Abstract
Purpose
To: (1) examine growth in family conflict during adolescence as a predictor of depressive symptoms in early adulthood; (2) examine adult stressful life events as a possible mechanism linking prior family conflict with depressive symptoms; and (3) examine adolescent school bonding as a possible moderator of family conflict and stressful life events in relation to later depression.
Methods
Analyses used a latent variable growth curve modeling approach to examine longitudinal patterns in data from the Seattle Social Development Project (SSDP). Assessments of a gender-balanced and ethnically diverse sample of 754 participants were conducted from age 10 to age 27.
Results
Results show an increase in conflict each year between ages 14 and 18 for participating youth. High initial levels and growth in family conflict predicted adult stressful life events, which, in turn, predicted adult depressive symptoms, controlling for earlier risks of poverty and internalizing problems. Bonding to school in mid adolescence did not significantly change the associations among the variables in the model.
Conclusions
Inhibiting the growth in family conflict over the course of adolescence may reduce the risk for some life stresses linked to depression in early adulthood. While a test of the protective influence of school bonding during mid adolescence was not significant, the study offers an example of how longitudinal patterns and protective factors can be analyzed.
Keywords: family conflict, depression, stressful life events, bonding to school, poverty, adolescence, early adulthood
Introduction
Research has shown that conflict in the home—particularly severe and prolonged conflict—can lead to worse psychosocial functioning for adolescents and young adults [1, 2]. High-level conflict, including or leading to violence and abusive behavior on the part of one family member toward another, has been repeatedly shown to increase the risk of many problems for children living in the home, including conduct problems and depression [3-5]. For example, in the Lehigh Longitudinal Study, Herrenkohl and Herrenkohl [6] found a significant increase in the risk of both externalizing and internalizing symptoms among youths who were earlier abused or exposed to violence between parents in the home. Moylan et al. [7] documented a significant increase in the likelihood of depression and other internalizing symptoms, as well as externalizing behaviors, in youth previously abused and/or exposed to domestic violence. Elsewhere, Reinherz et al. [2] reported a relatively strong bivariate association (OR: 2.73) between family violence by age 15 (retrospectively measured) and major depression diagnosis for individuals in late adolescence and early adulthood.
Other studies suggest that even less severe forms of conflict (e.g., arguing and yelling) and closely related dynamics (e.g., parent-child disagreements and negative relationship quality), which are considered a normal part of parent-teen relationships [8-11], can have immediate and some enduring consequences [12]. For example, Aseltine et al. [13] used a probability sample of high school students to examine the association between quality of adolescents’ social relationships (peer and family) and risk of depression and substance use. Findings show the co-occurrence of depression and substance use is linked to having had low family support and a negative relationship with one’s parents. A baseline measure of family conflict (e.g., frequent arguments with parents) was modestly correlated with depression at around .20.
Using data from the national Add Health study, Matjasko, Grunden, and Ernst [14] examined predictors of stability and change in functioning profiles of adolescents measured over a 2-year period. Predictors included parent-adolescent conflict (e.g., serious arguments), family climate (e.g., warmth), and parental involvement. Results indicate that, compared to stable, well-adjusted adolescents, those whose depressive symptoms remained stable or worsened over a year’s time experienced less family warmth and more parent-adolescent conflict.
Additionally, Rueter and colleagues [15] conducted a longitudinal study of the relation between parent-child disagreements, internalizing symptoms, and the onset of depressive and anxiety disorders in late adolescence. The study found an indirect effect of disagreements on later depression and anxiety through base level and subsequent changes in internalizing symptoms during early adolescence.
Further, in a study of depression recurrence at ages 19 - 23 among 274 formerly depressed adolescents, Lewinsohn et al. [16] found parent-child conflict was a statistically significant predictor that interacted with child gender; here, the association of conflict with depression among young adults was stronger for females than for males. However, Sheeber et al. [12] found that the effect of conflict on depression was the same for boys and girls. Finally, Reinherz et al. [2] found that a low rating of family cohesion at age 15, a likely correlate of overt conflict, increased the risk of depression in young adulthood (ages 18 - 26) after controlling for gender (OR: 1.75).
