Abstract
OBJECTIVE: To institute a patient navigator program for underinsured women to eliminate delays in diagnostic resolution of abnormal screening mammograms, provide services for abnormalities noted during breast cancer screening, describe demographic and clinical characteristics of enrollees, and assess postscreening follow-up care.
PATIENTS AND METHODS: Coordinators from area health departments worked with a navigator nurse at Mayo Clinic Cancer Center in Jacksonville, FL, to refer patients for additional diagnostic services, including diagnostic mammography, ultrasonography, ultrasonography-guided biopsy, stereotactic biopsy, breast magnetic resonance imaging, and biopsy guided by magnetic resonance imaging. Women with abnormal screening mammograms (Breast Imaging Reporting and Data System [BI-RADS] category 4 or 5) or palpable suspect breast masses were eligible. Data were extracted from clinical service records. Timeliness of postscreening follow-up was assessed.
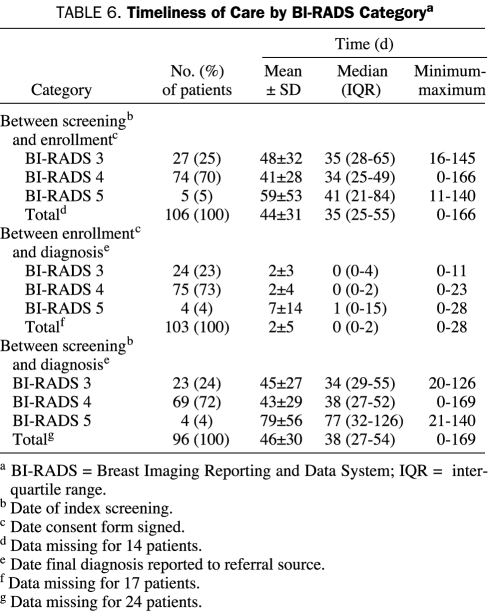
RESULTS: The study enrolled 447 women from June 30, 2000, to December 29, 2006. Data on the time from screening to diagnosis were available for 399 women, and median time from detection of screening abnormality to diagnosis was 37 days. Time between screening and diagnosis was 60 days or less for 325 (81%) of the 399 women for whom data were available and for 60 (82%) of the 73 women with BI-RADS category 4 or 5 assessments. Both of these percentages exceeded the Centers for Disease Control and Prevention quality benchmark of 75%. Mean time from study enrollment to diagnosis was 2 days for women with BI-RADS category 3 or 4 assessments and 7 days for women with BI-RADS category 5 assessments.
CONCLUSION: This program demonstrated a successful collaboration between an academic medical center and community health centers. Most women with BI-RADS category 4 or 5 assessments received a diagnosis within 60 days of screening.
A collaboration between an academic medical center and community health centers was found to be successful; most women with Breast Imaging Reporting and Data System category 4 or 5 assessments received a diagnosis within 60 days of screening.
BI-RADS = Breast Imaging Reporting and Data System; CDC = Centers for Disease Control and Prevention; DCIS = ductal carcinoma in situ; NBCCEDP = National Breast and Cervical Cancer Early Detection Program
In 2006, 47 million people in the United States (15.8% of the total population) had no health insurance, and the number of the uninsured has continued to increase.1 When the underinsured are also considered, the true scope of the problem begins to emerge. For women with breast cancer, a lack of or inadequate insurance is associated with shorter overall survival.2,3 Many factors contribute to the survival disadvantage of underinsured women with breast cancer. In addition to lack of access to new treatments, these factors include less frequent screening,4 more advanced stage at diagnosis,2,5 and inadequate patient follow-up.6 Complications in the health care system contribute to delays for the underinsured because these patients have less access to services at health care facilities and fewer prompt appointments.7,8 They are also less likely to have access to a consistent primary care physician.3 Compared with whites, racial and ethnic minorities are more likely to be uninsured. In addition, according to the 2004 position paper of the American College of Physicians on health care disparities, racial and ethnic minorities have less access to and lower quality of health care than nonminorities, even after adjustment for insurance status and income.9
Several programs provide breast cancer screening for financially disadvantaged, medically uninsured women nationwide; however, there is no unified system to provide diagnostic services when breast abnormalities are detected through these screening programs. Therefore, for uninsured women, a free screening mammogram that shows an abnormality may lead to weeks or even months of waiting before a diagnosis can be made. The “system delay” between screening and diagnosis may also negatively affect prognosis.10,11 Considering that 80% of breast biopsies yield benign results,12 minimally invasive diagnostic procedures can potentially spare a large number of women surgical procedures and their associated costs (eg, actual charges, effect on quality of life, and lost income due to time away from work).
