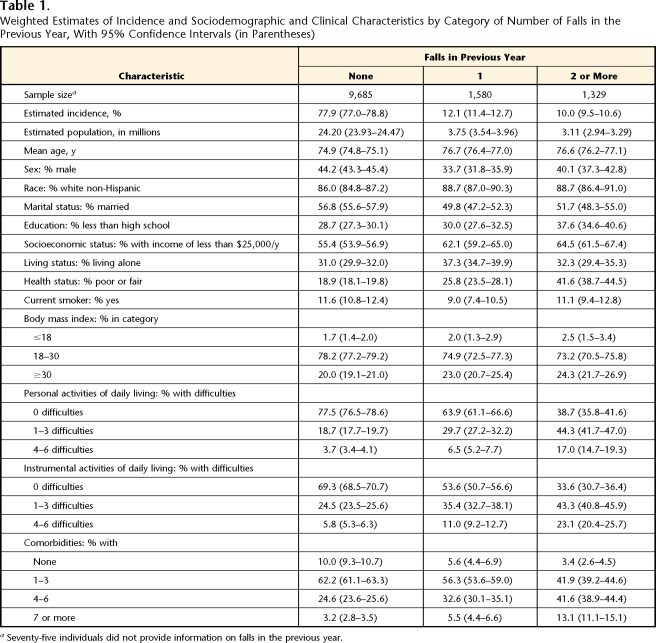
Table 1 summarizes the estimated incidence of falls and compares the distribution of sociodemographic and clinical characteristics by fall category. From the MCBS, we estimated that 22.1% of Medicare beneficiaries 65 years of age and older fell in the previous year, representing 6.86 million people. Recurrent falls occurred in 10% of this population, translating to 3.1 million people. Mean age was slightly higher for fallers than for nonfallers. Among the fallers, there were higher percentages of women, white non-Hispanic participants, and participants who were not married, had lower education, had a lower SES, were living alone, reported fair or poor health, were either underweight or overweight, had at least one ADL or IADL difficulty, and had 4 or more comorbidities.
Table 1.
Weighted Estimates of Incidence and Sociodemographic and Clinical Characteristics by Category of Number of Falls in the Previous Year, With 95% Confidence Intervals (in Parentheses)
a Seventy-five individuals did not provide information on falls in the previous year.
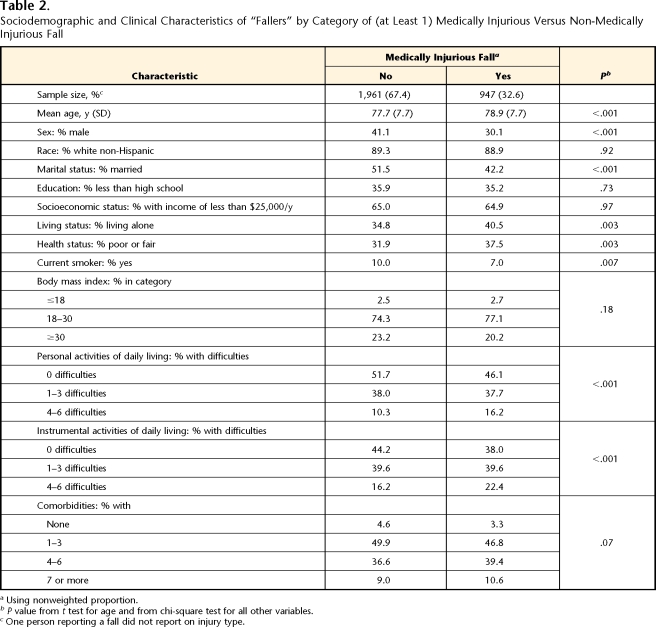
Table 2 shows sociodemographic and clinical characteristics of fallers by the categories of falls requiring versus not requiring medical attention. Thirty-three percent of the participants who reported at least one fall in the previous year required medical attention for at least one fall. This percentage would translate roughly to an estimated 2.23 million older adults who require medical attention due to a fall. Older adults who required medical attention tended to be slightly older, with higher proportions of women, participants who were not married, and participants who were living alone, reported fair or poor health, were not smoking (though this may be because this was an older group), had at least one ADL or IADL difficulty, and had more comorbidities.
