Abstract
This study examined the relation between method of weight loss and long-term maintenance among successful weight losers enrolled in a weight loss maintenance trial. Participants were 186 adults (mean age=51.6 ± 10.7 years, mean BMI=28.6 ± 4.7 kg/m2) enrolled in the STOP Regain trial who had lost at least 10% of their body weight in the prior two years using a very low calorie diet (VLCD; n=24), commercial program (n=95), or self-guided approach (n=67). Participants were randomized to a weight maintenance intervention delivered face-to-face or over the internet or to a newsletter control condition, and followed for 18 months. At study entry, individuals who had used a VLCD had achieved a weight loss of 24% of their maximum weight within the last two years compared to 17% achieved by those who had used a commercial program or self-guided approach (p<.001). However, individuals who had used a VLCD regained significantly more weight than the other two groups and by six months, there were no significant differences in overall percent weight loss (i.e., initial weight loss and maintenance) between VLCD, commercial, and self-guided methods. In contrast, individuals who had used a self-guided approach maintained their weight losses from baseline through 18 months. The large initial weight losses achieved by individuals who had used a VLCD were not maintained over time, while individuals who had used a self-guided approach maintained their initial weight losses with the greatest success. The generalizability of these findings is limited by the sizeable weight losses achieved by study participants.
Keywords: weight maintenance, weight regain, diet
Approximately two thirds of American adults are overweight or obese (1). This presents a significant public health problem since obesity is associated with numerous medical complications, including increased risk of type 2 diabetes, cardiovascular disease, certain cancers, and death (2, 3).
A variety of weight loss methods are available, from minimally structured self-guided approaches to medically supervised very low calorie diet (VLCD; e.g., 400–800 kcal/day) regimens. The approach used to lose weight may be an important factor in both short-term and long-term weight control success. For example, research shows that intensive VLCD programs produce impressive weight losses of up to 20% in the short-term (4) but more than half of that weight loss is regained within 1–5 years (mean = 1.9 years) (5). Fewer studies have been conducted to examine the effectiveness of self-guided weight loss methods. Some data suggest that these approaches appear to result in minimal long-term (e.g., 2-year) weight loss outcomes compared to a commercial program (6). However, findings from the National Weight Control Registry (NWCR), a database of individuals who have achieved successful long-term weight loss, indicate that approximately 45% of NWCR members reported losing weight on their own (7). These individuals have lost large amounts of weight (mean=30 kg) and have maintained this weight loss for an average of 6.9 years (8).
An earlier study from the NWCR (8) compared weight maintenance strategies among successful weight losers who had initially lost weight either on their own, using an organized commercial or self-help program, or using a program with a liquid formula diet. This study showed some demographic differences between individuals who had used a liquid formula diet and those who had used either of the other approaches. For example, liquid formula users were older, heavier, had a greater history of weight cycling, and were more likely to have been diagnosed with a medical disorder compared to individuals who had lost weight on their own or had used an organized commercial or self-help program. All groups were found to use similar strategies to maintain their weight, such as consuming a low-calorie, low-fat diet and performing high levels of physical activity. However, this study did not evaluate patterns of weight regain across method of initial weight loss. In a recent chapter discussing NWCR members who used self-help or commercial programs to lose weight, weight regain over a 2-year period was noted to be comparable between these two groups, but the liquid formula group was not included (9).
Relatively little is known about whether method of initial weight loss impacts long-term weight control once significant weight loss has been achieved. Therefore, in the current study we examined long-term weight maintenance success among individuals who had lost at least 10% of their body weight using a VLCD, a commercial program, or a self-guided approach and subsequently entered an 18-month stand-alone weight maintenance program called STOP Regain.
METHOD
Participants
Participants enrolled in STOP Regain were adult men and women (N=314) who had lost at least 10% of their body weight within the two years prior to study entry (amount and timing of weight loss was confirmed in writing by a physician, friend, or weight loss counselor). Characteristics of the total sample have been reported (10). The current study included 186 STOP Regain participants who at baseline reported using one of the following methods to lose weight: a self-guided approach (e.g., followed a diet program from a book/magazine/other person, or used their own approach without following a published diet; n=67), a commercial program (e.g., Weight Watchers, Jenny Craig, Nutrisystem, or other commercial program; n= 95) or a medically supervised very low calorie liquid diet (VLCD; n=24). Individuals who used other methods of weight loss (e.g., counseling with a health care professional, medication, hypnosis, support groups) or reported using a combination of commercial and self-guided approaches were excluded.
