Abstract
Objectives
Assessments of population-level effects of antiretroviral therapy (ART) programs in Africa are rare. We use data from burial sites to estimate trends in adult AIDS mortality and the mitigating effects of ART in Addis Ababa. ART has been available since 2003, and for free since 2005.
Methods
To substitute for deficient vital registration, we use surveillance of burials at all cemeteries. We present trends in all-cause mortality, and estimate AIDS mortality (ages 20–64) from lay reports of causes of death. These lay reports are first used as a diagnostic test for the true cause of death. As reference standard we use the cause of death established via verbal autopsy interviews conducted in 2004. The Positive Predictive Value and Sensitivity are subsequently used as anchors to estimate the number of AIDS deaths for the period 2001–2007. Estimates are compared with Spectrum projections.
Results
Between 2001 and 2005, the number of AIDS deaths declined by 21.9% and 9.3% for men and women, respectively. Between 2005 and 2007, the number of AIDS deaths declined by 38.2% for men and 42.9% for women. Compared to the expected number in the absence of ART, the reduction in AIDS deaths in 2007 is estimated between 56.8% and 63.3%, depending on the coverage of the burial surveillance.
Conclusion
Five years into the ART program, adult AIDS mortality has been reduced by more than half. Following the free provision of ART in 2005, the decline accelerated and became more gender balanced. Substantial AIDS mortality, however, persists.
Keywords: HIV/AIDS, antiretroviral therapy, mortality, population surveillance, vital statistics, verbal autopsy, Ethiopia, Africa
Introduction
Reports about the efficacy of antiretroviral therapy (ART) rollout in sub-Saharan Africa are encouraging. Although concerns persist about access to treatment [1], and reports on adherence are mixed [2–4], the virological and immunological responses to treatment are good, and most cohort studies report substantial mortality reductions following the initiation of ART [4–8]. Most ART efficacy studies, however, are based on patient cohorts from health facilities, and do not account for those who never reach the ART clinic. Issues related to the coverage of treatment programs and equitable access to treatment are thus beyond reach of current studies. As a result, most of our insights about the population-level effects of ART are based on epidemiological models, and our experience with HIV prevalence estimates has demonstrated that model-based and observational estimates can be quite different [5].
Population-based and cause-specific mortality estimates thus provide necessary empirical validity checks for the epidemiological modeling of the effects of ART, but require vital registration-type data. Vital registration systems are notoriously difficult to set up and maintain in resource-constrained countries, not coincidentally also those that are hardest hit by the HIV/AIDS epidemic [6–8]. In this article, we use an ongoing registration of burials as an alternative to a conventional vital registration for estimating trends in all-cause mortality and adult AIDS mortality in the period 2001–2007.
Addis Ababa had an estimated population of just over two million in the last (1994) census [9]. The first AIDS cases were documented in 1986 [10]. By 2005, HIV prevalence in the age group 15–49 had grown to 7.1% according to the Ministry of Health [11], an estimate that lies between those of the 2005 Demographic and Health Survey (5.0%) (DHS) [12], and earlier extrapolations from antenatal clinic data (11.7%) [13]. The impact of HIV on mortality is substantial: estimates for 2001 attribute between 54.7% and 62.4% of adult deaths (ages 20–64, both sexes) to AIDS [14].
Since 1999, a limited number of AIDS patients have been receiving ART through the informal market [15]. In July 2003, the government launched a program to provide antiretrovirals through a co-pay scheme whereby the cost to the end user ranged from US$28 to US$80 per month depending on the combination of drugs—a substantial amount for a population in which more than three-quarters survive on less than $2 a day [16]. Since February 2005, ART has been available free of charge, but, but patients had to obtain a poverty certificate from the local administration in order to qualify. In October 2005, the government started providing free ART in public hospitals regardless of socioeconomic status [17]. Statistics reported in Table 1 suggest that close to 14,000 patients had ever started ART before the end of January 2006. In the following two years, the number of patients who initiated ART at any of Addis Ababa’s health facilities more than tripled. A similar trend is visible in the number of patients on treatment at the time of reporting.
