Abstract
The Brown Norway rat was recently described as a bubonic plague model that closely mimics human disease. We therefore evaluated the Brown Norway rat as an alternative small animal model for pneumonic plague and characterized both the efficacy and potency of vaccine candidates. When infected by intranasal instillation, these rats rapidly developed fatal pneumonic plague within 2 to 4 days of infection. Plague disease was characterized by severe alveolar edema and vascular hemorrhage in the lung in addition to fulminant necrotizing pneumonia caused by massive bacterial replication and inflammation. Twenty-four hours before death, animals developed systemic disease with an apparent delayed inflammatory response. We evaluated the ability of the protective antigen, LcrV, and a mutant derivative, V10, to protect these rats from pneumonic plague. Both were highly effective vaccines because complete protection was observed at challenge doses of 7500 LD50. Antibody analyses suggested stronger potency of V10 immune sera compared with LcrV in the passive transfer of immunity to bubonic plague, with multiple neutralizing epitopes in LcrV. Taken together, these data demonstrate the effectiveness of inhibiting type III secretion in the prevention of pneumonic plague in rats and reveal critical contributions from both the cellular and humoral immune systems. Thus, the Brown Norway rat is an appealing alternative small animal model for the study of pneumonic plague pathogenesis and immunity.
Yersinia pestis is the causative agent of pneumonic plague, a disease that has killed more people in recorded history than any other bacterial pathogen. Pneumonic plague can arise either by inhalation of Y. pestis (primary) or as a result of septicemic spread of bacteria during bubonic plague (secondary). Both involve the congestion of the lower respiratory tract, severe hemorrhage, and edema caused by massive bacterial multiplication, and both progress rapidly to death.1,2 Infection of the respiratory system by Y. pestis initially proceeds without a high degree of bacterial replication and the bacteria are generally undetectable in the sputum for at least 24 hours.1 During this time, the patient is noninfectious but may have a fever and rapid pulse. The disease then suddenly and quite rapidly progresses, together with the appearance of high bacterial titers in the sputum and blood. Lungs show severe edema and necrotizing pneumonia. Bacteria escape the lung likely via the vascular system and cause a systemic infection, with hemorrhages throughout the body, including liver, spleen, and heart.1 Systemic disease resulting from pulmonary infection manifests similar to that resulting from bubonic plague, but rapid death is believed to result from pneumonia caused by bacterial replication in the lung and the accompanying destruction of tissue. Treatment must be initiated within 12 hours of fever onset, or the infection is almost invariably fatal.2 Although Y. pestis infections still occur naturally, large-scale epidemics have not occurred because of improved sanitation practices and successful antibiotic treatment of bubonic plague patients.3,4 Nevertheless, small Y. pestis pneumonic plague outbreaks have occurred in recent years and bubonic plague remains endemic in many areas of the world.5
In 1995, two cases of fatal bubonic plague were caused by Y. pestis bacteria that had acquired plasmids that carried resistance to multiple antibiotics.6,7 It was shown subsequently that horizontal acquisition of multidrug resistant plasmids can occur at high frequency in biofilms that form in the flea gut, part of the natural life cycle of Y. pestis.8 Thus, Y. pestis threatens to emerge as a deadly multidrug resistant epidemic, and it is likely that a vaccination program represents the best line of defense against resurgent plague.9 As yet, there are no licensed vaccines for plague. Current strategies use two antigens, CaF1 and LcrV, over whole cell vaccine approaches because of unreliability and safety concerns.10,11
CaF1, or F1, is an abundant cell-surface antigen that forms a capsule-like structure on Y. pestis at 37°C.12 F1 is thought to help provide Y. pestis with the ability to avoid recognition by innate immune cells; however, this activity is not essential for virulence.13,14 F1 elicits the dominant immune response to whole cell vaccines in humans, and this response provides a high level of protection from bubonic plague but is significantly less effective against pneumonic plague.15,16 Likewise, mice vaccinated with F1 as a single subunit vaccine can be protected from bubonic plague, but are less protected from pneumonic plague.17,18,19 These data suggest that protection from pneumonic plague requires additional anti-bacterial activities that are not prevented by neutralizing F1 antibodies and raise the possibility that F1 may not be essential to vaccine formulations.20 Moreover, because F1 is not required for virulence, vaccines that are based solely on this antigen will likely be ineffective against Y. pestis caF1 mutants that arise either spontaneously or through genetic engineering.21,22,23
LcrV was first described as a protective antigen by T.W. Burrows in 1956.24 LcrV antibodies can be found in the sera of mice that have survived Y. pestis infections or that have been vaccinated with live attenuated strains of Y. pestis, but they are in relatively low abundance as compared with antibodies to F1.16 LcrV is positioned on the surface of bacteria engaged in battle with cells of the innate immune system where it is essential for virulence.25,26,27 In this location, LcrV mediates insertion of a translocation pore in the host cell membrane assembled via the type III secretion system.28 Anti-phagocytic and pro-apoptotic bacterial proteins, collectively known as Yersinia outer proteins or Yops, are then transported through this pore and into the cytoplasm of the host cell where they lead to destruction and subsequent bacterial evasion of the innate immune system.29,30,31,32,33,34 Polyclonal antibodies to LcrV raised in mice, rabbits, and nonhuman primates are able to block type III injection of Yops into macrophages, and this activity is thought to promote phagocytosis and killing by the innate immune system.14,35
In addition to its role as a virulence factor during type III secretion, LcrV can modulate immune responses through the induction of interleukin-10 secretion. This likely dampens innate and adaptive immune responses, but is thought to play only a minor role in virulence.36,37 Large amounts of LcrV circulating in the blood of mice are capable of disabling immune responses to some bacterial pathogens,37 raising concerns that LcrV may be immune-suppressive when used as a vaccine. This concern is substantiated by the recently reported clinical application of LcrV to deliberately suppress mucosal immunity.38
Nevertheless, inclusion of LcrV with F1 in a vaccine formulation produced a highly effective vaccine that protected against bubonic and pneumonic plague in mice and nonhuman primates and two formulations are currently under investigation for human use.39,40,41 Both vaccines result in the production of high levels of antibodies that neutralize Y. pestis infections, and these antibodies correlate with vaccine efficacy. In addition, each of these vaccines can protect from aerosol challenge with F1 mutant Y. pestis in mice. In all cases, immunity correlates with in vitro assays that demonstrate the ability of LcrV antibodies to block macrophage apoptosis caused by the injection of Yops.14,18,41,42,43 Results of phase I clinical trials so far indicate that humans raise antibodies with similar potency and activity against Y. pestis in both animal and in vitro assays, although it has not been formally demonstrated that these antibodies indicate immunity to plague in humans.20,44
Recently we sought to improve the safety and potency of LcrV vaccines by creating mutant variants with decreased immune-suppressive activities. We described a novel candidate called V10, which is a deletion of amino acids 271 to 300 near the carboxyl terminus of LcrV, and this deletion protein induces little to no interleukin-10 secretion from mouse and human phagocytic cells.45 This derivative was nevertheless found to be highly antigenic and elicited high titers of neutralizing IgG in the blood of vaccinated mice.46 In fact, V10 was found to be more potent than LcrV in both protection and antibody titers in the mouse pneumonic plague model. We therefore decided to further investigate its mechanism of action, and to ask whether similar findings would be made in other animal models. We focused our attention on the Brown Norway rat because of close similarities between rat and human bubonic plague.47 In this study, we describe the Brown Norway rat as a model for pneumonic plague and its use in the evaluation of LcrV plague vaccines.