Patient navigator programs have been implemented to specifically address barriers to cancer care.13-15 Patient navigation is a method for improving access to health care systems for medically underserved populations whereby trained individuals proactively guide patients through and around barriers in the complex cancer care system to decrease fragmentation of care and to coordinate services.16 Ongoing improvements in the time from breast cancer screening to diagnosis have been reported with continued support from patient navigator programs.17,18 Nonetheless, further study is needed to more fully understand the role of patient navigators and to determine how best to use them in other medically underserved populations to improve time from screening to diagnosis.
The Mayo Clinic Cancer Center in Jacksonville, FL, instituted a patient navigator program to begin addressing the gap in health care for medically underserved women with abnormal breast screening evaluations in its surrounding community. This report describes the demographic and clinical characteristics of enrollees in the program and assesses its effect on the timeliness of postscreening follow-up care and clinical services provided to enrollees.
PATIENTS AND METHODS
Program Description
Beginning in 2000, Mayo Clinic's site in Jacksonville, FL, instituted a comprehensive diagnostic study for the medically underserved women from 4 neighboring county health departments and 2 local Jacksonville, FL, clinics. The Mayo Clinic Institutional Review Board approved this study (IRB No. 378-00), and patients gave written informed consent. The data reported here are from women who were enrolled in the study from June 30, 2000, to December 29, 2006. Women were referred from facilities where they had completed breast screening examinations with or without a mammogram. Those with abnormal results were provided with a timely diagnosis and any needed diagnostic services. The program used a nurse as a patient navigator, and its objective was to ensure timely diagnosis of breast cancer after an initial mammographic screening abnormality.
Role and Responsibilities of Navigator
The nurse selected as patient navigator was required to have the following competencies: understanding of the educational, financial, and cultural barriers to health care; effective communication skills with patients, families, and health care professionals; good organizational and problem-solving skills; resourcefulness and ability to help patients find resources; and compassion when working with patients from different socioeconomic levels.
The nurse navigator participated in ongoing training at Mayo Clinic's site in Jacksonville, FL, which included training in clinical research, case management, health disparities, and cultural diversity. The navigator also participated actively on the Diversity Committee, which has the charge and goal of creating a caring service environment within the institution, one that ensures that individual differences of the personnel and patients are valued. In addition, Mayo Clinic's site in Jacksonville, FL, uses training provided by the Health Resources and Services Administration, an agency of the US Department of Health and Human Services and the primary federal agency for improving access to health care services for people who are uninsured, isolated, or medically vulnerable.
The nurse navigator was responsible for confirming patient eligibility criteria, which included income at or below 200% of the federal poverty level, breast abnormality on a screening mammogram, and ability to give informed consent. In addition, the nurse navigator identified patient and facility system barriers or possible barriers to care and facilitated solutions. If language was a barrier, the nurse navigator collaborated with the site's International Services division to provide non-English-speaking patients with an interpreter for guidance throughout their visit. The nurse navigator was also responsible for guiding referred patients through the clinic's system and ensuring that patients received a timely diagnosis. Other responsibilities included contacting patients to remind them of appointments, documenting missed appointments, and streamlining and assisting with appointments and necessary paperwork. Consideration was given to assessing and implementing needed changes to system barriers while keeping communication open with health care professionals, caregivers, and patients to coordinate services within the clinic, at outside facilities, and within the community along the continuum of patient care. This allowed for linkage of patients, caregivers, and families with needed national and community resources.