Table 1.
HIV care and ART enrollment statistics, Addis Ababa (2003–2008)
| Ever enrolled in an HIV care program a | Ever started ART a | On ART at time of reporting a | Number of facilities reporting | |
|---|---|---|---|---|
| July 2004 b | - | 5,593 | - | 12 |
| July 2005 b | - | 7,742 | - | 13 |
| January 2006 c | 21,459 | 13,739 | 10,888 | 22 |
| January 2007 c | 43,857 | 26,623 | 20,863 | 46 |
| January 2008 c | 68,550 | 42,324 | 29,764 | 51 |
Notes:
Statistics are for all ages combined. At the national level, around 95% of patients who ever started, or, are on ART at the time of reporting are 15 years or older. In January 2008, less than 2% of adults patients were on 2nd line drug regimen.
Source: Addis Ababa City Administration Health Bureau (unpublished figures).
Source: Ministry of Health; Monthly HIV care and ART update [18]. Includes the Armed Forces, Bella Defense and Police hospitals, and the Federal Prison health center. Data represent the status at the end of the month.
Methods
We use data from surveillance of burials and from verbal autopsy interviews. The burial surveillance was initiated at all cemeteries of Addis Ababa in February 2001 and registers around 20,000 deaths a year [14, 19–21]. At the end of 2007, the surveillance covered 62 Orthodox Christian, 7 Muslim, 2 Catholic, 1 Jewish, and 9 municipal cemeteries. The largest of the municipal cemeteries, Baytewar,* buries persons without close relatives or friends to facilitate a funeral. Baytewar alone accommodates approximately 15% of burials, and most of its records lack socio-demographic background information. Over 40% of persons buried at Baytewar are infants.
The surveillance is conducted by cemetery clerks who are regularly briefed in training workshops. The clerks collect information on the date of burial, age, name, sex, address, marital status, region of birth, ethnicity, religion, and a lay report of the cause of death from relatives or close friends while they make arrangements for burial. Just 5.3% of the records have missing values for age and 5.5% have missing values for sex. Excluding cases from the Baytewar cemetery, fewer than 1% have missing values for either age or sex. Missing values for age and sex are imputed using a hot-deck procedure [22].
Infants who die before the naming ceremony (40 days for boys and 80 days for girls) are often not given a formal funeral. The burial surveillance is thus prone to underreporting of infant mortality. After correcting the underreporting of early childhood deaths, the crude death rate (CDR) for 2001 was estimated at just over 9 per 1,000 [14]. Other potential sources for underreporting are the burial of residents beyond the city administration limits, the return of terminally sick migrants to their families for care [23, 24], the repatriation of bodies for burial, failure of cemetery clerks to register burials, and possibly also illegal burials.
The verbal autopsies (VAs), our second data source, are post-mortem interviews with close relatives or caretakers of the deceased about the signs and symptoms experienced during terminal illness [25]. The VAs were administered for adult deaths (twelve years and above) randomly selected from burials registered in November and December of 2003. Most records from the Baytewar cemetery were de facto excluded for a VA interview because selection required complete information for the name, age, sex, and address of the decedent.
VAs were conducted by a pair of trained community health workers who visited the household two to four weeks after the death. Of the cases selected for interview, 78.6% of the interviews were completed, 4.5% of the caretakers refused an interview, 13.8% of the households could not be found, and 2.9% of the interviews were not completed for other reasons. Eleven questionnaires were discarded because interviewers doubted the truthfulness of the respondent’s answers.
Causes of death were ascertained via physician review. Two physicians independently assigned an underlying cause of death. If the assigned ICD10 code (three digits) for the first two physicians did not match, the VA questionnaire was reviewed by a third physician. In eleven cases the cause of death could not be established. The data used in this paper are the remaining 413 cases (ages 20–64) with a physician-assigned cause of death. These were classified as AIDS and non-AIDS deaths. We group TB and AIDS together because they are highly correlated and both laymen and physicians tend to have difficulties distinguishing both causes of death. For validating our estimation method, we also report on the results of 141 and 625 VAs that were conducted in 2001 and 2007, respectively. Only minor changes were implemented in the questionnaires and fieldwork procedures in the different VA survey rounds.
