Abstract
Background and objectives: Changes in ESRD reimbursement policy, including proposed bundled payment, have raised concern that dialysis facilities may use “cherry picking” practices to attract a healthier, better insured, or more adherent patient population.
Design, setting, participants, & measurements: As part of a national survey to measure beliefs about drivers of quality in dialysis, respondents were asked about their perceptions of cherry picking, including the frequency and effect of various cherry picking strategies on dialysis outcomes. We surveyed a random sample of 250 nurse members of the American Nephrology Nurses Association, 250 nephrologist members of the American Medical Association, 50 key opinion leaders, and 2000 physician members of the Renal Physicians Association. We tested hypothesized predictors of perception, including provider group, region, age, experience, and the main practice facility features.
Results: Three-quarters of respondents reported that cherry picking occurred “sometimes” or “frequently.” There were no differences in perceptions by provider or facility characteristics, insurance status, or health status. In multivariable regression, perceived cherry picking was 2.8- and 3.5-fold higher in the northeast and Midwest, respectively, versus the west. Among various cherry picking strategies, having a “low threshold to ‘fire’ chronic no-shows/late arrivers,” and having a “low threshold to ‘fire’ for noncompliance with diet and meds” had the largest perceived association with outcomes.
Conclusions: Under current reimbursement practices, dialysis caregivers perceive that cherry picking is common and important. An improved understanding of cherry picking practices, if evident, may help to protect vulnerable patients if reimbursement practices were to change.
In hopes of stimulating quality improvement, the Centers for Medicare and Medicaid Services (CMS) and private payers have placed increased emphasis on aligning financial incentives with quality through pay-for-performance (P4P) or value-based purchasing initiatives. Although some of these initiatives have shown promise in improving process-based measures, the long-term outcomes and economic effects of these policy changes remain uncertain (1–4). Prior experiences with changes in reimbursement policy suggest that insufficient funding or poorly designed incentive mechanisms can result in unintended and unwanted consequences (5,6).
One potential consequence is “cherry picking,” which is a behavior rooted in the basic economic concept of adverse selection. Adverse selection results from imperfect markets in which there are information asymmetries among buyers and sellers. In health care, insurers and providers can try to protect themselves from these information asymmetries by avoiding sicker patients or preferentially attracting healthier patients. Payment systems that do not address adverse selection may limit access to those patients who are sicker or require more complex care.
Dialysis payment policies could promote cherry picking through various mechanisms (7–9). In particular, payments from CMS have not historically been adjusted for case mix or severity of illness. In addition, private insurers traditionally reimburse at higher rates compared with Medicare. Because an empty chair in a dialysis unit is a net loss of revenue, and because private insurers pay more than CMS, there may be an incentive to attract and accept privately insured and/or healthier patients who are potentially less likely to miss appointments (resulting in nonreimbursed dialysis sessions) because of hospitalization.
Moreover, CMS adopted a new case-mix adjustment system in 2005 based on age and body size (6). Under this system, Medicare modifies reimbursement on the basis of patient characteristics. Correction factors increase reimbursement for facilities that care for younger and older individuals, and for people of very large or very low body mass index. Some observers have argued that dialysis facilities, in response to the new case-mix adjustment payment, may alter their patient recruitment strategies and place the most vulnerable populations at risk (10).
A case-mix adjustment that evaluates the intensity of interventions and acuity of patients, conversely, may lead to a more equitable distribution of resources for ESRD care (8). For example, a study that used a modified Charlson comorbidity index to predict outcomes and costs in dialysis patients demonstrated an 87% cost differential between providing care to patients with low versus high comorbidity scores (11). A well designed case-mix adjustment can provide a safeguard to ensure that providers do not turn away sicker patients or those who require more complex care. Yet even a Charlson-based system will have shortcomings, because nonadherence is not a component of the Charlson score, and this index will not adjust for disparities in achieving optimal targets due to patient choices in diet or adherence to dialysis sessions.
The regulatory landscape has recently been altered further with the passage of the Medicare Improvements for Patients and Providers Act of 2008, which calls for a bundled payment system to be in place for ESRD by 2011. Although the details of the payment bundling remain under discussion, the act ensures that the federal government will seek to streamline ESRD payments by bundling resources into one payment. Because dialysis facilities already operate close to the margin, and because Medicare reimbursements are often below the cost of providing care, the act may further burden private payers with underwriting dialysis facilities. Moreover, bundling may also drive dialysis organizations to prefer better insured and more compliant patients, because these patients may help to maximize profits under the bundling regulations.
