Abstract
Consistent with a risk reduction model of targeted prevention, the present investigation piloted and empirically evaluated the feasibility and short-term efficacy of a first-generation panic prevention program that targeted two malleable risk factors for panic development – anxiety sensitivity and daily cigarette smoking. Members of a high risk cohort, defined by high levels of anxiety sensitivity and current daily smoking (n = 96), were randomly assigned to either (1) a one session intervention focused on proximally increasing motivation to quit smoking and reducing anxiety sensitivity to distally prevent the development of panic or (2) a health information control condition of comparable length. Participants were followed for six months. Consistent with hypotheses, those in the treatment condition showed reduced anxiety sensitivity and this effect was maintained across the follow-up period. Limited evidence also suggested the intervention increased motivation to quit smoking. We discuss how this prevention protocol can be modified in the future to enhance its effects as part of second-generation larger-scale outcome evaluations.
Keywords: prevention, panic, anxiety sensitivity, smoking, comorbidity
Although there have been notable advances in prevention programs for anxiety and its disorders (see Feldner, Zvolensky, & Schmidt, 2004, for a review), this corpus of work is currently at an early stage in its development (Dozois & Dobson, 2004; Ginsburg, 2004; Rapee, 2002; Schmidt & Zvolensky, 2007). Programs targeting the prevention of panic psychopathology, specifically, are still highly limited. In the only available study in this domain, Gardenswartz and Craske (2001) examined participants at risk for developing panic disorder, as indexed by having had an unexpected panic attack within the past 12 months and endorsing at least moderate levels of anxiety sensitivity (AS; Reiss & McNally, 1985; Taylor, 1999) on the Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986). Young adults were randomly assigned to either a wait-list control (n = 66) or a preventive intervention condition (n = 55) that consisted of a single 5-hour group session. Components of the intervention included psychoeducation, breathing retraining, cognitive restructuring, interoceptive exposure, instruction to expose in-vivo to agoraphobic-type situations, and homework. Findings indicated that more of the wait-list (13%) than workshop (1%) group developed panic disorder by the 6-month follow-up. Additionally, a composite of panic frequency × panic intensity decreased significantly more in the workshop than wait-list group. This study provides empirical support for the potential utility of using anxiety-related cognitive behavioral methods in the prevention of panic disorder among young adults.
An important next step in work on the prevention of panic development is expanding in a theoretically-driven manner the type of risk factors targeted and the intervention methods used. Although there are numerous empirically-supported risk factors across levels of analysis (biological, social, behavioral; see Craske & Zucker, 2001; Otto, 2002) that could be targeted in prevention programs, one promising avenue is to integrate substance use into intervention models. Indeed, aside from being highly common in the general population (Grant et al., 2004), various forms of substance use, abuse, and dependence are related to increased risk for panic attacks and panic disorder (Kushner, Sher, & Erikson, 1999; Price & Giannini, 1987; Zvolensky, Bernstein et al., 2006; Zvolensky, Feldner, Leen-Feldner, & McLeish, 2005). One theoretically and empirically promising risk factor for panic psychopathology is daily cigarette smoking (Zvolensky & Bernstein, 2005). Indeed, cigarette smoking is prospectively related to increased risk for panic attacks, panic disorder, and agoraphobia (Breslau & Klein, 1999; Breslau, Novak, & Kessler, 2004; Isensee, Wittchen, Stein, Höfler, & Lieb, 2003; Johnson et al., 2000; McLeish, Zvolensky, & Bucossi, 2007; Zvolensky, Lewinsohn et al., in press) as well as more severe concurrent panic symptoms (Zvolensky, Forsyth, Fuse, Feldner, & Leen-Feldner, 2002; Zvolensky, Leen-Feldner et al., 2004; Zvolensky, Sachs-Ericsson, Feldner, Schmidt, & Bowman 2006; Zvolensky, Schmidt, & McCreary, 2003).
Integrative theoretical models of the nature of smoking-panic comorbidity suggest this type of drug behavior may interplay with other risk factors for panic problems in a clinically meaningful manner (Zvolensky & Bernstein, 2005; Zvolensky, Schmidt, & Stewart, 2003). Anxiety sensitivity (AS) is a relatively stable fear of anxiety-related sensations (McNally, 2002; Reiss & McNally, 1985). Evidence suggests that high levels of this cognitive factor increase the likelihood of the future development for panic attacks, and possibly panic disorder (Donnell & McNally, 1990; Ehlers, 1995; Hayward, Killen, Kraemer, & Taylor, 2000; Maller & Reiss, 1992; Schmidt, Lerew, & Jackson, 1997, 1999; Weems, Hayward, Killen, & Taylor, 2002). Though AS is not the only panic risk factor relevant to smoking (see e.g., Zvolensky, Sachs-Ericsson et al., 2006), there is now empirical and theoretical evidence that suggests it is a particularly important one (Zvolensky, Feldner et al., 2005; Zvolensky, Schmidt et al., 2003).
These models begin with the recognition that, in the majority of instances, smoking precedes the development of panic attacks and panic disorder (Bernstein, Zvolensky, Schmidt, & Sachs-Ericsson, 2007). Among certain daily smokers, such as those who fear anxiety, smoking serves important affect regulatory functions (Zvolensky & Bernstein, 2005). These individuals, specifically, expect tobacco use to help alleviate aversive anxiety states (Gregor, Zvolensky, McLeish, Bernstein, & Morissette, in press; Zvolensky, Feldner et al., 2004) and often principally smoke to regulate affect in a habitual manner (Leyro, Zvolensky, Vujanovic, & Bernstein, in press; Zvolensky, Bonn-Miller et al., 2006). As the objective mood-dampening qualities of smoking are complex (Kassel, Stroud, & Paronis, 2003; Parrot, 1999), it may well be useful to conceptualize these processes at the cognitive level of analysis. Thus, in the absence of other more adaptive coping strategies, high anxiety sensitive smokers may learn to rely on smoking to manage anxiety states and fears of bodily sensations in the short-term. Over longer periods of time, however, smoking itself will lead to increased risk of bodily sensations and aversive internal states via a number of routes, including nicotine-based withdrawal symptoms, health impairment, and physical illness. Exposure to these types of aversive stimuli may facilitate learning that internal cues can be personally harmful, dangerous, and anxiety-evoking. Although smokers with pre-morbid vulnerability factors, like high levels of AS, are often especially motivated to quit smoking (Zvolensky, Baker et al., 2004; Zvolensky, Vujanovic et al., 2007), they also are at high risk for problems in quitting (Lasser et al., 2000; Zvolensky, Lejuez, Kahler, & Brown, 2004). Specifically, these persons are apt to be particularly fearful of, and emotionally reactive to, internal states that occur during smoking discontinuation; they may therefore experience more distressing emotional experiences in general (Zvolensky, Kotov, Antipova, & Schmidt, 2003), but particularly during cessation attempts (Zvolensky, Lejuez et al., 2004). Thus, a vicious cycle may develop, whereby smoking is used as a coping strategy for managing aversive states in the short term, yet paradoxically confers longer-term risk for panic development.
From a general intervention standpoint, risk reduction models of prevention that highlight the importance of simultaneously targeting multiple independent risk factors for a given disorder (Mrazek & Haggerty, 1994; National Advisory Mental Health Council Workgroup on Mental Disorders Prevention Research, 1998) suggest targeting both of these empirically and theoretically supported risk factors for panic development may be particularly fruitful for the development of panic prevention programs. In terms of panic development specifically, simultaneously targeting these risk factors to reduce the future onset of panic problems as well as stimulate cessation-oriented behavior (e.g., enhance motivation to quit; Zvolensky, Bernstein, Yartz, McLeish, & Feldner, 2008) may yield a particularly efficacious approach to panic prevention (Zvolensky, Schmidt, Bernstein, & Keough, 2006). Specifically, because AS and smoking interact in clinically meaningful ways, addressing one of these factors without considering the other may not be optimal. For example, simply targeting AS without recognition of smoking among high AS daily smokers who manage affect by smoking (Zvolensky, Bonn-Miller et al., 2006) neglects clinically-relevant self-regulation processes (e.g., negative affect reduction motives for smoking; Schmidt et al., 2007). Likewise, because AS is related to poorer success in quitting smoking (Brown et al., 2001; Zvolensky, Bonn-Miller, Bernstein, & Marshall, 2006), a failure to target this cognitive vulnerability may yield lower rates of success in quitting (Zvolensky & Bernstein, 2005).
The overarching aim of the present study was to develop and empirically evaluate a theoretically-driven prevention protocol for high AS daily smokers that proximally targets increasing motivation to quit smoking and reducing anxiety sensitivity in order to distally prevent panic development. The Psychosocial Intervention targeting AS and Smoking (PIAS) consisted of a single two-hour session focused on (1) psychoeducation regarding anxiety, panic, and associations between panic and smoking, (2) instruction in basic smoking cessation skills, (3) practice in various panic-relevant interoceptive exposure techniques, and (4) homework assignments consisting of practicing self-guided exposure. Program effects were compared to a health information control group, which was based on previous control conditions utilized in anxiety prevention research (Schmidt et al., 2007).
