Abstract
Background and objectives: Nocturnal home hemodialysis (NHHD) has been shown to improve clinical outcomes, although adoption has been limited. Given the known benefits, an understanding of the barriers to adoption is needed.
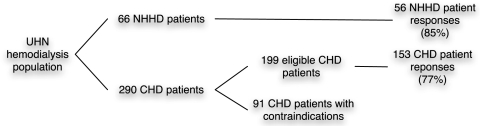
Design, setting, participants, & measurements: Patient-perceived barriers were studied through a cross-sectional survey of prevalent hemodialysis patients using validated instruments, study-specific questions, and ethnographic interviews. Fifty-six of 66 NHHD patients and 153 of 199 conventional hemodialysis (CHD) patients were included in the survey. Twenty interviews were conducted with NHHD, CHD, and predialysis patients.
Results: Compared with CHD patients, NHHD patients had higher perceived physical health scores (Short Form 12 [SF-12]: 41.47 ± 10.9 versus 34.73 ± 10.6, P < 0.0001), but had similar mental health scores (47.30 ± 11.1[NHHD] versus 45.27 ± 11.3[CHD]), P = 0.25). Despite having similar measures of education and perceived social support as NHHD patients, CHD patients had a low interest (1.68 [out of 5] ± 1.26) in adopting NHHD. The major barriers perceived by CHD patients were lack of self-efficacy in performing the therapy, lack of confidence in self-cannulation, and length of time on current therapy. Similar themes emerged from the qualitative analysis as well as: burden on family members and fear of a catastrophic event.
Conclusions: Patient-perceived barriers are primarily fears of self-cannulation, a catastrophic event, and the burden on family. These findings should form the basis of screening patients for interest in NHHD and serve to mitigate these concerns.
Health care organizations continue to face resource challenges to accommodate the sustained increase in the number of end-stage renal disease (ESRD) patients requiring renal replacement therapy. Nocturnal home hemodialysis (NHHD) has been shown in some studies to improve cardiovascular health and sleep quality, as well as to eliminate the need for dietary restrictions (1,2), while providing resource and financial motivation (3–6).
Despite these significant improvements in health outcomes and resource utilization, the adoption of NHHD has been limited (7). As illustrated previously (8), understanding of patient-perceived barriers to the adoption of any form of dialysis central to the development of strategies to mitigate these significant concerns. The aim of the present study was to determine the perceived barriers to the adoption of NHHD by conventional hemodialysis (CHD) patients. Given that CHD is the dominant form of renal replacement therapy in North America, we elected to focus on this patient population to enhance our understanding of their perception of NHHD. To this end, patient-perceived barriers were studied through a cross-sectional survey using validated instruments, study-specific questions, and ethnographic interviews.
Materials and Methods
The study protocol was approved by the University Health Network and University of Toronto Research Ethics Board. Patient-perceived barriers were determined through a cross-sectional survey of prevalent hemodialysis patients using validated instruments, study-specific questions, and ethnographic interviews.
Hemodialysis patients from the University Health Network in Toronto were recruited in the study. Specifically, 66 NHHD patients and 290 CHD patients were considered. The intent was to elicit a response from a “typical” CHD population being considered for NHHD. Patients were excluded on the basis of the following: medical contraindications to NHHD, life expectancy <6 mo, physical and/or visual impairments limiting the ability to conduct home hemodialysis, and mental or psychiatric diagnoses that would prevent them from living independently. All study subjects also were required to have a permanent address and a working knowledge of English.
NHHD patients received hemodialysis at home for 6 to 8 h, 4 to 6 nights per week. Vascular access was achieved through either a long-term internal jugular catheter (Uldall catheter; Cook Critical Care, Bloomington, IN) or an arteriovenous fistula. A dialysate flow rate of 350 ml/min and a blood flow rate of 200 to 300 ml/min were used. F80 polysulfone dialyzers (Fresenius Medical care, Lexington, MA) or Exceltra 120 dialyzers (Baxter, Chicago, IL) were used. CHD patients received hemodialysis 3 times per week for 4 h, via similar vascular access. A blood flow rate of 400 ml/min, a dialysate flow rate of 500 to 750 ml/min, and F80 polysulfone dialyzers (Fresenius Medical Care, Lexington, MA, USA) were used. Unfractionated heparin was used for anticoagulation on CHD and NHD.