Patient Assessments
Demographic information was initially collected from the referring county health department or agency for each patient and was confirmed during the initial patient interview at Mayo Clinic's site in Jacksonville, FL. Information collected comprised age at time of study enrollment, income, ZIP code, and patient-reported race or ethnicity.
On the basis of the reported examination by the referring physician and radiographic findings, 1 or more of the following diagnostic studies were performed: diagnostic mammography, ultrasonography, ultrasonography-guided biopsy, stereotactic biopsy, breast magnetic resonance imaging, or magnetic resonance imaging-guided biopsy. When possible, the necessary procedure or procedures were completed during the initial visit. A follow-up visit with the physician was arranged for the patient after diagnostic services were completed; any biopsy results and further management options were discussed at that visit.
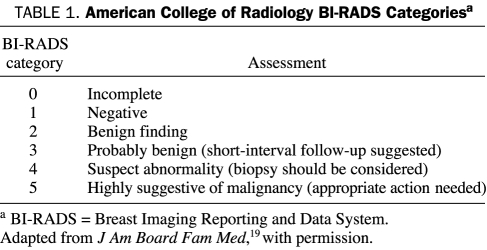
The American College of Radiology's Breast Imaging Reporting and Data System (BI-RADS) was used to provide a standard classification for mammographic studies, with BI-RADS 0, 3, 4, or 5 (Table 1) considered for evaluation.19 Procedures and dates performed were recorded. Diagnosis categories were defined by the investigators as benign, high-risk (surgical consultation advised), ductal carcinoma in situ (DCIS) (surgical and oncology consultations advised), and invasive carcinoma (surgical and oncology consultations advised). Appointment information and procedures were recorded, including referral date (date when referral was received), enrollment date (date when consent form was signed), appointment date, diagnosis date (date when diagnosis report was sent to referral source), and date of screening mammography. Information on additional procedures and dates was recorded in the comments section of the data collenction tool.
TABLE 1.
American College of Radiology BI-RADS Categoriesa
Statistical Analyses
Descriptive statistics were reported for patient demographics and clinical characteristics. The Statistical Package for the Social Sciences, version 14.0 (SPSS, Chicago, IL), was used for statistical analyses.
RESULTS
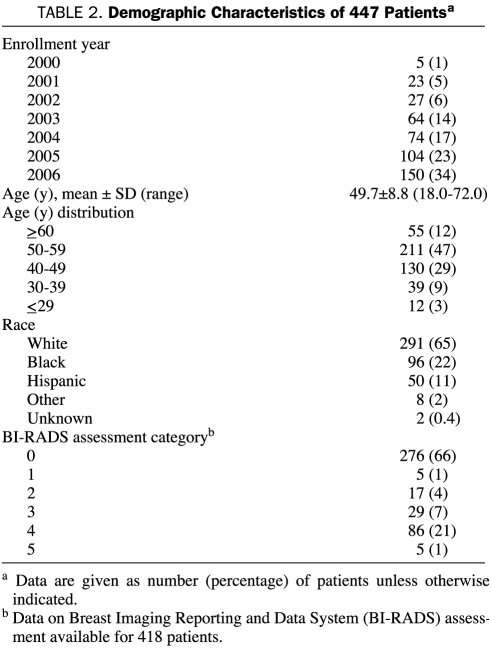
Demographic information for the 447 patients is presented in Table 2. The mean ± SD age was 49.7±8.8 years. The racial distribution of the sample correlates with the overall racial makeup for Jacksonville, FL, based on 2005 census data.20
TABLE 2.
