Abstract
Parents of premature infants often receive infant cardiopulmonary resuscitation (CPR) training prior to discharge from the hospital, but one study showed that 27.5% of parents could not demonstrate adequate CPR skills after completing an instructor-led class. We hypothesized that parents who viewed an instructional video on infant CPR before attending the class would perform better on a standardized skills test than parents who attended the class with no preparation. Parents randomized to the intervention (video) group viewed the video within 48 hours of the CPR class. Parents in the control group attended the class with no special preparation. All parents completed the CPR skills checklist test, usually within 7 days after class and before the infant's hospital discharge. The test rated subjects' skills in the areas of assessment, ventilation, and chest compressions; each section was rated as good, fair, or fail. In this pass/fail test, students had to be rated good or fair on all three sections to pass. All 10 subjects in the video group passed the test versus only 9 of 13 in the control group, but this difference was not significant (P = 0.08). However, 8 of 10 (80%) subjects in the video group were rated as good on all three sections, versus only 3 of 13 (18.7%) in the control group, and this was a significant difference (P = 0.012). We conclude that preparation of students using an instructional video prior to infant CPR class is associated with improvement in skills performance as measured by a standardized skills test. Video preparation is relatively inexpensive, eliminates the barrier of reading ability for preparation, and can be done at the convenience of the parent.
Infants requiring care in the neonatal intensive care unit (NICU) often have conditions that put them at increased risk of cardiorespiratory arrest after discharge. Many hospitals require that the parents of these infants learn how to perform infant cardiopulmonary resuscitation (CPR) before discharge home. A nurse or respiratory therapist usually teaches the parents with direct practice of skills using an infant CPR mannequin. Often this teaching is done at the same time that parents are busy learning other aspects of care at home, such as medication administration, home oxygen use, or operation of home apnea monitors. They may feel overwhelmed by the volume of information, in addition to the emotional aspect of caring for a child with special needs, and this may lead to less effective learning (1, 2).
A study by Dracup et al showed that 27.5% of parents were unable to demonstrate satisfactory infant CPR skills immediately after a conventional instructor-led class (3). A related study of a subgroup of these subjects showed that after 6 months, only 33% of those trained were still able to demonstrate adequate CPR skills (4), so retention of skills is poor. Interviews of 94 parents in this study revealed that seven of them (7.4%) were required to deliver infant CPR in an actual emergency after discharge. The peak incidence of sudden infant death syndrome occurs between 1 and 4 months of age (5), so long-term retention of infant CPR skills is critical. These findings suggest a significant need for improvement in the way infant CPR is taught.
Video self-instruction (VSI) has been used successfully to teach adult CPR to lay persons. Braslow used a 34-minute video-tape along with an inexpensive mannequin and found that VSI learners performed better than those given conventional CPR instruction (6). VSI has also been studied for parents learning infant CPR, but in that group it was not as successful. Dracup found that only 38% of parents could successfully demonstrate infant CPR skills after receiving VSI alone (3).
An instructional video for teaching adult and infant CPR is available from the American Heart Association. Designed for use by a facilitator, this video demonstrates all the necessary skills and is designed for a student to follow along using a mannequin in the style of an exercise video. It was not designed for a class offering CPR certification but is intended to make CPR instruction more widely available (7). Educational psychology recognizes that individuals have different learning styles. An instructional video could provide learners with a different representation to facilitate multiple exposures to the same material and thus promote better learning for some students (8, 9). The video can also serve as an “advanced organizer,” a way for the learner to have an introductory experience with the material before the in-hospital training (10).
This study assessed the efficacy of using this instructional video as a supplemental learning tool for parents before they attended a formal instructor-led infant CPR class.
MATERIALS AND METHODS
Recruitment of subjects
Parents and other significant caregivers were recruited at Baylor University Medical Center at Dallas' level III NICU, which has approximately 800 discharges per year. Infant CPR training is strongly encouraged for all parents, especially those caring for children on home oxygen or home apnea monitoring or children with tracheostomies or other special needs. Exclusion criteria were 1) attendance in a CPR class (adult or infant) within the last 2 years, and 2) inability to understand English, since the video was available only in English. There were no exclusion criteria concerning the medical diagnoses of the infant. Approval for the study was obtained from the institutional review boards for Baylor Health Care System and the University of Texas Health Science Center at Houston.
Informed consent was obtained from all subjects prior to enrollment in the study. Subjects were randomized by family unit into either the experimental group or the control group, so all subjects who would care for the same infant were in the same study group.