In light of this background, including the advent of P4P and payment bundling, we initiated the Identifying Best Practices in Dialysis (IBPiD) study to help define drivers of quality care. IBPiD is a multidisciplinary research effort conducted through the University of California–Los Angeles (UCLA) in collaboration with the Renal Physicians Association (RPA) and the American Nephrology Nurses Association (ANNA) that aims to identify best practices that may improve facility-level achievement of clinical performance measures and overall outcomes in dialysis patients (12). As a part of IBPiD, we conducted a national survey in which we elicited caregiver perceptions regarding the extent and consequences of cherry picking in dialysis care.
Materials and Methods
Survey Overview
The IBPiD study is an ongoing, multiphase, health services research project that aims to identify modifiable practice patterns that drive outcomes in dialysis. The three-phase study has been described in detail elsewhere (10). The study includes a national survey that measured provider beliefs about drivers of quality in dialysis. The survey contains a module regarding cherry picking practices, including perceived frequency and effect of various cherry picking strategies on dialysis facility achievement of clinical performance measures, such as dialysis adequacy, mineral metabolism indices, anemia management, albumin levels, and interdialytic weight gain, among others. In this module, respondents were first asked the following question: “Because dialysis facilities are judged on their ability to achieve key performance levels, it is possible that some facilities might choose to accept healthier or more compliant patients. In other words, some facilities might ‘cherry pick’ their patients. Do you think this happens?” Answers were recorded on a five-point scale with the following options: “Yes—a lot of times in many facilities;” “yes—a lot of times in few facilities;” “yes—sometimes;” “yes—rarely;” and “no—never.” We subsequently dichotomized responses as positive (“sometimes” or more frequently) or negative (“rarely” or “never”).
Respondents were then asked to assess the perceived effect of five different cherry picking practices on facility-level outcomes, including:
Preferentially accepting privately insured patients
Having a low threshold to “fire” patients who are noncompliant with diet and medications
Having a low threshold to fire patients who are chronic “no-shows” or late arrivers for dialysis
Having a low threshold to fire patients who are disruptive to other patients and the staff
Discouraging acceptance of bed-bound patients from nursing facilities by failing to have dialysis beds in lieu of only having chairs
Respondents recorded perceived impact ratings onto a nine-point modified RAND appropriateness scale in which 1 = ”no impact on outcomes” to 9 = “large impact on outcomes.” This scale was originally developed by investigators at UCLA and the RAND Corporation to evaluate appropriateness of different types of medical care (13,14). It has been used and validated as a measure of provider perceptions of various medical practices (12,15,16). The RAND scale may be trichotomized with the following interpretation: 1 to 3 = “generally low impact;” 4 to 6 = “moderate impact;” and 7 to 9 = “generally high impact.” Therefore, using this interpretation scheme, an average score above 6.5 indicates that survey respondents believed that cherry picking practice is of generally high impact.
Sampling Frame
We surveyed a random sample of 250 nurse members of ANNA, a random sample of 250 community nephrologists from the American Medical Association (AMA) Masterfile, 2000 clinical members of RPA, and 50 academic key opinion leaders in nephrology care selected on the basis of publication records and membership on clinical practice guideline development committees. Assuming 15 subjects for each of 10 potential independent predictors in multivariable regression analysis (see Analytic Statistics below), we estimated that a minimum of 150 subjects would be required to complete the survey to avoid overmatching of the regression models. Assuming a 40% response rate, we needed to survey at least 380 providers in the sampling frame.
Survey Distribution and Follow-Up Procedures
Respondents initially received the survey electronically using an online questionnaire platform (Survey Monkey software, http://www.surveymonkey.com). Physicians received e-mails with cover letters and a link to the online survey. After 2 wk, nonresponders received a follow-up e-mail. Finally, 1 wk after the second e-mail correspondence, a paper version of the questionnaire was mailed to nonresponders. Using baseline data from RPA, ANNA, and AMA, we compared responders to nonresponders across key covariates, including age, region, practice setting, and years in practice.