Compared to STOP Regain participants not included in this investigation, the current study sample consisted of more men (22.6% vs. 13.3%, p=.038), had a slightly lower initial weight loss at baseline (17.7% vs. 19.5%, p=.047), reported lower cognitive restraint over eating (14.6 vs. 15.5, p=.017) and greater daily energy intake (1702 kcal vs. 1525 kcal, p=.013) at baseline, but did not differ with respect to age, racial background, employment status, intentional weight loss (cycling) history, baseline body mass index (BMI), or baseline levels of physical activity, daily fat intake, hunger, or disinhibition over eating.
Intervention
The STOP Regain weight maintenance intervention has been previously described (10). Briefly, the intervention was based on a self-regulation approach to weight control which focused on frequent self-weighing, self-reinforcement for successful weight maintenance, and immediate action to reverse small weight gains. Participants were randomized to the intervention delivered face-to-face or via the internet, or to a newsletter control in which information about diet, exercise, and weight control was sent quarterly. A recent report by Wing et al. (10).showed that the face-to-face intervention was more effective than either internet or control in reducing the magnitude of weight regain and that both face-to-face and internet modalities reduced the proportion of participants who regained 2.3 kilograms or more compared to the control condition. Participants in the present investigation were equally distributed across treatment conditions.
Assessments
Height and weight
Participant height was taken using a wall-mounted stadiometer. Weight was assessed in light street clothing using a calibrated scale and BMI was calculated as kg/m2. The primary weight change variable is overall percent weight loss from maximum weight in the last two years (also referred to as overall weight loss since it incorporates initial weight loss and maintenance). In addition, to be consistent with the results reported in Wing et al. (10), the proportion of each group that regained less than 2.3 kg (5 pounds) from baseline and the absolute magnitude of weight regain in kilograms from baseline to 6, 12, and 18 months are compared.
Other information was based on self-reported questionnaires from the baseline and 6-month assessments and included the following:
Demographic Information
Demographic information included age, gender, racial background, and employment status.
Weight loss (cycling) history
Intentional weight loss (cycling) history was assessed by asking participants the number of times (0, 1–2, 3–5, 6–10, or more than 10) they had intentionally lost 10–19 lbs, 20–49 lbs, 50–79 lbs, 80–99 lbs, and 100 lbs or more. Total amount of past intentional weight loss was calculated as a product of frequency and amount, using the lower end of both the frequency and amount ranges and summing across categories (11).
Eating behavior
Eating behavior was evaluated using the Eating Inventory (EI) (12, 13), a 51-item self-report scale comprised of three factors, including Cognitive Restraint, Disinhibition, and Hunger. The Cognitive Restraint subscale (range: 0–21) measures conscious restriction of food intake, the Disinhibition subscale (range: 0–16) measures tendency to experience eating dysregulation in response to emotional, cognitive, and social cues, and the Hunger subscale (range: 0–14) assesses susceptibility to hunger. The EI has well-established psychometric properties (12, 13).
Depressive Symptoms
Severity of depressive symptomatology was assessed using the Beck Depression Inventory (BDI) (14), a 21-item self-report measure (range = 0–63). The validity and reliability of the BDI have been well documented (15).
Dietary Intake
The Block Food Frequency Questionnaire (FFQ) (16) was used to assess total daily energy intake (kcals) and percent of daily intake from fat. The FFQ has been shown to correlate with 4-day food records (17).
Physical activity
Physical activity was measured using the Paffenbarger Activity Questionnaire (PAQ) (18), which provides an estimate of calories expended per week in overall leisure activity (e.g., number of stairs climbed, blocks walked) as well as in light (5 kcal/min), medium (7.5 kcal/min), and high (10 kcal/min) intensity activity. Previous studies have demonstrated associations between PAQ and weight change (19, 20).
