Computed tomography (CT) is a powerful tool. It allows very quick creation of x-ray images of the body with high-resolution cross-sectional imaging. The quick, detailed result has made CT very valuable, especially in the emergency department (ED). In a very short time period, high-quality, cross-sectional images are available that help to define the medical status of the patient. This has increased our ability to provide the correct care in a timely manner.
Although CT scans are not the most frequently used diagnostic study in the hospital, they provide the majority of the radiation dose to the patient population (1)—and this dose level is steadily increasing. For example, a 2004 article in Radiology documented that CT scans constituted approximately 13% of the diagnostic imaging orders for hospitals in the United States but provided 70% of the dose (2). In addition, a 2006 National Cancer Institute report suggested that the number of CT scans ordered in adults and children has increased by about 7 times over the last 10 years (3). This trend of increased use has also been seen at Baylor University Medical Center (BUMC) when a second CT scanner was added to the ED during the recent remodel of the department.
A LACK OF KNOWLEDGE ABOUT RADIATION DOSE
A number of medical institutions have recently assessed their medical staff's knowledge of radiation dose and its associated risk. Many studies have demonstrated a lack of knowledge by staff about radiation dose for common radiological procedures. In a 2004 study at a 1285-bed hospital, only 27.5% of the physicians surveyed were able to score 45% or greater on 11 questions about radiation dose (4). In addition, 28% and 10% of the physicians surveyed, respectively, incorrectly believed that magnetic resonance angiography and ultrasound posed a risk from ionizing radiation. In a 2004 survey at a Yale University tertiary care center, most patients, ED physicians, and radiologists were unable to determine the correct radiation dose of a CT scan versus a chest radiograph (2). In addition, 78% of ED physicians at this facility admitted that they did not explain the risks and benefits of the CT scan to patients, and 93% of the surveyed patients claimed that they did not receive this information. A 2007 study involving three university hospitals, a research hospital, and three outpatient clinics found that 93% of staff surveyed underestimated the amount of radiation dose for diagnostic procedures (5). A 2005 article in the International Journal of Cardiology concluded that most physicians do not possess knowledge about the radiation dose for the diagnostic procedures they prescribe (6). These articles all recommended better education of physicians and staff about radiation exposure and its associated risks.
In November 2007, the New England Journal of Medicine published an article by Brenner and Hall entitled “Computed tomography—an increasing source of radiation exposure” (7). The authors acknowledged that most CT scans have a positive risk-to-benefit ratio but commented that “physicians often view CT studies in the same light as other radiological procedures, even though radiation doses are typically much higher with CT than with other radiological procedures.” They summarized a survey of pediatric physicians that found about one third of all CT studies could be replaced with other studies or not performed at all. Brenner and Hall suggested a threefold method for addressing these issues: 1) alter the CT scan protocols to minimize the dose for each study; 2) when possible, replace the CT scan with other diagnostic imaging tools that provide a lower ionizing radiation dose or none at all; and 3) decrease the number of CT studies prescribed. The article raised awareness about the recent increase in use of CT and its consequences and risks.
Not every conclusion made in the New England Journal of Medicine article is indisputable, and a variety of responses have poured in from many organizations, including the Food and Drug Administration (8), the American Association of Physicists in Medicine (9, 10), the American College of Radiology (11), the Society for Pediatric Radiology (12), the Health Physics Society (13), the Radiological Society of North America (14), and the American Council on Science and Health (15). However, the article also sparked several radiation reduction initiatives, including the Image Gently Campaign to reduce CT dose in pediatric patients (16) as proposed by the Alliance for Radiation Safety in Pediatric Imaging. BUMC has also started an initiative to reduce our patients' radiation exposure from CT scans.
BUMC'S CT DOSE REDUCTION INITIATIVE
The BUMC Radiology Imaging Department has invested in CT technology with equipment and software purchases and made efforts to reduce patient dose through protocol changes. To some extent, we have been successful in lowering the dose per study. However, for the CT dose reduction initiative to be successful, the medical staff who order the scans must also contribute to the effort.