Analyses
For the cherry picking frequency item, we first calculated the proportion of respondents endorsing each of the five prespecified levels. We then compared dichotomous endorsement of cherry picking among provider groups, as described above. We compared the proportions across provider groups with a χ2 test. We then performed multivariable logistic regression analysis to determine if provider or practice-type characteristics predicted perception about dichotomized cherry picking frequency. Independent variables included provider age, gender, years in practice, region of practice, and each respondent's primary dialysis facility characteristics such as unit type (small versus large dialysis organization—as defined by the respondent) and size. For each predictor variable we calculated the adjusted odds ratio with 95% confidence intervals (CI) from the model parameter estimates and standard errors. Two-tailed P values <0.05 were considered statistically significant.
For the cherry picking impact items, we calculated the mean nine-point RAND score for each cherry picking strategy, and highlight strategies achieving a mean score above 6.5, as described above. We compared mean scores among provider groups using unadjusted ANOVA to evaluate for systematic differences in perception. All analyses were performed using SAS for Windows v9.2.
Results
Sample Characteristics
Table 1 displays the characteristics of the survey respondents. Three hundred eighty-four respondents returned their surveys, including 25 of 50 key opinion leaders (50% response rate), 62 of 250 AMA nephrologists (25% response rate), 203 of 2000 RPA nephrologists (10% response rate), and 95 of 250 ANNA nurses (38% response rate). To screen for potential systematic differences between responders and nonresponders, we compared groups across age, region, practice setting, and years in practice. There were no statistically significant differences between responders and nonresponders for these variables.
Table 1.
Demographic and practice-pattern information of respondents
| Variable | Dialysis Opinion Leaders (n = 25) | Community Nephrologists (AMA + RPA) (n = 297) | ANNA Nurses (n = 95) | P |
|---|---|---|---|---|
| Age (mean yr ± SD) | 53 ± 9 | 50.4 ± 10 | 50.4 ± 7 | 0.81 |
| Male gender (%) | 95 | 86 | 4 | <0.001 |
| Primary practice is in large dialysis organization (%) | 41 | 69 | 40 | <0.001 |
| Years of experience in dialysis (mean yr ± SD) | 17 ± 11 | 14 ± 9 | 8 ± 7 | <0.001 |
| Based primarily in university/academic practice setting (%) | 72 | 14 | 1 | <0.001 |
| Number of dialysis patients seen/wk | 52.6 ± 26 | 65.9 ± 45 | 66.9 ± 60 | 0.11 |
| Geographic location (%) | ||||
| west | 20 | 22 | 21 | 0.91 |
| Midwest | 40 | 18 | 20 | 0.07 |
| south | 15 | 37 | 29 | 0.09 |
| northeast | 25 | 23 | 30 | 0.73 |
Perceived Frequency of Cherry Picking
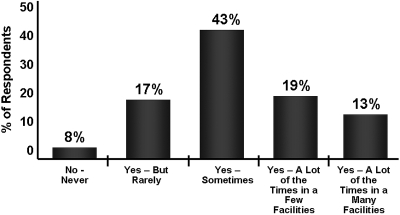
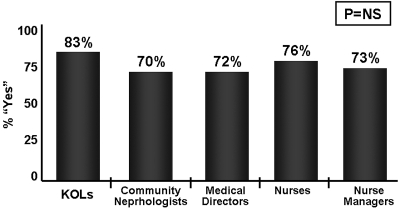
Figure 1 provides the breakdown of responses regarding the perceived frequency of cherry picking in the ESRD system. More than three-quarters of respondents across groups believed that cherry picking occurs at least sometimes, whereas fewer than 1 in 10 believed that cherry picking never occurs (8%). There were no differences in perceptions by provider or facility type. In multivariable regression, perceived cherry picking was 2.8- (95% CI = 1.2 to 6.4) and 3.5- (95% CI = 1.4 to 9.0) fold higher in the northeast and Midwest, respectively, versus the western region of the United States. Figure 2 provides the breakdown of perceived cherry picking frequency by group. Although there were numeric differences across provider groups (e.g., 83% of experts believed cherry picking occurs at least sometimes, whereas 70% of community nephrologists held this belief), the differences across groups were not statistically significant.
Figure 1.
Perceived frequency of cherry picking across full provider sample.
Figure 2.
Perceived frequency of cherry picking by provider group. KOLs, key opinion leader.
There were no significant differences in perceived cherry picking practices by facility type (large dialysis organization versus non-large dialysis organization), facility size, perceived staffing levels, or a variety of physician characteristics, including age, sex, years in practice, and practice setting.