Materials and Methods
Bacteria Strains and Growth Conditions
For challenge experiments, Y. pestis CO92 was streaked from frozen stock onto heart infusion agar with Congo Red and grown for 48 hours at 26°C.48 A single red colony, indicative of expression of the pgm locus was inoculated in 10 ml of heart infusion broth supplemented with 2.5 mmol/L CaCl2 and grown for 18 to 24 hours at 37°C.49 Bacteria were diluted in sterile phosphate-buffered saline (PBS) to the desired dose just before use in challenge studies. All experiments performed with Y. pestis CO92 were performed in compliance with the select agent regulations at biosafety level 3. E. coli BL21 (Novagen, San Diego, CA) was used for the overexpression and purification of recombinant LcrV and V10 as previously described.45
Pneumonic Plague Challenge Studies
Six- to eight-week-old (200 g) female Brown Norway rats were purchased from Charles River Laboratories (Wilmington, MA). Animals were housed in BSL3 containment at least 3 days before challenge. For challenge, groups of four to six animals were anesthetized with ketamine/xylazine, and bacteria prepared as described above, were instilled by pipetting into the left naris of the anesthetized animal. Infected animals were observed for recovery from anesthesia and for the development of signs of lethal plague disease for a period of 14 days. After the observation period, remaining animals were humanely euthanized by CO2 asphyxiation, a method approved by the Panel on Euthanasia of the American Veterinary Medical Association. Euthanized animals were necropsied and blood drawn by cardiac puncture. For histochemical analyses, lungs were perfused in 10% formalin and tissues were fixed in 10% formalin for 48 hours. Sections of the left lower lobe were submitted for tissue sectioning, staining with hematoxylin and eosin (H&E), and pathological analysis. For bacterial enumeration, whole tissues were homogenized in sterile PBS and plated on heart infusion agar with Congo Red. All studies conformed to guidelines set forth by the National Institutes of Health and were reviewed and approved by the Institutional Animal Care and Use Committee at the University of Chicago. A 50% lethal dose of 171 cfu, as calculated according to the method of Reed and Muench,50 was used to calculate challenge dose for disease and vaccine experiments.
Immunohistochemistry
Tissues that had been fixed in 10% formalin as described above were sectioned on slides for immunohistochemical analysis. Slides were stained with mouse anti-rat CD68 (MorphoSys, Oxford, UK) or rabbit anti-cleaved caspase-3 (Trevigen, Gaithersburg, MD) according to the manufacturer’s protocol. Detection of CD68 was achieved by secondary staining with biotinylated polyclonal rabbit anti-mouse IgG (DAKO, Carpinteria, CA), and detection of activated caspase-3 was achieved by secondary staining with polyclonal anti-rabbit IgG conjugated to horseradish peroxidase (HRP). Staining and detection were performed according to the manufacturer’s guidelines.
Immunizations
Fifty μg of recombinant protein was emulsified in 25% Alhydrogel (Brenntag Biosector, Frederikssund, Denmark) (v/v) and delivered by intramuscular injection into the leg of the animals. Animals were boosted with an equal dose of antigen emulsified in 25% Alhydrogel on day 21. On day 42, five animals per study group were deeply anesthetized and blood for antibody analysis was withdrawn by cardiac puncture followed by euthanizing the animals by CO2 asphyxiation.
Passive Transfer of Immunity
Immune sera from five rats per group were collected by cardiac puncture from animals immunized as described above. Individual serum was pooled, and IgG purified by filtration through the Melon purification kit (Pierce, Rockford, IL). Purified IgG, 400 μg, 200 μg, or 100 μg, was delivered by intraperitoneal injection to each of 10 BALB/c mice (female, 6 to 8 weeks of age). After 60 minutes, mice were challenged with 20 MLD of Y. pestis CO92 by subcutaneous injection (corresponds to 20 cfu bacteria and ∼90 to 95% lethality). Infected mice were monitored for 14 days for signs of lethal bubonic plague, including severe weight loss of >25% body mass and immobility when stimulated. The mouse protection index (MPI) was calculated as the number of susceptible mice divided by their mean time to death. These data were then normalized by dividing the sample MPI by the PBS control MPI. Neutralizing activity was concluded if the normalized value was less than 0.8 because this was the maximum variability observed in control mice between experiments. Statistical significance of time to death was evaluated by unpaired Student’s t-test; significance was concluded when P < 0.05.
Enzyme-Linked Immunosorbent Assay (ELISA)
Micro wells were coated with recombinant antigen (LcrV, V10, or CaF1) at 1 μg/ml in carbonate buffer and incubated overnight at 4°C. After washing three times with PSB-Tween, plates were incubated in PBS/1% bovine serum albumin (BSA) for 1 hour at room temperature to block nonspecific binding to wells. Dilutions of rat sera were made in PBS/1% BSA solution and 100 μl of each sample was added to the well in triplicate and incubated overnight at 4°C. Plates were washed three times with PBS/BSA. Biotinylated secondary anti-rat IgG, IgG1, or IgG2a (BD Biosciences, San Jose, CA) was then diluted in PBS/1% BSA, added to the wells, and incubated for 1 hour. Detection was performed after incubation with streptavidin-alkaline phosphatase according to the manufacturer’s recommendations, and binding measured at 450 nm in a plate reader. For antibody epitope mapping, peptides conjugated to keyhole-limpet hemocyanin were used at 1 μg/ml to coat ELISA plates. Sera from immunized rats were used as primary antibodies and incubated with antigen for 2 hours at room temperature. Anti-rat IgG conjugated to HRP was used to detect binding to the peptides according to the manufacturer’s recommendations.
Competitive ELISA
One μg/ml of recombinant LcrV was bound to a 96-well plate and incubated overnight at 4°C. After washing, plates were incubated in blocking buffer (PBS with 5% BSA); then 0.2 μg/ml of LcrV mAb BA-5 was added to each well and incubated at 4°C for 16 hours. Rat immune sera or rat serum from adjuvant-only immunized animals were diluted 1:3 in PBS with 5% BSA in duplicate. Diluted serum (0.1 ml) was added to the plates and incubated for 1 hour at 37°C and then washed three times in PBS, followed by the addition of HRP-goat anti-mouse IgG. Binding of LcrV mAb BA-5 was detected according to the manufacturer’s instructions and measured in a plate reader at 450 nm. Absorbance was adjusted for background binding and percent competition was calculated in the presence of diluted test and control serum.
Memory T-Cell Assay
Six- to eight-week-old female Brown Norway rats were immunized with Alhydrogel, LcrV, or V10 by intramuscular injection on days 0 and 21 as described above. Seven days after the boost, animals were humanely sacrificed and spleens harvested and prepared as previously described.51 The modified enzyme-linked immunospot assay (ELISpot) was used to enumerate interferon (IFN)-γ secreting T cells in the splenocyte population. Cells (1 × 107 cells/ml) were seeded in 96-well nitrocellulose-bottomed ELISpot plates and incubated for 18 hours at 37°C in the presence of 10 μg of LcrV or V10. T cells producing IFN-γ were detected by incubation with HRP-conjugated rat anti-IFN-γ following the manufacturer’s protocol.