BUMC's Patient Safety Committee, chaired by Dr. William Sutker, recommended the creation of a task group to examine the issue of CT radiation dose at BUMC. This group, led by Gail Maxwell, Baylor Health Care System's vice president of administration, consisted of ED physicians, trauma surgeons, radiologists, and other key personnel. The goal is to reduce the radiation dose to patients at BUMC by 1) minimizing the dose for each CT scan ordered and 2) providing information to the physicians who order imaging studies so that they can make educated decisions about the CT scans that they prescribe. Data on prescribing habits will be reviewed over a 6-month period to determine if the physician education efforts lead to a decrease in the number of CT scans ordered.
Three of the physician education components—the cancer risk from radiation, equating risk from different types of radiological studies, and considerations for choice of imaging study—are reviewed below.
RADIATION AND CANCER RISK
Cancer induction from radiation exposure occurs after a latent period of about 7 to 50 years after the initial exposure. Much of what is known about radiation risk and cancer comes from the US government's 50-year follow-up studies of survivors of the 1945 atomic bombs in Hiroshima and Nagasaki, Japan. From these data and smaller studies of other radiation exposures (such as cancer patients undergoing radiation therapy treatments and radiation workers), we have a better understanding of the risk of inducing cancer from radiation exposure.
The most recent comprehensive estimate of radiation risk appears in the Biologic Effects of Ionizing Radiation (BEIR) VII report (17), published by the National Academies' Committee to Assess the Health Risks from Exposure to Low Levels of Ionizing Radiation. This committee is chaired by Richard Monson of the Harvard School of Public Health and has members from many prominent universities worldwide and from the National Cancer Institute.
The BEIR VII report's lifetime risk model predicts that there is a 1% increase in risk of developing cancer (solid tumor or leukemia) after a radiation exposure of 10,000 mrem (which is equivalent to approximately 2500 anteroposterior chest radiographs or two to three CT abdomen scans for a larger patient). This statistical chance of developing a cancer is based on a linear model and thus can be scaled up or down depending on the radiation dose. For example, a dose of 5000 mrem would correspond to a 0.5% increase in cancer risk, and a 20,000 mrem dose, a 2% increase. BEIR VII also estimated that there is a 42% chance of getting cancer from reasons other than radiation; however, we can better control the radiation exposure risk.
EQUATING RISK FROM DIFFERENT TYPES OF RADIOLOGICAL STUDIES
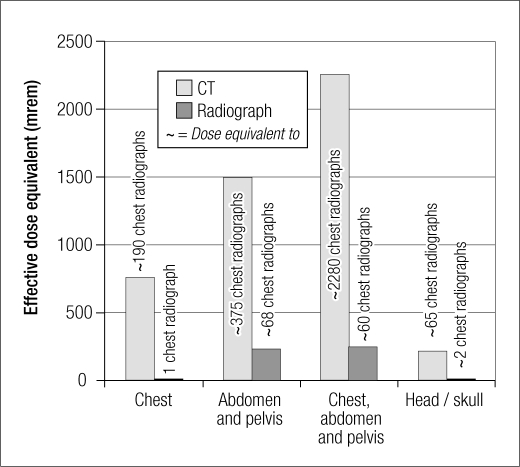
It becomes more difficult to equate radiation risk based on unit values of mrem (or mGy, mrad, or mSv), since these units are not commonly understood by most medical professionals or patients (4). To simplify the message, we created a table of common diagnostic procedures from CT, nuclear medicine, radiography, and fluoroscopy in units of mrem and estimated the number of corresponding anteroposterior chest radiographs (Table). Bar charts further compare the radiation dose of CT and radiographs (Figure). The mrem units were chosen because they represent the whole-body effective dose, which is a better estimate of radiation risk. (mSv is an equivalent unit in standard international units.)
Table.