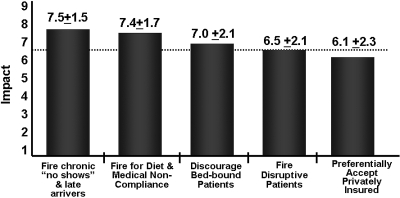
Perceived Effect of Cherry Picking
Figure 3 provides data on the perceived effect of cherry picking practices on outcomes. Among the five evaluated cherry picking practices, having a low threshold to fire chronic no-shows/late arrivers and having low threshold to fire for noncompliance with diet and meds had the largest perceived effect on dialysis outcomes. Accepting privately insured patients had the lowest perceived effect (6.1 ± 2.3). On average, all cherry picking practices were viewed as having moderate to large effects on outcomes. There were no significant differences in perceived effect across provider groups.
Figure 3.
Perceived effect of cherry picking strategies on dialysis outcomes. The perceived effect of each potential cherry picking strategy was ranked by each respondent using a nine-point modified RAND scale in which 9 = highest impact and 1 = lowest impact. Mean scores exceeding 6.5 (dotted line) denote practices that are generally high impact on patient outcomes, as described in the text. Four of the five strategies were rated as being of generally high impact on dialysis outcomes.
Discussion
In a national survey of dialysis care providers, most respondents believed that cherry picking occurs in dialysis facilities, independent of ownership status. Although we did not find evidence of cherry picking based on insurance or health status, cherry picking practices are perceived to have a large effect on dialysis outcomes. Although there are regional differences in perceived cherry picking frequency, there is significant agreement across respondents as well as practice type regarding the frequency and effect of cherry picking in the ESRD population.
Because this survey measures perceptions of providers in dialysis facilities, it is hypothesis generating and thus only reflects beliefs. It is possible that the perceptions expressed in this survey may not reflect reality. Nonetheless, most of the respondents indicated that cherry picking is common in the ESRD program and did so in a confidential, nonreportable survey. It is reasonable to assume that the views expressed by hundreds of dialysis stakeholders across several regions and provider groups may reflect some element of truth. Future research should investigate the degree to which provider perception matches reality. In the meantime, our hypothesis-generating data indicate that cherry picking may be a prevalent practice in the ESRD system. We believe these data provide sufficient rationale to investigate the hypothesis further. While awaiting these future studies, it is reasonable to enact efforts now to proactively identify and correct, where tenable, cherry picking practices.
Because P4P and bundled payments may create additional incentives for cherry picking, it is critical to understand the effect of payment structures on patient selection and provider practices. Reimbursement policies that do not adequately fund the provision of dialysis may have the perverse effects of promoting inappropriate underuse of essential resources in the sickest and most disadvantaged patients while promoting inappropriate overuse of nonessential resources in the healthiest and best insured patients. Indeed, there is already evidence of variation in the quality of care provided to dialysis patients across sociodemographic strata. For example, black patients are less likely to be treated with peritoneal dialysis, are less likely to receive a fistula than a graft, and may have lower urea reduction ratios and hematocrit levels compared with other ESRD patients (17–19). Payment systems that promote adverse selection behavior may, in fact, exacerbate these disparities in care and further disadvantage more vulnerable dialysis patients.
We found variations in the perceived frequency of cherry picking by region. Specifically, perceived cherry picking was 2.8- and 3.5-fold higher in the northeast and Midwest, respectively, compared with the western United States. Regional variations in medical practice are well documented throughout all areas of medicine (20). However, our data reveal that perceptions vary widely between regions—more than would be expected by chance alone. It is unclear why perceptions might vary so dramatically. Possibilities include a mere sampling error in the survey, possible case-mix variations in patient populations between regions, or true differences in perception that reflect acculturated practice patterns within regions. Evidence from other areas of medicine reveal that variation in medical practice across regions is a general indicator of poor consensus and may indicate that inadequate care is being provided in some settings (13). Future research should investigate whether and why there may be regional variations in cherry picking practices in dialysis. If such variations exist, investigators should aim to identify the root causes of these variations and, assuming the causes are modifiable, seek to correct potential inequities across regions.
Our analysis has several limitations. First, as noted above, the survey responses may not be reflective of actual decision-making in clinical practice. The gold standard for assessing process of care is to directly observe real-time decision-making in clinical practice. However, this approach is also limited because of the Hawthorne effect, in which providers and organizations artificially alter practice when knowingly observed. Standardized patients and medical record data abstraction are alternatives (21,22). Notably, provider surveys are validated as an accurate surrogate for chart abstraction and standardized patients and therefore often accurately reflect actual decision-making (23).
