Abstract
Ewing's sarcoma usually arises from skeletal bone, but rarely may have an extraskeletal origin. However, Ewing's sarcoma that originates around the spinal column, especially, the intradural extramedullary type is extremely rare. We report a rare case of primary intraspinal extraskeletal Ewing's sarcoma.
Keywords: Extraskeletal Ewing's sarcoma, Intradural extramedullary type
INTRODUCTION
Ewing's sarcoma, which was described for the first time as an osteolytic lesion by James Ewing in 19211), is a malignant, small, round-cell tumor of the bone. Extraskeletal Ewing's sarcoma, the extraosseous form of Ewing's sarcoma, was first described by Tefft in 196910). It is a rare malignant neoplasm of uncharacterized mesenchymal cell origin that is histologically similar to primary osseous Ewing's sarcoma. The most frequent sites of extraskeletal Ewing's sarcoma are the chest wall, lower extremities, and the trunk7,8). However, these tumors rarely originate around the spinal column and when they do, they are referred to as epidural Ewing's sarcoma. We report a very rare case of an intradural dumbbell shaped extraskeletal Ewing's sarcoma with a review of the medical literature.
CASE REPORT
A 32-year-old woman was admitted via emergency unit with one day history of progressive paresis of the upper extremities. She had a 6-week history of pain and numbness of the upper extremities. There was no urinary retention. The motor strength of the upper extremities was Grade III/Grade I. The magnetic resonance imaging (MRI) confirmed the presence of an intradural extramedullary dumbbell shaped tumor at the C3-C5 level compressing the spinal cord and displacing it to the right side. The T1-weighted and enhanced MRI images showed that the tumor was largely isointense and enhanced homogeneously with gadolinium (Fig. 1). However, the computed tomography (CT) scan showed no osteolytic or osteosclerotic changes in the vertebral bones. Surgery was performed by a posterior laminectomy at the C3-C5 level. A subtotal resection of the tumor, following durotomy, was carried out. The tumor was located in the intradural, extramedullary space and adhered to the arachnoid membrane and posterior nerve roots. The histological examination revealed diffuse proliferation of undifferentiated tumor cells with round to polygonal nuclei and scant cytoplasm (Fig. 2). Neuroblastic (Homer Wright type) rosettes were not present but mitotic figures were occasionally seen. Massive necrosis and hemorrhage were present in some areas. No appreciable glycogen was identified in the tumor cells by the periodic acid-Schiff (PAS) reaction. After tumor extirpation, the patient was treated with multiagent chemotherapy with Etoposide and lfosfamide combined with 30 Gy of radiotherapy. The paresis of upper extremities was improved (Grade IV/Grade IV) after the operation. The patient remains alive and continues to be disease free 12 months after the operation.
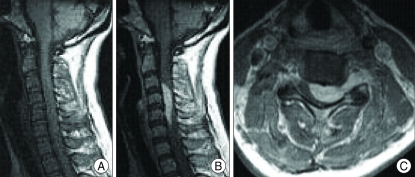
Fig. 1.
A : T1-weighted magnetic resonance image shows an isointense tumor. B and C : Gadolinium enhanced sagittal and axial magnetic resonance images show a homogeneously enhanced large dumbbell tumor at C3-C5 level.
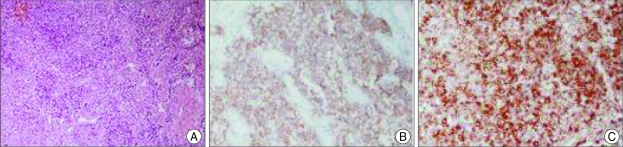
Fig. 2.
Photomicrographs of the resected tumor. A : Microscopically, this tumor is composed of uniform small round cells that are slightly larger than lymphocytes. The tumor cells have scant cytoplasm, although some cells appear clear due to abundant glycogen. There are focal necrotic areas revealing weak nuclear basophilia (×40). B and C : Immunohistochemically, the tumor cells show immunoreactivity for CD 99 and Vimentin. These morphologic and immunohistochemical features are consistent with the diagnosis of Ewing's sarcoma (×100).