Total-body effective dose and comparable number of chest x-rays for radiological studies in a patient with a normal body mass index∗
| Study | Estimated total body effective dose (mrem) | Comparable no. of posteroanterior chest x-rays (film or digital radiograph) |
|
Head/neck | ||
| Radiograph: skull | 10 | 3 |
| CT: head | 222 | 56 |
| NM: brain (20 mCi99m Tc-HMPAO) | 690 | 173 |
| PET: brain | 700 | 175 |
|
Spine | ||
| Radiograph: C-spine series | 27 | 7 |
| Radiograph: T-spine series | 140 | 35 |
| Radiograph: L-spine series | 180 | 45 |
| CT: C-spine | 450 | 113 |
| CT: T-spine | 1000 | 250 |
| CT: L-spine | 1000 | 250 |
|
Chest/lungs | ||
| Radiograph: posteroanterior chest | 4 | 1 |
| Radiograph: lateral chest | 8 | 2 |
| Radiograph: posteroanterior and lateral chest | 12 | 3 |
| NM: lung ventilation/perfusion (1 mCi 99mTc-DTPA aerosol + 5 mCi MAA) | 97 | 24 |
| CT: chest | 760 | 190 |
| CT: chest pulmonary embolism series | 1500 | 375 |
|
Heart | ||
| CT: coronary artery calcium scan | 300 | 75 |
| CT: coronary angiography with prospective gating | 300 | 75 |
| CT: calcium scoring | 500 | 125 |
| NM: MUGA | 520 | 130 |
| NM: cardiac stress (25 mCi 99mTc-tetrofosmin) | 325 | 81 |
| NM: cardiac rest and stress (8 mCi rest + 25 mCi stress 99mTc-tetrofosmin) | 429 | 107 |
| PET: cardiac | 1500 | 375 |
| Fluoroscopy: coronary angiogram | 1580 | 395 |
| CT: coronary angiography | 1600 | 400 |
| Fluoroscopy: percutaneous transluminal coronary angioplasty | 5000 | 1250 |
|
Abdomen/pelvis | ||
| Radiograph: pelvis | 110 | 28 |
| Radiograph: abdomen | 120 | 30 |
| Radiograph: intravenous pyelogram | 160 | 40 |
| NM: hepatobiliary (7 mCi 99mTc-mebrofenin) | 140 | 35 |
| NM: kidney (7.5 mCi 99mTc-MAG3) | 500 | 125 |
| CT: pelvis | 700 | 175 |
| CT: abdomen | 800 | 200 |
| CT: abdomen/pelvis without contrast (renal stone) | 1400 | 350 |
| CT: 3-phase liver | 1500 | 375 |
| CT: abdomen/pelvis | 1500 | 375 |
|
Bone | ||
| DEXA bone scan | 2.5 | 1 |
| NM: bone (20 mCi 99mTc-HDP) | 440 | 110 |
|
Breast | ||
| Radiograph: mammography (per view) | 10 | 3 |
|
Tumor | ||
| NM: PET (15 mCi of 18F-FDG) | 1100 | 275 |
| NM: tumor (10 mCi Ga67) | 2600 | 650 |
|
Combination studies | ||
| Fluoroscopy: barium swallow (24 images, 106 seconds) | 150 | 38 |
| Fluoroscopy: barium meal (11 images, 121 seconds) | 300 | 75 |
| Fluoroscopy: barium follow-up (4 images, 78 seconds) | 300 | 75 |
| Fluoroscopy: barium enema (10 images, 137 seconds) | 700 | 175 |
| NM: PET (15 mCi of 18F-FDG) | 1100 | 275 |
| PET/CT | 2000 | 500 |
| CT: chest/abdomen/pelvis | 2260 | 565 |
| CT angiography: chest and abdomen with contrast | 3120 | 780 |
|
Other | ||
| MRI: any type | 0 | 0 |
| Ultrasound: any type | 0 | 0 |
| Warning level (30% annual limit) for a radiation worker | 1500 | 375 |
| Annual limit for a radiation worker | 5000 | 1250 |
∗Radiographic or CT patient dose in some cases can increase significantly with patient size.
CT indicates computed tomography; NM, nuclear medicine; PET, positron emission tomography; MRI, magnetic resonance imaging; DEXA, dual-energy x-ray absorptiometry; HMPAO, hexamethyl propyleneamine oxime; DTPA, diethylene triamine pentaacetic acid; MAA, macroaggregated albumin; MUGA, multiple gated acquisition scan; HDP, hydroxymethyl diphosphonate; FDG, fluorodeoxyglucose; Ga67, gallium citrate 67.
Figure.
Comparison of radiation dose (mrem) for computed tomography (CT) and radiographic studies.
