Abstract
Traumatic brainstem hemorrhage after blunt head injury is an uncommon event. The most frequent site of hemorrhage is the midline rostral brainstem. The prognosis of these patients is poor because of its critical location. We experienced a case of traumatic brainstem hemorrhage. A 41-year-old male was presented with drowsy mentality and right hemiparesis after blunt head injury. Plain skull radiographs and brain computerized tomography scans revealed a depressed skull fracture, epidural hematoma, and hemorrhagic contusion in the right parieto-occipital region. But, these findings did not explain the right hemiparesis. T2-weighted magnetic resonance (MR) image of the cervical spine demonstrated a focal hyperintense lesion in the left pontomedullary junction. Brain diffusion-weighted and FLAIR MR images showed a focal hyperintensity in the ventral pontomedullary lesion and it was more prominent in the left side. His mentality and weakness were progressively improved with conservative treatment. We should keep in mind the possibility of brainstem hemorrhage if supratentorial lesions or spinal cord lesions that caused neurological deficits in the head injured patients are unexplainable.
Keywords: Brain stem hemorrhage, Head trauma, Hemiparesis
INTRODUCTION
Traumatic brain injury can result from a closed head injury or a penetrating head injury. The damage from traumatic brain injury can be focal or diffuse. Diffused trauma to the brain is frequently associated with concussion, diffuse axonal injury. Focal injury of brain is consists of epidural hematoma, subdural hematoma, and subarachnoid hemorrhage. But, brainstem hemorrhage after blunt head injury is a rare event. It occurs in 0.75%-3.6% of all patients admitted to hospital with head injury5,12,16,17). The prognosis of these patients is dismal because of its critical location. Previous studies have shown that the mortality of this patients ranged from 67% to 83%1,12,17).
We experienced a case with brainstem hemorrhage in the pontomedullary junction after blunt head injury. In this case, we describe this uncommon case with good recovery in mental status and right hemiparesis, and discuss clinical characteristics of brainstem hemorrhage.
CASE REPORT
A 41-year-old man was presented with drowsy mentality and right hemiparesis (grade I/V) after a motorcycle accident rammed by another vehicle. His mental status was graded as a Glasgow coma scale (GCS) score of 14. His pupils were equal in size and reactive to light. Sensory and motor function in his left extremities was undamaged. However, motor function was weak in right sided extremities. Other neurological examination didn't reveal any abnormal findings.
Plain skull radiographs showed a depressed fracture in the right parietal bone. Brain computerized tomography (CT) scans also revealed an epidural hematoma, depressed fracture, and hemorrhagic contusion in the right parieto-occipital area (Fig. 1). But these supratentorial lesions didn't represent paresis of left sided extremities. Cervical magnetic resonance (MR) image was taken to evaluate the right side weakness. Sagittal T2-weighted MR image of the cervical spine demonstrated a focal hyperintense lesion in the left pontomedullary junction (Fig. 2A). Brain diffusion-weighted and fluid-attenuated inversion recovery (FLAIR) MR images also showed a focal high signal intensity in the upper medulla (Fig. 2B), lower pons (Fig. 2C), and pontomedullary junction (Fig. 2D). It was more prominent in the left side.
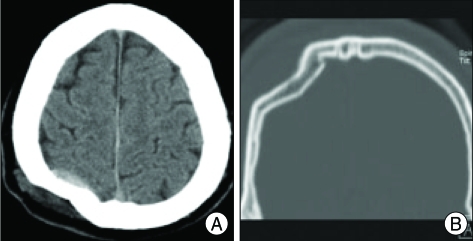
Fig. 1.
Axial (A) and coronal (B) brain computerized tomographic scans showing the depressed fracture, epidural hematoma, and hemorrhagic contusion in the parieto-occipital area. But any lesions responsible for hemiparesis are not seen in the motor cortex or premotor area.
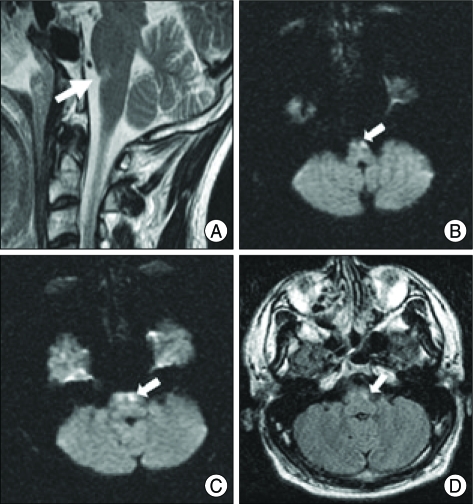
Fig. 2.