However, few studies have accounted for longitudinal changes in less severe or low-level family conflict over the course of adolescence and its subsequent effects on outcomes in early adulthood, including depression. A longitudinal examination of family conflict as a dynamic risk factor for adult depression should help determine if stability and/or change in this presumed normative process of adolescent development has any bearing on an individual’s later vulnerability to mental health problems. For example, boys and girls who experience a steeper rate of increase in conflict relative to their peers may be at particularly high risk for depression that persists into adulthood; that is, conflict that increases rapidly during adolescence may lead to chronic depression that extends into the adult years, or symptoms of depression that emerge years after the conflict was first experienced. Moreover, there has been little research on the role of family conflict in the context of both distal stressors such as childhood poverty, and proximal stressors such as traumatic early adult events. These variables have been independently shown to increase risk of adult psychopathology [17-19]. For example, in adulthood, experiences such as loss of a loved one, breakup or divorce, and job loss have been linked to depression [18], although studies have failed to account for the effects of co-occurring and/or earlier risk factors (including poverty, internalizing symptoms or prior depression, and family conflict), which might account in full or in part for the proximal influence on depression of stressful life events.
The cause of some stressful life events during early adulthood may be less attributable to earlier life experiences than are others (e.g., family breakup or divorce). However, there is ample evidence that events, like divorce, are themselves tied to relationship patterns set early in life through patterns in one’s family [20]. Yet, research has not examined whether adulthood stressful life events of any form can be linked to earlier risk factors, such as family conflict, and whether these risk factors work through or around stressful life events in predicting adult depression.
Related research suggests that healthy prosocial bonds may have a protective effect, mitigating the impact of earlier conflict or stress on later depression [21]. Attachment (bonding) to school has been shown in some research to buffer the effect of early risk factors on problems (e.g., conduct problems) in adolescence [22, 23]. An association between school bonding and mental health outcomes, such as depression, is less well established [24], although theory hypothesizes a similar moderating effect of early risk exposure [25].
According to social developmental theory [25], strong interpersonal bonds and attachment to prosocial institutions, like school, should protect against the negative effects of family conflict by exposing children to positive norms, role models, and healthy expectations of those within those settings. This perspective hypothesizes that bonding to school should increase academic achievement, promote good work habits, and lessen the risk of psychosocial problems by bringing a child’s beliefs and behavior in line with those of the school. To the extent that doing well in school leads to a feeling of achievement-- and praise from likeminded peers-- it is conceivable the risk of depression and other mental health problems would diminish, even in the presence of ongoing conflict in the home [26].
Objectives and Hypotheses
Goals of this study are: (1) to examine growth in family conflict during adolescence as a predictor of depressive symptoms in early adulthood (ages 21 - 27). We hypothesize that a rapid increase in family conflict during adolescence will, in turn, elevate the risk of depressive symptoms during early adulthood, controlling for childhood poverty and early internalizing problems; (2) to examine adult stressful life events as a possible mechanism linking prior family conflict with depressive symptoms. We hypothesize that stressful life events will mediate, in part or full, the effect of family conflict on later depression; and (3) to examine adolescent school bonding as a possible moderator of family conflict in the prediction of later depression. We hypothesize that school bonding will buffer the effect of family conflict and other risk factors on adult depression.
Methods
Sample
The sample consists of all participants in the Seattle Social Development Project (SSDP) (N = 754) who completed one or more surveys across 11 waves of data collected from ages 10 to 27. The sample, originally recruited from 18 elementary schools in urban Seattle in 1985, contains near equal numbers of males and females (50%) and is ethnically diverse: 47% Caucasian; 26% African American; 22% Asian American; and 5% Native American. Just over half the sample (51%) are from childhood poverty, as measured by eligibility for the federal school lunch program at ages 10 - 13. SSDP has maintained a 92% minimum retention of the original sample since the survey assessment of youth respondents at age 14. Detailed summaries of the SSDP sample and study methods can be found in earlier papers [27, 28]. Data collection procedures were approved by the Human Subjects Review Committee of the University of Washington.