Two attempts were made to survey our eligible patient cohorts over a 3-mo period. CHD patients were provided the survey in-center, whereas NHHD patients received the survey by mail. The survey consisted of 122 questions. SF-12 was used to determine general self-perceived health. The Modified Appraisal of Self-Care Agency was used to measure a patients’ ability for self-care (9). The Spielberger State-Trait Anxiety Inventory for Adults was used as a measure of trait anxiety (10). The Multidimensional Scale of Perceived Social Support was used to measure the perceived social support from patients’ family and friends (11,12). (13) Specific questions related to NHHD included the patients’ perceptions of NHHD, their likelihood of NHHD adoption, and their perceived barriers to adoption.
For the qualitative ethnographic interviews, we used a purposive sampling method for recruitment with specific criteria for inclusion, as above (14). In this case, we sought “typical” patients who could be found in a nonrandomized qualitative study (15). The principal investigator for the study prepared a roster of recommended patients. A series of ethnographic interviews of three ESRD patient groups was undertaken. The three groups were NHHD patients, CHD patients, and predialysis patients. The interview guide was structured around the concepts of the Health Belief Model using the ethnographic interview approach (16). Specifically, lines of questioning were around the informant's (1) perceived susceptibility to and severity of their disease condition, (2) overall perceived threat to their health, (3) perceived benefits and barriers to adopting NHHD, (4) level of self-efficacy in performing NHHD, (5) process for taking action, and (6) external factors that affect their behavior or decision-making.
Statistical Analysis
Data are presented as mean ± SD. We used t test to evaluate differences in variables between the two modalities of renal replacement therapy. A two-tailed probability of <0.05 was required for significance, using SPSS 15 (Chicago, IL).
To evaluate the levels of interest in the adoption of NHHD, we performed a nonparametric analysis. Responses to Likert questions were recoded into a dichotomous variable. Chi-square cross-tabulation and Spearman correlations were generated to determine which factor showed a significant relation to the dependent variable. A within-subject logistic regression was performed to determine if any identified barrier had an interaction with a demographic variable.
Qualitative Analysis
Interviews were recorded and later transcribed verbatim. Interviews were conducted until it was felt that no new themes were introduced and the interviewer felt that saturation had been achieved (17). A general inductive method was used in the analysis of the transcripts. Transcripts were read repeatedly, and text segments were coded for potential themes. As the coding framework developed, transcripts were reanalyzed in light of new emerging themes. Major themes were derived that were relevant to the research question. Coding was performed along various factors of the Health Belief Model to form a priori codes, but was not limited to the theoretical framework. Coding was free not to assume any presuppositions. NVivo qualitative analysis software (QSR International, Doncaster, Australia) was used to facilitate the coding of the interview transcripts.
Results
The response rates for the survey were 85% for the NHHD group (56 of 66 patients), and 77% for CHD patients (153 of 199 eligible patients). A total of 91 of 290 CHD patients were considered ineligible for the study (Figure 1). For the qualitative component, saturation occurred at 20 interviews, comprising seven NHHD patients, six CHD patients, and seven predialysis patients.
Figure 1.
Patient recruitment.
NHHD patients were younger than CHD patients (47.0 ± 13.4 versus 55.4 ± 16.2 yr, P = 0.01). There were no significant differences with respect to gender or educational attainment. Compared with CHD patients, the majority of NHHD patients were nonimmigrant (60.7% versus 35.8%, P = 0.01). NHHD patients had lower prevalence of diabetes (12.5% versus 31.4%, P = 0.006) and tended to have lower burden of heart disease (10.7% versus 22.9%, P = 0.050). The prevalence of hypertension and cancer were similar in the two groups. (Table 1).
Table 1.