A : Sagittal T2-weighted magnetic resonance (MR) image of the cervical spine showing focal high signal intensity in the left lower pons (arrow). B : Axial diffusion-weighted MR image obtained at the 2nd hospital day after injury. MR images demonstrated a focal hyperintensity of the ventral upper medulla (arrow), more prominent in the left side. C : Axial diffusion-weighted MR displaying a focal hyperintensity in the lower pontine lesion (arrow). D : Axial fluid-attenuated inversion recovery MR image showing a focal hyperintensity in the ventral pontomedullary junction.
The patient was treated conservatively in the intensive care unit. On the 2nd hospital day, his mentality was recovered to be alert, but his weakness did not improve. Right side motor weakness was also improved (grade III/V) 3 weeks later. Two months later, he was discharged with mild motor weakness (grade IV/V).
DISCUSSION
Traumatic brainstem hemorrhage is an uncommon finding in patients with blunt head injury. Traumatic brainstem hemorrhage typically results in coma, decerebrate posturing, and autonomic nervous system dysfunction12). It is commonly believed that brainstem hemorrhage is associated with the worst prognosis. Previous studies have indicated mortality rates of 83%, with up to one-half of the surviving patients remained in a persistent vegetative state17).
Two types of traumatic brainstem hemorrhage have been reported6,12,13,15). Primary type is the result of direct mechanical distortion of the brain stem. Secondary type results from diffuse cerebral edema, hypoxia, posttraumatic vasospasm, and transtentorial herniation10,12). Meyer CA et al.12) reported that the most frequent site of hemorrhage, in 31 (69%) of 45 patients, was the ventral rostral midbrain adjacent to the interpeduncular cistern. Disruption of axonal tracts in the brainstem injured patients occurs as part of the widespread white matter damage. This lesion often coexists with other brain lesions such as acute epidural hematoma, acute subdural hematoma, and hemorrhagic contusion. Neurological deficits of the affected patients are usually considerable, and thus subsumed in the category of those with severe brainstem injuries3,7). In some cases, however, an isolated type without supratentorial lesions has been described with unexpectedly good recovery7,12). In our case, a brain CT scans and MR images of the cervical spine showed a brainstem hemorrhage and supratentorial lesions including epidural hematoma, hemorrhagic contusion, and depressed skull fracture.
The mechanism of injury can be hypothesized considering the dynamics of trauma : tearing or maximally stretched vessels arising from the basal artery seems to play a relevant role. Ropper and Miller13) proposed three mechanisms to cause traumatic brainstem hemorrhage. Brainstem hemorrhage can be caused by primary lesion resulting from either rotational forces, or from transient acceleration-deceleration forces that cause contusion against the tentorium, or secondary to the brainstem compression. However, it is uncertain to define the exact one mechanism because of conflicting neuropathological evidences in brainstem hemorrhage. Some authors described it as a discrete entity attributable to the hyperextension injury of patients who have sustained an impact on the forehead along the rostrocaudal axis7,12,14). Others have been advocate the acceleration-deceleration injury model in a sagittal plane as the most frequent cause of traumatic brainstem hemorrhage2,4,11). On the other hands, the distinction between primary and secondary injuries is indefinite. In our case, the evidence of tissue compaction against the tentorium and brainstem compression was not seen. These findings indicated that brainstem hemorrhage in the present case was caused by primary mechanism resulting from either rotational forces or transient acceleration-deceleration forces.
Brain MR imaging remains to be the modality of choice for the recognition of brainstem hemorrhage in patients with traumatic head injury. Several recent studies using diffusion MR have mainly focused on hyperacute and acute hemorrhages9). Diffusion MR imaging shows the hematoma as hyperintense. In the respect of diagnostic value of brain CT scans, the previous literatures have emphasized the limitations of CT scans to diagnose the brain stem hemorrhage because one-third of these patients showed the findings of false-negative scans8). Some authors have supposed that there were several lesions to be required a contrast infusion for visualization of hemorrhages, but there was difficulty in distinguishing such primary lesions from damage due to herniation and brainstem compression2,16).
It is commonly believed that brainstem hemorrhage is associated with the worst prognosis. However, our case revealed a good outcome including improvement of mental status and right hemiparesis after conservative treatment. We believe that these favorable results are due to the relatively good neurological conditions on the admission and a small amount of hemorrhage measured about 1 mL.
CONCLUSION
The authors report an unusual case with brainstem hemorrhage after blunt head injury. If the supratentorial lesion or spinal cord lesion is unexplainable for neurological deficits, we should keep in mind the possibility of brainstem hemorrhage, and MR imaging should be performed to evaluate such lesion.