Our survey is further limited by the relatively low response rate. There may be systematic differences between responders and nonresponders. Nonresponders typically cite several reasons for their failure to participate, including not receiving the survey, believing the survey did not pertain to their practice, lacking sufficient time, or simply choosing not to participate. We cannot know the specific reasons for nonresponse to this survey. It is possible that nonresponders were too busy, did not receive the e-mail or paper surveys, or had other systematic differences (i.e., do not evaluate enough ESRD patients to feel comfortable taking the survey, do not participate in academic studies, are not clinically active, etc.) Using data from the AMA Masterfile, we were able to confirm that nonresponders were similar to responders in terms of age, gender, years in practice, practice setting, and geographic location. This suggests that respondents were not systematically different from nonrespondents for key measured characteristics. Nonetheless, there may be unmeasured factors, including those described above, that remain systematically different between groups. As with any provider survey, a higher response rate could have potentially altered the results, although it is difficult to accurately predict in what direction, if any, the results would be different.
Because nonadherence in ESRD is closely related to socioeconomic status, it is possible that P4P could disproportionately penalize dialysis units and nephrologists providing care to underserved populations. This could threaten the viability of dialysis units located in socioeconomically disadvantaged areas. Because P4P could further marginalize underserved communities, it would be useful to evaluate the zip codes of survey respondents to establish whether perceived cherry picking correlates with socioeconomic regions—in contrast to wider national regions. However, we did not collect zip codes in our survey and are not able to conduct an analysis to evaluate the socioeconomic characteristics of areas where respondents practice. Future research should establish whether cherry picking varies by socioeconomic regions—not just by national regions as we have found here.
Our analysis does not address where in the delivery system cherry picking may be most evident (e.g., provider level, administrative level, etc.). If cherry picking behavior exists, as strongly suggested by this survey, additional studies must identify at what point in the care process it occurs. Understanding where in the system and by whom patients are denied access would allow for targeted programs to reduce or eliminate cherry picking in dialysis.
Well designed payment systems will reward quality while maintaining appropriate accountability and fairness for providers. Future policies must emphasize adequate payment for dialysis and case-mix adjustment to ensure fairness and limit cherry picking practices (6,8,17). Cherry picking practices should be strongly discouraged. Developing clinical performance measures highlighting fair and equitable access to dialysis care for all persons should be among the highest priorities of the United States ESRD program.
Disclosures
None.
Acknowledgments
Dr. Spiegel is supported by Veteran's Affairs Health Services Research and Development (HSR&D) Career Development Transition Award (RCD 03-179-2), and by the CURE Digestive Disease Research Center (NIH 2P30 DK 041301-17). Dr. Desai is supported by a training grant from the Agency for Healthcare Research and Quality (AHRQ). Support for this investigator-initiated study was provided by a research grant from Amgen, Inc. The principal investigator, Dr. Spiegel, maintained full control over all aspects of the study design, implementation, data collection, data analysis, data interpretation, and manuscript preparation. This study was presented as an oral presentation at the 2007 annual meeting of the American Society of Nephrology. The opinions and assertions contained herein are the sole views of the authors and are not to be construed as official or as reflecting the views of the Department of Veteran Affairs.
Amar Desai: Study design, study implementation, data collection, data interpretation, manuscript preparation.
Roger Bolus: Study design, study implementation, data collection, data analysis, manuscript review.