Statistical Analyses
Data were analyzed using SPSS for Windows version 13.0 (21). Descriptive statistics are presented as means ± standard deviation (SD). Group differences on continuous variables assessed at baseline were evaluated using analyses of variance (ANOVA) with weight loss method as the grouping variable. Chi square tests were used to examine group differences on categorical variables. Group differences in weight regain at 6, 12, and 18 months were evaluated using analyses of variance (ANOVA) with weight loss method as the between subjects factor. Group differences across time in overall percent weight loss (initial weight loss and maintenance) were evaluated using repeated measures ANOVA, with weight loss method as the between subjects factor and percent weight reduction from maximum weight (at baseline, 6, 12, and 18 months) as the within subjects factor. Participants lost to follow-up were assumed to have gained .30 kilograms per month, as has been used in prior studies (10, 22, 23). Analyses were first conducted without adjustments for covariates and were then adjusted for variables found to differ at baseline (p<.10) across weight loss method, including gender, baseline weight, intentional weight loss (cycling) history, baseline percent fat intake, and percent weight reduction at baseline (i.e., initial weight loss). Analyses were also adjusted for duration of weight loss maintenance and STOP Regain treatment group (face-to-face intervention, internet intervention, newsletter control). Repeated measures ANOVAs with weight loss method as the between subjects factor and time (baseline and 6 months) as the within subjects factor were used to examine group × time interactions for dietary intake, physical activity, depressive symptoms, and eating behavior. Tests of significance were based on alpha of .05. For repeated measures analyses, Greenhouse-Geisser correction was used, where appropriate, to adjust for sphericity. Bonferroni adjustment was applied to main effect and simple effect post-hoc contrasts.
RESULTS
Table 1 shows the baseline characteristics of the 186 participants in the present study, categorized by type of weight loss method. Participants who had used a VLCD reported greater initial weight loss prior to enrolling in STOP Regain (p<.001) and a greater weight cycling history (p=.001) compared to those who had used either a commercial program or self-guided approach. Women comprised the majority of participants in all weight loss methods; however, a larger percentage of men used a self-guided approach than a commercial program (31% vs. 15%, p=.011).
Table 1.
Participant characteristics at baseline across weight loss method
| VLCD (n=24) | Commercial (n=95) | SG (n=67) | |
|---|---|---|---|
| Age (years) | 52.7 ± 9.3 | 51.8 ± 10.8 | 51.0 ± 11.1 |
| Gender (% female)* | 71 | 85 | 69 |
| Race (% Caucasian) | 100 | 97 | 97 |
| Employment Status (% employed) | 75 | 82 | 78 |
| Weight (kg) | 84.6 ±17.4 | 76.2 ± 15.4 | 79.1 ± 17.6 |
| BMI (kg/m2) | 30.5 ± 5.0 | 28.1 ± 4.2 | 28.6 ± 5.2 |
| % weight reduction (initial weight loss)† | 24.1 ± 9.4 | 16.6 ± 6.1 | 17.1 ± 7.1 |
| Duration of weight loss maintenance (mo) | 12.9 ± 6.9 | 12.4 ± 7.1 | 12.8 ± 8.9 |
| Intentional weight loss (cycling) history (kg)‡ | 98.1 ± 105.1 | 45.5 ± 41.8 | 46.3 ± 63.8 |
| Caloric intake (kcals/day) | 1821 ± 876 | 1632 ± 575 | 1760 ± 749 |
| % of total kcals from fat§ | 33.5 ± 6.4 | 31.9 ± 6.3 | 38.7 ± 11.8 |
| Physical activity (kcals expended/week) | 2060 ± 1072 | 1787 ± 1429 | 2024 ± 1351 |
| Beck Depression Inventory | 4.7 ± 4.3 | 4.0 ± 4.2 | 3.6 ± 3.5 |
| EI Cognitive Restraint | 15.0 ± 3.6 | 14.9 ± 3.2 | 14.4 ± 3.3 |
| EI Disinhibition | 8.5 ± 3.9 | 8.5 ± 3.2 | 8.2 ± 3.9 |