Measures
Variables consisted of childhood poverty (age 10 - 13), a measure of family eligibility for the federal school lunch program when children were in the fifth, sixth, or seventh grades. Approximately 51% of the sample was found to have been in poverty. Internalizing problems (age 14) was measured by items from the Achenbach Child Behavior Checklist (CBCL) [29] for self-reported anxious and withdrawn behaviors (6 items, α = .71). Items include a child’s tendency to ‘worry’; be ‘nervous or tense’; ‘too fearful/anxious’; ‘anxious to please’; ‘secretive’; and ‘afraid of mistakes’. The mean of this 0 - 12 scale is 4.20 and the standard deviation is 2.52. Gender is a dichotomous variable for which males were coded 0 and females were coded 1. Family conflict (age 14 - 18) is based on youth reports of the frequency with which family members argue; are critical of each other; and yell (3 items at each age, α = .71 to .85). Scores on each item at each age were coded 0 ‘almost never’; 1 ‘seldom’; 2 ‘sometimes’; 3 ‘fairly often’; 4 ‘almost always,’ and then summed within year (total scale scores for each year ranged from 0 - 12). The scale has a mean of 4.58 and a standard deviation of 2.20. Stressful life events (age 21) summed the number of events reported and included family or household problems; death of someone close; breakup or divorce; fired; and victim of crime (19 items, α = .61). The scale has a range of 0 - 19, a mean of 3.19, and a standard deviation of 2.40. Finally, depressive symptoms (age 21 - 27) was measured by summing the total number of past-year depressive symptoms from the Diagnostic Interview Schedule (DIS) [30] across 3 ages (21, 24, and 27 years), including anhedonia; weight changes; sleep problems; psychomotor agitation or retardation; fatigue; feelings of worthlessness; concentration difficulties; and suicidal ideation (27 total symptoms assessed by 54 items, α = .94).The scale has a mean of 5.13 and a standard deviation of 6.27.
School bonding (age 16) is included as a hypothesized moderator of the relations between predictors and the measured outcome of depression. This youth-report measure is based on questions of whether youth like school, their teachers, and classes; whether they do extra work in class; look forward to school; and finish assignments (7 items, α = .73).
Analysis
Analyses used a latent variable growth curve modeling approach (Mplus 4.2) [31] with full-information maximum likelihood estimates for incomplete data. To examine growth in family conflict from ages 14 - 18, we included in the model 2 latent constructs, 1 for the average frequency of family conflict at age 14 (intercept) and 1 for the change (slope) in family conflict over 4 time points: ages 14, 15, 16, and 18 (no data were collected at age 17). Factor loadings of the intercept factor were set to 1; factor loadings of the slope factor were set to model a linear pattern in the data; that is, loadings were set to 0, 1, 2, and 4 to reflect the yearly measurements to age 16, and the 2-year span from age 16 to age 18. All other variables in the analysis are measured variables.
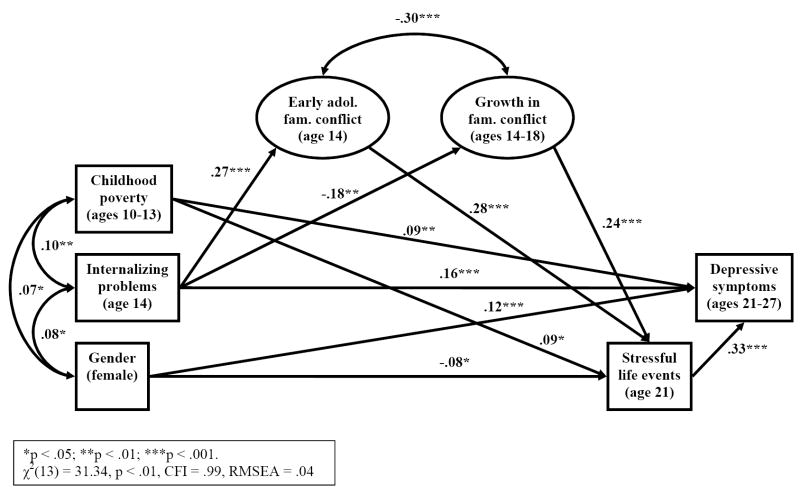
A confirmatory factor analysis (CFA) was conducted first to examine the fit of the model to the data and the correlations among the latent and measured variables. A test of structural paths consistent with the hypothesized model (Figure 2) followed the CFA. The model included paths from childhood poverty and internalizing problems predicting family conflict (intercept and slope), stressful life events at age 21, and depressive symptoms at ages 21 - 27. Family conflict was modeled as both a direct predictor of depressive symptoms and indirect predictor of the outcome through stressful life events at age 21. Gender was also included as a covariate.1 Multiple-group structural equation modeling (MGSEM) was used to examine possible moderating effects of bonding to school at age 16. To test the degree to which stressful life events acted as a mediator of family conflict and adult depression, we used an estimate of the indirect effect generated with the Mplus Model Indirect command, which computes the product of component paths and Delta method standard errors [31].