Demographic and comorbidity profile of CHD and NHHD patients
| Variable | CHD | NHHD | P |
|---|---|---|---|
| Gender (% male) | 56.3 | 60 | 0.490 |
| Age, mean (SD) | 55.4 (16.24) | 47.0 (13.38) | 0.001 |
| Education | |||
| elementary | 10.8% | 3.6% | |
| high School | 37.2% | 40% | 0.457 |
| college/undergradute | 35.8% | 40.0% | |
| postgraduate | 16.2% | 16.4% | |
| English as a first language | 66.9% | 78.6% | 0.103 |
| Born in Canada | 35.8% | 60.7% | 0.001 |
| Diabetes | 31.4% | 12.5% | 0.006 |
| Hypertension | 57.5% | 50.0% | 0.333 |
| Heart disease | 22.9% | 10.7% | 0.050 |
| Cancer | 6.5% | 7.1% | 0.876 |
CHD, conventional hemodialysis; NHHD, nocturnal home hemodialysis.
Compared with CHD patients, NHHD patients had better physical quality of life scores (41.47 ± 10.9 versus 34.73 ± 10.6, P < 0.0001), but had similar perceived mental health outcome (47.30 ± 11.1 versus 45.27 ± 11.3, P = 0.25). Interestingly, NHHD and CHD patients scored similarly in their measures of trait and state anxiety, appraisal of self-care agency, and perceived social support. (Table 2).
Table 2.
Comparison of mean (SD) self-perceived measures of health and psychosocial attributes between CHD and NHHD patients
| Measures | CHD | NHHD | P |
|---|---|---|---|
| SF-12 | |||
| Physical Component score | 34.73 (10.6) | 41.47 (10.9) | 0.000 |
| Mental Component score | 45.27 (11.3) | 47.30 (11.1) | 0.251 |
| Self-care agency | 3.85 (0.41) | 3.91 (0.33) | 0.394 |
| Perceived social support | 5.18 (1.49) | 5.42 (1.23) | 0.274 |
| Anxiety | |||
| state | 38.44 (13.39) | 38.15 (10.68) | 0.882 |
| trait | 39.68 (12.32) | 37.93 (10.19) | 0.350 |
CHD, conventional hemodialysis; NHHD, nocturnal home hemodialysis.
Despite similarities in self-perceived measures of health as NHD patients, CHD patients had little interest in NHHD adoption (1.68 ± 1.26, score of 5 indicates strong interest). CHD patients differed from the NHHD population in multiple domains, including lack of self-efficacy in performing NHHD, the lack of quality of care, lack of confidence in self-cannulation, and fear of a catastrophic event. (Table 3)
Table 3.
Differences in mean (SD) patient perception of nocturnal home hemodialysis
| Domain | CHD | NHHD |
|---|---|---|
| Self-cannulation (“I will be comfortable inserting the needles by myself”) | 2.11 (1.55)* | 3.57 (1.44) |
| Quality of care (“I will receive as good care as I would in the hospital”) | 2.34 (1.48)* | 4.10 (1.29) |
| Self-efficacy (“I will be able to perform the treatment [nocturnal hemodialysis] properly”) | 2.57 (1.52)* | 4.37 (1.19) |
| Fear of a catastrophic event (“I worry that something will go wrong during my treatment”) | 3.72 (1.54)* | 2.94 (1.47) |
P < 0.05
Logistic regression modeling was focused on CHD patient predictors of interest in the adoption of NHHD. The predictors entered into the model that were found to be significant were self-efficacy in performing NHHD, confidence in performing self-cannulation, and time on current therapy (negatively associated). The mean length of time on their current therapy for those patients who expressed an interest in NHHD was approximately 3 yr. For those with no interest, it was 5.3 yr. This finding was not related to patient age. Using a conditional stepwise method, we used the aforementioned independent variables to develop a model of predicting a CHD patient's interest in NHHD. The analysis included four iterations before resolving on a model that maximized the approximated R2 to 0.437 (Nagelkerke), explaining 43.7% of the variability in predicting interest in NHHD (Table 4).
Table 4.