Instructional video
The Family & Friends CPR video was used with permission of the American Heart Association. The segment on infant CPR was dubbed from DVD to a VHS videocassette. VHS video allowed subjects to more easily rewind and play back segments they might want to see again. The final video was approximately 30 minutes long and included instruction on CPR and airway obstruction (choking).
CPR skills checklist
The skills checklist was originally developed by Mandel (11) and has been used in several studies of CPR performance (3, 4, 12). It has been shown to have very high interrater reliability and high agreement when compared with a printout from an instrumented CPR mannequin (13, 14). The checklist was adapted by Dracup et al for neonatal CPR skills (4), and Dracup's version was used in our study. The only modification we made was for assessment of the victim's perfusion instead of directly checking for a pulse, based on current American Heart Association guidelines (15). The checklist assesses 15 discrete skills that are grouped by 1) initial assessment, 2) chest compressions, and 3) ventilation. Each group of skills was rated as “good,” “fair,” or “needs improvement.”
A good performance using the skills checklist was one in which all steps were performed in the proper sequence and according to American Heart Association standards. However, a performance that did not meet these standards was still rated fair—i.e., adequate and safe—if the majority of compressions and ventilation met the standard but with the following errors:
Timing was off
Hand position, mouth, or nose seal slipped, but the subject corrected
The call for help was left out or improperly timed, but all other sequencing was correct
A needs improvement performance was one in which:
Sequencing was incorrect
Some maneuver was potentially injurious
- Inadequate compressions were delivered owing to
- —poor depth of compression
- —problems with hand placement
- —problems with the compression/relaxation component
- —poor timing of compressions
- Ineffective ventilation was delivered due to
- —uncorrected failure to open the airway
- —poor volumes
- —poor timing
To pass the skills test, a subject had to achieve a rating of either good or fair on each of the three groups of skills.
Experimental design
A post-test–only control group design was chosen for the study, since subjects were selected to have no previous recent CPR experience.
At the time of study enrollment, subjects were randomized by family into either an intervention (video) group or a control group. They also completed a brief demographic questionnaire. All subjects were then scheduled to take one of the regularly scheduled instructor-led CPR classes for parents with infants in the NICU. They were all provided with a brief written outline of the steps in infant CPR, which was the normal practice of the instructors. Anecdotal experience has shown that few students actually study these outlines. These subjects who underwent the current educational procedures served as the control group.
Subjects in the intervention (video) group were also scheduled to watch the instructional video within 48 hours of attending the class. The viewings were conducted in a small meeting room in the NICU using a 20-inch conventional television set connected to a VHS video player. Subjects were encouraged to watch the video as long as they wished and to rewind and review as needed. All the viewings were conducted inside the hospital to ensure a consistent viewer experience and to ensure that only subjects in the intervention group had access to the video.
All subjects then attended the conventional instructor-led class as scheduled. The classes were typically 60 minutes long and were limited to six students at a time, including students who were not participating in the study. Each student was seated in front of his own infant mannequin to practice the skills during the class. The instructor led the students through learning all the skills of infant CPR with the proper sequencing using the mannequins. Subjects from both study groups took the class together, but all were asked not to discuss their participation in the study with the instructor or any other stu-dents (i.e., the instructor was blinded to their study participation and group assignment).
Prior to discharge home (with a goal of 7 days or less after completing the class), subjects were asked to demonstrate their infant CPR skills with a mannequin to a trained nurse observer. The nurse observers performing the skills assessments were blinded to the study group assignment of the subjects. The nurse observer rated the student as good, fair (both of which were considered passing), or needs improvement (i.e., fail) using the skills checklist. Any student needing improvement received additional instruction immediately after this testing was completed.
Statistical analysis
The SPSS 15.0 statistical software package was used for all calculations (SPSS, Inc., Chicago, IL). Descriptive statistics were used to characterize the demographic data collected on the questionnaire from the two study groups. The independent t test was used to analyze data for continuous variables such as subject age. Nonparametric data such as sex and ethnicity were compared using chi-square analysis (Fisher's exact test). The primary outcome variable in this study was dichotomous: passing or failing the CPR skills checklist test. The secondary outcome variable was the frequency of an ideal performance, defined as passing the skills test with a rating of good on all three parts (assessment, chest compressions, and ventilation). Statistical significance was set at P < 0.05 for all analyses.