There were two primary objectives of the study. First, we sought to develop and standardize intervention materials for an integrative prevention program for panic problems. This approach is consistent with Phase 1 of behavioral therapy development (Rounsaville, Bruce, Carroll, & Onken, 2001). In particular, we aimed to standardize a two-hour group-based intervention. A group format was adopted because this approach typically requires fewer resources to implement; therefore, a group format may ultimately be less costly relative to individually-administered interventions. Second, we sought to recruit a target young adult sample of high AS daily smokers and evaluate the feasibility of enrolling and retaining them in a group-based prevention protocol. Due to limited knowledge regarding challenges of recruiting and retaining this high risk group, this aspect of the study represents an important and recommended step in gauging the feasibility of ultimately implementing this type of prevention program (Mrazek & Haggerty, 1994). In addition to these general objectives, we also tested specific hypotheses pertaining to the proximal targets of the PIAS. Here, we tested the hypotheses that the PIAS would proximally reduce AS and increase cognitive-affective aspects of smoking cessation “readiness” (i.e., increase motivation and confidence to quit smoking and reduce cigarettes smoked per day) compared to the control group. These hypothesized effects were expected to maintain throughout the six-month follow-up period. Finally, we also conducted exploratory analyses that examined possible longer-term outcomes of the PIAS. These included comparing groups at the six month follow-up in terms of smoking status, smoking quit attempts during the follow-up period, incidence of panic attacks, agoraphobic avoidance, anxiety, and depression. This broad assessment of factors that may have been affected by the PIAS was conducted consistent with recommendations for conducting prevention trials (Mrazek & Haggerty, 1994).
Method
Screening
A two-phase screening process was utilized to identify eligible persons. Phase I consisted of administration of the ASI (Reiss et al., 1986) and a single question that indexed daily cigarette use (i.e., “How many cigarettes a day do you smoke?”) to college students at four Universities and members of the general community in the northeastern United States. Screenings were administered in person at recruitment booths in local market places and on multiple college campuses as well as via electronic mail messages. Inclusionary criteria included being a regular smoker (≥ 10 cigarettes per day) and having total scores on the ASI (Reiss et al., 1986) of at least one standard deviation above the mean for males (≥ 24) or females (≥ 31).
Phase II consisted of contacting, via telephone, potentially eligible persons (i.e., high AS regular smokers) to administer the screening portion of the Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-NP; First, Spitzer, Gibbon, & Williams, 1995) and portions of the Psychosocial Treatment Interview (PTI; Steketee et al., 1997). Consistent with contemporary models of selective prevention (Mrazek & Haggerty, 1994), persons with a positive lifetime history of panic attacks or mental health treatment (psychosocial or pharmacological), Axis I psychopathology, suicidal ideation, or inability to give informed, voluntary, written consent to participate (assessed via unstructured clinical interview) were excluded from participation and provided referral information upon request. These conservative exclusionary criteria permit tests of the effects of the PIAS on the etiology of panic-related psychopathology, as opposed to effects on the maintenance of such problems. During both phases, persons were informed that screenings were being conducted to identify persons eligible for a study focused on the prevention of anxiety and no information regarding participants’ risk was provided.
Participants
Of approximately 500 persons participating in Phase I of the screening, 185 met inclusionary criteria. Of the 185 people meeting AS and smoking inclusionary criteria, 36 (19%) were no longer interested upon contact in Phase II of the screening and 53 (28%) were excluded from participation for one or more of the following reasons: panic attacks or panic disorder (PD; n = 28), depression (n = 13), psychotropic medication use (n = 13), and other anxiety-related problems (n = 10). The final sample consisted of 96 high AS daily smokers (38 women; Mage = 19.79 years, SD = 2.23), as defined by smoking at least 10 cigarettes per day for at least one year. Race was as follows: 93% Caucasian, 1% Asian, 1% American Indian/Alaska Native, and 5% choose not to specify race. At the pre-experimental assessment, participants smoked on average 12.21 (SD = 3.92) cigarettes per day, began smoking at age 13.88 (SD = 2.48), and considered themselves regular smokers by age 16.51 (SD = 3.55).
Measures
The screening portion of the SCID-NP was used to measure lifetime prevalence of panic attacks, Axis I diagnoses, suicidal ideation, and medication use (First et al., 1995). Responses that indicated uncertainty (e.g., “I don’t know,” “I can’t remember,” or “Yes, but it wasn’t bad”) were treated as a positive endorsement. This interview was employed during the screening phase of the project because of its broad focus on Axis I psychopathology generally, which was necessary given the exclusionary criteria described above.
The Anxiety Disorders Interview Schedule-IV (ADIS-IV; Di Nardo, Brown & Barlow, 1994) was administered at the six-month follow-up to measure the six-month prevalence of panic attacks, Axis-I diagnoses, and suicidal ideation. The ADIS-IV was utilized, rather than the SCID-NP, at the six-month follow-up due to its specific and more detailed focus on anxiety disorders (of central interest at the follow-up assessment). Adequate reliability of the ADIS has been demonstrated (Di Nardo, Moras, Barlow, Rapee, & Brown, 1993).
The Anxiety Sensitivity Index (ASI; Reiss et al., 1986) is a 16-item measure in which respondents indicate on a five-point Likert-type scale (0 = very little to 4 = very much) the degree to which they are concerned about possible negative consequences of anxiety symptoms. The means for nonclinical male and female college students are 15.40 (SD = 8.10) and 20.50 (SD = 10.20), respectively (Reiss et al., 1986). The ASI has high levels of internal consistency in clinical and nonclinical populations (range of alpha coefficients: 0.79 to 0.90) and good test-retest reliability (r = .75 for two weeks to r = .70 for three years; Peterson & Reiss, 1992). The ASI is unique from, and demonstrates incremental validity compared to, negative affectivity (Zvolensky, Kotov, Antipova, & Schmidt, 2005) and trait anxiety (Rapee & Medero, 1994). In the present investigation, we utilized the total ASI score, as it represents the global-order AS factor and therefore takes into consideration different types of fears, including fears of panic-related somatic, cognitive, and social cues (Zinbarg, Mohlman, & Hong, 1999).
The Mobility Inventory for Agoraphobia (MI; Chambless, Caputo, Jasin, Gracely, & Williams, 1985) is a widely used measure of agoraphobic avoidance. Participants rate the degree to which they avoid 27 specific situations (e.g., theatres) on a 1 (never avoid) to 5 (always avoid) Likert-type scale. The MI can be used to assess agoraphobic avoidance of various situations under two conditions: when the respondent is alone or when accompanied by a friend. Evidence supports the validity of the MI (Chambless et al., 1985; Craske, Rachman, & Tallman, 1986; Kotov, Schmidt, Zvolensky, Vinogradov, & Antipova, 2005).
The Mood and Anxiety Symptom Questionnaire (MASQ; Watson et al., 1995) is a 40-item comprehensive measure of affective symptoms (e.g., cheerful, afraid, confused). This self-report instrument assesses mood dimensions important to the tripartite model of anxiety and depression (Watson et al., 1995). The General Distress: Depressive Symptoms scale (MASQ: GDD) measures depressed mood expected to be nondifferentiating relative to anxiety (e.g., “felt discouraged”). The General Distress: Anxious Symptoms scale (MASQ: GDA) indexes anxious mood expected to be nondifferentiating relative to depression (e.g., “felt nervous”). The Anxious Arousal scale (MASQ-AA) measures the symptoms of somatic tension and arousal (e.g., “felt dizzy”). The Anhedonic Depression scale (MASQ-AD) measures a loss of interest in life (e.g., “felt nothing was enjoyable”) and reverse-keyed items measuring positive affect. The MASQ-AD was used in the current project to index depressive symptoms and the MASQ-AA was used to index anxiety symptoms. Participants indicated on a five-point Likert-type scale how much they experienced each symptom from 1 (not at all) to 5 (extremely) during the past week. The MASQ shows excellent convergence with other measures of anxiety and depression (Watson et al., 1995) and has been employed in studies of panic vulnerability (Zvolensky, Kotov, Antipova, & Schmidt, 2005).
The Psychosocial Treatment Interview (PTI; Steketee et al., 1997) measures the type and frequency of psychosocial services received by research participants. Series of service utilization as well as specific types of treatments administered by providers are measured by the PTI. The PTI was utilized to identify history of psychosocial treatment utilization (for assessing exclusionary criterion) and to measure total number of psychosocial health care service uses during the six-month follow-up. The PTI has demonstrated good psychometric properties (Steketee et al., 1997).
The Motivational Aspects of Smoking Cessation Questionnaire (MASC-Q; Rundmo, Smedslund, & Götestam, 1997) is an 11-item questionnaire that measures various aspects of participants’ motivation to quit smoking. Section A of the MASC-Q indexes motivation to utilize 10 different specific approaches to smoking cessation, which participants rate on a 0 (no, not at all motivated) to 4 (yes, very motivated) Likert-type scale. An example item is “I wish to try nicotine gum because I wish to quit smoking.” Section B of the MASC-Q consists of a 0 (no interest) to 100 (complete interest) scale that assesses participants’ overall motivation to quit smoking. The MASC-Q has demonstrated good internal consistency (Cronbach’s α = .95) and has been employed successfully both as an index of overall motivation to quit smoking (Rundmo et al., 1997) and in work on anxiety and smoking (Zvolensky, Baker et al., 2004).