Figure 2.
Results of the hypothesized model showing statistically significant paths.
Results
Growth in Family Conflict
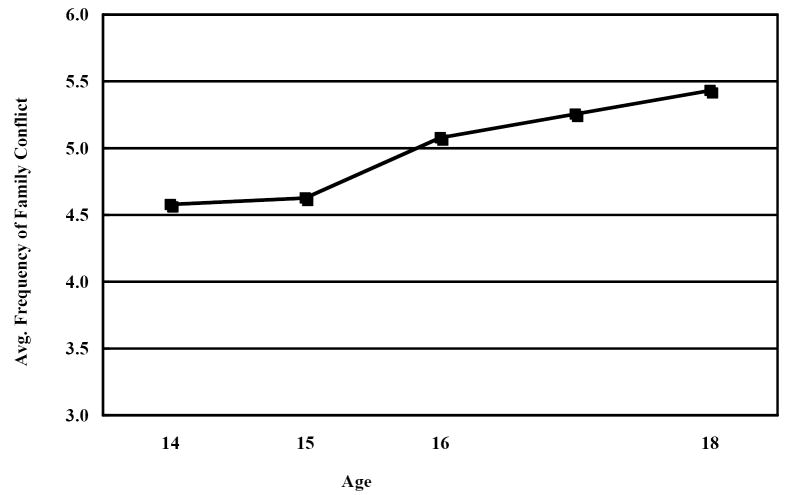
Figure 1 shows the average frequency of family conflict at each age examined (14 - 18), where high scores indicate increasingly higher frequency of conflict. Participants reported the average frequency of conflict in their families during adolescence was between “seldom” (4.61 on the 0 - 12 scale at age 14) and “sometimes” (5.44 on an identical scale at age 18). As shown, family conflict, on average, increases over the course of adolescence.
Figure 1.
Average frequency of family conflict at ages 14-18.
Correlations and Means
Table 1 shows the correlations among all variables from the CFA analysis. Zero-order correlations show a significant but modest association for adult depressive symptoms and early family conflict (r = .19, p < .001) and a weak, nonsignificant association for depressive symptoms and growth in family conflict during adolescence (r = .02, p > .10). Female gender and distal factors including childhood poverty and early internalizing problems were significantly, but modestly correlated with adult depressive symptoms at ages 21 - 27 (r = .14, .15, and .19, respectively). Proximal stressful life events in early adulthood had the strongest correlation with depressive symptoms (r = .35, p < .001). Table 1 also shows a relatively strong correlation between early family conflict and internalizing problems for youth at age 14 (r = .28, p < .001) and a significant, modest correlation between early family conflict and later stressful life events at age 21 (r = .19, p < .001).
Table 1.
Correlations, means, and standard deviations among the variables from the CFA analysis.
| Internalizing problems | Gender | Early family conflict | Growth in family conflict | Stressful life events | Depressive symptoms | School bonding | |
|---|---|---|---|---|---|---|---|
| Child poverty (10 - 13) | .10** | .07* | .06 | .06 | .11** | .15*** | .09* |
| Internalizing problems (14) | .08* | .28*** | -.17** | -.01 | .19*** | -.03 | |
| Gender (female) | .10* | .05 | -.04 | .14*** | .11** | ||
| Early family conflict (14) | -.34*** | .19*** | .19*** | -.16*** | |||
| Growth in family conflict (14 - 18) | .15** | .02 | .09 | ||||
| Stressful life events (21) | 35*** | -.04 | |||||
| Depressive symptoms (21 - 27) | -.06 |
p < .05;
p < .01;
p < .001.