References
- 1.Cooper PR, Maravilla K, Kirkpatrick J, Moody SF, Sklar HF, Diehl J, et al. Traumatically induced brain stem hemorrhage and the computerized tomographic scan : clinical, pathological, and experimental observations. Neurosurgery. 1979;4:115–124. doi: 10.1227/00006123-197902000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Crompton MR. Brainstem lesions due to closed head injury. Lancet. 1971;1:669–673. doi: 10.1016/s0140-6736(71)92680-8. [DOI] [PubMed] [Google Scholar]
- 3.Firsching R, Woischneck D, Klein S, Ludwig K, Dohring W. Brainstem lesions after head injury. Neurol Res. 2002;24:145–146. doi: 10.1179/016164102101199684. [DOI] [PubMed] [Google Scholar]
- 4.Freytag E. Autopsy findings in head injuries from blunt forces. Statistical evaluation of 1,367 cases. Arch Pathol. 1963;75:402–413. [PubMed] [Google Scholar]
- 5.Gentry LR, Godersky JC, Thompson B. MR imaging of head trauma : review of the distribution and radiopathologic features of traumatic lesions. AJR Am J Roentgenol. 1988;150:663–672. doi: 10.2214/ajr.150.3.663. [DOI] [PubMed] [Google Scholar]
- 6.Goscinski I, Kwaitkowski S, Cichonski J, Moskala M. Posttraumatic primary brainstem haematoma. Acta Neurochir (Wien) 1995;134:16–20. doi: 10.1007/BF01428496. [DOI] [PubMed] [Google Scholar]
- 7.Hashimoto T, Nakamura N, Richard KE, Frowein RA. Primary brain stem lesions caused by closed head injuries. Neurosurg Rev. 1993;16:291–298. doi: 10.1007/BF00383839. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs L, Kinkel WR, Heffner RR., Jr Autopsy correlation of computerized tomography : experience with 6,000 CT scans. Neurology. 1976;26:1111–1118. doi: 10.1212/wnl.26.12.1111. [DOI] [PubMed] [Google Scholar]
- 9.Kang BK, Na DG, Ryoo JW, Byun HS, Roh HG, Pyeun YS. Diffusion-weighted MR imaging of intracerebral hemorrhage. Korean J Radiol. 2001;2:183–191. doi: 10.3348/kjr.2001.2.4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klintworgh GK. The pathogenesis of secondary brainstem hemorrhages as studied in an experimental model. Am J Pathol. 1965;47:525–536. [PMC free article] [PubMed] [Google Scholar]
- 11.Lindenberg R. Significance of the tentorium in head injuries from blunt forces. Clin Neurosurg. 1966;12:129–142. doi: 10.1093/neurosurgery/12.cn_suppl_1.129. [DOI] [PubMed] [Google Scholar]
- 12.Meyer CA, Mirvis SE, Wolf AL, Thompson RK, Gutierrez MA. Acute traumatic midbrain hemorrhage : experimental and clinical observations with CT. Radiology. 1991;179:813–818. doi: 10.1148/radiology.179.3.2027997. [DOI] [PubMed] [Google Scholar]
- 13.Ropper AH, Miller DC. Acute traumatic midbrain hemorrhage. Ann Neurol. 1985;18:80–86. doi: 10.1002/ana.410180114. [DOI] [PubMed] [Google Scholar]
- 14.Sganzerla EP, Rampini PM, De Santis A, Tiberio F, Guerra P, Zavanone M, et al. Primary traumatic benign midbrain haematoma in hyperextension injuries of the head. Acta Neurochir Suppl(Wien) 1992;55:29–32. doi: 10.1007/978-3-7091-9233-7_9. [DOI] [PubMed] [Google Scholar]
- 15.Tandon PN. Brainstem hemorrhage in cranio-cerebral trauma. Acta Neurol Scand. 1964;40:375–385. doi: 10.1111/j.1600-0404.1964.tb02762.x. [DOI] [PubMed] [Google Scholar]
- 16.Tsai FY, Teal JS, Quinn MF, Itabashi HH, Huprich JE, Ahmadi J, et al. CT of brainstem injury. AJR Am J Roentgenol. 1980;134:717–723. doi: 10.2214/ajr.134.4.717. [DOI] [PubMed] [Google Scholar]
- 17.Zuccarello M, Fiore DL, Trincia G, De Caro R, Pardatscher K, Andrioli GC. Traumatic primary brain stem haemorrhage : a clinical and experimental study. Acta Neurochir (Wien) 1983;67:103–113. doi: 10.1007/BF01401670. [DOI] [PubMed] [Google Scholar]