Allen Nissenson: Study design, data interpretation, manuscript review
Glenn Chertow: data interpretation, manuscript preparation and review
Sally Bolus: Study design, data interpretation, manuscript review
Matthew Solomon: Study design, data interpretation, manuscript review
Osman Khawar: Study design, data interpretation, manuscript review
Matthew Gitlin: Data interpretation, manuscript review
Jennifer Talley: Study implementation, data collection
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Rosenthal MB, Fernandopulle R, Song HR, Landon B: Paying for quality: providers’ incentives for quality improvement. Health Aff (Millwood) 23: 127–141, 2004 [DOI] [PubMed] [Google Scholar]
- 2.Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S: Does pay-for-performance improve the quality of health care? Ann Intern Med 145: 265–272, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis, E, Hiroeh U, Roland M: Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med 355: 375–384, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Epstein AM: Paying for performance in the United States and abroad. N Engl J Med 355: 406–408, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal MB, Frank RG, Li Z, Epstein AM: Early experience with pay-for-performance: From concept to practice. JAMA 294: 1788–1793, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Desai AA, Garber AM, Chertow GM: Rise of pay for performance: Implications for care of people with chronic kidney disease. Clin J Am Soc Nephrol 2: 1087–1095, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Himmelfarb J, Pereira BJ, Wesson DE, Smedberg PC, Henrich WL: Payment for quality in end-stage renal disease. J Am Soc Nephrol 15: 3263–3269, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Chertow GM: Leveling the “paying” field in end-stage renal disease. Am J Med 108(8): 666–668, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Himmelfarb J, Chertow GM: Medicare ESRD prospective payment system: Weighing the evidence. J Am Soc Nephrol 16: 1164–1165, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Nissenson AR: Models of capitated payment for endstage renal disease. Am J Med 110: 504–505, 2001 [DOI] [PubMed] [Google Scholar]
- 11.Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML: A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med 108: 609–613, 2000 [DOI] [PubMed] [Google Scholar]
- 12.Desai AA, Bolus R, Nissenson A, Bolus S, Solomon MD, Khawar O, Gitlin M, Talley J, Spiegel BM: Identifying best practices in dialysis care: Results of cognitive interviews and a national survey of dialysis providers. Clin J Am Soc Nephrol 3: 1066–1076, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brook RH, Lohr KN: Efficacy, effectiveness, variations, and quality. Boundary-crossing research. Med Care 23: 710–722, 1985 [DOI] [PubMed] [Google Scholar]
- 14.Fitch K; Bernstein SJ, Aguilar, MS, Burnand B, Ramon LaCalle J, Lazaro P, van het Loo M, McDonnell J, Vader J, Kahan JP: The RAND/UCLA Appropriateness Method User's Manual, Santa Monica, CA, RAND Corporation, 2001
- 15.Esrailian E, Spiegel BM, Targownik LE, Dubinsky MC, Targan SR, Gralnek IM: Differences in the management of Crohn's disease among experts and community providers, based on a national survey of sample case vignettes. Aliment Pharmacol Ther 26: 1005–1018, 2007 [DOI] [PubMed] [Google Scholar]
- 16.Esrailian E, Gralnek IM, Jensen D, Laine L, Dulai GS, Eisen G, Spiegel BMR: Evaluating the process of care in non-variceal upper gastrointestinal hemorrhage: A survey of expert vs. non-expert gastroenterologists. Aliment Pharmacol Ther 28: 1199–1208, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Barker-Cummings C, McClellan W, Soucie JM, Krisher J: Ethnic differences in the use of peritoneal dialysis as initial treatment for end-stage renal disease. JAMA 274: 1858–1862, 1995 [PubMed] [Google Scholar]
- 18.Reddan D, Klassen P, Frankenfield DL, Szczech L, Schwabb S, Coladonato J, Rocco M, Lowrie EG, Owen WF: National profile of practice patterns for hemodialysis vascular access in the United States. J Am Soc Nephrol 13: 2117–2224, 2002 [DOI] [PubMed] [Google Scholar]
- 19.Frankenfield DL, Rocco MV, Frederick PR, Pugh J, McClellan WM, Owen WF Jr: Racial/ethnic analysis of selected intermediate outcomes for hemodialysis patients: Results from the 1997 ESRD Core Indicators Project. Am J Kidney Dis 34: 721–730, 1999 [DOI] [PubMed] [Google Scholar]
- 20.The Dartmouth Atlas of Healthcare. Available online at http://www.dartmouthatlas.org. Accessed March 2009.
- 21.Colliver JA, Swartz MH: Assessing clinical performance with standardized patients. JAMA 278: 790–791, 1997 [DOI] [PubMed] [Google Scholar]
- 22.Luck J, Peabody JW, Dresselhaus TR, Lee M, Glassman P: How well does chart abstraction measure quality? A prospective comparison of standardized patients with the medical record. Am J Med 108: 642–649, 2000 [DOI] [PubMed] [Google Scholar]
- 23.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M: Comparison of vignettes, standardized patients, and chart abstraction: A prospective validation study of 3 methods for measuring quality. JAMA 283: 1715–1722, 2000 [DOI] [PubMed] [Google Scholar]