Demographic Characteristics of 447 Patientsa
Diagnoses and Procedures
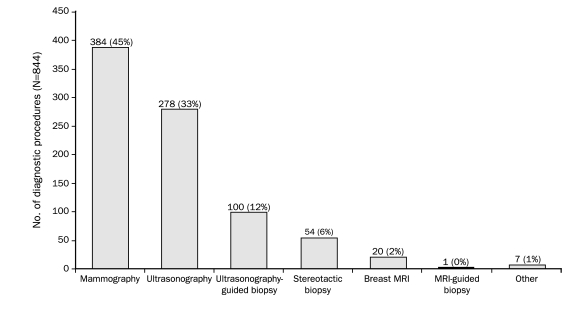
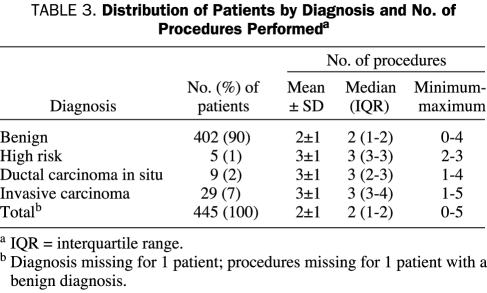
Patient distribution by diagnostic procedures is presented in the Figure. Of the 844 procedures performed, 384 (45%) were mammographies. Of 447 women, 403 (90%) had a benign diagnosis, 29 (6%) had invasive carcinoma, 9 (2%) had DCIS, and 5 (1%) were deemed at high risk. The sample distribution by diagnosis and number of procedures performed is presented in Table 3. As expected, patients with invasive carcinoma had the highest mean ± SD number of procedures (3±1).
FIGURE 1.
Distribution of study patients by diagnostic procedures. MRI = magnetic resonance imaging.
TABLE 3.
Distribution of Patients by Diagnosis and No. of Procedures Performeda
Timeliness of Care
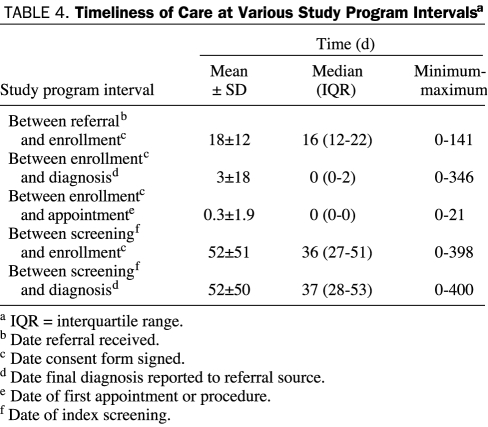
The timeliness of care is illustrated in Table 4. The median time from study enrollment to diagnosis was 0 days (ie, most patients received a diagnosis the same day they were enrolled). This was possible because 403 (90%) of the 447 patients had benign conditions that could be confirmed during immediate imaging procedures the same day that consent was obtained (ie, date of initial visit). A median of 1 visit was necessary to complete diagnostic evaluations.
TABLE 4.
Timeliness of Care at Various Study Program Intervalsa
Data on the time from screening to diagnosis were available for 399 (89%) of the 447 women. These data were missing for the other 48 women (11%) because screening dates were not available for all patients initially seen in their individual county health departments or local clinics. Of the 399 women with data on the time from screening to diagnosis, 325 (81%) had a time interval of less than 60 days from screening to diagnosis, which meets the Centers for Disease Control and Prevention (CDC) quality benchmark. The other 74 women (19%) had a time interval of more than 60 days from screening to diagnosis because of appointment rescheduling and other socioeconomic barriers. Of these 74 women, 14 (19%) had to reschedule their appointments; no reasons for the extended interval were documented for any of the other women.