Results
Brown Norway Rats Are Highly Susceptible to Pneumonic Plague
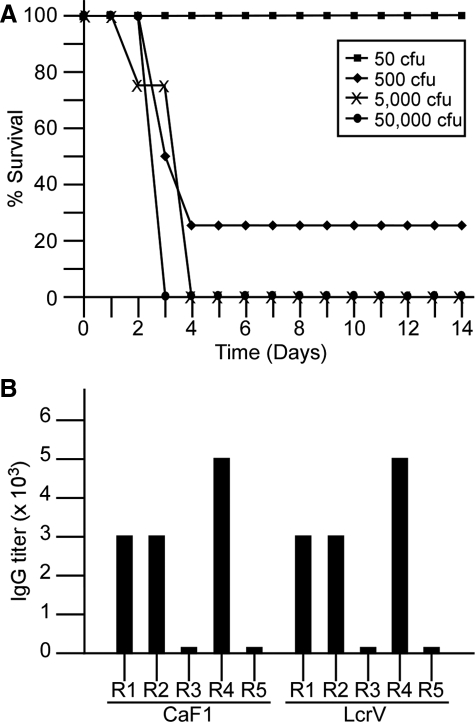
We sought to determine the susceptibility of Brown Norway rats to pneumonic plague. Y. pestis CO92 was used to infect 6- to 8-week-old Brown Norway rats by intranasal instillation. This method resulted in uniform susceptibility and rapid lethality, and all rats infected with a bacterial dose greater than or equal to 5 × 103 cfu succumbed to the infection within 96 hours (Figure 1A). We determined the 50% lethal dose in three independent experiments using the method of Reed and Muench,50 and calculated an average LD50 of 171 ± 69 cfu. In all cases disease progression presented similarly. Twenty-four hours after infection, animals appeared healthy: they were active, eating normally, and responded well to being handled. By 36 hours after infection, the animals still appeared relatively healthy, were eating and moving about when stimulated, but were often found in a hunched posture. At 48 hours after infection, a dramatic change in activity could be observed. The animals had hunched posture, rapid breathing, and responded slowly to stimulation, but little to no weight loss. Many of the animals exhibited ocular discharge shortly before death. Animals that succumbed to infection did so by day 4, all animals surviving beyond day 4 survived through the observation period of 14 days. We tested these surviving animals for seroconversion to the dominant plague antigens CaF1 and LcrV. The results showed no bacteria in the blood, but three of five of the animals had seroconverted as they harbored modest but detectable antibody titers to F1 and LcrV in their blood (Figure 1B), indicating they had developed an immune response against the bacteria. Interestingly, the remaining two animals did not appear to have mounted an immune response to the sublethal challenge by Y. pestis.
Figure 1.
Brown Norway rats are highly susceptible to pneumonic plague but only sometimes generate immunity after sublethal challenge. Groups of four to six Brown Norway rats were challenged with increasing doses of Y. pestis CO92 delivered by intranasal instillation. A: Animals succumbed to disease between 60 and 108 hours after infection, with a mean 50% lethal dose (LD50) of 171 cfu. Data shown are representative of three independent experiments. B: Rats that survived sublethal infection (R1 to R5) did not consistently develop antibodies to dominant plague antigens, CaF1 and LcrV, because only three of five survivors (R1, R2, and R4) from the experiment in A had seroconverted by day 14 after challenge.
Progression of Bacterial Growth during Pneumonic Plague in Brown Norway Rats
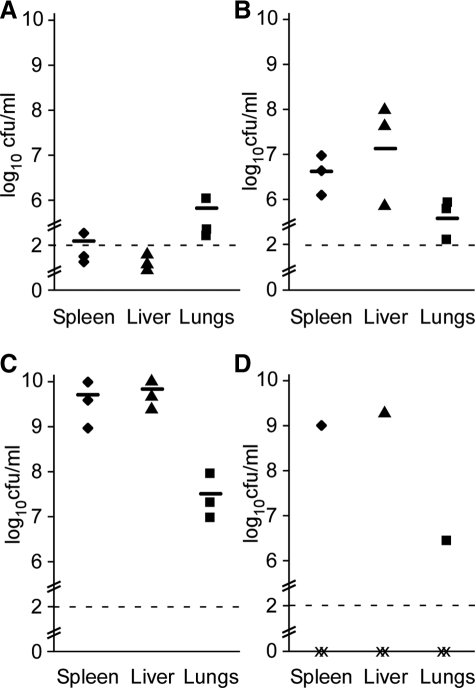
We next monitored disease progression in a time course experiment. Six- to eight-week-old Brown Norway rats were infected with 1 × 105 cfu of Y. pestis CO92 (corresponding to ∼600 MLD) by intranasal instillation. Three rats were sacrificed 60 minutes after infection, and then at 12 hours, 24 hours, 36 hours, 48 hours, and 60 hours. This dose causes lethality within 48 to 72 hours, and as such only one of three animals survived until the 60-hour time point. Sacrificed animals were necropsied and their lungs, liver, and spleen were removed. Whole tissues were then homogenized in sterile PBS and plated for viable bacteria. After 12 hours, bacteria could be recovered from the lungs, and none was recovered in any of the other tissues (data not shown). The results were similar at the 24-hour time point, with slow bacterial growth appearing in the lungs and no dissemination to other tissues (Figure 2A). These data indicate a primary lung infection is caused by this method of inoculation, with moderate initial bacterial growth and little to no disease during the first 24 hours after infection. However, the situation began to change dramatically within the next 12 hours, as by 36 hours, higher bacterial titers were observed in the lungs, and bacteria have now escaped the lung and could be recovered from distal tissues such as the spleen and liver (Figure 2B). At 48 hours, when the animals appeared visibly ill, high titers of bacteria were recovered in all tissues examined (Figure 2C). At 60 hours the animal harbored bacterial titers similar to those harvested at 48 hours after infection and appeared very near death when it was sacrificed (Figure 2D). Gross pathology of these animals showed development of large hemorrhagic lesions in the lung that could be observed as early as 36 hours and appeared in all animals by 48 hours (data not shown). Importantly all animals analyzed after 36 hours appeared visibly ill with systemic spread of bacteria. Together with the data collected during the determination of lethal dose (Figure 1A) our data suggest that Y. pestis infections of Brown Norway rats uniformly progress to fatal pneumonic plague.
Figure 2.
Time course of bacterial dissemination in rats infected with 600 LD50 Y. pestis CO92 showed systemic spread by 48 hours after infection. Viable bacteria recovered from the lung, liver, and spleen after 24 hours (A), 36 hours (B), 48 hours (C), or 60 hours (D). Three animals were analyzed per time point; two of the three animals in group 4 succumbed to the infection before 60 hours and are indicated as × on the graph. Y. pestis was identified by colony morphology and pigmentation on heart infusion agar with Congo Red; each sample was plated in triplicate; data shown are average cfu/ml of homogenized tissue. This experiment was repeated with similar results; a representative experiment is shown.
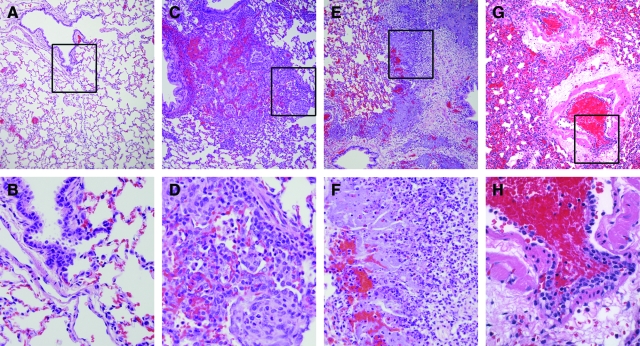
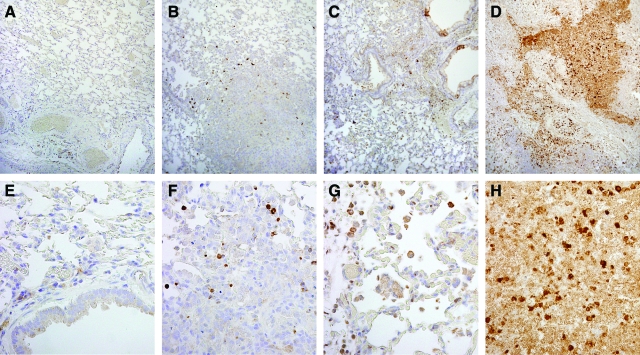
Pneumonic Plague Pathology in Brown Norway Rats
We next analyzed the pathology of disease in the lower lung, liver, and spleen in rats infected with 1 × 105 cfu of Y. pestis CO92 (∼600 MLD). Lungs harvested 60 minutes after infection appeared normal with well-formed alveoli and few inflammatory cells and red blood cells (Figure 3, A and B; see also Supplemental Figure S1, A and E, at http://ajp.amjpathol.org). The bronchiolar epithelia were also normal and none of these cells were vacuolated. As early as 24 hours later, we found lesions throughout the lung, with the most severe concentrated at terminal bronchioles (Figure 3, C and D; and see Supplemental Figure S1, B and F, at http://ajp.amjpathol.org). These lesions harbored increased perivascular inflammatory infiltrate, alveolar macrophages, and multifocal type II pneumocyte hyperplasia. By 48 hours after infection, when greater than 1 × 108 bacteria/g tissue could be recovered in the lung, the pathology in this tissue was severe (Figure 3, E–H; and see Supplemental Figure S1, C and G, and Supplemental Table 1, at http://ajp.amjpathol.org). Marked increases in alveolar hemorrhage, perivascular edema, and inflammation were prevalent throughout the tissue and the animals suffered from diffuse interstitial pneumonia. The bronchiolar epithelium was generally hyperplastic with vacuolated cells consistent with the high degree of inflammation in the tissue. Hemorrhage and polymorphonuclear (PMN) cell infiltration affected both the submucosal and smooth muscle layers surrounding the bronchiole. Some sections harbored areas of liquefactive necrosis with degenerating PMN cells localized to the tissues around the airways. Gram stains of these lesions reveal large populations of bacteria, showing this to be an active area of infection (see Supplemental Figure S1, D and H, at http://ajp.amjpathol.org).