DISCUSSION
Ewing's sarcoma is a highly undifferentiated tumor; it is generally found in children and young adults and usually develops in the skeleton. Ewing's sarcoma is rare and usually occurs in the long bones and pelvis; the spinal column is the affected site in only 3.5-7% of cases. Spinal Ewing's sarcomas most often are located at the side of a vertebral body9,11). Typical radiographic features include varying degrees of osteolytic or osteosclerotic changes of the vertebral body5). In the present case, the tumor was located in the intradural and extramedullary space, extending into the vertebral foramen. No osteolytic or osteosclerotic changes were noted on the CT or intraoperatively. Magnetic resonance imaging, especially the contrast-enhanced spinal MRI, is most useful for early diagnosis of tumors around the spinal column. Although MRI is nonspecific for determining the histology of malignant tumors, it is useful for determining the extent of local involvement with the surrounding structures4). After the tumor is delineated on MRI, laminectomy with tumor resection is necessary for the relief of neurological symptoms and for histopathological examination and diagnosis. Despite the histopathological disagreements concerning the possible differences between skeletal and extraskeletal Ewing's sarcoma, no histological differences are generally recognized6,8). Cytogenetic alterations such as the chromosomal translocation [t (11;22) (q24;q12); (EWS-FLT1)], as well as strong MIC2 expression have been shown to occur commonly in both Ewing's sarcomas and primitive peripheral neuroectodermal tumors. Since no skeletal involvement was demonstrable in the present case, the spinal root was considered the origin of this primitive tumor. The 5-year survival rate of extraskeletal Ewing's sarcoma has been reported to be between 38% and 67%. However, the clinical outcomes of extraskeletal Ewing's sarcoma around the spinal column are very poor, even with both chemotherapy and radiotherapy2). The 5-year survival rate in extraskeletal Ewing's sarcoma of the spinal canal has been reported to be between 0% and 37.5%3). This poor prognosis may result from the high rate of partial resections of the tumors. Partially resected tumors are associated with a greater incidence of local recurrence and a higher mortality. Therefore, it is important to remove as much of the tumor as possible. In view of the late relapses that have been reported in patients with extraskeletal Ewing's sarcoma, a longer follow-up and larger series are both required to improve our understanding of the natural history of this disease.
CONCLUSION
Although extraskeletal Ewing's sarcoma that originates around the spinal column is very rare, this case illustrates that Ewing's sarcoma should be considered in the differential diagnoses of intradural tumors of the spinal cord. Aggressive treatment with multiagent chemotherapy combined with en bloc resection and radiation therapy are the preferred treatment in confirmed cases.
References
- 1.Ewing J. Diffuse endothelioma of bone. Proc NY Pathol Soc. 1921;21:17–24. [Google Scholar]
- 2.Harimaya K, Oda Y, Matsuda S, Tanaka K, Chuman H, Iwamoto Y. Primitive neuroectodermal tumor and extraskeletal Ewing sarcoma arising primarily around the spinal column : report of four cases and a review of the literature. Spine. 2003;28:E408–E412. doi: 10.1097/01.BRS.0000085099.47800.DF. [DOI] [PubMed] [Google Scholar]
- 3.Kaspers GJ, Kamphorst W, van de Graaff M, van Alphen HA, Veerman AJ. Primary spinal epidural extraosseous Ewing's sarcoma. Cancer. 1991;68:648–654. doi: 10.1002/1097-0142(19910801)68:3<648::aid-cncr2820680335>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy JG, Eustace S, Caulfield R, Fennelly DJ, Hurson B, O'Rourke KS. Extraskeletal Ewing's sarcoma : a case report and review of the literature. Spine. 2000;25:1996–1999. doi: 10.1097/00007632-200008010-00022. [DOI] [PubMed] [Google Scholar]
- 5.Murphey MD, Andrews CL, Flemming DJ, Temple HT, Smith WS, Smirniotopoulos JG. From the archives of the AFIP. Primary tumors of the spine: radiologic pathologic correlation. Radiographics. 1996;16:1131–1158. doi: 10.1148/radiographics.16.5.8888395. [DOI] [PubMed] [Google Scholar]
- 6.Rose JS, Hermann G, Mendelson DS, Ambinder EP. Extraskeletal Ewing sarcoma with computed tomography correlation. Skeletal Radiol. 1983;9:234–237. doi: 10.1007/BF00354123. [DOI] [PubMed] [Google Scholar]
- 7.Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA. Extraosseous Ewing's sarcoma. A study of 42 cases. Cancer. 1989;64:1548–1553. doi: 10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 8.Shimada H, Newton WA, Jr, Soule EH, Qualman SJ, Aoyama C, Maurer HM. Pathologic features of extraosseous Ewing's sarcoma : a report from the Intergroup Rhabdomyosarcoma Study. Hum Pathol. 1988;19:442–453. doi: 10.1016/s0046-8177(88)80495-7. [DOI] [PubMed] [Google Scholar]
- 9.Simonati A, Vio M, Iannucci AM, Bricolo A, Rizzuto N. Lumbar epidural Ewing sarcoma. Light and electron microscopic investigation. J Neurol. 1981;225:67–72. doi: 10.1007/BF00313464. [DOI] [PubMed] [Google Scholar]
- 10.Tefft M, Vawter GF, Mitus A. Paravertebral "round cell" tumors in children. Radiology. 1969;92:1501–1509. doi: 10.1148/92.7.1501. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein JB, Siegel MJ, Griffith RC. Spinal Ewing sarcoma : misleading appearances. Skeletal Radiol. 1984;11:262–265. doi: 10.1007/BF00351350. [DOI] [PubMed] [Google Scholar]