The Smoking Situations: Confidence Questionnaire (SS-CQ; Velicer, DiClemente, Rossi, & Prochaska, 1990) is a well-established nine-item measure of confidence in remaining abstinent from smoking that has been utilized in previous work on anxiety and smoking (e.g., Zvolensky, Bonn-Miller et al., 2006). The SSC includes nine different situations (e.g., “when I am extremely anxious or stressed”) and asks respondents to indicate whether or not they would smoke in such situations, with extent of confidence in such judgments rated on a five point Likert type scale (1 = not at all confident to 5 = extremely confident).
Standardized smoking history and current status indices, as agreed upon by a National Cancer Institute consensus panel, were utilized to measure smoking history and pattern. Items from this measure were administered in questionnaire format (i.e., Smoking History Questionnaire; SHQ) at the pre-group assessment and in interview format (i.e., Smoking History Interview; SHI) at the follow-up assessment. Both administration formats have successfully been utilized in prior research on smoking and panic (Zvolensky, Feldner, Eifert, & Brown, 2001; Zvolensky, Forsyth, Fuse, Feldner, & Leen-Feldner, 2002). Smoking-related behaviors measured included (but were not limited to) smoking rate, number and duration of previous smoking quit attempts, and age of smoking onset. Consistent with previous studies (Brown, Lejuez, Kahler, & Strong, 2002; Zvolensky, Lejuez et al., 2004), this measure was used to index total number of smoking cessation attempts made during the six-month follow-up period.
Assessment Strategy and Interviewers
Screening procedures (see “Participants” section) were completed using the screening portion of the SCID-NP (First et al., 1995), a single question that indexed cigarettes smoked per day, a screening question added to the PTI (Steketee et al., 1997), and the ASI (Reiss et al., 1986). The pre-intervention assessment consisted of re-administration of the ASI and the question indexing cigarette use as well as administration of the MASQ (Watson et al., 1995), MI (Chambless et al., 1985), MASC-Q (Rundmo et al., 1997), SS-CQ (Velicer et al., 1990), and SHQ. The post-intervention assessment consisted of the ASI, MASC-Q, and SS-CQ. The three-month phone contact consisted of administration of the ASI and the single question indexing cigarettes smoked per day. The six-month follow-up assessment consisted of the ADIS-IV, SHI, PTI, ASI, MASQ, MI, MASC-Q, SS-CQ, and the question indexing cigarettes smoked per day.
The two interviewers were trained upper-level undergraduate students who were supervised by the Principal Investigator (PI; MTF). Interviewers received intensive training in the administration of the SCID-NP screener and the ADIS-IV prior to initiation of the study that included: (1) weekly individual and group supervision meetings; (2) observing the PI administer both interviews; and (3) administering both interviews under direct observation of the PI at least twice and until both the interviewer and the PI determined mastery criteria were met. Specifically, interviews were administered under the supervision of the PI until at least 95% inter-rater reliability was obtained. Throughout the duration of the study, both interviewers were carefully supervised and psychologists other than the PI (Ellen W. Leen-Feldner, Ph.D., and Michael J. Zvolensky, Ph.D.) were available to correct for rater drift and for consultation regarding specific diagnostic questions.
Procedures
Eligible participants were randomly assigned to either the PIAS or a control group. Group size was allowed to vary to increase our ability to schedule eligible participants (M = 8.72; range = 3 to 17). All groups were conducted by the PI or other psychologists trained in both the cognitive behavioral treatment of PD and smoking cessation (Ellen W. Leen-Feldner, Ph.D., Michael J. Zvolensky, Ph.D.). All participants were informed that the study was testing the effects of a program designed to prevent the development of anxiety. No information regarding participants’ "at risk" status was provided. Upon arrival to the group session, participants were administered the pre-intervention assessment battery. Then group leaders completed the procedures for the panic-specific intervention or general health information control group (see below). All materials for both groups were tailored to low-literacy populations (e.g., lecture material was targeted for persons with approximately an 8th grade education). Immediately after the 2-hour group session, participants completed the post-intervention assessment battery and were compensated $30. Three months post-group session, participants were contacted via telephone and administered the three-month assessment battery. Six months post-group session, participants were contacted and scheduled to attend a follow-up assessment session; here, the six-month follow-up assessment was completed. Upon completion of the follow-up session, participants were debriefed and compensated $50.
Psychosocial Intervention targeting Anxiety Sensitivity and Smoking (PIAS)
The PIAS consisted of a single two-hour group session. The two-hour duration was chosen to balance feasibility with ensuring time to address the main targets of the intervention. The first (30-min) component of the 2-hour session consisted of psychoeducation regarding the nature of anxiety/fear, PD, the role of common misinterpretations involved in maintaining panic problems, and how such emotional processes can presumably be affected by smoking. Psychoeducation regarding anxiety, panic, and common misinterpretations was adapted from the Mastery of Your Anxiety and Panic III (MAP-III; Craske & Barlow, 2000) PD treatment manual. Explicit attention was devoted to the smoking-stress relation, which suggests emotionally vulnerable persons may tend to rely on smoking as a coping strategy for negative emotional states (Parrott, 1999). We also discussed that although the potential anxiolytic effects of smoking are complex (Kassel & Unrod, 2000), smokers generally expect tobacco smoking to (temporarily) relieve anxiety-related states (Juliano & Brandon, 2002). Thus, a self-perpetuating cycle may ensue, whereby smoking among high AS individuals is used to cope with anxiety states, yet such behavior will be ineffective in reducing overall levels of anxiety about bodily sensations. The second (45-min) component involved basic instruction in smoking cessation. Given the brief nature of this intervention, this component was primarily designed to increase smoking cessation motivation and self-efficacy, rather than increase quitting per se. Information about standard, individual smoking cessation treatments based on the most recent clinical practice guidelines from the U.S. Department of Health and Human Services, Treating Tobacco Use and Dependence, was provided to participants. Included was a brief review of the positive health consequences of quitting and education about techniques associated with successful quit attempts (e.g., self-monitoring cigarettes smoked per day, identifying high risk situations and developing coping strategies for each situation identified, discussing ways to increase social support during a quit attempt). Additionally, a copy of the National Cancer Institute’s publication, Clearing the Air, which discusses these types of cessation strategies for smokers who are trying to quit, was given to each participant. Throughout this instructional phase, the importance of quitting smoking in terms of helping reduce panic problems also was emphasized. Although the overall context and information provided to participants was encouraging change toward non-smoking behavior, participants were not asked specifically to quit smoking. Rather, this component was designed primarily to demonstrate that the provision of brief smoking cessation information can be successfully integrated into a panic prevention program at this stage of research development. The third (45-min) component consisted of teaching participants the rationale for, and procedures utilized in, self-guided interoceptive exposure. This component was based on the MAP-III (Craske & Barlow, 2000). Three exposure techniques were practiced in the session: voluntary hyperventilation, breathing through a small straw, and rapid head lifts. Participants were instructed to practice these same strategies at home twice per week for approximately 30 seconds after bodily sensations are first experienced. Participants also were taught to use the Exposure Exercise Record (Craske & Barlow, 2000) to monitor self-guided exposure.
Control Group
Participants in the general health information control condition attended one two-hour group session that included discussion of the following: the importance of maintaining a healthy body weight (e.g., calculating and understanding body mass indices); healthy dietary habits (e.g., reading food nutritional labels); and sleep hygiene recommendations (e.g., get enough sleep to feel rested). No information relevant to anxiety, panic, or smoking was presented. Participants were instructed in the use of daily meal planning forms and asked to complete a meal plan twice weekly. This control condition was employed to increase the internal validity of the current study by controlling for therapist contact time. In addition, health-related information, as opposed to other information, was presented to maintain consistency with prior anxiety prevention work targeting AS (Schmidt et al., 2007).