RESULTS
A total of 28 subjects enrolled in the study over a 6-month period, with 12 in the video group and 16 in the control group. Two subjects in the video group and three in the control group did not return to take the CPR skills test (5/28 = 18%). There were no explicit refusals or withdrawals from the study, but those subjects did not present themselves at the appointed time to take the test. Analysis of results was conducted based on the 23 subjects who actually took the CPR skills test.
As shown in Table 1, there were no significant demographic differences between the two experimental groups for age, sex, race, education, marital status, or previous completion of a CPR class (>2 years before study entry). No subject had ever performed CPR in an actual emergency. All 10 subjects in the video group were employed outside the home versus only 9 of 13 in the control group, but this difference was not statistically significant (P = 0.104).
Table 1.
Comparison of video and control groups
| Variable | Video group | Control group | P value |
| Age in years ± SD | 34.5 ± 4.8 | 33.2 ± 7.3 | 0.622∗ |
| Education years ± SD | 16.6 ± 2.7 | 15.6 ± 5.7 | 0.623∗ |
| Days from CPR class until skills test ± SD | 2.7 ± 3.2 | 4.2 ± 3.6 | 0.291∗ |
| Sex | 0.685† | ||
| Male | 5 | 5 | |
| Female | 5 | 8 | |
| Race | 0.221† | ||
| White | 5 | 10 | |
| African American | 3 | 1 | |
| Hispanic | 0 | 2 | |
| Asian | 2 | 0 | |
| Marital status | 0.229† | ||
| Married | 10 | 10 | |
| Single or divorced | 0 | 3‡ | |
| Employed outside home | 0.104† | ||
| Yes | 10 | 9 | |
| No | 0 | 4 | |
| Prior CPR class | 0.669† | ||
| Yes | 7 | 7 | |
| No | 3 | 6 |
∗By Student's t test, two-tailed.
†By Fisher's exact test, two-tailed.
‡Only one subject was divorced.
Testing results
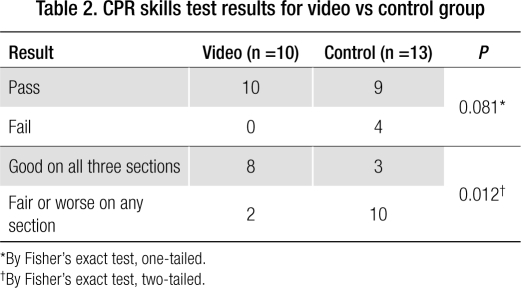
Experimental outcomes are shown in Table 2. Nine of the 13 subjects in the control group passed the CPR skills test. This represents a 69% pass rate, similar to the 72.5% pass rate observed by Dracup (3). All 10 subjects in the video group passed the test (100% pass rate). However, there was no significant difference between the groups (P = 0.081 by Fisher's exact test, one-tailed) despite the 100% pass rate in the video group. Subjects were also rated as good, fair, or needs improvement on all three sections of the test. Eight out of 10 subjects in the video group (80%) were rated good on all three sections of the test, versus only 3 of 13 (18.7%) in the control group, a significant difference (P = 0.012).
Table 2.
CPR skills test results for video vs control group
Using the same demographic factors as in Table 1, there were no significant differences between the subjects who passed the test and those who failed or between those who were rated good on all three test sections and those who were not.
Time interval before testing
The time interval between attending the instructor-led CPR class and taking the CPR skills checklist test ranged from <1 (same day) to 13 days. The goal was to test all subjects within 7 days after taking the CPR class, but some variation was expected due to the availability of study personnel when subjects were able to visit their infant in the hospital. Only two subjects in the video group and one in the control group were tested at >7 days. Subjects in the video group were tested at a mean of 2.7 ± 3.2 days after the class versus 4.2 ± 3.6 days for the control group, but this difference was not significant (P = 0.291). The four subjects who failed the CPR skills test were tested a mean of 6.0 ± 5.1 days after taking the class versus only 3.05 ± 2.9 days in those who passed, but again this difference was not significant (P = 0.120). There was also no significant difference in this time interval between the subjects rated good in all three categories on the skills test (3.3 ± 3.2 days) and those who were rated merely fair or needs improvement on any section (3.8 ± 3.8 days).
Interobserver differences
Four observers evaluated the study subjects. Observer 4 was able to perform only one test before the end of the study, and that subject passed. Otherwise, the other three observers performed approximately the same number of tests (9, 6, and 7). Of the four subjects who failed the CPR skills test, two were tested by Observer 1 and two by Observer 2. Observer 3 did not rate any subject as “failed” overall but did issue fair ratings as often as Observer 1.