Predictors of interest in the adoption of nocturnal home hemodialysis
| Predictor | β | SE β | Wald's χ2 | df | P | eβ |
|---|---|---|---|---|---|---|
| Constant | −5.469 | 1.527 | 12.823 | 1 | 0.000 | 0.004 |
| self-efficacy | 0.457 | 0.226 | 4.071 | 1 | 0.044 | 1.579 |
| self-cannulation | 0.450 | 0.198 | 5.171 | 1 | 0.023 | 1.568 |
| time on current therapy (in years) | −0.162 | 0.076 | 4.627 | 1 | 0.031 | 0.850 |
| Trait Anxiety | 0.073 | 0.025 | 8.762 | 1 | 0.003 | 1.076 |
| Test | χ2 | df | p | |||
| Hosmer and Lemeshow | 9.866 | 8 | 0.275 |
|
Logistic regression model–Classification Table (cut value of 0.5)
| ||||
|---|---|---|---|---|
| Observed | Predicted | |||
| Interest in NHD | Percentage Correct | |||
| Yes | No | |||
| Interest in NHD | Yes | 15 | 14 | 51.7 |
| No | 8 | 54 | 87.1 | |
| Overall Percentage | 75.8 | |||
Sensitivity = 15/(15 + 14)% = 51.7%. Specificity = 54/(8 + 54)% = 87.1%. False positive 8/(8 + 15)% = 34.8%. False negative = 14/(14 + 54)% = 20.6%.
Complementing the quantitative analysis, the main themes identified in the qualitative component of the study as barriers to the adoption of NHHD were burden on family members, fear of self-cannulation, fear of a catastrophic event, and low self-efficacy.
Perceived Burden on Family Members
Most patients were aware that a decision to adopt NHHD would have a significant impact on their family members and cohabitants. In multiple instances, family members who were the primary caregivers voiced their lack of appreciation of the extent of the patients’ condition until the therapy was administered in the home. Family members might be fearful of the notion of complex home therapy and that there will be additional responsibility of caring for the patient.
Patient NHHD2: I know it was very hard for my family. My mother was petrified. I don't think she wanted me to, but I kind of said, you know, I need to do it.
Fear of Self-Cannulation
Interviewer: So, with the proper training you think you could do it, you could manage doing the needles yourself, setting up the machine?
Patient CHD2: Oh, I'm afraid of needles.
Interviewer: You're afraid of needles so that would be a problem for you doing the needles?
Patient CHD2: Yeah, I don't like needles.
Perhaps, the most often reported perceived barrier was the act of self-cannulation. Patients recognized the need of frequent cannulation when adopting NHHD. The fear of self-cannulation extended beyond the perception of pain to include the potential occurrence of mishaps and complications.
Fear of a Catastrophic Event in the Absence of Nursing Support
Patients also expressed a fear of a life-threatening event associated with NHHD. In particular, patients who had experienced prior medical emergencies articulated potential problems with the adoption of NHHD. There was also the realization of the loss of nursing support during critical situations, which was perceived as a loss of safety.
Patient NHHD5: If anything happens, you don't have the immediate support. There is a certain degree of comfort in hospital, you know, if something goes wrong there is somebody who knows what they are supposed to do, in place, to help you overcome this. At home, there's nobody. There's just yourself.
Lack of Self-Efficacy
Patient CHD6: I'm still not confident to do it on my own. I felt better going to the hospital to get the doctor to check me regularly.
In addition to determining the benefits and barriers of a therapy, patients must weigh their self-efficacy to perform such therapy. Self-efficacy in this context can be defined as the estimation of one's capacity to engage in behaviors that contribute to desired health outcomes (18).