Data Analytic Strategy
To test the hypotheses regarding the effects of the PIAS, relative to the control group, on AS, motivation to quit smoking, smoking cessation self-efficacy, and cigarettes per day individual growth curve models estimated in Proc Mixed in SAS (Littell, Milliken, Stroup, & Wolfinger, 1996) were utilized. This approach to data analysis is also referred to as hierarchical linear modeling (HLM) and random effects regression analysis. Individual growth curve modeling procedures were utilized because they are more powerful for examining response patterns over time compared to repeated measures ANOVAs (Muthén & Curran, 1997). These analyses allow for testing the current investigation’s hypotheses by determining whether variability in post-group measures and the trajectory of change during the follow-up period could be accounted for by group membership. Two parameters are estimated in individual growth curve modeling. It was hypothesized that group membership would predict proximal target levels by the post-group assessment, rather than the pre-group assessment. Thus, the first parameter (intercept or starting point) was defined as the first post-group data point (e.g., ASI score post-group). Therefore, an association between group membership and the intercept parameter reflects a relation between group membership and immediately-post-group levels of each target. The second parameter (change over time or slope) represents the slope of the growth curve or trajectory during the follow-up period after the first data point (intercept). For example, an association between group membership and the slope parameter indicates group membership was associated with the slope of change in the repeated measure (e.g., ASI scores) across time during the follow-up period. Individual growth curve models also provide an overall estimate of the effects of change over time, which in the current study indicates how the proximal targets changed across the follow-up period without consideration of other predictors. All intercept (post-group) and time (slope) parameters were entered first into the models as random effects. As we were primarily interested in the relation between group membership and levels of targeted factors post-group, we entered pre-group levels of the each proximal target as covariates into each model, which is recommended for examining change over time as opposed to employing change scores (Cohen, Cohen, West, & Aiken, 2003). For instance, baseline AS level was included as a covariate in models predicting post-group through follow-up levels of AS. Theoretically-relevant variables found to differ between groups at baseline also were entered as covariates. Finally, group membership (coded: 0 = control, 1 = intervention) and the first order interaction [time (slope) × group membership] were entered.2
Results
Descriptive Data and Zero-order Correlations
Zero-order correlations among theoretically-relevant variables at the pre-group assessment are provided in Table 1. Of particular interest is the nonsignificant correlation between AS and cigarettes smoked per day (r = .07). While this correlation may have been attenuated by excluding persons low in AS, the nonsignificant association is consistent with several prior studies of healthy young adults (Feldner et al., in press; Zvolensky, Bonn-Miller, Feldner et al., 2006; Zvolensky, Feldner, Leen-Feldner, Gibson et al., 2005) and suggests these are two distinct risk factors. Gender was associated with daily cigarettes smoked, where women reported smoking fewer per day (M = 11.06, SD = 3.04) than men (M = 12.98, SD = 4.24). In terms retention, 73 participants (76%) were contacted at the 3-month follow-up and 62 (64%) returned for the 6-month follow-up assessment. Rates of participant retention did not differ between the PIAS and control groups (p > .1). Also, participants who did not return for the six-month follow-up assessment did not differ from those who did return in terms of any baseline variable (e.g., pre-group ASI scores, cigarettes smoked per day; all p’s > .1).
Table 1.
Zero-order Correlations among Theoretically-relevant Variables at Baseline
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | |||||||||||
| 1. Gender | - | .18 | −.24* | .12 | .15 | −.06 | .00 | .07 | .26* | −.07 | .06 |
| Primary (Proximal) Targets | |||||||||||
| 2. Anxiety Sensitivity (ASI) | - | - | .07 | .26** | .03 | −.15 | .35** | .42** | .42** | .48** | −.04 |
| 3. Cigarettes per Day | - | - | - | .22* | −.02 | −.31** | .21* | .15 | −.03 | .16 | −.11 |
| 4. Motivation to Quit (MASC-Q Section A) | - | - | - | - | .33** | −.07 | .17 | .15 | .23* | .31** | .05 |
| 5. Motivation to Quit (MASC-Q Section B) | - | - | - | - | - | .18 | .03 | −.15 | .08 | .03 | .18 |
| 6. Confidence to Quit (SS-CQ) | - | - | - | - | - | - | −.06 | −.11 | −.09 | −.07 | .00 |
| Secondary (Distal) Targets | |||||||||||
| 7. Anxious Arousal (MASQ) | - | - | - | - | - | - | - | .38** | .42** | .33** | −.16 |
| 8. Anhedonic Depression (MASQ) | - | - | - | - | - | - | - | - | .29** | .40** | −.29** |
| 9. Agoraphobic Avoidance–Alone (MI) | - | - | - | - | - | - | - | - | - | .59** | .12 |
| 10. Agoraphobic Avoidance - Accompanied (MI) | - | - | - | - | - | - | - | - | - | - | .00 |
| 11. Lifetime Quit Attempts (SHQ) | - | - | - | - | - | - | - | - | - | - | - |
Note: Total n = 96.
Gender coded 1 = male, 2 = female; ASI = Anxiety Sensitivity Index (Reiss et al., 1986); MASC-Q = Motivational Aspects of Smoking Cessation Questionnaire (Rundmo et al., 1997); SS-CQ = Smoking Situations: Confidence Questionnaire (Velicer et al., 1990); MASQ = Mood and Anxiety Symptom Questionnaire (Watson et al., 1995); MI = Mobility Inventory for Agoraphobia (Chambless et al., 1985); SHQ = Smoking History Questionnaire.
p for between group difference < .05
p for between group difference < .01.
Pre-experimental Comparisons
To test the efficacy of the random assignment procedure, one way ANOVAs were conducted to compare the PIAS and control groups at baseline in terms of demographic variables and proximal targets (see Table 2). In terms of participant demographics, there was a significant difference in terms of gender [t (94) = 2.11, p < .05], with fewer women in the PIAS (n = 14; 29%) than control (n = 24; 50%) group. Participants in the PIAS group also reported (on Section B of the MASC-Q) less motivation to quit smoking (M = 50.62, SD = 24.74) than those in the control group [M = 61.64, SD = 25.43; t (94) = 4.62, p < .05]. There were no other baseline between-group differences (all p’s > .1; see Table 3).
Table 2.
Means (Standard Deviations) for Psychological and Smoking-Related Proximal Variables at the Pre and Post-Group, Three-Month, and Six-Month Follow-Up Assessments as a Function of Group
| Assessment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Screening | Pre | Post | 3-Months | 6-Months | ||||
| Anxiety-Related Variable | ||||||||
| Anxiety Sensitivity (ASI) | ||||||||
| Intervention | 30.83 (5.37)** | 23.18 (8.50) | 15.25 (8.50)* | 17.27 (8.78)** | 16.59 (8.20) | |||
| Control | 35.33 (9.08)** | 23.26 (10.59) | 18.08 (9.69)* | 24.30 (11.04)** | 20.63 (13.19) | |||
| Smoking-Related Variables | ||||||||
| Cigarettes per Day | ||||||||
| Intervention | 13.58 (4.04)12.13 (3.81) | N/A | 9.05 (5.76) | 8.07 (5.98) | ||||
| Control | 13.36 (3.21)12.31 (4.04) | N/A | 11.40 (5.89) | 7.42 (5.49) | ||||
| Motivation to Quit (MASC-Q – Section A) | ||||||||
| Intervention | N/A | 12.06 (8.22) | 10.34 (12.10) | N/A | 12.53 (10.43) | |||
| Control | N/A | 12.50 (7.34) | 12.10 (8.89) | N/A | 12.20 (10.03) | |||
| Motivation to Quit (MASC-Q – Section B) | ||||||||
| Intervention | N/A | 50.62 (24.74)* | 53.95 (28.49) | N/A | 61.12 (34.79) | |||
| Control | N/A | 61.64 (25.43)* | 65.29 (24.97) | N/A | 57.66 (30.88) | |||
| Confidence to Quit (SS-CQ) | ||||||||
| Intervention | N/A | 20.33 (5.44) | 20.72 (5.58) | N/A | 25.30 (8.71) | |||
| Control | N/A | 19.16 (4.90) | 19.45 (5.59) | N/A | 25.53 (9.03) | |||
Note: Total n = 96 at screening, pre, and post-group, 73 at the 3-month follow-up, and 62 at the 6-month follow-up.
N/A = Not assessed; MASC-Q = Motivational Aspects of Smoking Cessation Questionnaire (Rundmo et al., 1997); SS-CQ = Smoking Situations: Confidence Questionnaire (Velicer et al., 1990); ASI = Anxiety Sensitivity Index (Reiss et al., 1986).
p for between group difference < .05
p for between group difference < .01.
Table 3.
Means (Standard Deviations) or Frequencies for Psychological and Smoking-Related Outcomes at the Pre-Group and Six-Month Follow-Up Assessments as a Function of Group
| Group | ||||
|---|---|---|---|---|
| Intervention | Control | |||
| Pre-Group | 6-Monthsa | Pre-Group | 6-Monthsa | |
| Smoking Characteristics | ||||
| Smoking Quit Attempts | ||||
| Lifetime (SHQ) | 2.47 (2.26) | 2.27 (1.87) | ||
| Past Six Months (SHI) | 0.96 (0.84) | 1.10 (0.99) | ||
| Quit by Six-Month Follow-Up | 7 (14%) | 3 (6%) | ||
| Panic-Related Symptoms | ||||
| Panic Attacks | 3 (6%) | 2 (4%) | ||
| Agoraphobic Avoidance (MI) | ||||
| Alone | 38.46 (10.12) | 38.73 (12.52) | 43.33 (14.77) | 37.66 (10.85) |
| Accompanied | 28.73 (6.13) | 29.34 (6.54) | 32.02 (9.77) | 30.60 (9.77) |
| Anxious Arousal (MASQ) | 26.06 (7.45) | 25.21 (8.66) | 27.41 (6.40) | 26.70 (9.44) |
| Anhedonic Depression (MASQ) | 60.14 (12.64) | 57.63 (14.39) | 61.64 (13.12) | 55.96 (14.78) |
Note: Total n = 96 (48 in intervention, 48 in control) pre-group and 62 (32 in intervention, 30 in control) at the 6-month follow-up.
SHQ = Smoking History Questionnaire; SHI = Smoking History Interview; MI = Mobility Inventory for Agoraphobia (Chambless et al., 1985); MASQ = Mood and Anxiety Symptom Questionnaire (Watson et al., 1995)
percentages were calculated assuming participants not returning for follow-up did not quit smoking or develop an anxiety problem
n reflects number of participants seeking treatment during the six-month follow-up period.