To demonstrate mortality trends, we (1) compare observed age and sex-specific deaths with those implied in population projections excluding an AIDS effect, and (2) develop a method to estimate the number of AIDS deaths from lay reports of causes of death.
Observed versus projected deaths
To estimate the annual number of deaths that would occur in the absence of HIV/AIDS, we use the Spectrum package (v.3.14) [26] to emulate population projections from the Central Statistical Authority (CSA) [9]. These use 1994 census population as the baseline and assume a steady increase in life expectancy (e0) from e0m: 56.2 and e0f: 58.8 to e0m: 62.0 and e0f: 66.0 between 1995 and 2007. We assume a decline in the Total Fertility Rate from 2.14 in 1995 to 1.94 in 2000 and 1.80 in 2007. These values reflect that fertility in Addis Ababa is below replacement [27, 28]. For migration, we follow CSA’s high variant assumption of a constant number of in-migrants at the 1994 level. With the exception of the implied effect of AIDS on the population age structure in the 1994 census, these projections thus ignore the demographic impact of AIDS. We compare the projected deaths (by age and sex) with observed numbers from the burial surveillance.
Extrapolations from lay reports of causes of death
The second, less common, method for estimating mortality trends is based on lay reports of causes of death. Table 2 shows the distribution of lay reports for 2002 (first full year of observation) and 2007. Although few deaths are explicitly ascribed to HIV/AIDS, some of the lay diagnoses are very suggestive of AIDS. This is also demonstrated in Table 3, which maps lay reports against the cause of death attributed by physicians in the sample with a reviewed verbal autopsy. Deaths explicitly labeled as TB or AIDS deaths have a positive predictive value (PPV) of 89%, but account for only 7% of AIDS deaths. Herpes zoster, diarrhea, uterine cancer, mental problem, and emaciation account for another 8% of AIDS deaths, and their PPV is 71%. Lung disease and cough are other good predictors of AIDS mortality, and about 40% of all adult cases are labeled as such. Cold accounts for just under 25% of all AIDS deaths. Together these lay reports accurately predict an AIDS death 80% of the time and have a sensitivity (SE) of 78%. Their cumulative specificity (SP) is 77%. Henceforth, this group of lay reports is labeled “AIDS-indicative lay reports” (LRA). Other lay reports of causes of death are less predictive of AIDS ascriptions by physicians (PPV: 25%, SE: 22%, SP: 23%).
Table 2.
Distribution of lay reports of causes of death by sex (Addis Ababa, age 20–64, 2002 and 2007)
| 2002 |
2007 |
|||||
|---|---|---|---|---|---|---|
| Men % a | Women % a | Total | Men % a | Women % a | Total N | |
| 1. Communicable diseases | 57.0 | 62.4 | 6,393 | 44.5 | 49.9 | 3,930 |
|
| ||||||
| Tuberculosis/Lung disease | 28.1 | 28.5 | 3,034 | 18.0 | 18.6 | 1,528 |
| Cold | 19.1 | 23.3 | 2,261 | 13.7 | 16.2 | 1,244 |
| Acute febrile illness | 4.2 | 3.6 | 420 | 2.8 | 2.1 | 204 |
| AIDS | 1.3 | 1.6 | 151 | 2.8 | 4.8 | 312 |
| Diarrheal diseases | 1.5 | 1.9 | 185 | 1.5 | 1.7 | 134 |
| Herpes zoster/Oral candidiasis | 0.7 | 1.5 | 114 | 0.2 | 0.6 | 33 |
| Other | 2.1 | 2.1 | 228 | 5.4 | 6.0 | 475 |
| 2. Maternal causes | - | 2.4 | 120 | - | 2.9 | 116 |
|
| ||||||
| 3. Non-communicable diseases | 26.3 | 28.4 | 2,926 | 36.0 | 40.9 | 3,197 |
|
| ||||||
| Cardiovascular disorders | 5.7 | 7.3 | 693 | 10.1 | 11.2 | 887 |
