Abstract
We present a case of an acute psoas muscle hematoma following percutaneous endoscopic lumbar discectomy. A 60-year-old female who presented with far lateral lumbar disc herniation underwent endoscopic discectomy on the right side at the L4-5 level. On the second postoperative day, the patient complained of severe right flank and leg pain and her blood pressure decreased. A computed tomography scan showed a large acute psoas muscle hematoma at right L4-5 level. The patient was transfused with packed red blood cells and placed at absolute bed rest. After observing the patient in intensive care, the severe flank and leg pain subsided, but the mild back pain persisted. Although percutaneous endoscopic lumbar discectomy is an effective minimally invasive surgical technique for the treatment of lumbar disc herniation, this case highlights the inherent risks of acute lumbar segmental vessel injury.
Keywords: Percutaneous endoscopic lumbar discectomy, Psoas muscle hematoma, Lumbar segmental vessel injury
INTRODUCTION
Percutaneous lumbar endoscopic discectomy has become a popular method for the treatment of disc herniation because it can be performed under local anesthesia and is minimally invasive. Despite the risks of vessel injury during surgery, the symptomatic complications of segmental vessel injury following percutaneous lumbar endoscopic discectomy have rarely been described. We recently experienced a large psoas muscle hematoma due to segmental vessel injury after percutaneous endoscopic discectomy.
CASE REPORT
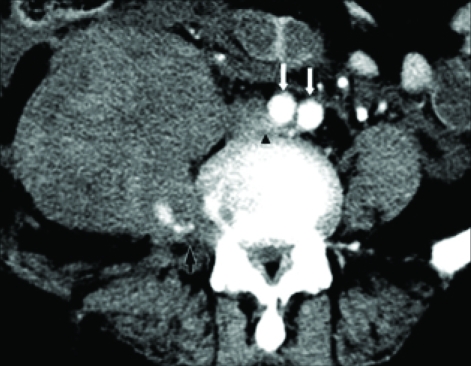
The patient, a 60-year-old female, presented with the acute onset of severe right leg radiating pain, as well as lower back pain. Examination showed pain at 60 degrees on the right side and no pain on the left side during the straight leg raising test, and reduced sensation was detectable in the L4 dermatome of the right leg. No reduction of motor power existed. Magnetic resonance imaging revealed a right, far lateral disc herniation at the L4-5 level (Fig. 1).
Fig. 1.
Transaxial T2-weighted magnetic resonance image shows a large right extraforaminal type of far lateral disc herniation (arrows) at the L4-5 level.
On the second day after admission, the patient was taken to the operating room for a percutaneous endoscopic discectomy at L4-5. During endoscopic surgery, epidural anesthesia was performed.
The order of surgery was identical to the general posterolateral procedure6-9). The patient was positioned prone on a Wilson frame. The entry site was 10 cm off the midline at the level of the pathologic disc. Under direct fluoroscopic visualization, the correct position of the 20-gauge spinal needle tip was confirmed using both anterior-posterior and lateral projections. The needle was placed parallel to the disc space, midway between the endplates, proximal to the annulus, with the tip lateral to the medial border of the pedicles. Prior to the procedure, using indigo-carmine dye, evocative chromodiscography was performed5,7). A guide wire was inserted through the needle channel into the annulus, and then a skin incision, about 1 cm in length, was made at the entry needle site. A hemostat was used to dilate a tract through the lumbodorsal fascia. The trocar was then placed through the tract adjacent and parallel to the spinal needle. The correct position of the trocar was confirmed using fluoroscopy, and the spinal needle was withdrawn. A working cannula was installed in the disc space through the transforaminal safety working zone. A rigid scope was then introduced down the cannula through the neural foramen. Disc decompression was then performed6-9). After dissecting around the space of the ruptured disc with a semi-rigid curved probe, the extruded disc material was removed with forceps, then the exiting nerve root was visible to move freely. When all the disc materials had been removed, the scope was withdrawn and the skin was sutured.
At the time the patient underwent routine examination on the 2nd day after the endoscopic discectomy, she complained of severe right flank and leg pain. The straight leg raising test showed pain at 10 degrees on the right side, as well as a limitation of hip flexion. Her vital signs were unstable and her blood pressure was 90/60 mmHg.