Post-Group through Follow-Up
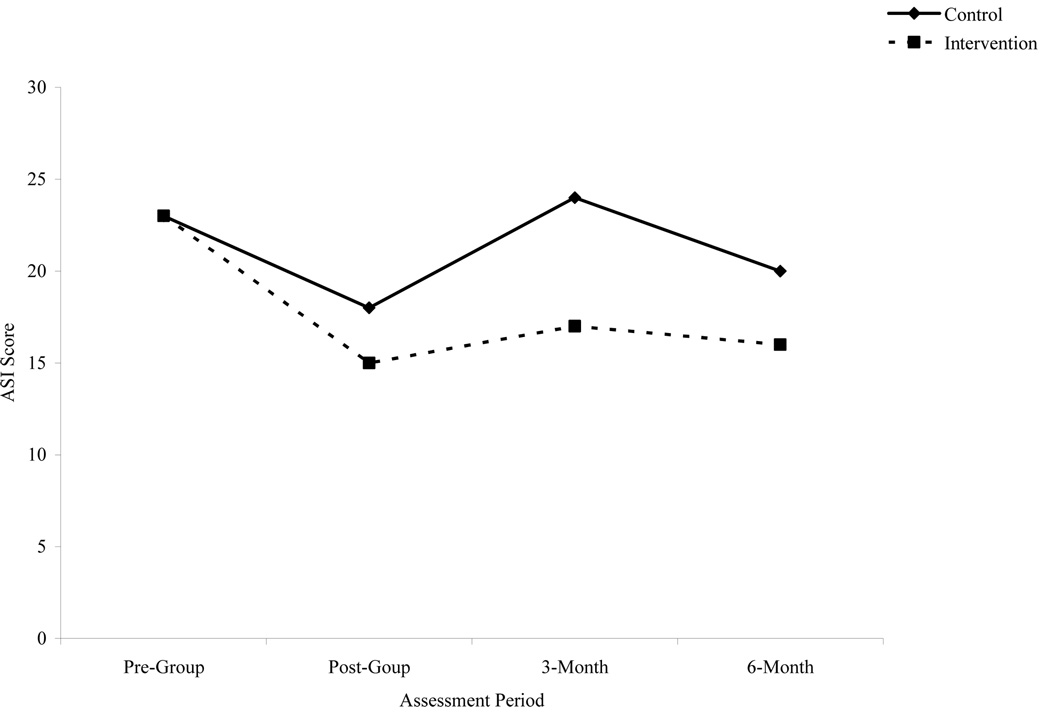
Based on the pre-experimental comparisons, gender was included as a covariate in all group comparisons in addition to baseline level of each outcome. Effects of the PIAS were first examined on AS and smoking-cessation related behaviors using individual growth curve modeling (see Table 4). In terms of AS, there was significant variability in post-group ASI scores [intercept; t (1, 92) = 8.37, p < .0001] and pre-group ASI scores significantly predicted post-group ASI scores [t (1, 92) = 8.53, p < .0001]. After controlling for pre-ASI levels, group membership predicted post-group (intercept) ASI scores [t (1, 92) = −2.41, p < .05]. Time (slope) also predicted ASI scores [t (1, 133) = 2.20, p < .05], suggesting AS increased across groups from the post-group to the 6-month follow-up assessment. Group membership did not predict change in ASI scores during the follow-up period (slope). See Figure 1 for a graphic representation of ASI scores as a function of group. Given the significant relation between group membership and post-group ASI scores, in combination with the finding that group membership was not related to rate of change in ASI scores across the recovery period, planned comparisons were utilized to compare groups in terms of ASI scores at the three-month and six-month follow-up assessments. Specifically, ANCOVAs, with gender and pre-group ASI scores as covariates, were employed with the Bonferroni correction procedure in place to protect against increased chances of Type I error resulting from these multiple comparisons. Groups were not compared at the post-group assessment because this time point is captured in the growth curve model as the intercept (i.e., group membership significantly predicted post-group ASI scores). At the 3-month follow-up, participants in the PIAS reported significantly lower ASI scores than those in the control group [F (3, 69), p < .05]. As an index of effect size, η2 = .08. Groups did not significantly differ at the six-month follow-up assessment. See Table 2 for means and standard deviations for ASI scores as a function of group at each assessment period.
Table 4.
Individual Variable Contributions in Growth Curve Models of the Effects of the PIAS on Proximal Targets
| Estimate | df | t | p | |
|---|---|---|---|---|
| Dependent Variable: Anxiety Sensitivity (ASI) | ||||
| Intercept | 18.86 | 92 | 8.37 | <.0001 |
| Time (slope) | 1.86 | 133 | 2.20 | <.05 |
| Gender | 0.05 | 92 | 0.04 | ns |
| Pre-Group Anxiety Sensitivity (ASI) | 0.59 | 92 | 8.53 | <.0001 |
| Group | −3.25 | 92 | 2.41 | <.05 |
| Time (slope) × Group | −0.61 | 133 | 0.52 | ns |
| Dependent Variable: Cigarettes per Day | ||||
| Intercept | 11.76 | 77 | 6.30 | <.0001 |
| Time (slope) | −3.83 | 51 | −3.12 | <.01 |
| Gender | −0.09 | 77 | −0.09 | ns |
| Pre-Group Cigarettes per Day | 0.64 | 77 | 4.70 | <.0001 |
| Group | −2.42 | 77 | −1.84 | .06 |
| Time (slope) × Group | 2.88 | 51 | 1.74 | ns |
| Dependent Variable: Motivation to Quit (MASC-Q Section A) | ||||
| Intercept | 10.26 | 90 | 6.03 | <.0001 |
| Time (slope) | 0.17 | 59 | 0.10 | ns |
| Gender | 1.11 | 90 | 1.10 | ns |
| Pre-group Motivation to Quit (MASC-Q Section A) | 0.83 | 90 | 13.40 | <.0001 |
| Group | −1.31 | 90 | −1.27 | ns |
| Time (slope) × Group | 1.89 | 59 | 0.79 | ns |
| Dependent Variable: Motivation to Quit (MASC-Q – Section B) | ||||
| Intercept | 54.03 | 92 | 11.37 | <.0001 |
| Time (slope) | −7.46 | 58 | −1.43 | ns |
| Gender | 3.60 | 92 | 1.25 | ns |
| Pre-group Motivation to Quit (MASC-Q Section B) | 0.92 | 92 | 16.45 | <.0001 |
| Group | 0.38 | 92 | 0.13 | ns |
| Time (slope) × Group | 16.29 | 58 | 2.22 | <.05 |
| Dependent Variable: Confidence to Quit (SS-CQ) | ||||
| Intercept | 19.20 | 92 | 15.92 | <.0001 |
| Time (slope) | 6.19 | 61 | 4.44 | <.0001 |
| Gender | 0.50 | 92 | 0.68 | ns |
| Pre-Group Confidence to Quit (SS-CQ) | 0.85 | 92 | 12.55 | <.0001 |
| Group | 0.37 | 92 | 0.52 | ns |
| Time (slope) × Group | −2.10 | 61 | −1.09 | ns |
Note: Gender coded 1 = male, 2 = female; Groups coded 0 = control, 1 = intervention; ASI =Anxiety Sensitivity Index (Reiss et al., 1986); MASC-Q = Motivational Aspects of Smoking Cessation Questionnaire (Rundmo et al., 1997); SS-CQ = Smoking Situations: Confidence Questionnaire (Velicer et al., 1990).
Figure 1.
Scores on the ASI as a function of group.
Number of cigarettes smoked per day was not assessed post-group, as this would not have differed from pre-group levels. Thus, the intercept in this model represented the number of cigarettes smoked per day as measured at the three-month assessment-period. There was significant variability [t (1, 77) = 6.30, p < .0001] in cigarettes smoked per day at the 3-month follow-up (intercept) and pre-group levels of cigarettes per day was a significant predictor [t (1, 77) = 4.70, p < .0001]. Although group membership approached traditional levels of statistical significance (p = .06), there were no statistically significant predictors of cigarettes smoked per day at the 3-month follow-up (intercept). Time (slope) was again a significant predictor [t (1, 51) = −3.12, p < .01], suggesting the number of cigarettes participants were smoking daily across groups decreased from the three-month to the six-month follow-up assessment. Group membership did not significantly predict change in cigarettes smoked per day from the three to the six-month follow-up assessment (slope).