| EI Hunger | 5.0 ± 3.2 | 5.6 ± 3.6 | 5.3 ± 2.9 |
Plus/minus values are means ± SD; VLCD = Very low calorie diet; SG = Self-guided; BMI = Body mass index; EI = Eating Inventory
More women in Commercial than SG, p=.011
VLCD > Commercial, VLCD > SG, p<.001
VLCD > Commercial, VLCD > SG, p=.001
SG > Commercial (p<.001), SG > VLCD, (p=.037)
Overall Percent Weight Loss
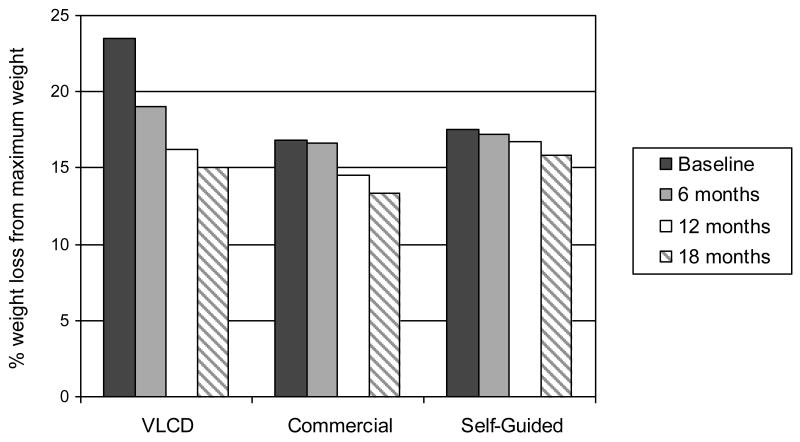
Analysis of group differences in overall percent weight loss (initial weight loss and maintenance) revealed a significant weight loss method × time interaction (p<.001). As illustrated in Figure 1, participants who had used a VLCD had achieved significantly greater initial percent weight reduction at entry to the STOP Regain trial compared to individuals who had used a commercial program or self-guided approach (p<.001). However, within six months, overall percent weight reduction among participants who had used a VLCD no longer differed significantly from that of participants who had used either of the other two methods. In addition, of the three groups, only individuals who had lost weight on their own maintained initial weight losses from baseline to 18 months, while individuals who had used a VLCD or commercial program evidenced significant decreases in overall percent weight loss over time. Findings remained significant after adjustments for gender, baseline weight, intentional weight loss (cycling) history, baseline fat intake, duration of weight loss maintenance, and STOP Regain treatment group (see Table 1 for descriptive statistics on relevant variables).
Figure 1.
Percent weight loss from maximum weight in the past two years (overall percent weight loss). A significant weight loss method × time interaction (p<.001) was found. At entry to STOP Regain, participants who had used a VLCD had lost significantly more weight than those who had used a commercial program or self-guided approach but by 6 months (and continuing through 12 and 18 months) no significant differences in percent weight reduction were present. Individuals who had used a VLCD or commercial program evidenced significant decreases in total weight losses over time while those who had lost weight on their own maintained initial weight losses from baseline to 18 months. Note: VLCD: very low calorie diet. Values are adjusted means controlling for gender, baseline weight, intentional weight loss (cycling) history, baseline fat intake, duration of weight loss maintenance, and STOP Regain treatment group.
Weight Regain
Fewer participants who had used a VLCD to lose weight maintained their weight loss within 2.3 kg from baseline compared to those who had used a commercial program or self-guided approach. By six months, only 21% of those who had used a VLCD were maintaining their weight loss within 2.3 kg compared to 76% of those who had used a commercial program and 75% of those who had lost weight on their own, p<.001. By 18 months, those numbers reduced to 13% for VLCD compared to 46% for commercial and 55% for self-guided, p<.01.
This pattern is also reflected in the absolute magnitude of weight regain over time as depicted in Table 2. Participants who had used a VLCD regained more weight than those who had used either a commercial program or self-guided approach during the first six months (p<.001), and greater weight regain in this group continued through the end of the 18-month STOP Regain trial. These findings remained significant after adjusting for gender, baseline weight, intentional weight loss (cycling) history, percent weight reduction at baseline (i.e., initial weight loss), fat intake at baseline, duration of weight loss maintenance, and STOP Regain treatment group.
Table 2.