Discussion
Patients’ perception and attitudes toward NHHD are arguably the most important determinants of the widespread applicability of this form of renal replacement therapy. Despite the clinical improvements of NHHD, home delivery of dialysis may pose significant challenges and barriers to a chronically ill population. The present study used a mixed-method strategy to identify potential differentiating characteristics between CHD and NHHD patients by contrasting their demographics, psychosocial attributes, anxiety measure, quality of life, and perceptions of NHHD therapy. Despite differences in patient demographics, CHD and NHHD patients scored similarly in most of the aforementioned domains except for their perceptions of NHHD. CHD patients had uniformly low interest in adopting NHHD. It should be noted that our CHD population represents a group from which NHHD patients had already been extensively recruited and hence may allow us to ascertain the difference between the two patient populations. Specifically, the barriers to adoption that CHD patients identified included lack of self-efficacy in performing NHHD, lack of confidence in self-cannulation, perceived lack of quality of care, and the length of time on the current therapy, indicating that the longer patients remain on CHD, the less likely they are to adopt NHHD.
Similar themes using a qualitative approach revealed concerns surrounding burden on family members, fear of self-cannulation, fear of a catastrophic event, and low self-efficacy. Given that our CHD population has previously been recruited for NHHD, these fears may represent a natural accommodation for CHD patients, forming a pretext to remain on their current therapy. Taken together, our study represents a systematic analysis of patient-perceived barriers to the adoption of NHHD, which are primarily the fears and burden of undertaking this form of home hemodialysis.
Other important findings include that patient's level of educational attainment does not appear to be a factor in adoption of NHHD, and that English as a second language does not appear to be a barrier. The use of anxiety as a measure to contraindicate NHHD is also not supported.
Limited studies have determined the willingness of CHD patients to convert to any forms of home hemodialysis. To date, most investigators have focused on the notion of early referral coupled with predialysis education in patients with chronic kidney disease (CKD). Although CKD is admittedly an important public health issue, it is tempting to speculate that CHD patients may benefit even more from conversion to intensive hemodialysis. Choosing a dialysis modality for most ESRD patients is a difficult decision. Given that our study has identified the patients’ perceived fears and burden of undertaking NHHD, are there strategies to reconcile and mitigate these concerns? Self-cannulation was highlighted as a central fear by the CHD population. It is interesting to note that the early Toronto NHHD experience as reported by Uldall et al. (19) included exclusively patients who dialyzed via permanent indwelling catheters to facilitate the transition from CHD to NHHD. Recently, our group has also implemented a step-wise approach to those patients who are overwhelmed by the multiple tasks of learning dialysis and self-cannulation. To date, the optimal strategy to teach and learn NHHD and self-cannulation has not been studied systematically. The risk benefit ratio of the various types of vascular accesses in home hemodialysis requires further clarification.
The second uniform barrier that emerged from our analysis was the lack of confidence in conducting NHHD. Hemodialysis is a technically complex procedure. Lehoux has previously reported on patients’ perceived technical challenges of various home-based therapies, such as peritoneal dialysis and oxygen therapy (20,21). Consistent with prior published studies, our results suggest that most patients may be overwhelmed by the complexity of present medical technology and that future home-based medical devices will require a greater focus on patient-centric design to improve patient perception and confidence. Fear of a catastrophic event at home was the last common theme emerged from our survey and interviews. Given that the majority of hemodialysis performed in North America is situated in a clinical setting, the perception of “loss of safety” should not come as a surprise. In the future, novel application of remote monitoring technology and further patient education are needed to potentially mitigate these concerns.
It is interesting to note that CHD and NHD patients had similar self-perceived measures of health. Aside from the physical component of SF12 scores, the two groups of ESRD patients did not differ in their psychosocial attributes, anxiety, and mental quality of life scores. Previous studies have examined the impact of NHHD on quality of life and other psychosocial metrics, with heterogeneous results (22–28). Some studies endorsed enthusiastic improvements, whereas others such as Heidenheim et al., using SF-36 as an indicator, showed a deterioration in mental quality of life scores over time for NHHD patients. Our data do not support the notion that augmented solute clearance alone determines an individual's perceived health-related quality of life. In addition, our study confirms that the choice of renal replacement modality is not simply a reflection of an individual's psychosocial attributes, but rather a complex interplay between the patient's health state and the perceived benefits and barriers to adopting the chosen therapy.