Figure 3.
Lungs from rats infected with Y. pestis CO92 were harvested and perfused with 10% formalin and stained with H&E after 60 minutes (control, A and B), 24 hours (C and D), or 48 hours (E–H) after infection. Boxes in lower magnification images indicate location where the higher magnification images were taken. Original magnifications: ×100 (A, C, E, G); ×400 (B, D, F, H).
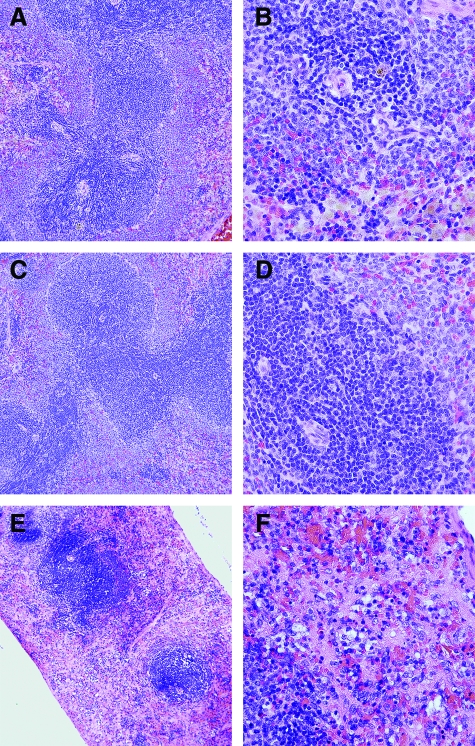
Immune tissue such as the spleen was also targeted by the bacteria during late-stage disease. In spleens harvested at 1 or 24 hours after infection, a time point when bacteria are not expected to have escaped the lung, no pathological lesions were seen (Figure 4, A–D). In striking contrast, at 48 hours after infection, the spleens have a massive bacterial infection that has virtually obliterated red pulp and, in many areas, white pulp as well (Figure 4, E and F). Thus, immune cells of the spleen appear to be undergoing active infection after bacterial dissemination from the lung with significant cell death. These observations are consistent with recent observations in mice that suggest Y. pestis actively targets immune cells during infection.26
Figure 4.
H&E-stained spleens show development of severe pathological lesions affecting primarily red pulp by 48 hours after infection. Spleens were harvested and fixed in 10% formalin after 1 hour (A and B), 24 hours (C and D), or 48 hours (E and F) after infection by Y. pestis CO92. Original magnifications: ×100 (A, C, E); ×400 (B, D, F).
In contrast, the liver was normal and without a significant inflammatory response throughout the infection (see Supplemental Figure S2, A–C, at http://ajp.amjpathol.org). Histochemical staining of the liver at 24 hours after infection showed no lesions and no infiltration of inflammatory cells. This is not surprising, because no bacteria could be recovered from the liver at this time point. However, at 48 hours after infection, where high-bacterial titers were found in the liver, the tissue appears unaffected, with no evidence of inflammation and no evidence of hemorrhage or cell death. Liver sections were Gram-stained to verify that these tissues harbored bacteria, and groups of bacteria could be found within the hepatic sinusoids (see Supplemental Figure S2D, at http://ajp.amjpathol.org). When these liver sections were stained for CD68, only small clusters of macrophages could be identified consistent with the lack of inflammation in the tissue (see Supplemental Figure S2, E and F, at http://ajp.amjpathol.org). Interestingly, some sections of liver harbored cells that stained positive for cleaved caspase-3 suggesting some cells are undergoing apoptosis (see Supplemental Figure S2, G and H, at http://ajp.amjpathol.org), and thus there is in fact infection of the liver. Together these data suggest there is a significant delay in the systemic inflammatory response to Y. pestis infection.
In summary, pathological examination of Brown Norway rats revealed that even though the bacteria have spread systemically, growing to high titers in every tissue examined, the animals suffered from a severe pneumonia, with generalized systemic spread of the infection through the vascular system.
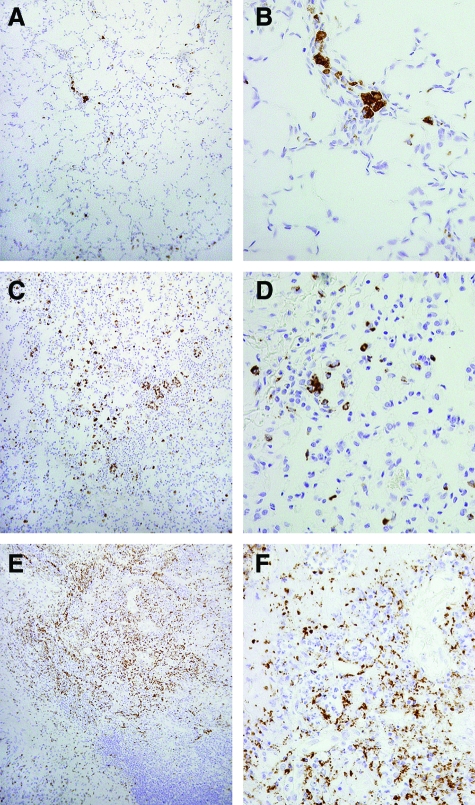
Immunohistochemistry for Plague-Induced Inflammation and Apoptosis in the Lung
We wondered whether macrophages were recruited to the lung where they might contribute to disease pathology. To begin to address this issue, we identified lung macrophages in these animals by immunohistochemical staining with antibody to CD68, a cell-surface marker for macrophages. Increased numbers of lung macrophages stained positive for CD68 as the disease progressed (Figure 5). Mild lesions where some alveolar architecture was intact appeared to harbor increased numbers of macrophages, and this was notable at only 24 hours after infection (Figure 5, A and B). Interestingly, at 48 hours, lung sections with severe cell death and destruction of alveoli stained positive for large numbers of macrophages (Figure 5, E and F), whereas sections with less disease harbored fewer macrophages (Figure 5, C and D). Thus, it appears that pathological lesions may correlate with macrophage recruitment, and future experiments will aim to resolve the contribution of macrophages to the pathology of the lung during pneumonic plague.
Figure 5.
Lung macrophages are recruited to the infection and rapidly killed by Y. pestis. Left lower lobe sections of lungs harvested 1 hour (A and B), 24 hours (C and D), or 48 hours (E and F) after infection were perfused in 10% formalin followed by immunohistochemistry with antibodies to CD68. Images are representative of lesions found in the tissues. Original magnifications: ×100 (A, C, E); ×400 (B, D, F).