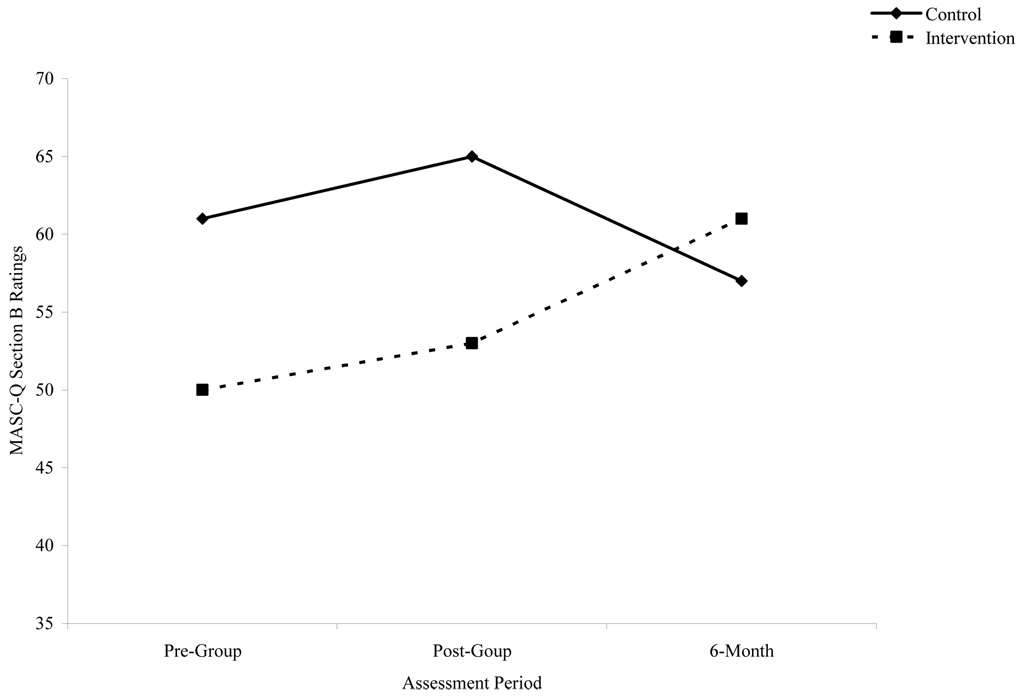
With regard to motivation to quit smoking, both MASC-Q Section A scores and Section B ratings were examined. First, there was significant variability in post-group MASC-Q Section A scores [t (1, 90) = 6.03, p < .0001]. Only pre-group MASC-Q Section A scores predicted post-group (intercept) scores [t (1, 90) = 13.40, p < .0001]. In terms of MASC-Q Section B ratings, there was again significant variability in post-group ratings [intercept; t (1, 92) = 11.37, p < .0001] and pre-group ratings significantly predicted post-group ratings [intercept; t (1, 92) = 16.45, p < .0001]. Here, group membership significantly predicted change in MASC-Q Section B ratings from the post-group to the 6-month follow-up assessments [slope; t (1, 58) = 2.22, p < .05]. See Figure 2 for a graphic representation of the regression lines for MASC-Q Section B ratings.
Figure 2.
Ratings on Section B of the MASC-Q as a function of group.
In terms of confidence to quit smoking, there was significant variability [t (1, 92) = 15.92, p < .0001] in SS-CQ scores at the post-group assessment (intercept) and pre-group SS-CQ levels significantly predicted post-group levels [intercept; t (1, 92) = 12.55, p < .0001].1 Time (slope) was again a significant predictor of change in SS-CQ scores across the follow-up period [t (1, 61) = 4.44, p < .0001], which suggested that across groups confidence to quit smoking increased from post-group to the six-month follow-up assessment. Group membership did not significantly predict SS-CQ scores.
Finally, ANCOVAs were employed to compare groups in terms of level of other psychological and smoking-related outcomes at the six-month follow-up assessment (see Table 3). While there was a trend consistent with expectation in terms of smoking cessation, no between-group differences reached statistical significance.
Discussion
In the present study, we developed and standardized intervention materials for the PIAS and successfully recruited and retained a target sample of high AS daily smokers. Indeed, a sample sufficient for monitoring the effects of the PIAS on targeted risk factors was obtained, which will allow for refinement of the intervention in subsequent iterations. Such refinement of preventive interventions is critical and recommended prior to larger scale implementation and evaluation (Mrazek & Haggerty, 1994). Two considerations for subsequent efforts at targeting this group, in particular, became apparent during the study. First, relatively large recruitment pools appear necessary for identifying high AS smokers with no history of psychopathology. Approximately 26% (132 of 500) of persons responding to recruitment efforts, all of whom were smokers, were eligible for participation and a portion of these (an additional 36 people) chose not to participate for a variety of reasons (e.g., burdensome time commitment, no longer interested). Thus, a recruitment pool of smokers approximately four times the size of the targeted size of the high AS smoker sample appears necessary. Therefore, recommendations to monitor the cost-effectiveness of prevention programs (Mrazek & Haggerty, 1994) are particularly pertinent to future larger-scale examinations of this type of intervention. Increasing follow-up durations that allow for a window into the distal effects of the PIAS (i.e., PD prevention) will provide important insight into the potential for these types of programs to reduce high public health costs associated with panic problems (Greenberg et al., 1999). For instance, integrating PIAS groups into smoking cessation programs where they can be delivered to patients high in AS could yield significant reductions in PD development. Given the group format and brief duration of the PIAS, even small preventive effects may result in substantial cost savings. Importantly, the cost effectiveness of this type of program needs to be addressed empirically after additional controlled testing and refinement of the program.
Second, targeting high AS smoking adolescents, as opposed to young adults, to increase the percentage of people without positive histories of anxiety psychopathology may prove fruitful. In the current study, approximately 28% (n = 53) of high AS young adult smokers who initially expressed interest in the study already reported psychopathology or related treatment. As smoking is common among adolescents (Johnston, O’Malley, Bachman, & Schulenberg, 2004), focusing on this younger age group may increase the feasibility of recruiting high AS smokers prior to psychopathology development and also increase the implementability of this intervention approach in larger-scale trials.
A second aim of the investigation pertained to gauging the feasibility of delivering the PIAS in a single-session group-based format. Here, we found that there were few obstacles to having individuals participate successfully in a group-based protocol; similar evidence has been reported for other group-based prevention programs for individuals at risk for anxiety problems (Gardenswartz & Craske, 2001; Lowry-Webster, Barrett, & Lock, 2003). Indeed, no problems were encountered during any portion of the group, including the conduct of exposure practice in a group setting. Even in groups with as many as 17 participants, no obstacles were encountered when teaching the principles behind exposure (e.g., eliciting and observing bodily sensations results in extinction of learned fear) and practicing related exercises. This pattern suggests using a group format with a population of high AS smokers is feasible and these persons do not appear avoidant of a group-based social context where preventive information is discussed and exposure exercises are practiced. These preliminary observations suggest adopting a group format in subsequent prevention tests with this population is warranted, particularly in light of possible reduced costs associated with group-based versus individual intervention. Future studies with this population should formally assess participants’ interest in, and satisfaction with, a group format to increase confidence in these observations. It is important to note here, however, that relatively consistent recruitment efforts likely are needed to fill groups of high AS regular smokers given the relatively low base rate of this combined risk profile (as discussed above). To increase the breadth of contexts where the PIAS may be implemented and empirically examine the effects of a group versus individual format, future development in this area should adapt the PIAS to fit an individual format.
In terms of the proximal effects of the PIAS on targeted risk factors, consistent with prediction, the PIAS reduced AS compared to the control group by the post-group assessment and this effect maintained through the three-month follow-up assessment. However, groups did not significantly differ by the six-month follow-up. In terms of smoking, results indicated the PIAS increased overall motivation to quit smoking. Specifically, ratings on Section B of the MASC-Q suggested the intervention increased motivation to quit during the follow-up period, whereas such motivation decreased among persons in the control group (see Figure 2). Although the different slopes observed as a function of group suggest this finding was not solely due to regression to the mean, replication of this result will be important to increase confidence that the PIAS increased motivation to quit smoking. There was relatively little change from post-group to the six-month follow-up assessment (see Table 4) in terms of motivation to utilize specific cessation techniques (as indexed on Section A of the MASC-Q; Rundmo et al., 1997). Also, there were no differences between groups in cigarettes smoked per day or smoking cessation rates by the six month follow-up. It is also important to note here that consistent with expectation, levels of AS and smoking were not significantly correlated, suggesting these are two distinct risk factors, which is critical for programs targeting multiple risk factors.
In regards to psychopathology outcomes, no effect of the intervention was observed in terms of panic or other anxiety-related psychopathology symptoms by the six-month follow-up assessment. This pattern of findings appears due to the fact that there was relatively little change in these outcomes across groups during this short follow-up period.
Two general points of consideration warrant comment. First, the current study demonstrated the feasibility of targeting two panic-relevant independent risk factors concurrently. At the same time, it appears the intervention had a significant effect on AS, but the PIAS did not result in lasting effects on smoking behavior. Thus, an increased focus on smoking reduction, perhaps via a larger intervention dose (e.g., via added booster sessions consisting of smoking cessation counseling), appears necessary to produce long term changes in smoking behavior among high AS smokers. Second, consistent with relevant risk factor research, the current study selected daily smokers who are high in AS. However, a burgeoning literature in the area of AS is focused on identifying a class of persons at particular risk for panic as a function of being in a taxonic class of AS (e.g., Bernstein, Leen-Feldner, Kotov, Schmidt, & Zvolensky, 2006; Schmidt, Kotov, Lerew, Joiner, & Ialongo, 2005). Similarly, heavier smokers than those in the current study may be at greater risk for panic problems. Further research into the degree of risk imparted at varying degrees of each risk factor is needed to further refine selection of participants.