The doses listed in the Table are for patients with a normal body mass index (BMI) and may substantially increase (depending on the study) for a larger patient. For most studies, the CT scanner automatically adjusts the output of the x-ray tube to properly penetrate the patient's body for optimum image quality. In smaller patients, the dose is decreased with this method. However, for larger patients, the dose increase can be significant. For example, patient data acquired in the BUMC ED during a recent survey showed that the patient dose for a single abdomen pelvis CT without contrast (renal study) varied from 446 to 2567 mrem (equivalent to 112 to 642 anteroposterior chest radiographs), depending on patient size and composition. For a single abdomen pelvis CT with contrast, the dose varied from 433 to 3687 mrem (equivalent to 108 to 922 chest radiographs). A single chest CT with contrast for pulmonary embolism would provide a dose range of 109 to 1762 mrem (equivalent to 27 to 441 anteroposterior chest radiographs). A few of these studies in a larger patient could easily approach 10,000 mrem and the 1% chance of radiation-induced cancer in the future.
Many of these CT studies also affect individual organs that are more sensitive to radiation, such as bone marrow, eyes, thyroid, breast, and gonads. For example, a chest CT scan provides a localized dose to the breast of approximately 2100 mrad for a patient with normal BMI (compared with 9 mrad for an anteroposterior chest radiograph) (18). An abdomen and pelvis CT scan in a normal BMI patient will directly irradiate the gonads and uterus to approximately 2300 and 800 mrad, respectively (compared with 120 and 290 mrad for abdomen and pelvis radiographs). A CT scan to the head will irradiate the bone marrow, thyroid, and eyes to approximately 270, 190, and 2500 mrad, respectively (compared with a head radiograph, with bone marrow and thyroid doses of 20 and 40 mrad).
ADDITIONAL CONSIDERATIONS
Other imaging studies
Before ordering a CT scan, physicians may want to consider other imaging modalities. Some imaging studies have a lower radiation dose, such as a lower-radiation-dose radiograph or a zero-radiation-dose ultrasound. Magnetic resonance imaging does not expose the patient to ionizing radiation—but it is not readily available in the ED. The Statscan device in the ED can also be used as a low-dose, quick assessment whole-body imaging tool. The goal is to educate physicians about radiation dose so that they can consider it during the assessment of study risk versus benefit.
Review of recent images
Another consideration is the avoidance of unnecessary repeat tests. Baylor's Picture Archive and Communications System (PACS) provides a network of digital images and reports that are available 24 hours a day, 7 days a week at all Baylor hospitals. Dedicated workstations are located at various locations in each Baylor hospital, and the system can be accessed through the Internet from any Baylor workstation and, with proper log-ins and passwords, from any computer through the Baylor physician portal. Radiological tests done at other Baylor hospitals can also be accessed—at either dedicated workstations in the BUMC ED or through the Radiology Imaging Department's reading room. Currently, images from Baylor Medical Center at Waxahachie and Baylor Medical Center at Garland can be viewed in the BUMC ED on dedicated workstations, and images from Baylor Plano and Baylor Grapevine will be added soon. Any physician can ask for assistance in accessing these images in the radiology ED reading room, if they do not have access to the dedicated workstations in the ED. Over the next few years, PACS should be enterprise-wide, with information on patients from all Baylor Health Care System facilities.
The Radiology Imaging Department at BUMC is also working to facilitate use of image CDs or DVDs from other facilities. Because special software is often required to open the images, the CDs and DVDs may appear to be unreadable. A system is being developed in the ED where the original CD or DVD can be dropped off, uploaded to PACS, and available at a workstation. An order will also be generated for a radiologist to read the images and provide a written report.
It is helpful to check the PACS for the availability of images. For example, a patient might return to the ED several times with the same symptoms and therefore receive the same CT scan repeatedly. After the CT exam, the radiology staff is aware of the repeated scans because PACS automatically brings up the historical image for comparison. However, the referring physician, without looking first on PACS, might not realize the scan had already been done prior to ordering the study. In some cases, the repeat exam is entirely justified, but this should be at the discretion of the physician.
CONCLUSIONS
Only a physician is properly trained to evaluate the benefit versus risk of a particular radiological study. Radiation dose and associated risk should be considered in addition to medical necessity. In addition, it might be possible to replace a CT order with an imaging study that has a lower radiation dose or to eliminate the study altogether. The latter could be considered, for example, when recent archived images could be reviewed. At BUMC, our goal is to do our best to reduce our patients' radiation exposure.