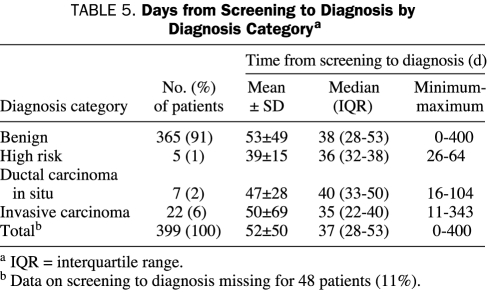
Time from screening to diagnosis by diagnosis category is presented in Table 5. The median time was shortest for patients with invasive carcinoma (35 days). Patients with DCIS had the longest interval (40 days). The mean time from screening to diagnosis for women undergoing biopsy was 56 days (range, 0-343 days) vs 51 days (range, 7-400 days) for those with no biopsy; median times were similar for both groups (37 vs 38 days). Timeliness of care for each BI-RADS category is presented in Table 6. Of the 73 patients with BI-RADS 4 or 5, 13 (18%) had a time interval of more than 60 days between screening and diagnosis. No significant differences were found between racial groups for any of the time intervals (eg, days from screening to diagnosis). The median time between screening and diagnosis for black, white, and Hispanic women was 36, 38, and 40 days, respectively; the median time for the entire patient population was 37 days.
TABLE 5.
Days from Screening to Diagnosis by Diagnosis Categorya
TABLE 6.
Timeliness of Care by BI-RADS Categorya
DISCUSSION
Our findings suggest that implementation of the patient navigator program at Mayo Clinic's site in Jacksonville, FL, was successful in providing timely diagnosis to underinsured women with breast cancer screening abnormalities. Of the 73 women with BI-RADS class 4 or 5 assessments, 60 (82%) received a diagnosis within 60 days of screening, which meets the CDC quality benchmark of 75% or more of patients receiving their diagnosis within 60 days.21,22 Most patients received a diagnosis in far less time; the median time from enrollment to diagnosis was 0 days for women assessed as either BI-RADS category 3 or 4 and 0.5 day for those assessed as BI-RADS category 5. Most patients enrolled in the program could be seen and given a diagnosis during the same visit. The highest number of procedures was performed in patients with a diagnosis of invasive carcinoma; the benign diagnosis group had the lowest number of procedures. The median time from screening to diagnosis was similar regardless of whether women underwent biopsy.
Similar successes in reaching the CDC benchmark by the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) have recently been reported. One series of studies examined the time intervals between breast cancer screening, diagnosis, and treatment among low-income women in the NBCCEDP during 2 periods (1996-2000 and 2001-2005).23 The median interval from screening to diagnosis for the 2 periods was 25 and 23 days, respectively. An earlier NBCCEDP study covering the years 1991-1995 reported a median interval from screening to diagnosis of 32 days, with 22% of women having an interval of more than 60 days.17 Although the median interval from screening to diagnosis in the current study (37 days) was higher than that reported in the earlier NBCCEDP studies, the trend for improved timeliness of diagnosis over the life of the NBCCEDP suggests further improvements may be attained with greater use of the patient navigator program. Several other possible explanations exist for the disparities reported for these different studies, and the CDC specifically advises against comparing performance across grantee programs owing to the extensive variation among them.16 For example, the NBCCEDP population was older than that in the current study (95% were aged 50-64 years).23 Programs also vary in support from state and community partners and in funding and other resources at their disposal. Nevertheless, comparing lessons from NBCCDP program implementation across programs by identifying barriers to care within each program ought to be a future goal.