Several limitations regarding interpretation of the current findings should be considered. First, due to the nature of this short-term efficacy trial, a follow-up period was utilized that did not allow sufficient time for psychopathology to develop, prohibiting conclusions regarding the ultimate preventive effects of the PIAS on panic development. Second, intervention fidelity and participants’ follow through with homework (e.g., independent practice of exposure exercises) was not monitored. Third, the current study relied exclusively on self-report measures. Inclusion of a panic-relevant biological challenge (e.g., voluntary hyperventilation) to index sensitivity and reactivity to interoceptive arousal, both pre-group and at the six-month follow-up, would substantiate our assessment of participants’ sensitivity to anxious states. Fourth, random assignment resulted in group differences. Specifically, there were more women in the control group, which co-occurred with higher screening levels of AS. While these differences may be interpreted as a conservative bias because participants in the control group were theoretically at greater risk for developing panic problems, future investigations may benefit from matching groups in terms of gender. Fifth, we employed the screening portion of the SCID-NP at the outset of the study and then measured anxiety psychopathology with the anxiety-focused ADIS-IV at the conclusion of the study. While both of these interviews are well established, future studies should utilize the same interviews throughout the project to increase confidence in any change documented via clinical interviews. Finally, participant attrition in the current study was relatively high (36%). Improving participant retention would increase confidence in the generalizability of follow-up assessments to the sample studied and ultimately increase methodological power for detecting intervention effects on distal outcomes in larger scale trials.
Overall, the current study contributes significantly to the literature on anxiety prevention by applying conceptual models of anxiety-drug comorbidity to a novel integrative panic prevention program. Moreover, this was the first study to demonstrate the feasibility of concurrently targeting distinct psychological and drug-related risk factors implicated in the development of a specific type of anxiety psychopathology. This study suggests that conducting such an intervention in a group format is feasible. Although several studies are needed prior to testing this approach in large scale trials, this study hopefully will lay the groundwork for such programs of research.
Acknowledgments
The authors thank Mark Bouton, Ph.D., Laura Solomon, Ph.D., Laura Gibson, Ph.D., Meggan Buccossi, B.A., and Matthew Stattel, B.A., for their assistance with this project. This project also was supported, in part, by a National Research Service Award (F31 MH66430) and Centers for Disease Control and Prevention grant (U49 CE001248) awarded to Dr. Feldner, National Institute on Drug Abuse research grants (R01 MH076629, R01 DA018734, and R03 DA16307) awarded to Dr. Zvolensky, a National Research Service Award (F31 MH081402) awarded to Kimberly Babson, and a National Institutes of Health grant (R03 MH077692) awarded to Dr. Leen-Feldner. Data for the present study were collected in the Anxiety and Health Research Laboratory at the University of Vermont.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Consistent with recommendations (Cohen et al., 2003), each of these growth curve models also was examined with an intraclass correlation coefficient as well as the two (e.g., time × gender) and three way interaction terms (e.g., time × group × gender) included as covariates. Including these covariates did not change the pattern of findings.
The equation used to examine ASI data over time, which more broadly illustrates the type of equations used, was as follows: proc mixed covtest data=perm.panicpreventionwithrecodedtime; class subject_; model ASI_across_time=timerecoded grp_numb gender Pre_ASI group group*timerecoded/solution ddfm=bw; random intercept timerecoded/subject=subject_ type=un gcorr
References
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Leen-Feldner EW, Kotov R, Schmidt NB, Zvolensky MJ. A test of a panic-relevant diathesis-stress model using a taxonic index of anxiety sensitivity. In: Sanfelippo AJ, editor. Panic Disorders: New Research. Hauppauge, NY: Nova Science Publishing; 2006. pp. 15–40. [Google Scholar]
- Bernstein A, Zvolensky MJ, Schmidt NB, Sachs-Ericsson N. Developmental course(s) of lifetime cigarette use and panic attack comorbidity: An equifinal phenomenon? Behavior Modification. 2007;31:117–135. doi: 10.1177/0145445506295056. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kilbey M, Andreski P. Nicotine dependence, major depression, and anxiety in young adults. Archives of General Psychiatry. 1991;48:1069–1074. doi: 10.1001/archpsyc.1991.01810360033005. [DOI] [PubMed] [Google Scholar]
- Breslau N, Klein DF. Smoking and panic attacks: An epidemiologic investigation. Archives of General Psychiatry. 1999;56:1141–1147. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychological Medicine. 2004;34:323–333. doi: 10.1017/s0033291703008869. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive Behaviors. 2001;26:887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111:180–185. [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Jasin SE, Gracely EJ, Williams C. The Mobility Inventory for agoraphobia. Behaviour Research and Therapy. 1985;23:35–44. doi: 10.1016/0005-7967(85)90140-8. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd (Edition) Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Craske MG, Barlow DH. Mastery of your anxiety and panic. 3rd Ed. Albany, NY: Graywind Publications; 2000. [Google Scholar]
- Craske MG, Rachman SJ, Tallman K. Mobility, cognitions, and panic. Journal of Psychopathology & Behavioral Assessment. 1986;8:199–210. [Google Scholar]
- Craske MG, Zucker BG. Prevention of anxiety disorders: A model for intervention. Applied & Preventive Psychology. 2001;10:155–175. [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. The Anxiety Disorders Interview Schedule for DSM-IV. Albany, NY: Graywind Publications; 1994. [Google Scholar]
- Di Nardo PA, Moras K, Barlow DH, Rapee RM, Brown TA. Reliability of DSM-III-R anxiety disorder categories using the Anxiety Disorders Interview Schedule – Revised (ADIS-R) Archives of General Psychiatry. 1993;50:251–256. doi: 10.1001/archpsyc.1993.01820160009001. [DOI] [PubMed] [Google Scholar]
- Donnell CD, McNally RJ. Anxiety sensitivity and panic attacks in a nonclinical population. Behaviour Research and Therapy. 1990;28:83–85. doi: 10.1016/0005-7967(90)90058-q. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Dobson KS, editors. The prevention of anxiety and depression: Theory research and practice. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Ehlers A. A 1-year prospective study of panic attacks: Clinical course and factors associated with maintenance. Journal of Abnormal Psychology. 1995;104:164–172. doi: 10.1037//0021-843x.104.1.164. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, Zvolensky MJ, Monson CM, Bonn-Miller MO, Gibson LE. An examination of anxiety sensitivity as a moderator of the relationship between smoking level and posttraumatic stress symptoms among trauma-exposed adults. Cognitive Therapy and Research. (in press) [Google Scholar]
- Feldner MT, Zvolensky MJ, Schmidt NB. Prevention of anxiety psychopathology: A critical review of the empirical literature. Clinical Psychology: Science and Practice. 2004;11:405–424. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - Non-Patient Edition. New York: New York State Psychiatric Institute; 1995. [Google Scholar]
- Gardenswartz CA, Craske MG. Prevention of panic disorder. Behavior Therapy. 2001;32:725–737. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS. Anxiety prevention programs for youth: Practical and theoretical considerations. Clinical Psychology: Practice and Science. 2004;11:430–434. [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JRT, Ballenger JC, Fuyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Gregor K, Zvolensky MJ, McLeish AC, Bernstein A, Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: Associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine and Tobacco Research. doi: 10.1080/14622200801978706. (in press) [DOI] [PubMed] [Google Scholar]
- Haynes SN, Lench HC. Incremental validity of new assessment measures. Psychological Assessment. 2003;15:456–466. doi: 10.1037/1040-3590.15.4.456. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:207–214. doi: 10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- Isensee B, Wittchen H, Stein MB, Hofler M, Lieb R. Smoking increases the risk of panic: Findings from a prospective community study. Archives of General Psychiatry. 2003;60:692–700. doi: 10.1001/archpsyc.60.7.692. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, Brook JS. Association between cigarette smoking and anxiety disorders during adolescence and early adulthood. Journal of the American Medical Association. 2000;284:2348–2351. doi: 10.1001/jama.284.18.2348. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Bethesda, MD: National Institute on Drug Abuse; Monitoring the Future national survey results on drug use, 1975–2003. Volume I: Secondary school students (NIH Publication No. 04-5507) 2004
- Juliano LM, Brandon TH. Effects of nicotine dose, instructional set, and outcome expectancies on the subjective effects of smoking in the presence of a stressor. Journal of Abnormal Psychology. 2002;111:88–97. doi: 10.1037//0021-843x.111.1.88. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Unrod M. Smoking, anxiety, and attention: Support for the role of nicotine in attentionally mediated anxiolysis. Journal of Abnormal Psychology. 2000;109:161–166. doi: 10.1037//0021-843x.109.1.161. [DOI] [PubMed] [Google Scholar]
- Kotov R, Schmidt NB, Zvolensky MJ, Vinogradov A, Antipova AV. Adaptation of panic-related psychopathology measures to Russian. Psychological Assessment. 2005;17:242–246. doi: 10.1037/1040-3590.17.2.242. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Erikson DJ. Prospective analysis of the relation between DSM-IV anxiety disorders and alcohol use disorders. American Journal of Psychiatry. 1999;156:723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Vujanovic A, Bernstein A. Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: Replication and extension. Nicotine and Tobacco Research. doi: 10.1080/14622200802097555. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- Lowry-Webster HM, Barrett PM, Lock S. A universal prevention trial of anxiety symptomatology during childhood: Results at 1-year follow-up. Behaviour Change. 2003;20:25–43. [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6:241–247. [Google Scholar]