Table 2.
Sociodemographic and Clinical Characteristics of “Fallers” by Category of (at Least 1) Medically Injurious Versus Non-Medically Injurious Fall
a Using nonweighted proportion.
b P value from t test for age and from chi-square test for all other variables.
c One person reporting a fall did not report on injury type.
The ordinal logistic regression analysis examined the factors associated with being in 1 of 3 categories of falling (no falls, 1 fall, and 2 or more falls). The likelihood of being in the higher categories of falling (1 fall and 2 or more falls) increased with advancing age (odds ratio [OR]=1.01, P=.02, 95% confidence interval [CI]=1.00–1.02), being female (OR=1.14, P=.01, CI=1.03–1.27), being white (OR=1.40, P<.001, CI=1.20–1.63), reporting fair or poor health (OR=1.20, P=.001, CI=1.08–1.34), reporting more ADL or IADL limitations and comorbidities (OR=1.94 [CI=1.72–2.18] and 2.39 [CI=1.90–3.00] for ADL categories compared with none; OR=1.54 [CI=1.37–1.73] and 1.94 [CI=1.59–2.35] for IADL categories compared with none; OR=1.32 [CI=1.06–1.64], 1.74 [CI=1.39–2.16], and 2.54 [CI=1.91–3.39] for categories of comorbidity compared with none; all P≤.01). Education (P=.90), SES (P=.32), marital status (P=.24), smoking status (P=.46), living status (P=.11), and BMI categories (P=.93 and .78) were not statistically significant in the model.
For injurious falls, only the subset of participants who had at least one fall was analyzed. The likelihood of having an injurious fall increased for being female (OR=1.56, P<.001, CI=1.30–1.88), having an SES of $25,000 or more (OR=1.28, P=.01, CB=1.06–1.55), not being married (OR=1.30, P=.04, CI=1.01–1.65), reporting poor or fair health (OR=1.31, P=.006, CI=1.08–1.59), and not being a current smoker (OR=1.41, P=.03, CI=1.03–1.92). Age (P=.12), race (P=.98), education (P=.42), living status (P=.67), BMI categories (P=.93 and .54), and categories of ADL (P=.81 and .06), IADL (P=.81 and .41), and comorbidities (P=.30, .28, and .23) were not statistically significant in the model.
Provider Response to Falls
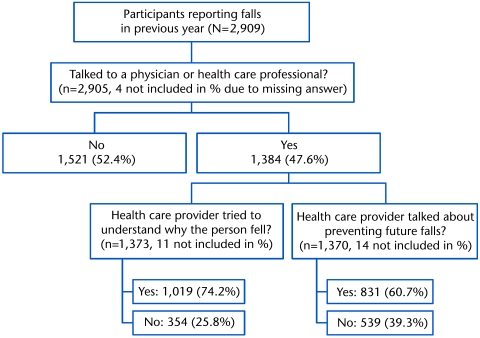
Health care provider response to falls as reported by Medicare beneficiaries is summarized in the Figure. Among beneficiaries who reported falls, fewer than half (≈48%) reported talking to a health care professional about their fall. Of those who did report talking to a health care provider, 75% indicated that their health care provider tried to understand the circumstances and reasons for the fall, and 61% reported receiving fall prevention information following their fall.
Figure.
Medicare beneficiary–reported provider response to falls.