Our center has few short daily home hemodialysis (SDHD) patients. However, given the nature of the themes derived from the data, we speculate that patients considering SDHD would have similar concerns as those considering NHHD. It is possible that SDHD candidates may express the fear of a catastrophic event to a lesser degree than those considering NHHD, which requires further investigations.
Our study is limited by its observational design. Other populations, such as CKD and peritoneal dialysis patients, could also have been studied. A future, prospective study of NHHD dropouts may prove useful to determine actual rationale for discontinuing the therapy. Currently there are insufficient patients who discontinued home hemodialysis for a proper evaluation, as the dropout rate is only 3.4% over a 10-yr period. We have also noted that predialysis patients had difficulty articulating their opinions on modality choice as they had little knowledge of the specifics of the various dialytic therapies. Their lack of experience and knowledge of the ESRD therapies limited their participation in the qualitative study, and thus it was decided to exclude them from the quantitative component of the evaluation.
In addition, few clinical studies have relied on the use of a mixed-method design. Our study highlighted the unique complementary nature of combining quantitative and qualitative approaches to assess our patients’ perception to NHHD. Existing instruments for measuring patient self-care agency and social support may lack the sensitivity required for determining a patient's appropriateness for NHHD. The implementation of a mixed-method approach enhanced the robustness of the present results.
This is the first comprehensive mixed-methods study to specifically investigate the patient-perceived barriers of NHHD. Beyond policy making and determining selection criteria, these findings add to the existing knowledge in the implementation of a NHHD program, including predialysis counseling, therapy choice, dialysis training, and continual quality assurance.
Disclosures
None.
Acknowledgments
The authors would like to thank the patients and care providers who participated in this study. Dr. Chan holds the R Fraser Elliott Chair in Home Dialysis. Bell University Labs at the University of Toronto supported this study through grant funding (87285).
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “New Options to Improve Hemodialysis Patient Outcomes,” on pages 694–695.
References
- 1.Hanly PJ, Gabor JY, Chan C, Pierratos A: Daytime sleepiness in patients with CRF: Impact of nocturnal hemodialysis. Am J Kidney Dis 41: 403–410, 2003 [DOI] [PubMed] [Google Scholar]
- 2.Chan CT: Nocturnal hemodialysis: an attempt to correct the “unphysiology” of conventional intermittent renal replacement therapy. Clin Invest Med 25: 233–235, 2002 [PubMed] [Google Scholar]
- 3.Gonzalez-Perez JG, Vale L, Stearns SC, Wordsworth S: Hemodialysis for end-stage renal disease: A cost-effectiveness analysis of treatment-options. Int J Technol Assess Health Care 21: 32–39, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Lee H, Manns B, Taub K, Ghali WA, Dean S, Johnson D, Donaldson C: Cost analysis of ongoing care of patients with end-stage renal disease: The impact of dialysis modality and dialysis access. Am J Kidney Dis 40: 611–622, 2002 [DOI] [PubMed] [Google Scholar]
- 5.McFarlane PA: Reducing hemodialysis costs: Conventional and quotidian home hemodialysis in Canada. Semin Dial 17: 118–124, 2004 [DOI] [PubMed] [Google Scholar]
- 6.McFarlane PA, Bayoumi AM, Pierratos A, Redelmeier DA: The quality of life and cost utility of home nocturnal and conventional in-center hemodialysis. Kidney Int 64: 1004–1011, 2003 [DOI] [PubMed] [Google Scholar]
- 7.MacGregor MS, Agar JW, Blagg CR: Home haemodialysis-international trends and variation. Nephrol Dial Transplant 21: 1934–1945, 2006 [DOI] [PubMed] [Google Scholar]