We also sought to determine whether we could detect cleavage of caspase-3 in the lung. Cleavage of caspase-3 is an early step in the signaling of apoptosis and therefore indicates the host cell has initiated programmed cell death.52,53 During Y. pestis infections of macrophages in vitro, caspase-3 is cleaved and activated by the injection of YopJ by the type III secretion system and this activity has been proposed as a means to evaluate the potency of antibodies to LcrV generated in response to vaccination.30,33 Indeed, immune responses that result in high titers of antibodies that block activation of caspase-3 in vitro appear to correlate with immunity to pneumonic plague in nonhuman primates.14,20,43 Despite these observations that point to an important contribution of macrophage apoptosis to disease pathology, it is unclear if macrophages indeed initiate apoptosis in vivo and if so, how this contributes to disease. To begin to address these questions, we stained lung sections for cleaved caspase-3, an apoptosis-specific marker (Figure 6, A and E). Concentrations of cleaved caspase-3 staining could be found in lung sections as early as 24 hours after infection in areas that also exhibited pathological lesions (Figure 6, B and F). After 48 hours, staining was particularly intense in areas that were heavily congested and less intense in sections that appeared normal (Figure 6, C, D, G, and H). These results suggest that, similar to macrophage infiltration, activation of caspase-3 may indeed correlate with disease pathology. Thus, Y. pestis infection not only causes tissue necrosis, but the bacteria also activate apoptosis in host cells, suggesting there are multiple mechanisms by which the bacteria destroy host tissue.
Figure 6.
Cleaved caspase-3 is found in infected areas of the lungs suggesting host cells are undergoing apoptosis. Left lower lobe sections of lungs harvested 1 hour (A and E), 24 hours (B and F), or 48 hours (C, D, G, and H) after infection were perfused in 10% formalin followed by immunohistochemistry with antibodies to cleaved caspase-3. C and G: In moderate lesions, caspase-3 staining appears limited to the periphery of the lesion. D and H: More intense staining and higher background were found in congested areas. Images are representative of lesions found in the tissues. Original magnifications: ×100 (A–D); ×400 (E–H).
In summary, Brown Norway rats that have been infected with Y. pestis CO92 through intranasal instillation develop primary pneumonic plague that is characterized by interstitial pneumonia, delayed systemic inflammatory responses, and destruction of immune cells and tissues. The severity of disease in the lung appears to correlate with the recruitment of macrophages and the induction of apoptosis in host cells. Rats suffering from late-stage pneumonic plague develop a systemic infection, with delayed inflammatory response and massive bacteremia. Together, these data are comparable with pathological data collected from human pneumonic plague patients, in which high titers of bacteria grow essentially unimpeded in the lung before systemic spread of the infection.1,2 Patients rapidly succumbed to respiratory distress, often without symptoms of systemic infection. The Brown Norway rat therefore appears to be a suitable model for the study of host-pathogen interactions that lead to acute pulmonary plague.
LcrV Vaccines Protect Brown Norway Rats from Pneumonic Plague
We next sought to evaluate LcrV vaccines in the Brown Norway rat. For this work, we chose to compare two vaccines: wild-type LcrV and a mutant derivative called V10, which lacks amino acid residues 271 to 300 near the C-terminus of LcrV and this deletion cripples LcrV’s immune-suppressive effects without detrimental effects to vaccine efficacy.45,46 Recombinant LcrV and V10 were purified as histidine-tagged proteins from Escherichia coli BL21. Purified protein (50 μg) was emulsified in 25% Alhydrogel and delivered by intramuscular injection into each of 15 female Brown Norway rats. On day 21 after immunization, animals were boosted with an identical immunization. On day 43, five rats in each group were deeply anesthetized and blood was harvested by cardiac puncture for analyses on the immune sera (see below). The remaining rats were moved into the BSL3 facility and challenged with 7500 LD50 of Y. pestis CO92 by intranasal inoculation. At this challenge dose, we had previously observed that LcrV-vaccinated BALB/c mice exhibited breakthrough of immunity, whereas V10-immunized mice were still protected from pneumonic plague.46 In contrast to mice, rats vaccinated with either LcrV or V10 were completely protected from pneumonic plague at this challenge dose whereas all animals in the adjuvant control group succumbed to the infection by day 3 (Table 1). All vaccinated animals showed no signs of disease at any time. Two animals in each vaccination group were necropsied at the end of the 14-day observation period. No viable Y. pestis bacteria could be recovered from the lungs or the spleens of these animals (data not shown). Thus, both LcrV and V10 vaccines resulted in complete clearance of bacteria.
Table 1.
Rats Develop Neutralizing Antibody Titers and Are Protected from Pneumonic Plague by Vaccination with LcrV or V10
| Antigen | Survival* | IgG1† | IgG2a† | 400 μg IgG‡
|
200 μg IgG‡
|
100 μg IgG‡
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Survival | MTTD§ | MPI¶ | Survival | MTTD§ | MPI¶ | Survival | MTTD§ | MPI¶ | ||||
| Alhydrogel | 0/10 | NT | NT | 0/10 | 5.1 ± 0.5 | NT | 0/10 | 5.1 ± 0.5 | NT | 0/10 | 5.1 ± 0.5 | NT |
| LcrV | 10/10 | 37,500 | 37,500 | 2/10 | 11.1 ± 3.2 | 0.4 | 1/10 | 8 ± 1.9 | 0.7 | 0/10 | 6.2 ± 1.2 | 0.9 |
| V10 | 10/10 | 37,500 | 7500 | 7/10 | 11.7 ± 1.0 | 0.1 | 0/10 | 9 ± 2.3 | 0.6 | 0/10 | 6.7 ± 1.2 | 0.8 |
Survival against intranasal challenge with 7500 MLD Yersinia pestis CO92 (1 × 107 cfu). Two independent vaccination and challenge experiments were performed. Results shown are from a representative experiment.
Antibody titer to LcrV as determined by ELISA.
Rat LcrV or V10 antibody dose delivered for passive transfer of immunity to bubonic plague in BALB/c mouse model.
MTTD: Mean time to death; unpaired Student’s t-test gave P < 0.04 for the 400-μg dose, P < 0.05 for the 200-μg dose, and P = 0.2 for the 100-μg dose.
MPI: Mouse protection index.
LcrV and V10 Immune Sera Neutralize Y. pestis Infections
Previous studies on plague vaccines indicated that the concentration of neutralizing antibodies correlated with protection. To determine whether this is true in the Brown Norway rat, we tested LcrV and V10 immune sera in a passive transfer experiment. Briefly, serum from five animals per group was collected by cardiac puncture on day 43 after immunization and pooled. Antigen-specific immunoglobulin titers were determined by ELISA (Table 1). Interestingly, although the overall titers were similar, LcrV vaccination resulted in a higher titer of IgG2a antibodies, giving an IgG1:IgG2a ratio of 1:1. In contrast, V10 vaccination resulted in predominantly IgG1 antibodies, with a resulting IgG1:IgG2a ratio of 5:1. These data suggest that LcrV immunization elicits a greater Th1 response than the V10 vaccine, which results in a predominant Th2 response. LcrV-specific IgA, IgE, and IgM antibodies were not detectable in any of the sera (data not shown).
We tested the biological activity of V and V10 antibodies in a passive transfer experiment. IgG was purified from pooled V or V10 immune serum and quantified. Decreasing doses (400 μg, 200 μg, and 100 μg) of purified IgG were injected intraperitoneally into each of 10 BALB/c mice. As a control, 400 μl of PBS was injected intraperitoneally into each of 10 mice. After 60 minutes, these mice were challenged by subcutaneous injection of 20 MLD of Y. pestis CO92. Survival and time to death were monitored for 14 days and used to calculate the MPI. In this biological assay, both vaccines result in the generation of neutralizing antibodies in the Brown Norway rat because a MPI of 0.4 or 0.2 was observed after administration of a single 400-μg dose of LcrV IgG or V10 IgG, respectively (Table 1). Interestingly these data suggest that V10 antibodies may be more potent than V, as lower MPI values for both 400-μg and 200-μg doses of V10 IgG were observed as compared with LcrV IgG. We used an unpaired Student’s t-test to evaluate the statistical significance of the time to death used to calculate the MPI. This analysis resulted in P < 0.04 for both the 400-μg and 200-μg dose groups, indicating these differences are statistically significant.