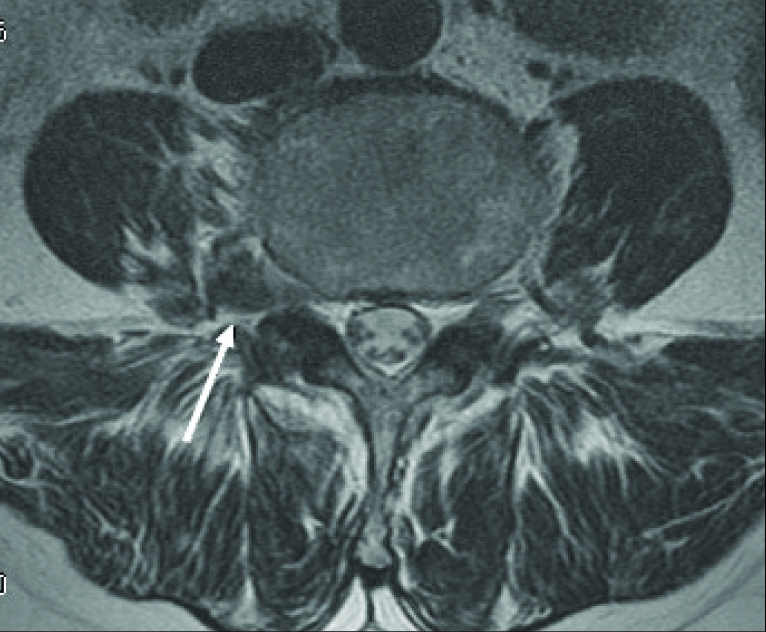
Plain X-ray films did not show any changes in the endplates around the L4/5 disc. A dynamic single-section computed tomography (CT) scan revealed a large hematoma in the right psoas muscle, probably caused by the endoscopic discectomy. Dynamic single-section CT images 15 seconds after intravenous injection of contrast (arterial phase) showed leakage of contrast media into the hematoma directly, implying active arterial bleeding (Fig. 2).
Fig. 2.
Dynamic single-section computed tomography scan revealed a large hematoma in the right psoas muscle, probably caused by the endoscopic discectomy. Computed tomography image 15 seconds after intravenous injection of contrast (arterial phase) showed leakage of contrast media into the hematoma directly, implying active arterial bleeding (black arrow). long arrow: both common iliac arteries bifurcate from the aorta; delta arrow: common iliac vein.
The prothrombin time, partial thromboplastin time, and international normalized ratio (INR) were in the normal ranges. The patient's hemoglobin decreased to 8.4 g/dL and the platelet count was 176,000/µL. Three units of packed red blood cells (PRCs) were immediately transfused and the blood pressure recovered to 120/80 mmHg. On the 3rd day after the endoscopic procedure, the hemoglobin was 8.1 g/dL and the platelet count was 60,000/µL, so an additional three units of PRCs were transfused. On the 4th day after the endoscopic procedure, the hemoglobin was 11.6/dL, the platelet count was 77,000/µL, and her vital signs were stable. On the 5th day after the endoscopic procedure, she had no flank and leg pain, and all the vital signs and laboratory data had returned to normal but, the mild back pain persisted. At the 6 month follow-up examination, she had mild intermittent pain and mild hypesthesia on her right leg, but no neurologic deficits.
DISCUSSION
Generally, endoscopic lumbar discectomy is a minimally invasive procedure which, by dispensing with the need for resection of bone and ligament and performing selective evacuation of the intervertebral disc, the incidence of complications is low2,12,13) and surgery-induced instabilities can be prevented14-19,21). In addition, it is less traumatizing, has a shorter operating time, minimal scarring, and conserves the intact intra-epidural lubricant structure, such as epidural fat and yellow ligaments. But, as percutaneous endoscopic discectomy techniques become more popular, the possibility of complications rises accordingly.
Postoperative hematomas following spinal surgery are mostly spinal epidural hematomas. A spinal epidural hematoma is an uncommon complication of spinal surgery10). The incidence of postsurgical spinal epidural hematomas that result in neurologic deficits is extremely rare. Lawton et al.11) reported the incidence rate to be 0.1%. Uribe et al.23) reported the incidence rate of postsurgical spinal epidural hematomas to be 0.22%, and they also reported the effects of delayed postoperative spinal epidural hematomas, which resulted in clinical deterioration after an asymptomatic postoperative period of about 3 days. There have been no reported cases of psoas muscle hematomas following percutaneous endoscopic operation of lumbar disc herniation in the English medical literature.