Model
Figure 2 shows the significant structural paths of the tested model, in which each prior factor was included as a predictor of each subsequent factor longitudinally. Path coefficients are standardized. Neither early family conflict nor growth in family conflict during adolescence had a significant direct effect on adult depressive symptoms (paths not shown). However, each was associated with more stressful life events in early adulthood (coefficients of .28 and .24, respectively), which, in turn, predicted an increase in depressive symptoms (β = .33, p < .001). Tests of the indirect of effects of the family conflict intercept and slope variables on depressive symptoms through stressful life events were in both cases statistically significant (p < .05). Childhood poverty, internalizing problems in early adolescence, and female gender all had significant direct effects on depressive symptoms in adulthood, even after accounting for family conflict and proximal stressful life events. Early internalizing problems (i.e., anxious and withdrawn behaviors at age 14) were significantly associated with early family conflict and growth in family conflict over the course of adolescence. The hypothesized model fit the data well: χ2(13) = 31.34, p < .01, CFI = .99, RMSEA = .04.
Model for High Versus Low School Bonding
To examine the extent to which school bonding was protective against earlier risks in the prediction of adult depression, we conducted a multiple-group structural equation model (MGSEM) test for high versus low school bonders in mid adolescence (age 16). We chose age 16 to coincide with the midpoint of adolescence between the first and last measures of family conflict (age 14 and age 18); this tests the protective role of school bonding at an age when family conflict is likely to increase (during mid adolescence) and when buffering effects on later risk may be particularly beneficial. The high and low bonder groups were determined using a median split in the distribution of scores of the original variable.3 For the analysis, we compared the fit of an unconstrained model to one in which all structural paths for the 2 groups were constrained to be equal. This provided an overall test of the moderating role of bonding. Results of the analysis showed no significant differences between the 2 models (Δχ2(21) = 7.21, p = .998), indicating that the structural paths of the models for high and low school bonders are statistically equivalent.
To assess whether a more extreme cutoff on the school bonding variable would change the results of the analysis, we re-ran the multi-group model defining “high” school bonding as the upper 25% of the score distribution [32]; however, results again showed no overall group differences in paths of the tested model.
Discussion
The frequency of criticism, arguing, and yelling within families while participants were in their adolescent years was relatively low overall, averaging between “seldom” and “sometimes.” However, results suggest a steady increase in conflict between ages 14 and 18 for participating youth. In addition, the tested models help further understanding of the relationship between family conflict and adult depressive symptoms in the context of other important risks and outcomes. In particular, adult depressive symptoms were significantly correlated with all predictors in the model except growth in family conflict. High initial levels and growth in family conflict, however, remained important predictors of adult stressful life events, even after accounting for earlier risks of poverty and internalizing problems. And stressful life events, in turn, predicted adult depressive symptoms. Thus, family conflict does appear to have an enduring effect on later depressive symptoms—through proximal events, including those over which an individual has some control (e.g., experiencing a breakup or getting divorced; being fired). This holds true even when accounting for the significant roles of gender, prior poverty, and internalizing problems.
These results advance knowledge of the pathways through which earlier conflict and other risk factors affect later depression but remain consistent with the key findings of prior research, including a study by Reinherz and colleagues [2] who studied the effects of family functioning (e.g., family violence and cohesion at/by age 15) on major depression between the ages of 18 and 26. Results of their study suggest that family violence by age 15 (possibly an extreme form of conflict) was among the most significant predictors of early adult depression, increasing the risk of depression for boys and girls by nearly four times. The study also found that self- and mother-rated internalizing problems at age 15 was predictive of later depression, independent of other variables examined.