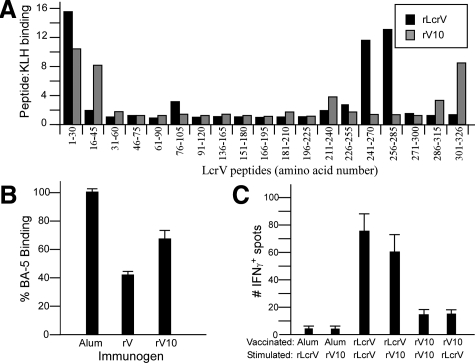
In an effort to identify potential LcrV epitopes that were bound by these antibodies, we mapped the immune sera for recognition of peptide epitopes of LcrV. In this qualitative assay, 30 amino acid peptides, spanning the entire length of LcrV in overlapping series, were individually conjugated to keyhole-limpet hemocyanin. We used these peptides or keyhole-limpet hemocyanin alone as a control, to coat 96-well plates followed by probing with LcrV or V10 rat immune sera. Binding was detected using a secondary rat IgG antibody conjugated to HRP, followed by detection at 450 nm. Somewhat to our surprise, the linear epitope-binding profile was markedly different between LcrV and V10 immune sera (Figure 7A). Dominant epitopes in LcrV immune sera were amino acids 1 to 30, 76 to 105, and 241 to 285. In contrast, V10 sera recognized dominant epitopes at amino acids 1 to 45, 211 to 240, and 301 to 326. These data suggest multiple neutralizing epitopes may exist on LcrV, and each vaccine may target different regions on bacterially located LcrV.
Figure 7.
Humoral and cell-mediated immune responses to V and V10 in Brown Norway rat reveals complexity in antibody-mediated neutralization of plague. A: LcrV peptide epitope mapping of V and V10 immune sera shows different epitope binding profiles elicited by the two antigens. B: Competition for binding LcrV between neutralizing LcrV monoclonal antibody BA-5 and V or V10 rat immune sera. C: Memory T-cell assay in splenocytes purified from rats immunized with V or V10 shows greater IFN-γ production in V-immunized rats compared with V10-immunized rats.
To further investigate this possibility, we performed a competitive ELISA that measures competition of the immune sera with a neutralizing monoclonal antibody to LcrV.41 This assay can be used to determine relative levels of antibodies to a specific neutralizing epitope on LcrV. We recently developed a monoclonal antibody to LcrV called BA-5 that neutralizes Y. pestis bubonic plague infections in mice with a corresponding MPI at 100-μg antibody of 0.2 (data not shown). mAb BA-5 is allowed to bind LcrV and the complex is incubated with immune sera. If the serum contains antibodies that bind the same epitope as BA-5, it will compete with the mAb for binding, and less antigen-bound mAb will be detected. Detection with a secondary anti-mouse IgG antibody that does not cross-react with rat IgG can then be used to determine relative levels of BA-5-specific antibodies in the rat serum. When adjuvant serum was used as a competitor, 100% binding of mAb BA-5 to LcrV was observed (Figure 7B). In contrast, both LcrV and V10 rat sera competed with mAb BA-5 for binding to LcrV because only 44% and 68% BA-5 binding was observed in the presence of V or V10 serum, respectively. LcrV sera showed greater competition with mAb BA-5 for binding LcrV, suggesting it may harbor greater amounts of antibodies with the same specificity as BA-5. Together with the peptide mapping data, these data support the notion that multiple protective epitopes exist in LcrV and that LcrV and V10 antibodies may have different mechanisms of binding and neutralization of antigen. Moreover, assays that measure immune serum competition for LcrV binding with a single neutralizing monoclonal antibody do not directly correlate with immunity in the Brown Norway pneumonic plague vaccine model.
LcrV and V10 Vaccines Induce Robust Memory T-Cell Responses
We also characterized the memory T-cell response to LcrV vaccines in the Brown Norway rat. To this end, we vaccinated groups of two Brown Norway rats with LcrV, V10, or Alhydrogel by intramuscular injection on days 0 and 21 as described above. On day 28, rats were humanely culled and the spleens removed. Splenocytes were then incubated with LcrV or V10 for 18 hours and IFN-γ production was measured by ELISpot. Both LcrV- and V10-vaccinated rats harbored IFN-γ-producing cells in their spleens, although it appears that LcrV vaccination resulted in greater numbers of splenocytes activated for IFN-γ production (Figure 7C). These data suggest that LcrV may be better than V10 in inducing a Th1 response, consistent with the presence of higher titers of IgG2a antibodies in V sera. The relevance of this observation to plague immunity by LcrV vaccines is not yet clear, but these data suggest that IFN-γ producing T cells may not directly correlate with immunity. Nevertheless, the contributions of cell-mediated immune responses to protection from pneumonic plague is likely significant.
Discussion
Plague vaccines in the United States will be subjected to the Food and Drug Administration’s Animal Rule for Licensure as it applies to efficacy testing because human clinical trials that measure efficacy against pneumonic plague are not feasible. To be licensed via the Animal Rule, plague vaccines will likely be required to be tested in two well-characterized animal models that closely resemble human disease (http://www.fda.gov/cber/minutes/plague101304t.htm, last accessed January 15, 2009). In this study, we developed a rat model of pneumonic plague and used it to evaluate LcrV-based plague vaccines to test its utility for the Animal Rule. This model may be preferable to the mouse model for some applications because rats are relatively inexpensive, their larger size facilitates both pathological and immunological evaluation, and this animal was most commonly associated with plague outbreaks in humans.
In the Brown Norway rat, Y. pestis establishes a rapid and lethal pneumonia, characterized by the development of severe hemorrhage and edema, as well as massive tissue destruction in the lung. This pathology accompanies macrophage recruitment, but rather than engulfing the bacteria, these macrophages are ineffective and instead the bacteria trigger apoptotic signaling in these cells. Systemic disease develops late, and is characterized by extensive necrosis in the lung, accompanied by only a small inflammatory response in distal tissues. These observations suggest the animals succumb to pulmonary failure, and not septicemia. Pathological examinations of human pneumonic plague reveal a similar role for lung involvement in the severity of the disease. Bacteria replicate to massive numbers, progressing essentially unimpeded in the lung, such that by the time the disease spreads systemically, the bacterial numbers overwhelm the host and death follows soon after.1,2 Thus the disease progression we observed in the Brown Norway rat model is very similar human pneumonic plague, supporting our use of this model for evaluation of a vaccine to be used in humans.
Vaccination with LcrV or its mutant derivative V10 prevented these lesions and resulted in complete clearance of bacteria even after high-challenge doses. Immunity correlated with IgG antibodies specific for LcrV that carried biological activity in neutralizing Y. pestis. Antibody analyses suggested multiple avenues for active antibodies to neutralize LcrV function, an observation made by other groups in both mouse and nonhuman primate pneumonic plague models. For example, F1-V and F1+V vaccines have been shown to give rise to neutralizing antibodies in mice and nonhuman primates, and these antibodies inhibit macrophage apoptosis in vitro. This activity was also strongly manifested by neutralizing LcrV mAb 7.3, and not nonneutralizing mAbs, but nevertheless competitive ELISA against mAb 7.3 did not correlate with immunity.14,20 For this reason, these investigators have discarded ELISA-based methods that measure antibody specificity and concentration as inappropriate immune correlates and instead rely on biological assays that measure inhibition of LcrV function to predict immunity. Unfortunately, infection assays are technically difficult and require the use of live Y. pestis bacteria, thus making them impractical for high throughput use. Our data suggest that future development of ELISA-based methods for predicting efficacy and potency of LcrV vaccines may be possible if they use multiple neutralizing monoclonal antibodies that bind to distinct epitopes on LcrV. This possibility is currently being pursued in our laboratory.