Numeric score system
To gain further insight, the data from the three parts of each CPR skills test were analyzed using a numeric score system. For each part of the test (assessment, ventilation, and compressions), a numeric score of 2 was assigned for good, 1 for fair, and 0 for needs improvement. Thus, a subject rated good on all three parts of the test received a numeric score of 6, and a subject rated needs improvement on all three parts received a score of 0. This created a nonparametric data set since the only possible score values were whole numbers (0, 1, 2, 3, 4, 5, and 6). A histogram of the total scores clustered by study group demonstrates the skewness of the data toward a high score of 6 for the video group compared with the control group (Figure).
Figure.
Numeric scoring system: distribution of total scores by group. A perfect score was 6.
Table 3 shows the results of the Mann-Whitney U test applied separately to the assessment, compression, ventilation, and total test scores. P values were significant for the assessment, compression, and total scores, but there was no difference between video and control groups for the ventilation scores alone.
Table 3.
Mann-Whitney analysis of the numeric score data
| Test | Assessment score | Compressions score | Ventilation score | Total score |
| Mann-Whitney U | 30.0 | 35.5 | 45.0 | 25.5 |
| Wilcoxon W | 121.0 | 126.5 | 136.0 | 116.5 |
| Z | –2.497 | –2.178 | –1.471 | –2.606 |
| Asymptotic significance (two-tailed) | 0.013 | 0.029 | 0.141 | 0.009 |
| Exact significance [two∗(one-tailed significance)]∗ | 0.030 | 0.067 | 0.232 | 0.012 |
∗Not corrected for ties. Grouping variable: video vs control group.
DISCUSSION
Our results indicate that preparation of students using an instructional video prior to an infant CPR class is associated with a significant improvement in performance of CPR skills as measured by an objective skills test. The skills checklist was designed as a pass-fail test, and while more subjects in the video group “passed” the test, the difference compared with the control group was not significant. However, our analysis using all the data collected (good, fair, and needs improvement on each of the three parts) showed that significantly more subjects who viewed the video before class were rated good on all three parts of the test compared with the control group. Considering the differences between good and fair performance (described in the methods section), it is reasonable to hypothesize that students who were rated good on all three parts of the test may also have better retention of the skills during the months after discharge from the hospital, when such skills are most likely to be needed.
A pleasant surprise that complicated this study was the large number of potential subjects who had already received CPR training within the previous 2 years and thus could not be enrolled in the study. This made recruitment much slower than planned and ultimately led to a smaller number of subjects than desired. Also, it was planned to have a large number of subjects scored independently by two observers so that interrater reliability could be assessed. However, this was not possible due to logistics, since the nurses performing the skills tests did so while working in patient care in the NICU. Study enrollment was closed after 6 months to minimize possible subjective differences between subjects scored very early in the study and those scored near the end.
The variation in the time period between completing the CPR class and taking the CPR skills test was expected but unavoidable due to the resource limitations, as described. Some subjects lived 100 miles or more from the hospital, a regional referral center, so their visiting (and testing) opportunities were more limited. Testing all subjects at the same time interval after taking the class would have been ideal; however, no statistically significant effects of this variation could be demonstrated in the results.
It would have been desirable to perform follow-up CPR skills testing several months after the CPR class to measure retention of skills, especially during the first few months after hospital discharge when the risk of sudden infant death syndrome is highest. This was originally planned to be a part of the study but was found to not be feasible with the available resources.
A fair criticism of this study design is that it simply compares “more training” with “less training.” However, providing additional hands-on CPR training for new parents in the busy days before discharge home from the NICU is impractical and may simply take time away from other important preparations.
CPR is a psychomotor skill, so learning it requires more than just acquisition of knowledge. Practice with a mannequin is essential to ensure competence. Many students have difficulty with obtaining a proper seal over the nose and mouth of the infant for giving effective respirations. Students also have difficulty with giving adequate chest compressions, fearing they will harm the infant, so they must have direct practice with the mannequin to understand how deeply the chest must be compressed to produce an adequate blood pressure.
While it likely cannot totally replace an instructor-led class, effective video instruction could be a very useful adjunct for learning infant CPR. An instructional video could be viewed in the home at a time convenient for the parent and could be retained for future review. Preparation for the class by actually seeing someone perform all the skills on video might relieve some of the parents' anxiety about being in a classroom with several strangers and lead to more effective learning. Use of the video also avoids the barrier of reading ability, which could diminish the effectiveness of comparable written preparation guides. Video as an entertainment medium is pervasive in American culture, so compliance with class preparation using a video may be better compared with reading a written study guide.