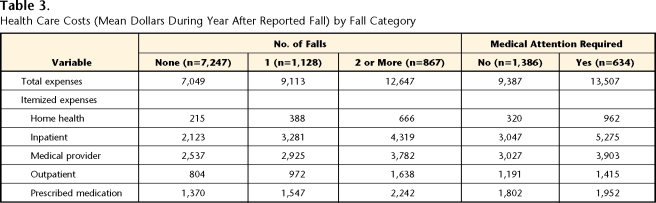
Aggregate Health Care Costs
Table 3 compares health care costs (mean US dollars per year by health care category and total costs) among the 3 fall status categories (no falls, 1 fall, and 2 or more falls). Compared with older adults reporting no falls, total aggregate health care costs were $2,000 (29%) higher in older adults reporting 1 fall and $5,600 (79%) higher among those reporting recurrent falls. The distribution of costs as a percentage of total costs by health care category was similar across the 3 fall status categories, with a range of 3% to 5% of health care dollars spent on home health, 30% to 36% spent on inpatient care, 30% to 36% spent on provider costs, 11% to 13% spent on outpatient costs, and 17% to 19% spent on medications. Total health care costs were $4,100 (44%) higher for beneficiaries reporting medically injurious falls compared with those with non-medically injurious falls. Among those with medically injurious falls, inpatient costs contributed 39% to total health care costs, compared with 32% in those with non-medically injurious falls.
Table 3.
Health Care Costs (Mean Dollars During Year After Reported Fall) by Fall Category
Discussion and Conclusions
This study estimated that 22% of community-dwelling Medicare beneficiaries 65 years of age and older have one or more falls in the previous year, slightly less than a previously published estimate of 30%.1 Consistent with other published reports,14 recurrent falls recalled retrospectively were reported by 10% of this population. Higher rates of recurrent falls (25%) have been reported among community-dwelling elderly people followed prospectively for 3 years.15 Having recurrent falls was associated with increased age, being female, being white, reporting fair or poor health, and increased limitations in activities of daily life, consistent with other published reports.16,17
Medically injurious falls were reported by 33% of the fallers in this population and, consistent with other reports,16,17 were associated with being female, having an SES of $25,000 or more, not being married, reporting poor or fair health, and not being a smoker. This study did not find that the rate of injurious falls increased with age, BMI, ADL or IADL disability, or comorbidity, as reported by other authors.7 Our study also showed a strong relationship between fall status and health care costs, consistent with the study by Rizzo et al,18 who reported a monotonic relationship between health care costs and the frequency and severity of falls among Medicare beneficiaries.
Our study showed that only half of older adults who fell reported discussing this with their health care provider. Among those who reported a fall-related discussion, 74% reported their health care provider attempted to ascertain the cause of the fall, and 61% reported receiving information on strategies to prevent future falls. These results suggest that a significant number of older adults who fall are not discussing the event with a health care provider. In addition, among those who did report falls to a health care provider, almost half reported failure to receive follow-up services related to the assessment and management of risk factors for falls. Again, this finding is consistent with other reports that health care providers underdetect and undermanage falls.19
Several authors20,21 have cited both patient-centered and system barriers to adherence to clinical guidelines related to fall prevention in older adults. Provider training in conjunction with education targeting older adults may be necessary to successfully implement an effective fall risk assessment and management program.20,21 Strategies to reduce falls among both geriatric and neurologic populations have been identified as a high priority in the profession of physical therapy, as evidenced by the American Physical Therapy Association's participation in the National Falls Prevention Coalition. However, there is no consensus as to best practices related to fall prevention that are uniformly and consistently adopted across physical therapists.
A recent study demonstrated that a multifactorial intervention, which included physical therapy, was not effective in decreasing falls in a population of community-dwelling older adults.22 Mahoney et al22 used a randomized control trial to investigate the impact of a moderate-intensity, multifactorial, community-based fall prevention program in 349 older adults (65 years of age and older) with a history of falls. The primary outcome was number of falls over a 12-month period. Participants in the intervention group received 2 in-home visits from either a trained nurse or physical therapist who assessed fall risk factors and made recommendations based on an intervention algorithm. The control group received a home safety assessment. The intervention algorithm evaluated medications, vision, balance and gait, some neurologic deficits, cognition, mood, home functioning, and home safety. Recommendations were mailed to the participants’ primary physician, and participants were asked to see their primary physician within 1 month to review recommendations. The recommendation to refer a participant for physical therapy was triggered by one of the following conditions: moderate impairment on the Berg Balance Test, abnormal gait on the Performance-Oriented Mobility Assessment, inability to stand for 30 seconds on a hard or foam surface with eyes open, or a history of pain while walking or exercising. Optional triggers including loss of balance with a sternal nudge, positive Romberg test, absent vibratory sensation at the ankle or metatarsophalangeal joint, inability to stand for 30 seconds on a hard or foam surface with eyes closed, a score less than 80 on the Activities Specific Balance Confidence Scale, and potentially risky mobility-related activity during the performance of daily activities. Physical therapists were asked to prescribe a home exercise program at the end of therapy and to encourage patients to participate in a group exercise program. Adherence to recommendations including physical therapy and exercise was determined through monthly telephone calls and or return of a monthly exercise calendar.