- McLeish AC, Zvolensky MJ, Bucossi MM. Interaction between smoking rate and anxiety sensitivity: Relation to anticipatory anxiety and panic-relevant avoidance among daily smokers. Journal of Anxiety Disorders. 2007;21:849–859. doi: 10.1016/j.janxdis.2006.11.003. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Mrazek PJ, Haggerty RJ. Reducing risks for mental disorders: Frontiers for preventive intervention research. Washington, DC, US: National Academy Press; National Academy of Sciences, Institute of Medicine. 1994 [PubMed]
- Muthén BO, Curran PJ. General longitudinal modeling of individual differences in experimental designs: A latent variable framework for analysis and power estimation. Psychological Methods. 1997;2:371–402. [Google Scholar]
- National Advisory Mental Health Council Workgroup on Mental Disorders Prevention Research. Bethesda, MD: National Institutes of Health/National Institute of Mental Health; Priorities for prevention research at NIMH. 1998
- Otto MW. Learning and "unlearning" fears: Preparedness, neural pathways, and patients. Biological Psychiatry. 2002;52:917–920. doi: 10.1016/s0006-3223(02)01719-5. [DOI] [PubMed] [Google Scholar]
- Parrott A. Does cigarette smoking cause stress? American Psychologist. 1999;18:817–820. doi: 10.1037//0003-066x.54.10.817. [DOI] [PubMed] [Google Scholar]
- Peterson RA, Reiss S. Anxiety Sensitivity Index Manual. 2nd ed. Worthington, OH: International Diagnostic Systems; 1992. [Google Scholar]
- Price WA, Giannini AJ. Phencyclidine and ”crack”-precipitated panic disorder. American Journal of Psychiatry. 1987;144:686–687. doi: 10.1176/ajp.144.5.686b. [DOI] [PubMed] [Google Scholar]
- Rapee RM. The development and modification of temperamental risk for anxiety disorders: Prevention of a lifetime of anxiety? Biological Psychiatry. 2002;52:947–957. doi: 10.1016/s0006-3223(02)01572-x. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Medoro L. Fear of physical sensations and trait anxiety as mediators of the response to hyperventilation in nonclinical subjects. Journal of Abnormal Psychology. 1994;4:693–699. doi: 10.1037//0021-843x.103.4.693. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical Issues in Behavior Therapy. San Diego: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Reiss S, Peterson RA, Gursky M, McNally RJ. Anxiety, sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Rounsaville I, Bruce J, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science & Practice. 2001;8:133–142. [Google Scholar]
- Rundmo T, Smedslund G, Götestam KG. Motivation for smoking cessation among the Norwegian public. Addictive Behaviors. 1997;22:377–386. doi: 10.1016/s0306-4603(96)00056-1. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Kotov R, Lerew DR, Joiner TE, Ialongo NS. Evaluating latent discontinuity in cognitive vulnerability to panic: A taxometric investigation. Cognitive Therapy and Research. 2005;29:673–691. [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Anxiety sensitivity in the pathogenesis of panic: A prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety Sensitivity Amelioration Training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007;21:302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ. Risk factor research and prevention for anxiety disorders: Introduction to the special series on risk and prevention of anxiety pathology. Behavior Modification. 2007;31:3–7. doi: 10.1177/0145445506295059. [DOI] [PubMed] [Google Scholar]
- Sechrest L. Incremental validity: A recommendation. Educational and Psychological Measurement. 1963;23:153–158. [Google Scholar]
- Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, et al. The Psychosocial Treatments Interview for anxiety disorders: A method for assessing psychotherapeutic procedures in anxiety disorders. Journal of Psychotherapy Practice and Research. 1997;6:194–210. [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Taylor S, Baker JM. Gender differences in dimensions of anxiety sensitivity. Journal of Anxiety Disorders. 1997;11:179–200. doi: 10.1016/s0887-6185(97)00005-4. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research and treatment of the fear of anxiety. Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc.; 1999. [Google Scholar]
- Velicer WF, DiClemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: An integrative model. Addictive Behaviors. 1990;15:271–283. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss O, McCormick J. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Weems CF, Hayward C, Killen J, Taylor CB. A longitudinal investigation of anxiety sensitivity in adolescence. Journal of Abnormal Psychology. 2002;111:471–477. [PubMed] [Google Scholar]
- Zinbarg RE, Mohlman J, Hong NN. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Erlbaum; 1999. Dimensions of anxiety sensitivity; pp. 83–114. [Google Scholar]
- Zvolensky MJ, Baker KM, Leen-Feldner EW, Bonn-Miller MO, Feldner MT, Brown RA. Anxiety sensitivity: Association with intensity of retrospectively-rated smoking-related withdrawal symptoms and motivation to quit. Cognitive Behaviour Therapy. 2004;33:114–125. doi: 10.1080/16506070310016969. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Current Directions in Psychological Science. 2005;14:301–305. [Google Scholar]
- Zvolensky MJ, Bernstein A, Sachs-Ericcson N, Schmidt NB, Buckner J, Bonn-Miller MO. Cannabis use, abuse, and dependence and panic attacks in a representative sample. Journal of Psychiatric Research. 2006;40:477–486. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Yartz AR, McLeish A, Feldner MT. Cognitive-behavioral treatment of comorbid panic psychopathology and tobacco use and dependence. In: Stewart SH, Conrad P, editors. Comorbidity of anxiety and substance use disorders. New York: Springer; 2008. pp. 177–200. [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Bernstein A, Marshall EC. Anxiety sensitivity and abstinence duration to smoking. Journal of Mental Health. 2006;15:659–670. [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Feldner MT, Leen-Feldner E, McLeish AC, Gregor K. Anxiety sensitivity: Concurrent association with negative affect smoking motives and abstinence self-confidence among young adult smokers. Addictive Behaviors. 2006;31:429–439. doi: 10.1016/j.addbeh.2005.05.027. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Eifert GH, Brown RA. Affective style among smokers: Understanding anxiety sensitivity, emotional reactivity, and distress tolerance using biological challenge. Addictive Behaviors. 2001;26:901–915. doi: 10.1016/s0306-4603(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, Gregor K. Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research. 2004;28:473–486. [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner EW, Gibson LE, Abrams K, Gregor K. Acute nicotine withdrawal symptoms and anxious responding to bodily sensations: A test of incremental predictive validity among young adult smokers. Behaviour Research and Therapy. 2005;43:1683–1700. doi: 10.1016/j.brat.2004.10.010. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner EW, McLeish AC. Smoking and panic attacks, panic disorder, & agoraphobia: A review of the empirical literature. Clinical Psychology Review. 2005;25:761–789. doi: 10.1016/j.cpr.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Forsyth JP, Fuse T, Feldner MT, Leen-Feldner EW. Panic attacks and smoking: An initial investigation of panic-relevant cognitive processes. Cognitive Behaviour Therapy. 2002;31:170–182. [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Leen-Feldner EW, Schmidt NB. Evaluating anxiety sensitivity, exposure to aversive life conditions, and problematic drinking in Russia: A test using an epidemiological sample. Addictive Behaviors. 2005;30:567–570. doi: 10.1016/j.addbeh.2004.05.025. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Diathesis-Stress model for panic-related distress: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2005;43:521–532. doi: 10.1016/j.brat.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Cross cultural evaluation of smokers risk for panic and anxiety pathology: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2003;41:1199–1215. doi: 10.1016/s0005-7967(03)00031-7. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Leen-Feldner EW, Feldner MT, Bonn-Miller MO, Lejuez CW, Kahler CW, Stuart G. Emotional responding to biological challenge as a function of panic disorder and smoking. Journal of Anxiety Disorders. 2004;18:19–32. doi: 10.1016/j.janxdis.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Panic attack history and smoking cessation: An initial examination. Addictive Behaviors. 2004;29:825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lewinsohn P, Bernstein A, Schmidt NB, Buckner JD, Seeley J, Bonn-Miller MO. Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. Journal of Psychiatric Research. doi: 10.1016/j.jpsychires.2007.10.012. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Sachs-Ericsson N, Feldner MT, Schmidt NB, Bowman C. Neuroticism moderates the effect of maximum smoking level on lifetime panic disorder: A test using an epidemiologically defined national sample of smokers. Psychiatry Research. 2006;141:321–332. doi: 10.1016/j.psychres.2005.07.019. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, Bernstein A, Keough ME. Risk factor research and prevention programs for anxiety disorders: A translational research framework. Behaviour Research and Therapy. 2006;44:1219–1239. doi: 10.1016/j.brat.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky M, Schmidt N, McCreary B. The impact of smoking on panic: An initial investigation of a pathoplastic relationship. Journal of Anxiety Disorders. 2003;17:447–460. doi: 10.1016/s0887-6185(02)00222-0. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, Stewart SH. Panic disorder and smoking. Clinical Psychology: Science and Practice. 2003;10:29–51. [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bonn-Miller MO, Bernstein A, Yartz AR, Gregor KL, McLeish AC, Marshall EC, Gibson LE. Incremental validity of anxiety sensitivity in terms of motivation to quit, reasons for quitting, and barriers to quitting among community-recruited daily smokers. Nicotine and Tobacco Research. 2007;9:965–975. doi: 10.1080/14622200701540812. [DOI] [PubMed] [Google Scholar]