Improved CPR training techniques for parents could make a tremendous difference in outcome for these infants. At the time of this writing, the Family & Friends CPR video cost about $30 and was available only in English. However, use of the video as a preparation tool might be even more beneficial for non-English speakers, since translators are currently needed to conduct those instructor-led classes, and this may impede learning. The investment required to implement this video learning intervention would be relatively small, so studies such as this are highly relevant.
Acknowledgments
We wish to express our appreciation to Craig Johnson, PhD (UT Health Science Center at Houston) and Richard Gilder, RN (Baylor Health Care System, Dallas, Texas) for their assistance with the statistical analyses.
References
- 1.Docherty SL, Miles MS, Holditch-Davis D. Worry about child health in mothers of hospitalized medically fragile infants. Adv Neonatal Care. 2002;2(2):84–92. doi: 10.1053/adnc.2002.32047. [DOI] [PubMed] [Google Scholar]
- 2.Drake E. Discharge teaching needs of parents in the NICU. Neonatal Netw. 1995;14(1):49–53. [PubMed] [Google Scholar]
- 3.Dracup K, Moser DK, Doering LV, Guzy PM. Comparison of cardio-pulmonary resuscitation training methods for parents of infants at high risk for cardiopulmonary arrest. Ann Emerg Med. 1998;32(2):170–177. doi: 10.1016/s0196-0644(98)70133-7. [DOI] [PubMed] [Google Scholar]
- 4.Dracup K, Doering LV, Moser DK, Evangelista L. Retention and use of cardiopulmonary resuscitation skills in parents of infants at risk for cardiopulmonary arrest. Pediatr Nurs. 1998;24(3):219–225. [PubMed] [Google Scholar]
- 5.Leach CE, Blair PS, Fleming PJ, Smith IJ, Platt MW, Berry PJ, Golding J. Epidemiology of SIDS and explained sudden infant deaths. CESDI SUDI Research Group. Pediatrics. 1999;104(4):e43. doi: 10.1542/peds.104.4.e43. [DOI] [PubMed] [Google Scholar]
- 6.Braslow A, Brennan RT, Newman MM, Bircher NG, Batcheller AM, Kaye W. CPR training without an instructor: development and evaluation of a video self-instructional system for effective performance of cardiopulmonary resuscitation. Resuscitation. 1997;34(3):207–220. doi: 10.1016/s0300-9572(97)01096-4. [DOI] [PubMed] [Google Scholar]
- 7.American Heart Association. HeartSaver and Family & Friends materials Available at http://www.americanheart.org/presenter.jhtml?identifier=3038993; accessed February 5, 2009.
- 8.Kozma RB. Learning with media. Review of Educational Research. 1991;61(2):179–211. [Google Scholar]
- 9.Allinson L, Hammond N. A learning support environment: the hitchhiker's guide. In: McAleese R, editor. Hypertext: Theory Into Practice. Oxford, England: Intellect Limited; 1989. pp. 53–63. [Google Scholar]
- 10.Hartley J, Davies IK. Preinstructional strategies: the role of pretests, behavioral objectives, overviews and advance organizers. Review of Educational Research. 1976;46(2):239–265. [Google Scholar]
- 11.Mandel LP, Cobb LA. Initial and long-term competency of citizens trained in CPR. Emerg Health Serv Q. 1982;1(3):49–63. doi: 10.1300/J260V01N03_08. [DOI] [PubMed] [Google Scholar]
- 12.Dracup K, Moser DK, Doering LV, Guzy PM, Juarbe T. A controlled trial of cardiopulmonary resuscitation training for ethnically diverse parents of infants at high risk for cardiopulmonary arrest. Crit Care Med. 2000;28(9):3289–3295. doi: 10.1097/00003246-200009000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Moser DK, Dracup K, Guzy PM, Taylor SE, Breu C. Cardiopulmonary resuscitation skills retention in family members of cardiac patients. Am J Emerg Med. 1990;8(6):498–503. doi: 10.1016/0735-6757(90)90150-x. [DOI] [PubMed] [Google Scholar]
- 14.Dracup K, Heaney DM, Taylor SE, Guzy PM, Breu C. Can family members of high-risk cardiac patients learn cardiopulmonary resuscitation? Arch Intern Med. 1989;149(1):61–64. [PubMed] [Google Scholar]
- 15.ECC Committee, Subcommittees and Task Forces of the American Heart Association 2005 American Heart Association guidelines for cardio-pulmonary resuscitation and emergency cardiovascular care. Circulation. 2005;112(24 Suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]