Mahoney and colleagues22 found no significant difference between the control and intervention groups with respect to falls. The study showed that although 84% of the participants were referred for physical therapy, one third of them refused physical therapy. The reasons cited for refusing physical therapy included difficulty traveling, concern about cost, and disbelief in its efficacy. In addition, the authors reported that among participants who attended physical therapy sessions, one half received one-time balance exercise instruction rather than a course of physical therapy, many physical therapists did not prescribe a home exercise program at the end of therapy, and there was limited progression of balance exercises. Finally, the authors reported inconsistency across physical therapists regarding the frequency, duration, and intensity of therapy needed to reduce falls.22 These findings suggest a need in the profession of physical therapy to identify and implement a consistent approach to management of falls due to physical factors such as reduced strength and impaired balance and gait among older adults.
A major limitation of this study was bias associated with a 12-month recall period. A recall period of 12 months has been shown to have good specificity but poor sensitivity.23 Our recall period of 12 months likely resulted in an underreporting of falls; thus, incidence rates are likely underestimated. “Falls” were not explicitly defined within the survey and thus were subject to respondents’ individual interpretation. In addition, health care provider response to reported falls was not measured directly but instead was determined by beneficiary report. It is possible that older adults may not have perceived some interventions, such as referral for management of gait and balance problems, as a strategy for reducing fall risk, thus failing to include this in their summary of provider response.
Our cost analysis examined per annum costs by fall category. We were unable to determine what percentage of costs were fall related, although fallers consistently had higher costs compared with nonfallers. However, it is possible that the higher costs are due to comorbidity conditions (eg, diabetes) that require higher health care utilization and are not a direct consequence of the falls. Finally, in the logistic regression models, there are 2 limitations. Although a person can be followed for up to 4 years in the MCBS, the available data for falls were cross-sectional, as the MCBS was applied during one round of the survey. Therefore, the logistic models can assess only association, and they cannot assess risk of falling. Additionally, factors statistically associated with being a recurrent faller or having an injurious fall in those models may be influenced by the correlation between variables used in the model.
Despite these limitations, this study provides the first national annual incidence estimate of falls among adults 65 years of age and older in the Medicare population and identified factors associated with being a recurrent faller or experiencing a medically injurious fall. This study confirms previous work suggesting that falls are common among elderly people and may lead to injury and increased medical costs. It extends the current literature by examining health care provider response to falls. Because there is growing consensus that interventions for prevention of falls are effective,8 these interventions should be provided routinely to elderly individuals who have fallen or who are at risk for falls. Our data suggest that this is not the case. Physical therapists are uniquely prepared to provide appropriate intervention. Clinicians not only should be aware of the high incidence of falls among community-dwelling elderly people and those factors that are associated with falls, but also should adopt consistent practices related to assessment and management of fall risk in elderly people. All patients above the age of 65 years should be asked about fall history, with follow-up screening for underlying risk factors, including balance, gait, and lower-extremity strength, in high-risk populations. Management of fall risk factors based on current best evidence needs to be integrated into physical therapist practices, and standardized measures to examine outcomes related to fall and risk factors need to be established. Finally, further research is needed to examine the effectiveness of physical therapy strategies for managing falls in both geriatric and neurologic populations.
Supplementary Material
All authors provided concept/idea/research design and writing. Dr Shumway-Cook, Dr Ciol, Dr Hoffman, and Dr Chan provided data analysis and interpretation. Dr Chan provided project management, fund procurement, facilities/equipment, institutional liaisons, and consultation (including review of manuscript before submission).