| Liver cirrhosis b | 6.7 | 4.5 | 609 | 8.2 | 6.0 | 593 |
| Neoplasms | 2.3 | 4.0 | 331 | 3.5 | 8.2 | 481 |
| Renal disorders | 3.1 | 3.2 | 334 | 3.2 | 4.5 | 317 |
| Diabetes | 2.1 | 1.8 | 209 | 3.2 | 2.9 | 253 |
| Other | 6.4 | 7.6 | 750 | 7.8 | 8.2 | 666 |
| 4. Symptoms, signs and syndromes | 5.4 | 5.4 | 579 | 5.3 | 5.2 | 438 |
|
| ||||||
| Mental problem | 2.8 | 1.9 | 257 | 3.0 | 2.6 | 231 |
| Emaciation/Cough | 0.1 | 0.2 | 16 | 0.1 | 0.2 | 12 |
| Other | 2.4 | 3.3 | 306 | 2.2 | 2.5 | 195 |
| 5. External causes | 11.3 | 3.8 | 636 | 14.3 | 4.0 | 617 |
|
| ||||||
| Subtotal of 1. to 5. (N) | 5,637 | 5,091 | 10,728 | 4,327 | 4,015 | 8,342 |
| Subtotal of 1. to 5. (%) | 76.4 | 82.5 | 88.1 | 92.6 | ||
| 6. Unknown - weakly specified c | 23.6 | 15.6 | 2,701 | 11.9 | 4.7 | 792 |
|
| ||||||
| No CoD assigned/missing | 11.3 | 5.5 | 339 | 8.2 | 2.7 | 119 |
| Medically not recognized community beliefs | 1.2 | 1.3 | 79 | 0.6 | 1.0 | 44 |
| Other | 11.1 | 8.8 | 545 | 3.1 | 1.0 | 43 |
|
| ||||||
| Total of 1. to 6. | 7,375 | 6,174 | 13,355 | 4,913 | 4,337 | 9,090 |
Notes:
Percentages are calculated with the subtotal as the denominator for categories 1–5, and the total as the denominator for category 6.
Sometimes arbitrary decisions were made to classify lay reports as communicable or non-communicable diseases. For example, all liver problems not explicitly referred to as hepatitis (in the community known as ye wof beshita and here classified under “other communicable diseases”) were interpreted as liver cirrhosis. The lay report in Amharic in these cases usually mentioned gubet beshita, which literally means liver disease.
Most unknown or weakly specified lay reports are cases where the cause of death is missing. These often pertain to burials at the Baytewar cemetery. At the outset of the burial surveillance many deaths were also attributed to sickness or accidental sickness (here included in the category “other”). During briefings, cemetery clerks were encouraged to probe for more specific lay reports, and that is probably why these weakly specific lay reports have declined over time.
Table 3.
Diagnostic values of lay reports of causes of death for identifying AIDS mortality (Addis Ababa, both sexes, age 20–64, 2003–4)
| Lay report | ||||||
|---|---|---|---|---|---|---|
| Reference Standard (physician review of VA) a | TB/AIDS | Herpez zoster/Diarrhea/Uterine cancer/Mental problem/Emaciation | Lung disease/Cough | Cold | Other | Total |
| AIDS | 16 | 17 | 88 | 52 | 48 | 221 |
| NoAIDS | 2 | 7 | 14 | 20 | 143 | 186 |
| Undetermined | 0 | 0 | 0 | 1 | 5 | 6 |
|
Diagnostic indicators, in % (95%-CI) | ||||||
| PPV | 89 (65–99) | 71 (49–87) | 86 (78–92) | 72 (60–82) | 25 (19–32) | |
| Sensitivity | 7 (4–11) | 8 (5–12) | 40 (33–47) | 24 (18–30) | 22 (16–28) | |
| Specificity | 99 (96–100) | 96 (92–98) | 92 (88–96) | 89 (84–93) | 23 (17–30) | |
|
Cumulative values for the diagnostic indicators, in % (95%-CI) | ||||||
| PPV | 89 (65–99) | 79 (63–90) | 84 (77–90) | 80 (74–85) | ||
| Sensitivity | 7 (4–11) | 15 (11–20) | 55 (48–61) | 78 (72–84) | ||
| Specificity | 99 (96–100) | 95 (91–98) | 88 (82–92) | 77 (70–83) | ||
Notes:
In the reference standard we combined TB and AIDS cases. Of the cases here classified as AIDS, the reviewing physicians diagnosed roughly 5% as pulmonary TB as the only underlying cause of death. In another 5%, TB was identified as the primary underlying cause of death in combination with another condition, but not AIDS. In 90%, HIV/AIDS was mentioned as the primary underlying cause of death.