Mean weight change (kg) from baseline across weight loss method
| VLCD (n=24) | Commercial (n=95) | SG (n=67) | |
|---|---|---|---|
| Baseline to 6 months*,† | 4.5 ± 0.9 | 0.5 ± 0.4 | 0.2 ± 0.6 |
| Baseline to 12 months‡,§ | 7.2 ± 1.4 | 2.7 ± 0.7 | 0.6 ± 0.8 |
| Baseline to 18 months‡,† | 7.9 ± 1.4 | 4.0 ± 0.7 | 1.7 ± 0.9 |
Plus/minus values are adjusted means (kg) ± SE controlling for gender, baseline weight, intentional weight loss (cycling) history, percent weight reduction at baseline (initial weight loss), baseline fat intake, duration of weight loss maintenance, and STOP Regain treatment group; VLCD = Very low calorie diet; SG = Self-guided
VLCD > Commercial, p=.001
VLCD > SG, p=.001
VLCD > Commercial, p<.05
VLCD > SG, p<.001
Since significantly greater weight regain among individuals who had used a VLCD was evident during the first six months of the STOP Regain trial, we examined whether there were differential changes in self-reported dietary intake, physical activity, depressive symptoms, or Eating Inventory scores during this period that may have accounted for group differences in weight outcomes (see Table 3). However, results showed no significant weight loss method × time interaction for any of these variables, indicating that dietary intake, physical activity, depressive symptoms, cognitive restraint, disinhibition, and hunger did not change differentially across weight loss method from months 1–6.
Table 3.
Self-reported dietary intake, physical activity, depressive symptoms, and Eating Inventory scores at baseline and 6 months across weight loss method*
| VLCD | Commercial | SG | ||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | Baseline | 6 months | Baseline | 6 months | |
| Caloric Intake (kcals/day)† | 1832 ± 916 | 1472 ± 717 | 1659 ± 576 | 1588 ± 586 | 1759 ± 761 | 1600 ± 608 |
| % kcals from fat | 33.8 ± 6.6 | 33.3 ± 5.0 | 32.1 ± 6.3 | 31.7 ± 6.5 | 39.0 ± 12.0 | 38.8 ± 12.0 |
| Physical activity (kcals expended per week) | 2060 ± 1072 | 2082 ± 1725 | 1837 ± 1433 | 1987 ± 1605 | 2077 ± 1345 | 2082 ± 2306 |
| Beck Depression Inventory | 4.7 ± 4.3 | 5.0 ± 4.1 | 4.0 ± 4.1 | 3.4 ± 4.1 | 3.6 ± 3.6 | 3.9 ± 5.3 |
| EI Cognitive Restraint | 15.1 ± 3.7 | 14.1 ± 4.4 | 14.9 ± 3.2 | 14.8 ± 3.6 | 14.3 ± 3.4 | 14.5 ± 3.7 |
| EI Disinhibition | 8.4 ± 3.9 | 8.9 ± 4.1 | 8.7 ± 3.2 | 8.3 ± 3.4 | 8.4 ± 3.8 | 8.5 ± 3.9 |
| EI Hunger | 5.2 ± 3.3 | 5.4 ± 3.8 | 5.9 ± 3.7 | 5.6 ± 4.0 | 5.2 ± 2.9 | 5.1 ± 3.1 |
Plus/minus values are means ± SD; VLCD = Very low calorie diet; SG = Self-guided; EI = Eating Inventory
Sample sizes vary due to missing data at 6 months: dietary intake (VLCD: n=22; Commercial: n=81; SG: n=62), physical activity (VLCD: n=24; Commercial: n=88; SG: n=63), Beck Depression Inventory (VLCD: n=24; Commercial: n=87; SG: n=63), EI subscales (VLCD: n=22; Commercial: n=84; SG: n=62).