Perhaps one explanation for the link between family conflict and stressful life events years later involves an individual’s struggle to overcome the emotional impact of growing up in a household characterized by hostile relationships. This could be manifested later in the inability to maintain employment and successful adult relationships due to poor stress management and inadvertently exposing oneself to experiences that are potentially self-defeating, yet familiar. This process, more broadly conceptualized, is consistent with the idea of individual susceptibility to later risks following risk exposure. It is also consistent with the notion of cumulative or aggregative risk processes, in which interactions among individual and environmental variables lead over time to greater vulnerability and a higher likelihood of problems for an individual, offset or moderated only by intervening protective or compensatory factors [33, 34]. In any case, inhibiting the growth in family conflict over the course of adolescence, even if relatively infrequent, appears a promising and worthwhile prevention strategy relevant to professionals in a variety of settings, including health care and social service agencies. Better screening protocols and treatment of internalizing problems and early-onset depression in adolescents also appears a worthwhile goal for its potential to impact the functioning of families and later symptoms of depression or recurrence [2].
Analyses found no moderating effects of adolescent school bonding, which compared those below (low bonding) and above the median (high bonding) on that variable. Thus, as operationalized in this study, an adolescent’s level of bonding to school did not, as originally hypothesized, buffer the effects of risks for adult depression. However, more research is needed on the role of bonding in relation to depression, including possible differences based on the age at which bonding is measured (e.g., early versus middle and late adolescence); and the type of bonding and social support that is studied (e.g., bonding to school versus work; support by family, partner, and/or peers).
Limitations
Limitations of the study include a targeted focus on just a few of the many possible risks and intervening variables that could predict symptoms of depression in early adulthood [2, 16]. Further research should help delineate additional pathways through which childhood risks increase the probability of primary onset and recurrence of mental health problems during and after adolescence [16]. Additionally, analyses focused on school bonding as one possible protective factor, although other sources of protection from depression in early adulthood are possible. For example, social competence, positive coping, and social support provided by family and friends during adolescence and early adulthood could lessen the risk of depression for those who experience childhood risks, although Lewinsohn and colleagues [16] did not find these to be among the most salient predictors of recurrent depression in formerly depressed adolescents. Additionally, our analyses did not account for aspects of the school context (e.g., resources, organization, perceptions of safety) that could influence the extent of students’ bonding to their individual schools. Finally, our use of only self-report data, a truncated CBCL measure of internalizing problems, and a scale of stressful life events at age 21 that had moderate internal consistency (α = .61) may be limitations.
Conclusion
This study helps to further illuminate the predictive role of family conflict in relation to stressful life events and adult depression, accounting for childhood poverty and internalizing problems. While our test of the protective influence of school bonding during mid adolescence was not significant, this part of the study offers an example of how longitudinal patterns of behavior and possible moderators can be examined using an integrated SEM approach. Overall, results are useful for planning developmentally informed interventions, particularly with families of adolescents, to lessen the risks of depressive symptoms for young adults, for whom the prevalence of depression is relatively high [35, 36].
Acknowledgments
This research was supported by grants #1R01DA09679-11 and #9R01DA021426-08 from the National Institute on Drug Abuse and #21548 from the Robert Wood Johnson Foundation. An earlier version of this paper was presented at the Society for Prevention Research Annual Meeting, Washington, DC, 30 May 2007.
Footnotes
Gender was also examined as a moderator variable: We conducted a multiple-group test (MGSEM) in which coefficients of the structural paths were constrained to be equal across the 2 groups. A comparison of the fully constrained model to one in which paths for the 2 groups were freely estimated showed no significant reduction in overall fit (Δχ(15) = 15.17, p > .05).
A portion of the sample was exposed to a multicomponent preventive intervention in the elementary grades, consisting of teacher training, parenting classes, and social competence training for children [28]. While differences in prevalences and means have been observed between the intervention and control groups on variables including school bonding and depression, prior analyses have shown few differences in the covariance structures of the groups [37-39]. Analyses for this report were based on the full sample after examining possible differences in the relationships of the predictors with stressful life events and adult depression, comparing the control group and the intervention conditions combined. For the comparison, we first conducted analyses of the variable covariances in a multiple-group CFA. Results of the fully constrained model to one in which associations among the variables were freely estimated showed no significant reduction in overall fit (Δχ(28) = 33.60, p > .05), indicating that the basic relationships among the variables were the same across groups. Next we added ‘intervention’ in the structural model as a predictor. Results showed that none of the paths was significant from intervention to the intercept or slope measures of family conflict; stressful life events; or depression. Moreover, fundamental associations among the primary variables in the analysis remained the same when intervention was included, thereby supporting a single-group analysis.