To estimate trends in AIDS mortality, we use the PPV and SE of the AIDS-indicative lay reports as anchors. This method was first explored in Araya et al. [20], and is extended to allow for age (x) and sex-specific variation in the diagnostic validity of the lay reports. In the subsample with a verbal autopsy diagnosis of the cause of death, the PPV and SE of lay reports are estimated by probit regression models (only age has a significant–negative–effect on the PPV). We then estimate the year and sex-specific number of AIDS deaths (DA) in the age range 20–64 as:
DA is first estimated for deaths that come with a sufficiently specific lay report (categories 1–5 in Table 2). The distribution of causes of death in deaths with an unknown or weakly specified lay report (category 6 in Table 2) is assumed to be the same as for other deaths and is added to the total of DA. Confidence intervals around DA are estimated by bootstrapping. These account for the uncertainty in the estimates of the PPV and SE as well as the stochastic variation in the imputation of missing values for age and sex.
This approach presumes that the diagnostic validity of lay reports remains stable over time, and that is not necessarily realistic. However, comparison of AIDS mortality fractions estimated by the method described above and those obtained from VAs conducted in 2001 and 2007 is encouraging: extrapolations from the lay reports establish the AIDS mortality fraction in the age range 20–64 in 2001 at 59.4% and 67.0%, and for 2007 at 45.4% and 48.8% for men and women, respectively. The VA estimates for 2001 are 58.4% (N=77) and 67.2% (N=64), and for 2007 they are 44.9% (N=314) and 51.1% (N=311) for men and women, respectively.
To determine the number of averted AIDS deaths, we compare the estimated number of AIDS deaths with the implied number of AIDS deaths in population projections that incorporate the effect of HIV/AIDS, but do not account for the impact of ART. These projections use the baseline population and projection parameters described earlier, and make additional assumptions about the course of the HIV/AIDS epidemic. As before, the projections are done with Spectrum [26]. Estimates of HIV prevalence were generated using the UNAIDS Estimation and Projection Package (EPP 2007) [29] with inputs from ANC data [13] and population-based seroprevalence surveys done in 1994 [30] and 2005 [12]. With these inputs, HIV prevalence is estimated to have reached 1.0% in the mid 1980s, peaked at 7.9% in 1997, and declined to 7.4% by 2007. The ratio of female to male infections is assumed to have increased from 1.00 to 1.35 between 1994 [30] and 2007.
Results
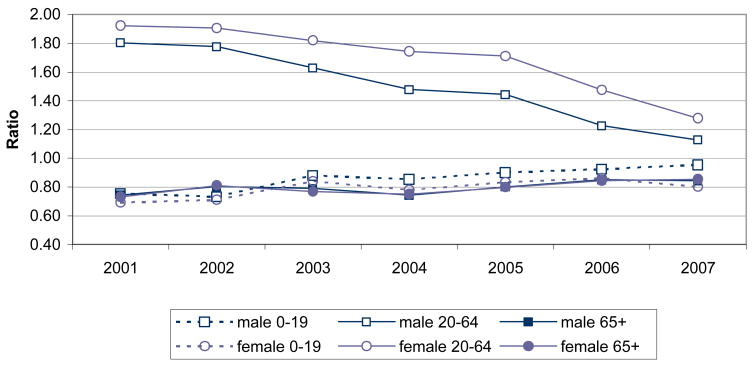
Figure 1 summarizes trends in the ratio of observed over projected deaths (all causes and assuming no AIDS effect) by sex and broad age groups. The ratio of deaths in adulthood (ages 20–64) is above unity for the whole period. This is a likely reflection of the HIV/AIDS epidemic, because it is the age range that is most typically affected by AIDS mortality. The higher ratio for women compared to men may reflect the sex ratio of HIV incidence in the early 1990s, it may be the result of underestimating female in-migration in the population projections, or, it may be due to greater underreporting of male mortality. Underreporting of male mortality could result from the return of terminally sick migrants to their families for care (i.e., a salmon effect) [31] as well as the return of bodies for burial in their region of origin. That explanation accommodates sex differences because male migrants in patrilineal societies tend to maintain greater ties with their relatives at origin. Based on the available evidence, it is difficult to establish whether this gender difference is genuine, or, due to biases in our data.