Another limitation of this report is the lack of a comparative arm demonstrating advantages over standard care. Several other studies have done such comparisons, highlighting the inability to meet the CDC benchmark without a supportive program. One previous study compared women in a patient navigator program with women not in the program to evaluate whether unnecessary delays existed in breast cancer care for women in underserved populations.14 More women in the patient navigator program than not in the program had timely follow-up care (78% vs 64%; P<.0001). Women in that program also had access to diagnostic procedures that otherwise would not have been available to them. Similarly, a pilot study in 605 low-income women reported that patients using the Screening Adherence Follow-up Program were 2 to 3 times more likely than those not using the program to experience follow-up within 60 days of an abnormal mammogram finding.13
The 2004 position paper of the American College of Physicians on health care disparities discusses the need, which is currently unmet, for the entire continuum of the health care system to cooperate in addressing disparities in health care delivery to racial and ethnic minorities.9 The position paper proposes that members of the health care system “should reach out to surrounding community members and involve community representatives in planning and quality improvement initiatives.” The patient navigator program reported here demonstrated a successful collaboration between an academic center (Mayo Clinic's site in Jacksonville, FL) and community health centers. According to 2006 estimates by the US Census Bureau, more than 470,000 women aged 18 years or older live in the 4-county region covered by this study.20 In Florida, 20.3% of the population had no health insurance coverage from 2004 to 2006.23 Thus, a large number of women in this area are in need of resources to adequately ensure proper breast cancer diagnosis and could potentially benefit from a patient navigator program. This single patient navigator program covered an increasing number of patients between 2000 and 2006 over a relatively large area of 4 Florida counties, indicating that a single such program can effectively facilitate patient follow-up care after breast cancer screening over a wide geographic area.
More information on the applicability of patient navigator programs to other health care centers and geographic areas is needed. Information regarding patient treatment was not available in our study; therefore, time from diagnosis to treatment was not analyzed. Future studies are needed to evaluate this time interval, as well as the effect of patient navigator programs on outcomes such as patient satisfaction, adherence to treatment recommendations, and survival. Undoubtedly, patient navigator programs have cost benefits for the health care system; future studies on health outcomes benefits and reduced treatment costs should be implemented.
CONCLUSION
Timely diagnostic resolution of abnormal mammograms in medically underserved women is possible by using a coordinated, collaborative program between an academic medical center and public health departments. Most women with BI-RADS category 4 or 5 assessments received a diagnosis within 60 days of screening. Although this study quantitatively documented the role of a patient navigator program and its positive influence on patient care, greater attention to the much-needed services bridging breast cancer screening and treatment is necessary.
Acknowledgments
Editorial support of the submitted manuscript was provided by Chris A. Kirk, PhD, of Complete Healthcare Communications, and was funded by Pfizer.
Footnotes
Dr Wen is an employee of Pfizer and owns Pfizer stock.
This study was supported in part by the National Breast Cancer Foundation and Pfizer Oncology and an initial grant from the Susan G. Komen Breast Cancer Foundation. Support for the navigator program was provided by sanofiaventis, Bristol-Myers Squibb, and the Breast Cancer Research Foundation. Funding for this ongoing program is provided by a Mayo Clinic Cancer Center Health Disparities grant.
REFERENCES
- 1.DeNavas-Walt C, Proctor BD, Smith J, US Census Bureau http://www.census.gov/prod/2007pubs/p60-233.pdf. Current population reports: income, poverty, and health insurance coverage in the United States: 2006: p60-233. Published August 2007. Accessed February 5, 2009.