In our case reported, the postoperative psoas muscle hematoma following percutaneous endoscopic discectomy might have been caused by the lumbar segmental artery injury.
Generally, angiography is a routine procedure for patients in whom suspicion of arterial injury is high, and the arterial bleeding can be controlled by endovascular embolization. But, in our case, without angiography, a lumbar segmental artery injury was able to be detected by dynamic single-section CT with intravenous contrast media. CT images 15 seconds after the intravenous injection of contrast (arterial phase) showed leakage of contrast media into the psoas muscle hematoma directly, implying active arterial bleeding. On the CT images, the region of active arterial bleeding was the space of the disc in which the material herniated far laterally with the segmental lumbar artery, which was divided into a posterior (vertebral) and an anterior (muscular) branch (Fig. 3).
Fig. 3.

Schematic view shows the region of active arterial bleeding which is the space of the disc in which material herniated far laterally and in which the segmental lumbar artery is divided into a vertebral and muscular branch.
The lumbar segmental arteries are important parietal branches for the spinal surgeon because of their very close relationship to the vertebral bodies. Because the aorta is situated somewhat to the left of the midline, the right lumbar segmental arteries are longer than those on the left. Both the right and left lumbar segmental arteries dip under the tendinous arch of the psoas muscles situated along the sides of the vertebral bodies. The arteries continue under the psoas muscles until they arrive at the interval between the transverse process of the vertebrae and the medial edge of the quadratus lumborum. While the lumbar segmental arteries course under the psoas muscles, they are accompanied by rami communicantes of the sympathetic chain and the lumbar veins. Anterior to the transverse process, the lumbar segmental arteries are crossed by branches of the lumbar plexus. Like their thoracic intercostal vascular counterparts, the lumbar segmental arteries course to the foramen and divide into a posterior (vertebral) and an anterior (muscular) branch. The anterior (muscular) branch travels forward between the abdominal muscles and terminates by anastomosing with other abdominal wall arteries3,22,24). The segmental vessels are identified at the inferior edge of the rostral pedicle, lateral to the existing nerve root20). Because of the higher muscular and interseg-mental distribution, the 4th lumbar arteries are often twice the caliber of the other lumbar arteries. The 4th lumbar arteries are involved in nutrition of the lower segments by contributions to the iliolumbar vessels. The lateral muscular branch of the 4th lumbar artery courses superior to the crest of the ilium. This position indicates that it is more likely to be encountered by percutaneous instrumentation. The 4th lumbar artery provides a relatively large, caudally-directed intersegmental branch that occurs near the level of the intervertebral foramen1).
Fortunately, in the case reported herein, the active arterial bleeding causing the psoas muscle hematoma was controlled spontaneously without any procedures, such as embolization or reoperation. If the arterial bleeding had continued, an angiography would have been performed and embolization may have been required. Under only conservative treatment, the unstable vital signs recovered to normal and the patient's pain improved.
It is unclear how the arterial injury occurred. There was no significant bleeding during the endoscopic discectomy, and the level of injury, as seen on CT images, appeared to be at the insertion site for the endoscope. It is doubtful that the working sheath approach to the disc space made at the level of the vertebra might have caused the vascular injury. The space of the disc in which material herniated far laterally is closely connected with the running lumbar segmental artery, making it highly likely that the segmental artery injury occurred while inserting the endoscope (Fig. 4).
Fig. 4.