A poster presentation of this research was given at the American Congress of Rehabilitation Medicine–American Society of Neuro-rehabilitation 2006 Joint Congress; September 27-October 1, 2006; Boston, Massachusetts.
This study was supported with funding from Centers for Disease Control and Prevention (MM-0625–04/04) through an Extramural Project Grant with the Association of Academic Medical Centers. Additional resources were provided by the Centers for Medicare and Medicaid Services.
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
StataCorp LP, 4905 Lakeway Dr, College Station, TX 77845.
References
- 1.Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056. [DOI] [PubMed] [Google Scholar]
- 2.Hornbrook MC, Stevens VJ, Wingfield DJ, et al. Preventing falls among community-dwelling older persons: results from a randomized trial. Gerontologist. 1994;34:16–23. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online], 2003. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (producer). Available at: www.cdc.gov/ncipc/wisqars. Accessed July 26, 2006.
- 4.Sattin RW, Lambert Huber DA, DeVito CA, et al. The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol. 1990;131:1028–1037. [DOI] [PubMed] [Google Scholar]
- 5.Laird RD, Studenski S, Perera S, Wallace D. Fall history is an independent predictor of adverse health outcomes and utilization in the elderly. Am J Manag Care. 2001;7:1133–1138. [PubMed] [Google Scholar]
- 6.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 1998;53:M112. [DOI] [PubMed] [Google Scholar]
- 7.Gillespie LD, Gillespie WJ, Robertson MC, et al. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;4:CD000340. [DOI] [PubMed]
- 8.Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomized clinical trials. BMJ. 2004;328:680–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl 2):37–41. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Medicare & Medicaid Services Web site. Available at: http://www.cms.hhs.gov/mcbs. Accessed September 24, 2006.
- 11.American Geriatrics Society. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49:664–672. [PubMed] [Google Scholar]
- 12.Chan L, Doctor JN, MacLehose RF, et al. Do Medicare patients with disabilities receive preventive services? A population-based study. Arch Phys Med Rehabil. 1999;80:642–646. [DOI] [PubMed] [Google Scholar]
- 13.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: John Wiley & Sons Inc; 1989.
- 14.Morris M, Osborne D, Hill K, et al. Predisposing factors for occasional and multiple falls in older Australians who live at home. Aust J Physiother. 2004;50:153–159. [DOI] [PubMed] [Google Scholar]
- 15.Pluijm SM, Smit JH, Tropm EA, et al. A risk profile for identifying community-dwelling elderly with a high risk for recurrent falling: results of a 2-year prospective study. Osteoporos Int. 2006;17:417–425. [DOI] [PubMed] [Google Scholar]
- 16.Stevens JA. Falls among older adults: risk factors and prevention strategies. In: Falls Free: Promoting a National Falls Prevention Action Plan. Washington, DC: National Council on Aging; 2004:3–19.
- 17.Annual rate of nonfatal medically attended fall injuries among adults aged >65: United States 2001–2203. MMWR. 2006;31:857. [Google Scholar]
- 18.Rizzo JA, Friedkin R, Williams CS, et al. Health care utilization and costs in a Medicare population by fall status. Med Care. 1998;36:1174–1188. [DOI] [PubMed] [Google Scholar]
- 19.Rubenstein LZ, Solomon DH, Roth CP, et al. Detection and management of falls and instability in vulnerable elders by community physicians. J Am Geriatr Soc. 2004;52:1527–1531. [DOI] [PubMed] [Google Scholar]
- 20.Chou WC, Tinetti ME, King MB, et al. Perceptions of physicians on the barriers and facilitators to integrating fall risk evaluation and management into practice. J Gen Intern Med. 2006;21:117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortinsky RH, Iannuzzi-Sucich M, Baker DI, et al. Fall-risk assessment and management in clinical practice: views from healthcare providers. J Am Geriatr Soc. 2004;52:1522–1526. [DOI] [PubMed] [Google Scholar]
- 22.Mahoney JE, Shea TA, Przybelski R, et al. Kenosha county falls prevention study: a randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc. 2007;55:489–498. [DOI] [PubMed] [Google Scholar]
- 23.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53:2190–2194. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.