A sensitivity test for the school bonding variable using an alternative threshold cutoff was conducted; results are addressed in the Discussion.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hoeve M, Smeenk W, Loeber R, et al. Long-term effects of parenting and family characteristics on delinquency of male young adults. Eur Journal Criminol. 2007;4:161–94. [Google Scholar]
- 2.Reinherz HZ, Paradis AD, Giaconia RM, et al. Childhood and adolescent predictors of major depression in the transition to adulthood. Am J Psychiatry. 2003;160:2141–47. doi: 10.1176/appi.ajp.160.12.2141. [DOI] [PubMed] [Google Scholar]
- 3.Herrenkohl TI, Sousa C, Tajima EA, et al. Intersection of child abuse and children’s exposure to domestic violence. 2007 doi: 10.1177/1524838008314797. manuscript under review. [DOI] [PubMed] [Google Scholar]
- 4.Edleson JL. Problems associated with children’s witnessing domestic violence. [June 9, 2004];Violence Against Women Online Resources. Available at: www.vaw.umn.edu.
- 5.Gewirtz AH, Edleson JL. Young children’s exposure to intimate partner violence: Towards a developmental risk and resilience framework for research and intervention. J Fam Violence. 2007;22 [Google Scholar]
- 6.Herrenkohl TI, Herrenkohl RC. Examining the overlap and prediction of multiple forms of child maltreatment, stressors, and socioeconomic status: A longitudinal analysis of youth outcomes. J Fam Violence. in press. [Google Scholar]
- 7.Moylan CA, Herrenkohl TI, Sousa C, et al. The combined effects of child abuse and witnessing domestic violence on adolescent internalizing and externalizing behavior problems. doi: 10.1007/s10896-009-9269-9. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adams R, Laursen B. The organization and dynamics of adolescent conflict with parents and friends. J Marriage Fam. 2001;63:97–110. [Google Scholar]
- 9.Allen JP, Hauser ST, OConnor TG, et al. The connection of observed hostile family conflict to adolescents’ developing autonomy and relatedness with parents. Dev Psychopathol. 1996;8:425–42. [Google Scholar]
- 10.Laursen B, Collins WA. Interpersonal conflict during adolescence. Psychol Bull. 1994;115:197–209. doi: 10.1037/0033-2909.115.2.197. [DOI] [PubMed] [Google Scholar]
- 11.Smetana JG, Campione-Barr N, Metzger A. Adolescent development in interpersonal and societal contexts. Annu Rev Psychol. 2006;57:255–84. doi: 10.1146/annurev.psych.57.102904.190124. [DOI] [PubMed] [Google Scholar]
- 12.Sheeber L, Hops H, Alpert A, et al. Family support and conflict: Prospective relations to adolescent depression. J Abnorm Child Psychol. 1997;25:333–44. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- 13.Aseltine RH, Gore S, Colten ME. The co-occurrence of depression and substance abuse in late adolescence. Dev Psychopathol. 1998;10:549–70. doi: 10.1017/s0954579498001746. [DOI] [PubMed] [Google Scholar]
- 14.Matjasko JL, Grunden LN, Ernst JL. Structural and dynamic process family risk factors: Consequences of holistic adolescent functioning. J Marriage Fam. 2007;69:654–74. [Google Scholar]
- 15.Rueter MA, Scaramella L, Wallace LE, et al. First onset of depressive or anxiety disorders predicted by the longitudinal course of internalizing symptoms and parent-adolescent disagreements. Arch Gen Psychiatry. 1999;56:726–32. doi: 10.1001/archpsyc.56.8.726. [DOI] [PubMed] [Google Scholar]
- 16.Lewinsohn PM, Rohde P, Seeley JR, et al. Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. Am J Psychiatry. 2000;157:1584–91. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- 17.Moren-Cross J. The effects of life course poverty on depression. Gerontologist. 2004;44:650–51. [Google Scholar]
- 18.Paykel ES. The evolution of life events research in psychiatry. J Affect Disord. 2001;62:141–49. doi: 10.1016/s0165-0327(00)00174-9. [DOI] [PubMed] [Google Scholar]