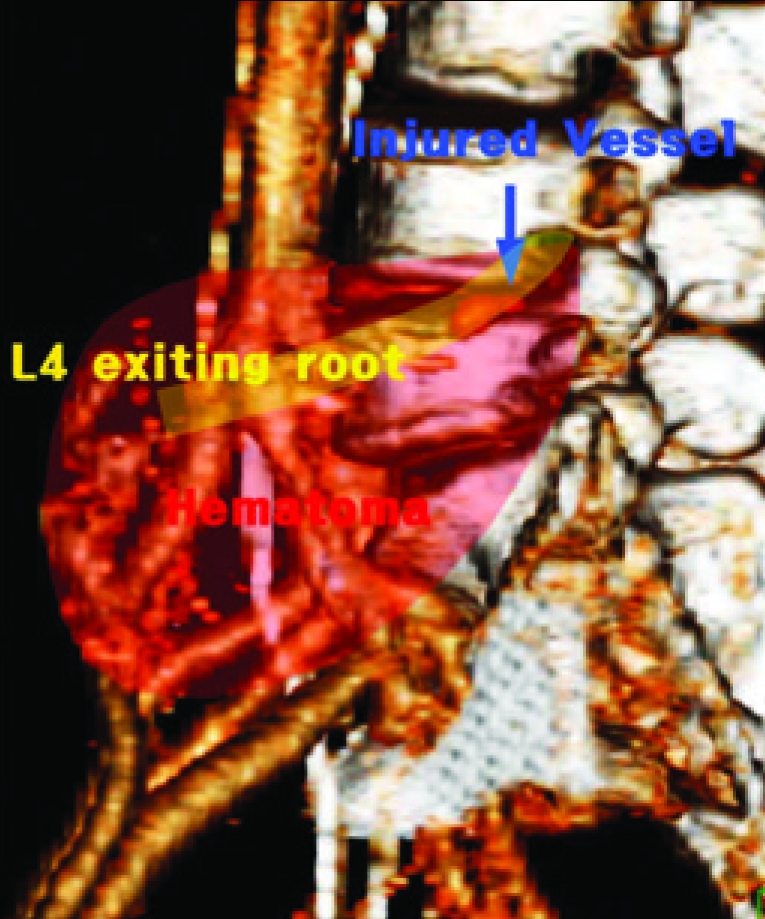
3D reconstruction computed tomography image shows the space of the disc in which the material herniated far laterally is closely connected with the running lumbar segmental artery; it is likely that injury of the segmental artery occurred during insertion of the endoscope.
The purpose of this case report was to present a case of an injury to a branch of the L4 segmental lumbar artery following percutaneous endoscopic lumbar discectomy and to give a warning to the surgeons of possibility of arterial injuries during percutaneous endoscopic lumbar discectomy.
CONCLUSION
Although percutaneous endoscopic lumbar discectomy is an effective minimally invasive surgery for treating lumbar disc herniation, the possibility of acute psoas muscle hematoma should be kept in mind. The pathogenic mechanisms of psoas muscle hematomas are unclear. However, in the development of acute flank and leg pain with hypotension after percutaneous posterolateral endoscopic lumbar discectomy, one should suspect the formation of a psoas muscle hematoma.
Acknowledgements
This paper was supported by research fund from Chosun University in 2008.
References
- 1.Biafora SJ, Mardjetko SM, Butler JP, McCarthy PL, Gleason TF. Arterial injury following percutaneous vertebral augmentation : a case report. Spine. 2006;31:E84–E87. doi: 10.1097/01.brs.0000197596.88416.02. [DOI] [PubMed] [Google Scholar]
- 2.Choi G, Lee SH, Bhanot A, Raiturker PP, Chae YS. Percutaneous endoscopic discectomy for extraforaminal lumbar disc herniations : extraforaminal targeted fragmentectomy technique using working channel endoscope. Spine. 2007;32:E93–E99. doi: 10.1097/01.brs.0000252093.31632.54. [DOI] [PubMed] [Google Scholar]
- 3.Clemente CD. Gray's Anatomy. ed 30 American. Baltimore: Williams & Wilkins; 1985. The arteries; pp. 648–787. [Google Scholar]
- 4.Clemente CD. Gray's Anatomy. ed 30 American. Baltimore: Williams & Wilkins; 1985. The veins; pp. 788–865. [Google Scholar]
- 5.Demirel CB, Kalayci M, Ozkocak I, Altunkaya H, Ozer Y, Acikgoz B. A prospective randomized study comparing perioperative outcome variables after epidural or general anesthesia for lumbar disc surgery. J Neurosurg Anesthesiol. 2003;15:185–192. doi: 10.1097/00008506-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Donceel P, Du Bois M. Fitness for work after lumbar disc herniation : A retrospective study. Eur Spine J. 1998;7:29–35. doi: 10.1007/s005860050023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: Reasons, intraoperative findings and long term results : A report of 182 operative treatments. Spine. 1996;21:626–633. doi: 10.1097/00007632-199603010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Gill K. Retroperitoneal bleeding after automated percutaneous lumbar discectomy-a case report. Spine. 1990;15:1376–1377. doi: 10.1097/00007632-199012000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Greenbarg PE, Brown MD, Pallares VS, Tompkins JS, Mann NH. Epidural anesthesia for lumbar spine surgery. J Spinal Disord. 1988;1:139–143. [PubMed] [Google Scholar]