- 8.McLaughlin K, Manns B, Mortis G, Hons R, Taub K: Why patients with ESRD do not select self-care dialysis as a treatment option. Am J Kidney Dis 41: 380–385, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Fok MS, Wong TK: Testing Orem's Self-Care Agency and Basic Conditioning Factors in a Chinese community undergoing haemodialysis. Contemp Nurse 15: 262–272, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Spielberger CD, O'Neil HF, Jr., Hansen DN: Anxiety, drive theory, and computer-assisted learning. Prog Exp Pers Res 6: 109–148, 1972 [PubMed] [Google Scholar]
- 11.Dahlem NW, Zimet GD, Walker RR: The Multidimensional Scale of Perceived Social Support: A confirmation study. J Clin Psychol 47: 756–761, 1991 [DOI] [PubMed] [Google Scholar]
- 12.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA: Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess 55: 610–617, 1990 [DOI] [PubMed] [Google Scholar]
- 13.Alvarez-Ude F, Valdes C, Estebanez C, Rebollo P: Health-related quality of life of family caregivers of dialysis patients. J Nephrol 17: 841–850, 2004 [PubMed] [Google Scholar]
- 14.Patton MQ, Patton MQ: Qualitative Evaluation and Research Methods, 2nd Ed. Newbury Park, CA, Sage Publications, 1990
- 15.Spradley JP: The Ethnographic Interview. Orlando, FL, Harcourt, Brace, Janovich, 2003
- 16.Bowes JE. Communication and Community Development for Health Information: Constructs and Models for Evaluation. Seattle, WA, National Network of Libraries of Medicine, Pacific Northwest Region, 1997
- 17.Padgett D: Qualitative Methods in Social Work Research: Challenges and Rewards. Thousand Oaks, CA, Sage Publications, 1998
- 18.Tsay SL, Healstead M: Self-care self-efficacy, depression, and quality of life among patients receiving hemodialysis in Taiwan. Int J Nurs Stud 39: 245–251, 2002 [DOI] [PubMed] [Google Scholar]
- 19.Uldall R, Ouwendyk M, Francoeur R, Wallace L, Sit W, Vas S, Pierratos A: Slow nocturnal home hemodialysis at the Wellesley Hospital. Adv Ren Replace Ther 3: 133–136, 1996 [DOI] [PubMed] [Google Scholar]
- 20.Lehoux P: Patients’ perspectives on high-tech home care: a qualitative inquiry into the user-friendliness of four technologies. BMC Health Serv Res 4: 28, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lehoux P, Saint-Arnaud J, Richard L: The use of technology at home: What patient manuals say and sell vs. what patients face and fear. Sociol Health Illn 26: 617–644, 2004 [DOI] [PubMed] [Google Scholar]
- 22.Ageborg M, Allenius BL, Cederfjall C: Quality of life, self-care ability, and sense of coherence in hemodialysis patients: a comparative study. Hemodial Int 9[Suppl 1]: S8–S14, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Courts NF: Psychosocial adjustment of patients on home hemodialysis and their dialysis partners. Clin Nurs Res 9: 177–190, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Culleton BF, Walsh M, Klarenbach SW, Mortis G, Scott-Douglas N, Quinn RR, Tonelli M, Donnelly S, Friedrich MG, Kumar A, Mahallati H, Hemmelgarn BR, Manns BJ: Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life: A randomized controlled trial. JAMA 298: 1291–1299, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Fong E, Bargman JM, Chan CT: Cross-sectional comparison of quality of life and illness intrusiveness in patients who are treated with nocturnal home hemodialysis versus peritoneal dialysis. Clin J Am Soc Nephrol 2: 1195–1200, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Heidenheim AP, Muirhead N, Moist L, Lindsay RM: Patient quality of life on quotidian hemodialysis. Am J Kidney Dis 42: 36–41, 2003[suppl 1] [DOI] [PubMed] [Google Scholar]
- 27.Kooistra MP, Vos J, Koomans HA, Vos PF: Daily home haemodialysis in The Netherlands: Effects on metabolic control, haemodynamics, and quality of life. Nephrol Dial Transplant 13: 2853–2860, 1998 [DOI] [PubMed] [Google Scholar]
- 28.Walsh M, Culleton B, Tonelli M, Manns B: A systematic review of the effect of nocturnal hemodialysis on blood pressure, left ventricular hypertrophy, anemia, mineral metabolism, and health-related quality of life. Kidney Int 67: 1500–1508, 2005 [DOI] [PubMed] [Google Scholar]