Main effect of time (p<.001)
DISCUSSION
Previous research has shown that individuals who lose weight using VLCD regimens achieve impressive short-term weight losses but subsequently experience significant regain such that mean weight losses at long-term follow-up are not different from those who followed a moderately restricted calorie diet (i.e., 800–1800 kcal/day) (5). Results of the current study support these previous findings. Specifically, we found that at the start of a weight loss maintenance trial, individuals who had used a VLCD to lose weight had achieved significantly greater weight losses compared to those who had used either a commercial program or self-guided approach. However, these participants regained a significant amount of weight rather quickly and as early as six months into the trial (and continuing through to 18 months), overall percent weight loss among individuals who had used a VLCD did not differ from those who had used a commercial program or self-guided approach. In contrast, individuals who had lost weight on their own maintained their initial weight loss throughout the 18-month period with great success. Initial weight losses among individuals who had lost weight using a commercial program or self-guided approach were large - both groups entered the STOP Regain program having achieved a 17% reduction from maximum weight. Both groups maintained these weight losses for the first six months, but those who had used a commercial program evidenced significant weight regain beginning at month 12.
As detailed by Elfhag and Rossner (24), there are numerous factors that influence successful weight loss maintenance, including weight history variables such as weight cycling and initial weight loss, behavioral factors such as eating patterns and physical activity, and cognitive factors such as motivation and self-efficacy. In the current study, we found no differences across method of weight loss on caloric intake, physical activity, eating behavior (e.g., restraint, disinhibition), or depressive symptoms at entry to the maintenance program. Further, we adjusted for several baseline variables that differed across method of weight loss and could have differentially impacted weight regain and overall weight loss over time, including weight cycling history, initial weight loss, and dietary fat intake. Controlling for these variables did not alter our finding that individuals who had used a VLCD regained significantly more weight than those who had used a commercial program or self-guided approach.
Since the pattern of regain among participants who had used a VLCD was evident during the first six months of the trial, we examined whether there were differential changes in self-reported dietary intake, physical activity, depressive symptoms, or eating behavior across method of weight loss during this period that may have partially explained the weight outcomes. However, no significant differential changes in these variables were found.
Failure to detect differences in behavior that parallel weight regain among individuals who had used a VLCD may reflect the influence of demand characteristics in the context of a weight maintenance program or inaccurate self-report of eating and physical activity in this group. Alternatively, these findings may suggest the presence of other important factors influencing weight loss maintenance for individuals who lose weight through VLCD regimens compared to less intensive approaches. For example, it is possible that choice of weight loss method reflects confidence in one’s ability to lose weight on one’s own vs. with support of a program. Individuals who select a very intensive treatment such as a VLCD may have lower confidence in their ability to lose weight than those who opt for a self-guided approach. Similarly, individuals who lose weight on their own may be more likely to attribute success to their own efforts rather than to a weight loss program. Potential differences in confidence and attributions regarding weight loss success may impact continued behavior change and long-term maintenance of weight loss. Although perceived difficulty with weight loss and maintenance were not evaluated in the current investigation, the earlier study from the NWCR (8) found that individuals who had used a liquid diet reported greater difficulty maintaining weight loss than losing weight, while individuals who had lost weight on their own reported the opposite pattern- that maintenance was less difficult than weight loss. Thus, it is also possible that different perceptions of how hard it is to maintain weight loss may play a role in long-term weight control success.
The present study confirms and extends earlier findings from the NWCR. Similar to reports from the NWCR (8), we note that women comprise a larger proportion of the commercial program group than the VLCD or self-help group, and that VLCD users have a greater history of weight cycling. While no differences in self-reported weight regain were found between commercial and self-help users in the NWCR (9) the present study indicates that among individuals who had used VLCD, commercial, or self-guided approaches to lose weight, only the self-guided group maintained their weight losses over 18 months. Strengths of the present study include the fact that all participants were actually weighed and that retention over 18 months was excellent.
The participants in this study had all been very successful at initial weight loss, achieving an average of an 18% reduction in body weight. Since these weight losses are larger than what is typically achieved in commercial and self-help approaches (but perhaps more comparable to weight losses achieved with very low calorie diets (4)), a primary limitation of the current findings is that they cannot be generalized to all who utilize these approaches. Data are not available that allow us to determine the percent of individuals who enter VLCD or commercial programs or attempt to lose weight on their own that achieve weight losses of this magnitude, but clearly only a subgroup of participants achieves such success. The purpose of this study was to examine weight loss maintenance among individuals who were initially successful at losing weight using these approaches. The selected nature of these participants must be kept in mind when considering the present findings. Additional limitations of this study include self-selection to weight loss method and the limited size of the VLCD group.