References
- 1.Colang JE, Killion JB, Vano E. Patient dose from CT: a literature review. Radiol Technol. 2007;79(1):17–26. [PubMed] [Google Scholar]
- 2.Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231(2):393–398. doi: 10.1148/radiol.2312030767. [DOI] [PubMed] [Google Scholar]
- 3.National Cancer Institute. Radiation Risks and Pediatric Computed Tomography (CT): A Guide for Health Care Providers Rockville, MD: NCI Division of Cancer Epidemiology and Genetics, 2008. Available at http://www.cancer.gov/cancertopics/causes/radiation-risks-pediatric-CT; accessed December 16, 2008.
- 4.Jacob K, Vivian G, Steel JR. X-ray dose training: are we exposed to enough? Clin Radiol. 2004;59(10):928–934. doi: 10.1016/j.crad.2004.04.020. discussion 926–927. [DOI] [PubMed] [Google Scholar]
- 5.Correia MJ, Hellies A, Andreassi MG, Ghelarducci B, Picano E. Lack of radiological awareness among physicians working in a tertiary-care cardiological centre. Int J Cardiol. 2005;103(3):307–311. doi: 10.1016/j.ijcard.2004.08.070. [DOI] [PubMed] [Google Scholar]
- 6.Arslanoĝlu A, Bilgin S, Kubal Z, Ceyhan MN, Ilhan MN, Maral I. Doctors' and intern doctors' knowledge about patients' ionizing radiation exposure doses during common radiological examinations. Diagn Interv Radiol. 2007;13(2):53–55. [PubMed] [Google Scholar]
- 7.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 8.US Food and Drug Administration. What Are the Radiation Risks from CT? Rockville, MD: FDA, 2008. Available at http://www.fda.gov/cdrh/CT/risks.html; accessed December 16, 2008.
- 9.American Association of Physicists in Medicine. The AAPM Statement on Radiation Dose from Computed Tomography, in Response to the Brenner and Hall NEJM Article Published Nov 29, 2007 College Park, MD: AAPM, 2008. Available at http://www.aapm.org/publicgeneral/CTScans.asp; accessed December 16, 2008.
- 10.AAPM Task Group 23 of the Diagnostic Imaging Council CT Committee. The Measurement, Reporting, and Management of Radiation Dose in CT [AAPM Report 96]. College Park, MD: American Association of Physicists in Medicine, January 2008. Available at http://www.aapm.org/pubs/reports/RPT_96.pdf; accessed December 16, 2008.
- 11.American College of Radiology. ACR responds to NEJM article on radiation risk associated with CT scans [press release] Available at http://www.acr.org/MainMenuCategories/media_room/FeaturedCategories/PressReleases/Archive/ACRRespondstoNEJMArticleonRadiationRiskAssociatedWithCTScans.aspx; accessed December 16, 2008.
- 12.Society for Pediatric Radiology. SPR responds to study linking CT and cancer risk [press release] Available at http://www.pedrad.org/displaycommon.cfm?an=1&subarticlenbr=340; accessed December 16, 2008.
- 13.Health Physics Society. HPS responds to CT article Available at http://hps.org/documents/hps_ctrisk_response.pdf; accessed December 16, 2008.
- 14.Radiological Society of North America. Radiologists, medical physicists working toward patient safety in CT [press release, November 28, 2007] Available at http://www.rsna.org/media/pressreleases/pr_target.cfm?ID=348; accessed December 16, 2008.
- 15.Ross G [American Council on Science and Health]. Unnecessary x-rays should be avoided (but which are unnecessary?). TCSDaily, December 7, 2007. Available at http://www.acsh.org/healthissues/newsID.1643/healthissue_detail.asp; accessed December 16, 2008.
- 16.Alliance for Radiation Safety in Pediatric Imaging. Image Gently Campaign Available at http://www.pedrad.org/associations/5364/ig/; accessed December 16, 2008.
- 17.National Research Council of the National Academies . Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 18.Bushberg JR, Seibert JA, Leidholdt EM, Boone JM. The Essential Physics of Medical Imaging. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. [Google Scholar]