Surprisingly, two very similar antigens produced markedly different immune responses in rats. LcrV, which is known to modulate cytokine production in mouse and human phagocytic cells through the induction of interleukin-10, activates both Th1 and Th2 responses in rats. This contrasts with observations in mice, in which LcrV is thought to activate a dominant Th2 response. On the other hand, V10, which lacks only 30 amino acids present in LcrV, activates a weak Th1 response and produces antibodies that recognize epitopes that are not observed in LcrV sera. Are some immunoglobulin isotypes more effective in bacterial clearance in pneumonic plague models? Are certain neutralizing epitopes on LcrV more potent than others? The answers to these questions are necessary not only for the development of in vitro correlates of protection, but will also permit further improvements to vaccines and therapeutics that target LcrV.
Supplementary Material
Acknowledgments
We thank Cindy Besch-Wiliford and Jeff Mitchell for assistance with the pathological analysis; Paul Anderson and Will DePaolo for helpful discussions and critical comments on the manuscript; the Fitch Monoclonal Antibody Facility at the University of Chicago for cloning and producing the monoclonal antibody BA-5; the University of Chicago Pathology Core Facility for sectioning and H&E staining of lung tissues; and the Research Animal Diagnostic Laboratory at the University of Missouri for performing immunohistochemistry.
Footnotes
Address reprint requests to Deborah Anderson, Department of Veterinary Pathobiology, University of Missouri, 302 Connaway Hall, 1600 E. Rollins St., Columbia, MO 65211. E-mail: andersondeb@missouri.edu.
Supported by the National Institutes of Health/National Institute of Allergy and Infectious Diseases (Great Lakes Regional Center of Excellence for Biodefense and Emerging Infectious Diseases grant U54 AI0157153 and Challenge grant U01 AI070559 to O.S.) and the Comparative Medicine Program (training grant T32 RR007004 to H.L.).
Supplemental material for this article can be found on http://ajp.amjpathol.org.
Current addresses of K.L.D.: National Institute of Allergy and Infectious Disease, Bethesda, MD; and K.A.O: Lovelace Respiratory Research Institute, Albuquerque, NM.
References
- Lien-Teh W. Geneva: League of Nations Health Organization,; A Treatise on Pneumonic Plague. 1926 [Google Scholar]
- Pollitzer R. Geneva: World Health Organization,; Plague. 1954 [Google Scholar]
- Petrie G, Todd R, Skander R, Hilmy F. A report on the plague investigations in Egypt. J Hygiene. 1924;23:117–150. doi: 10.1017/s0022172400008548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teh W, Han C, Pollitzer R. Plague in Manchuria. J Hygiene. 1923;21:307–358. doi: 10.1017/s0022172400031521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage K, Kosoy M. Natural history of plague: perspectives from more than a century of research. Annu Rev Entomol. 2005;50:505–528. doi: 10.1146/annurev.ento.50.071803.130337. [DOI] [PubMed] [Google Scholar]
- Galimand M, Guiyoule A, Gerbaud G, Rasoamanana B, Chanteau S, Carniel E, Courvalin P. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. New Engl J Med. 1997;337:677–680. doi: 10.1056/NEJM199709043371004. [DOI] [PubMed] [Google Scholar]
- Guiyoule A, Gerbaud G, Buchrieser C, Galimand M, Rahalison L, Chanteau S, Courvalin P, Carniel E. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg Infect Dis. 2001;7:43–48. doi: 10.3201/eid0701.010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinnebusch B, Rosso M, Schwan T, Carniel E. High-frequency conjugative transfer of antibiotic resistance genes to Yersinia pestis in the flea midgut. Mol Microbiol. 2002;46:349–354. doi: 10.1046/j.1365-2958.2002.03159.x. [DOI] [PubMed] [Google Scholar]
- Welch T, Fricke W, McDermott P, White D, Rosso M, Rasko D, Mammel M, Eppinger M, Rosovitz M, Wagner D, Rahalison L, LeClerc J, Hinshaw J, Lindler L, Cebula T, Carniel E, Ravel J. Multiple antimicrobial resistance in plague: an emerging public health risk. PLoS One. 2007;2:e309. doi: 10.1371/journal.pone.0000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell P, Eley S, Hibbs S, Manchee R, Stagg A, Titball R. A comparison of plague vaccine, USP and EV76 vaccine induced protection against Yersinia pestis in a murine model. Vaccine. 1995;13:1551–1556. doi: 10.1016/0264-410x(95)00090-n. [DOI] [PubMed] [Google Scholar]
- Anisimov A, Lindler L, Pier G. Intraspecific diversity of Yersinia pestis. Clin Microbiol Rev. 2004;17:434–464. doi: 10.1128/CMR.17.2.434-464.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Efraim S, Aronson M, Bichowsky-Slomnicki L. New antigenic component of Pasteurella pestis formed under specific conditions. J Bacteriol. 1961;81:704–714. doi: 10.1128/jb.81.5.704-714.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y, Rosqvist R, Forsberg A. Role of fraction 1 antigen of Yersinia pestis in inhibition of phagocytosis. Infect Immun. 2002;70:1453–1460. doi: 10.1128/IAI.70.3.1453-1460.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks S, Hill J, Friedlander A, Welkos S. Anti-V antigen antibody protects macrophages from Yersinia pestis-induced cell death and promotes phagocytosis. Microb Pathog. 2002;32:227–237. doi: 10.1006/mpat.2002.0498. [DOI] [PubMed] [Google Scholar]
- Meyer K. Effectiveness of live or killed plague vaccines in man. Bull World Health Organ. 1970;42:653–666. [PMC free article] [PubMed] [Google Scholar]
- Quenee L, Cornelius C, Ciletti N, Elli D, Schneewind O. Yersinia pestis caf1 variants and the limits of plague vaccine protection. Infect Immun. 2008;76:2025–2036. doi: 10.1128/IAI.00105-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson W, Thomas R, Schwan T. Recombinant capsular antigen (fraction 1) from Yersinia pestis induces a protective antibody response in BALB/c mice. Am J Trop Med Hyg. 1990;43:389–396. doi: 10.4269/ajtmh.1990.43.389. [DOI] [PubMed] [Google Scholar]
- Heath D, Anderson G, Mauro M, Welkos S, Andrews G, Adamovicz J, Friedlander A. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998;16:1131–1137. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- Andrews G, Heath D, Anderson G, Welkos S, Friedlander A. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect Immun. 1996;64:2180–2187. doi: 10.1128/iai.64.6.2180-2187.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashaw J, Norris S, Weeks S, Trevino S, Adamovicz J, Welkos S. Development of in vitro correlate assays of immunity to infection with Yersinia pestis. Clin Vaccine Immunol. 2007;14:605–616. doi: 10.1128/CVI.00398-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter C, Cherry W, Moody M. An unusual strain of Pasteurella pestis isolated from a fatal human case of plague. Bull World Health Organ. 1960;23:408–409. [PMC free article] [PubMed] [Google Scholar]
- Friedlander A, Welkos S, Worsham P, Andrews G, Heath D, Anderson G, Pitt M, Estep J, Davis K. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin Infect Dis. 1995;21:S178–S181. doi: 10.1093/clinids/21.supplement_2.s178. [DOI] [PubMed] [Google Scholar]
- Davis K, Fritz D, Pitt M, Welkos S, Worsham P, Friedlander A. Pathology of experimental pneumonic plague produced by fraction 1-positive and fraction 1-negative Yersinia pestis in African green monkeys (Cercopithecus aethiops). Arch Pathol Lab Med. 1996;120:156–163. [PubMed] [Google Scholar]
- Burrows T. An antigen determining virulence in Pasteurella pestis. Nature. 1956;177:426–427. doi: 10.1038/177426b0. [DOI] [PubMed] [Google Scholar]