The present study is unique in that participants were enrolled in a stand-alone weight maintenance program after having lost a clinically significant amount of weight using either a VLCD, commercial program, or self-guided approach. We found that individuals who had used a VLCD achieved the greatest initial weight losses but also experienced the greatest regain and within six months of entering the STOP Regain trial, their overall percent weight loss was comparable to those of individuals who had used a commercial program or self-guided approach. In contrast, individuals who had lost weight on their own maintained their initial weight losses with the greatest success. Further research is needed to better understand how these individuals may differ in terms of their level of confidence, motivation, commitment, or other factors that might be related to long-term weight loss maintenance.
Acknowledgments
This research was supported by National Institutes of Health grants R01DK057413 and K23DK075645.
Footnotes
Clinical Trial Registration for the “STOP Regain” clinical trial is NCT00067145 in www.clinicaltrials.gov
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 3.Field AE, Barnoya J, Colditz G. Epidemiology and health and economic consequences of obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. New York: The Guilford Press; 2002. pp. 3–18. [Google Scholar]
- 4.Wadden TA, Foster GD, Letizia KA. One-year behavioral treatment of obesity: comparison of moderate and severe caloric restriction and the effects of weight maintenance therapy. J Consult Clin Psychol. 1994;62:165–71. doi: 10.1037//0022-006x.62.1.165. [DOI] [PubMed] [Google Scholar]
- 5.Gilden Tsai A, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Obesity (Silver Spring) 2006;14:1283–93. doi: 10.1038/oby.2006.146. [DOI] [PubMed] [Google Scholar]
- 6.Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA. 2003;289:1792–8. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 7.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66:239–46. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 8.McGuire MT, Wing RR, Klem ML, Seagle HM, Hill JO. Long-term maintenance of weight loss: do people who lose weight through various weight loss methods use different behaviors to maintain their weight? Int J Obes Relat Metab Disord. 1998;22:572–7. doi: 10.1038/sj.ijo.0800627. [DOI] [PubMed] [Google Scholar]
- 9.Butryn ML, Phelan SP, Wing RR. Self-guided approaches to weight loss. In: Latner JD, Wilson GT, editors. Self-Help Approaches for Obesity and Eating Disorders: Research and Practice. New York: Guilford Press; 2007. pp. 3–20. [Google Scholar]
- 10.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355:1563–71. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 11.Jeffery RW, French SA. Socioeconomic status and weight control practices among 20- to 45-year-old women. Am J Public Health. 1996;86:1005–10. doi: 10.2105/ajph.86.7.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 13.Stunkard AJ, Messick S. Eating Inventory Manual. San Antonio, TX: Harcourt Brace Jovanovich; 1988. [Google Scholar]
- 14.Beck A, Steer RA. Beck Depression Inventory Manual. San Antonio, TX: The Psychological Corporation Harcourt Brace Jovanovich, Inc; 1987. [Google Scholar]
- 15.Beck A, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- 16.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–69. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 17.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 18.Paffenbarger R, Wing A, Hyde R. Physical activity as an index of heart attack risk in college alumni. Am J of Epidemiol. 1978;108:161–75. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 19.Harris J, French S, Jeffery R, PG M, Wing R. Dietary and physical activity correlates of long-term weight loss. Obesity Research. 1994;2:307–13. doi: 10.1002/j.1550-8528.1994.tb00069.x. [DOI] [PubMed] [Google Scholar]
- 20.Ewbank PP, Darga LL, Lucas CP. Physical activity as a predictor of weight maintenance in previously obese subjects. Obes Res. 1995;3:257–63. doi: 10.1002/j.1550-8528.1995.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 21.SPSS. SPSS for Windows, 13.0. Chicago: SPSS Inc; 2004. [Google Scholar]
- 22.Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C. Benefits of lifestyle modification in the pharmacologic treatment of obesity: a randomized trial. Arch Intern Med. 2001;161:218–27. doi: 10.1001/archinte.161.2.218. [DOI] [PubMed] [Google Scholar]
- 23.Wadden TA, Berkowitz RI, Womble LG, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med. 2005;353:2111–20. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- 24.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]