Figure 1. Ratio of observed to projected (excl. AIDS mortality) deaths by sex and age (Addis Ababa, 2001–2007).
Notes: The projected number of deaths comes from population projections with the 1994 census population as a baseline. The projections assume no HIV/AIDS effect. Other projection assumptions are described in the text. Observed number of deaths comes from the burial surveillance. The difference between men and women in the ratio of observed over expected number of deaths in adulthood is not due to the stochastic variation in the annual number of observed deaths in the burial surveillance (tested via a poisson model). This does not exclude, however, that the difference may be caused by systematic underreporting of male deaths in the burial surveillance or erroneous projection assumptions.
The ratio of observed over projected child deaths is below unity for the whole period and confirms the underreporting of early childhood mortality in the burial surveillance. The ratio of deaths in old age hovers around 0.8. Even though this is also suggestive of underreporting, the projected number of deaths above age 65 is probably an overestimate: because the projections do not incorporate the impact of HIV/AIDS, many of those who under actual conditions would have died in early adulthood survive in the projections until old age and thus depress the ratio above age 65. It is therefore likely that the coverage of the burial surveillance for adult deaths exceeds 80%.
Trends in mortality are more informative than estimates of mortality levels per se because trends are not affected by underreporting as long as the underreporting remains stable. With that in mind, it is of interest that the ratio of observed over projected deaths in adulthood peaked in 2001–2002. Between 2001 and 2005 the ratio dropped from 1.92 to 1.71 (or by 11.1%) for women, and from 1.80 to 1.44 (or by 20.0%) for men. Following the introduction of free ART in 2005, the decline accelerated: the ratio dropped from 1.71 to 1.28 (a 25.2% decline) for women, and from 1.44 to 1.13 (a 21.8% decline) for men in just two years.
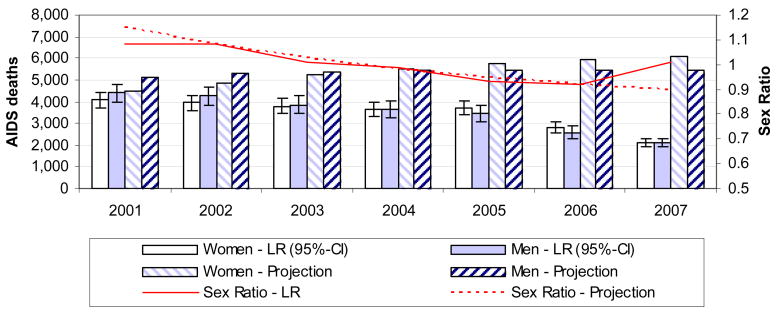
To seek confirmation that these trends in all-cause adult mortality are driven by a reduction in AIDS mortality, we turn to lay reports of causes of death. Table 2 demonstrates that the frequency of most AIDS-indicative lay reports declined over time (deaths explicitly attributed to AIDS being the exception). Estimates of the number of AIDS deaths based on extrapolations from the AIDS-indicative lay reports indicate a decline in the number of AIDS deaths from 8,467 in 2001 to 4,230 in 2007, a 50.0% reduction (Figure 2). The decline accelerated in the last two years: between 2001 and 2005, the number of AIDS deaths declined by 21.9% and 9.3% for men and women respectively; between 2005 and 2007, the number declined by 38.2% and 42.9% respectively.