- Skrzypek E, Straley S. Differential effects of deletions in lcrV on secretion of V antigen, regulation of the low-Ca2+ response, and virulence of Yersinia pestis. J Bacteriol. 1995;177:2530–2542. doi: 10.1128/jb.177.9.2530-2542.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marketon M, DePaolo R, DeBord K, Jabri B, Schneewind O. Plague bacteria target immune cells during infection. Science. 2005;309:1739–1741. doi: 10.1126/science.1114580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller C, Broz P, Muller S, Ringler P, Erne-Brand F, Sorg I, Kuhn M, Engel A, Cornelis G. The V-antigen of Yersinia forms a distinct structure at the tip of the injectisome needle. Science. 2005;310:674–676. doi: 10.1126/science.1118476. [DOI] [PubMed] [Google Scholar]
- Goure J, Broz P, Attree O, Cornelis G, Attree I. Protective anti-V antibodies inhibit Pseudomonas and Yersinia translocon assembly within host membranes. J Infect Dis. 2005;192:218–225. doi: 10.1086/430932. [DOI] [PubMed] [Google Scholar]
- Andersson K, Carballeira N, Magnussen K, Persson C, Stendahl O, Wolf-Watz H, Fallman M. YopH of Yersinia pseudotuberculosis interrupts early phosphotyrosine signalling associated with phagocytosis. Mol Microbiol. 1996;20:1057–1069. doi: 10.1111/j.1365-2958.1996.tb02546.x. [DOI] [PubMed] [Google Scholar]
- Monack D, Mecsas J, Ghori N, Falkow S. Yersinia signals macrophages to undergo apoptosis and YopJ is necessary for this cell death. Proc Natl Acad Sci USA. 1997;94:10385–10390. doi: 10.1073/pnas.94.19.10385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeth J, Straley S. Effect of Yersinia pestis YopM on experimental plague. Infect Immun. 1997;65:924–930. doi: 10.1128/iai.65.3.924-930.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Pawel-Rammingen U, Telepnev M, Schmidt G, Aktories K, Wolf-Watz H, Rosqvist R. GAP activity of the Yersinia YopE cytotoxin specifically targets the Rho pathway: a mechanism for disruption of actin microfilament structure. Mol Microbiol. 2000;36:737–748. doi: 10.1046/j.1365-2958.2000.01898.x. [DOI] [PubMed] [Google Scholar]
- Lemaitre N, Sebbane F, Long D, Hinnebusch B. Yersinia pestis YopJ suppresses tumor necrosis factor alpha induction and contributes to apoptosis of immune cells in the lymph node but is not required for virulence in a rat model of bubonic plague. Infect Immun. 2006;74:5126–5131. doi: 10.1128/IAI.00219-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adkins I, Koberle M, Grobner S, Bohn E, Autenrieth I, Borgmann S. Yersinia outer proteins E, H, P, and T differentially target the cytoskeleton and inhibit phagocytic capacity of dendritic cells. Int J Med Microbiol. 2007;297:235–244. doi: 10.1016/j.ijmm.2007.02.005. [DOI] [PubMed] [Google Scholar]
- Philipovskiy A, Cowan C, Wulff-Strobel C, Burnett S, Kerschen E, Cohen D, Kaplan A, Straley S. Antibody against V antigen prevents Yop-dependent growth of Yersinia pestis. Infect Immun. 2005;73:1532–1542. doi: 10.1128/IAI.73.3.1532-1542.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reithmeier-Rost D, Hill J, Elvin S, Williamson E, Dittmann S, Schmidt A, Wilharm G, Sing A. The weak interaction of LcrV and TLR2 does not contribute to the virulence of Yersinia pestis. Microbes Infect. 2007;9:997–1002. doi: 10.1016/j.micinf.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Nakajima R, Motin V, Brubaker R. Suppression of cytokines in mice by protein A-V antigen fusion peptide and restoration of synthesis by active immunization. Infect Immun. 1995;63:3021–3029. doi: 10.1128/iai.63.8.3021-3029.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foligne B, Dessein R, Marceau M, Poiret S, Chamaillard M, Pot B, Simonet M, Daniel C. Prevention and treatment of colitis with Lactococcus lactis secreting the immunomodulatory Yersinia LcrV protein. Gastroenterology. 2007;133:862–874. doi: 10.1053/j.gastro.2007.06.018. [DOI] [PubMed] [Google Scholar]
- Williamson E, Eley S, Stagg A, Green M, Russell P, Titball R. A single dose sub-unit vaccine protects against pneumonic plague. Vaccine. 2001;19:566–571. doi: 10.1016/s0264-410x(00)00159-6. [DOI] [PubMed] [Google Scholar]
- Williamson E, Eley S, Griffin K, Green M, Russell P, Leary S, Oyston P, Easterbrook T, Reddin K, Robinson A, Titball R. A new improved sub-unit vaccine for plague: the basis for protection. FEMS Immunol Med Microbiol. 1995;12:223–230. doi: 10.1111/j.1574-695X.1995.tb00196.x. [DOI] [PubMed] [Google Scholar]
- Williamson E, Flick-Smith H, LeButt C, Rowland C, Jones S, Waters E, Gwyther R, Miller J, Packer P, Irving M. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect Immun. 2005;73:3598–3608. doi: 10.1128/IAI.73.6.3598-3608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson E, Vesey P, Gillhespy K, Eley S, Green M, Titball R. An IgG1 titre to the F1 and V antigens correlates with protection against plague in the mouse model. Clin Exp Immunol. 1999;116:107–114. doi: 10.1046/j.1365-2249.1999.00859.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welkos S, Norris S, Adamovicz J. Modified caspase-3 assay indicates correlation of caspase-3 activity with immunity of nonhuman primates to Yersinia pestis infection. Clin Vaccine Immunol. 2008;15:1134–1137. doi: 10.1128/CVI.00091-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson E, Flick-Smith H, Waters E, Miller J, Hodgson I, LeButt C, Hill J. Immunogenicity of the rF1+rV vaccine for plague with identification of potential immune correlates. Microb Pathog. 2007;42:11–21. doi: 10.1016/j.micpath.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Overheim K, DePaolo R, DeBord K, Morrin E, Anderson D, Green N, Brubaker R, Jabri B, Schneewind O. LcrV plague vaccine with altered immunomodulatory properties. Infect Immun. 2005;73:5152–5159. doi: 10.1128/IAI.73.8.5152-5159.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBord K, Anderson D, Marketon M, Overheim K, DePaolo R, Ciletti N, Jabri B, Schneewind O. Immunogenicity and protective immunity against bubonic plague and pneumonic plague by immunization of mice with the recombinant V10 antigen, a variant of LcrV. Infect Immun. 2006;74:4910–4914. doi: 10.1128/IAI.01860-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebbane F, Gardner D, Long D, Gowen B, Hinnebusch B. Kinetics of disease progression and host response in a rat model of bubonic plague. Am J Pathol. 2005;166:1427–1439. doi: 10.1016/S0002-9440(10)62360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surgalla M, Beesley E. Congo red-agar plating medium for detecting pigmentation in Pasteurella pestis. Appl Microbiol. 1969;18:834–837. doi: 10.1128/am.18.5.834-837.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetherston J, Schuetze P, Perry R. Loss of the pigmentation phenotype in Yersinia pestis is due to the spontaneous deletion of 102kb of chromosomal DNA which is flanked by a repetitive element. Mol Microbiol. 1992;6:2693–2704. doi: 10.1111/j.1365-2958.1992.tb01446.x. [DOI] [PubMed] [Google Scholar]
- Reed L, Muench H. A simple method of estimating fifty percent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- Eyles J, Elvin S, Westwood A, LeButt C, Alpar H, Somavarapu S, Williamson E. Immunisation against plague by transcutaneous and intradermal application of subunit antigens. Vaccine. 2004;22:4365–4373. doi: 10.1016/j.vaccine.2004.02.049. [DOI] [PubMed] [Google Scholar]
- Jyonouchi H. Airway epithelium and apoptosis. Apoptosis. 1999;4:407–417. doi: 10.1023/a:1009607607603. [DOI] [PubMed] [Google Scholar]
- Labbé K, Saleh M. Cell death in the host response to infection. Cell Death Differ. 2008;15:1339–1349. doi: 10.1038/cdd.2008.91. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.