- 2.Halpern MT, Bian J, Ward EM, Schrag NM, Chen AY. Insurance status and stage of cancer at diagnosis among women with breast cancer. Cancer 2007;110(2):403-411 [DOI] [PubMed] [Google Scholar]
- 3.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008Jan–Feb;58(1):9-31 Epub 2007 Dec 20 [DOI] [PubMed] [Google Scholar]
- 4.Coughlin SS, Uhler RJ, Bobo JK, Caplan L. Breast cancer screening practices among women in the United States, 2000. Cancer Causes Control 2004;15(2):159-170 [DOI] [PubMed] [Google Scholar]
- 5.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008March;9(3):222-231 Epub 2008 Feb 20 [DOI] [PubMed] [Google Scholar]
- 6.Yabroff KR, Washington KS, Leader A, Neilson E, Mandelblatt J. Is the promise of cancer-screening programs being compromised? Quality of follow-up care after abnormal screening results. Med Care Res Rev. 2003;60(3):294-331 [DOI] [PubMed] [Google Scholar]
- 7.Asplin BR, Rhodes KV, Levy H, et al. Insurance status and access to urgent ambulatory care follow-up appointments. JAMA 2005;294(10):1248-1254 [DOI] [PubMed] [Google Scholar]
- 8.Hing E, Burt CW. Characteristics of office-based physicians and their medical practices: United States, 2005-2006. Vital Health Stat 13 2008April;(166):1-34 [PubMed] [Google Scholar]
- 9.Groman R, Ginsburg J, American College of Physicians Racial and ethnic disparities in health care: a position paper of the American College of Physicians. Ann Intern Med. 2004;141(3):226-232 [DOI] [PubMed] [Google Scholar]
- 10.GIVIO (Interdisciplinary Group for Cancer Care) Italy Reducing diagnostic delay in breast cancer: possible therapeutic implications. Cancer 1986;58(8):1756-1761 [DOI] [PubMed] [Google Scholar]
- 11.Robinson E, Mohilever J, Borovik R. Factors affecting delay in diagnosis of breast cancer: relationship of delay to stage of disease. Isr J Med Sci. 1986;22(5):333-338 [PubMed] [Google Scholar]
- 12.American Cancer Society http://www.cancer.org/docroot/CRI/CRI_2_3x.asp?dt=5. Detail Guide: Breast Cancer Web site. Accessed February 6, 2009.
- 13.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population: a patient navigation intervention. Cancer 2007;109(2 suppl):359-367 [DOI] [PubMed] [Google Scholar]
- 14.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer 2005;104(4):848-855 [DOI] [PubMed] [Google Scholar]
- 15.Ell K, Padgett D, Vourlekis B, et al. Abnormal mammogram follow-up: a pilot study in women with low income. Cancer Pract. 2002;10(3):130-138 [DOI] [PubMed] [Google Scholar]
- 16.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3(1):19-30 [PubMed] [Google Scholar]
- 17.Caplan LS, May DS, Richardson LC. Time to diagnosis and treatment of breast cancer: results from the National Breast and Cervical Cancer Early Detection Program, 1991-1995. Am J Public Health 2000;90(1):130-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richardson LC, Royalty J, Howe W, Helsel W, Kammerer W, Benard VB. Timeliness of breast cancer diagnosis and initiation of treatment in the National Breast and Cervical Cancer Early Detection Program (NBCCEDP). [ASCO Abstract 6571] J Clin Oncol. 2007;25(18S):339S [Google Scholar]
- 19.Eberl MM, Fox CH, Edge SB, Carter CA, Mahoney MC. BI-RADS classification for management of abnormal mammograms. J Am Board Fam Med. 2006;19(2):161-164 [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau http://factfinder.census.gov/servlet/ADPTable?_bm=y&-geo_id=16000US1235000&-qr_name=ACS_2007_3YR_G00_DP3YR5&-ds_name=&-_lang=en&-redoLog=false. American Community Survey (ACS) 2007. Accessed March 5, 2009.
- 21.Dept of Health and Human Services; Centers for Disease Control and Prevention http://www.cdc.gov/cancer/nbccedp/bccpdfs/policies_procedures.pdf. NBCCEDP program manual: NBCCEDP policies and procedures chapter. Accessed February 6, 2009.
- 22.Dept of Health and Human Services; Centers for Disease Control and Prevention http://www.cdc.gov/cancer/nbccedp/data/ National Breast and Cervical Cancer Early Detection Program: screening program data. Accessed February 6, 2009.
- 23.Dept of Health and Human Services; Centers for Disease Control and Prevention http://www.cdc.gov/cancer/nbccedp/data/summaries/florida.htm. National Breast and Cervical Cancer Early Detection Program: Florida. Accessed February 6, 2009.