- 10.Kotilainen E, Alanen A, Erkintalo M, Helenius H, Valtonen S. Postoperative hematomas after successful lumbar microdiscectomy or percutaneous nucleotomy : a magnetic resonance imaging study. Surg Neurol. 1994;41:98–105. doi: 10.1016/0090-3019(94)90105-8. [DOI] [PubMed] [Google Scholar]
- 11.Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma : relationship between surgical timing and neurological outcome. J Neurosurg. 1995;83:1–7. doi: 10.3171/jns.1995.83.1.0001. [DOI] [PubMed] [Google Scholar]
- 12.Lewis PJ, Weir BK, Broad RW, Grace MG. Long-term prospective study of lumbosacral discectomy. J Neurosurg. 1987;67:49–53. doi: 10.3171/jns.1987.67.1.0049. [DOI] [PubMed] [Google Scholar]
- 13.Maroon JC, Abla A, Bost J. Association between peridural scar and persistent low back pain after lumbar discectomy. Neurol Res. 1999;21 Suppl 1:S43–S46. doi: 10.1080/01616412.1999.11741026. [DOI] [PubMed] [Google Scholar]
- 14.Mayer HM, Brock M. Percutaneous endoscopic discectomy : surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–225. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 15.McCulloch JA. Principles of Microsurgery for Lumbar Disc Diseases. New York, NY: Raven Press; 1989. [Google Scholar]
- 16.McLain RF, Kalfas I, Bell GR, Tetzlaff JE, Yoon HJ, Rana M. Comparison of spinal and general anesthesia in lumbar laminectomy surgery : a case-controlled analysis of 400 patients. J Neurosurg Spine. 2005;2:17–22. doi: 10.3171/spi.2005.2.1.0017. [DOI] [PubMed] [Google Scholar]
- 17.Mekhail N, Kapural L. Intradiscal thermal annuloplasty for discogenic pain: an outcome study. Pain Pract. 2004;4:84–90. doi: 10.1111/j.1533-2500.2004.04203.x. [DOI] [PubMed] [Google Scholar]
- 18.Mochida J, Nishimura K, Nomura T, Toh E, Chiba M. The importance of preserving disc structure in surgical approaches to lumbar disc herniation. Spine. 1996;21:1556–1563. doi: 10.1097/00007632-199607010-00014. discussion 1563-1564. [DOI] [PubMed] [Google Scholar]
- 19.Mochida J, Toh E, Nomura T, Nishimura K. The risks and benefits of percutaneous nucleotomy for lumbar disc herniation. A 10-year longitudinal study. J Bone Joint Surg Br. 2001;83:501–505. doi: 10.1302/0301-620x.83b4.11508. [DOI] [PubMed] [Google Scholar]
- 20.Nho JS, Chung HY, Lee U, Kang DS, Kim YB, Bak KH. Clinical experience in the treatment of far lateral lumbar disc herinaton. J Korean Neurosurg Soc. 1995;24:1385–1391. [Google Scholar]
- 21.Onik G, Mooney V, Maroon JC, Wiltse L, Helms C, Schweigel J, et al. Automated percutaneous discectomy: a prospective multi-institutional study. Neurosurgery. 1990;26:228–232. discussion 232-233. [PubMed] [Google Scholar]
- 22.Patten BM. The cardiovascular system. In: Schaeffer JP, editor. Morris' Human Anatomy. Philadelphia: Blakiston; 1947. pp. 582–785. [Google Scholar]
- 23.Uribe J, Moza K, Jimenez O, Green B, Levi AD. Delayed postoperative spinal epidural hematomas. Spine J. 2003;3:125–129. doi: 10.1016/s1529-9430(02)00535-1. [DOI] [PubMed] [Google Scholar]
- 24.Warwick R, Williams PL. Gray's Anatomy. ed 35. British Philadelphia: W.B. Saunders Co; 1973. Angiology; pp. 588–744. [Google Scholar]