- 19.Pine DS, Cohen P, Johnson JG, et al. Adolescent life events as predictors of adult depression. J Affect Disord. 2002;68:49–57. doi: 10.1016/s0165-0327(00)00331-1. [DOI] [PubMed] [Google Scholar]
- 20.Teachman JD. Childhood living arrangements and the intergenerational transmission of divorce. J Marriage Fam. 2002;64:717–29. [Google Scholar]
- 21.Wallace JE. Job stress, depression and work-to-family conflict - A test of the strain and buffer hypotheses. Relations Industrielles-Industrial Relations. 2005;60:510–39. [Google Scholar]
- 22.Resnick MD. Protective factors, resiliency, and healthy development. Adolesc Med. 2000;11:157–64. [PubMed] [Google Scholar]
- 23.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278:823–32. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 24.Shocet IM, Dadds MR, Ham D, et al. School connectedness is an underemphasized parameter in adolescent mental health: Results of a community prediction study. J Clin Child Adolesc Psychol. 2006;35:170–79. doi: 10.1207/s15374424jccp3502_1. [DOI] [PubMed] [Google Scholar]
- 25.Catalano RF, Hawkins JD. The social development model: A theory of antisocial behavior. In: Hawkins JD, editor. Delinquency and crime: Current theories. New York: Cambridge University Press; 1996. pp. 149–97. [Google Scholar]
- 26.Way N. A longitudinal study of the effects of family, friends, and school experiences on the psychological adjustment of ethnic minority, Low SES adolescents. J Adolesc Res. 2003;18:324–46. [Google Scholar]
- 27.Battin SR, Hill KG, Abbott RD, et al. The contribution of gang membership to delinquency beyond delinquent friends. Criminology. 1998;36:93–115. [Google Scholar]
- 28.Hawkins JD, Catalano RF, Kosterman R, et al. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Arch Pediatr Adolesc Med. 1999;153:226–34. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- 29.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 30.Robins LN, Cottler L, Bucholtz K, et al. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University; 1995. [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus User’s Guide. 3. Los Angeles: Muthen & Muthen; 2004. [Google Scholar]
- 32.Farrington DP, Loeber R. Some benefits of dichotomization in psychiatric and criminological research. Crim Behav Ment Health. 2000;10:100–22. [Google Scholar]
- 33.Masten AS. Ordinary magic: Resilience processes in development. Am Psychol. 2001;56:227–38. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 34.Rutter M. Psychosocial adversity: Risk, resilience and recovery. In: Richman JM, Fraser MW, editors. The context of youth violence: Resilience, risk and protection. Westport, CT: Praeger Publishers; 2001. pp. 13–42. [Google Scholar]
- 35.Eaton WW, Anthony JC, Gallo J, et al. Natural history of Diagnostic Interview Schedule/DSM-IV major depression: The Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry. 1997;54:993–99. doi: 10.1001/archpsyc.1997.01830230023003. [DOI] [PubMed] [Google Scholar]
- 36.Kessler RC, Zhao S, Blazer DG, et al. Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. J Affect Disord. 1997;45:19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- 37.Abbott RD, Catalano RF, Hawkins JD. Issues in the analysis of data from the Seattle Social Development Project. Seattle: 1991. Unpublished technical report. [Google Scholar]
- 38.Catalano RF, Kosterman R, Hawkins JD, et al. Modeling the etiology of adolescent substance use: A test of the social development model. J Drug Issues. 1996;26:429–55. doi: 10.1177/002204269602600207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang B, Kosterman R, Catalano RF, et al. Modeling mediation in the etiology of violent behavior and adolescence: A test of the social development model. Criminology. 2001;39:75–107. [Google Scholar]