Figure 2. Estimated number and sex ratio of AIDS deaths based on extrapolations from lay reports of causes of death (LR), compared to projections including an AIDS effect (without ART) (Addis Ababa, age 20–64, 2001 – 2007).
Notes: The projected number of deaths comes from population projections based on the 1994 census population. The projections incorporate an HIV/AIDS effect on mortality and assume no availability of ART. Other projection assumptions are described in the text. The estimated number of AIDS deaths in the presence of ART is based on the methodology for extrapolating from lay reports of causes of death reported in the burial surveillance. The whiskers on these estimates represent 95%-confidence intervals.
Because HIV prevalence peaked in the late 1990s, the observed decline in the number of AIDS deaths occurred in a period when AIDS mortality was expected to increase. Compared to the anticipated number of AIDS deaths in the absence of ART, the number of observed AIDS deaths in 2007 is reduced by 63.3%. Assuming that the coverage of the burial surveillance is only 85%, the averted AIDS deaths in 2007 alone is estimated at 6,540, or, a reduction by 56.8%. The cumulative number of averted adult AIDS deaths between 2003 and 2007 exceeds 18,400, which is more than the total number of deaths (all ages) that were registered in 2007.
Discussion
Few populations in sub-Saharan Africa are covered by a sufficiently well functioning vital registration system for providing accurate cause-specific adult mortality estimates. As a result, little is known about the effect of HIV/AIDS at the population level, or, about efforts to mitigate its mortality impact. Using surveillance of burials, we document severe AIDS mortality in Addis Ababa, but also a reversal in the mortality trend following the introduction of ART. This reversal is indicated by a declining ratio of observed over projected deaths (for all-cause mortality), and by estimates of the trend in AIDS-specific mortality. The decline in the number of adult AIDS deaths since the introduction of ART is estimated at 50.0%. This reduction, albeit impressive, is not as steep as, for example, in New York, where the number of AIDS deaths (all ages) declined by 63% in just two years following the availability of effective antiretroviral therapy in the late 1990s [32]. Addis Ababa’s record comes closer to that of Sao Paulo where AIDS death rates dropped by 65% between 1995 and 2002 [33]. The reasons for the slower decline in mortality compared the US could be that (1) the New York epidemic peaked earlier compared to the timing of ART rollout, (2) the number of AIDS cases were lower in New York and therefore easier to absorb by the medical infrastructure, (3) the demand for treatment might have been higher in New York, or, that (4) mortality among those receiving treatment has been higher in Ethiopia than in the US.
The reduction in AIDS mortality in Addis Ababa, however, happened in a period when AIDS mortality was expected to increase in the absence of ART. Accounting for that, and adjusting for the fact that the coverage of the burial surveillance might not be complete, close to 60% of the expected number of adult AIDS deaths in Addis Ababa in 2007 were averted because of the availability of ART. This statistic gives us an indication of the effective coverage of ART: if AIDS patients are timely enrolled in ART programs and are fully compliant, then ART will avert almost all AIDS deaths in the early phases of an ART program. ART will inevitably become more complicated and less effective after several years, but that does not yet apply to Ethiopia: by the end of January 2008, less than 2% of adult patients on treatment were on 2nd line regimen [18]. In other words, effective coverage approximates the percentage of averted deaths. The actual coverage will be higher because of program mortality due to late initiation of ART and non-compliance.
Our results suggest that the free provision of ART accelerated the reduction of AIDS mortality. Under the ART program with patient co-pay, AIDS mortality dropped by 15.8% between 2001 and 2005. Since the availability of free ART, AIDS mortality declined by 40.6% between 2005 and 2007. While this suggests that treatment costs are an important element in the accelerated decline of AIDS deaths [34], other factors, such as an increase in the number of accredited VCT and treatment centers and increasing advocacy around ART, may have contributed to that trend.
Under the co-pay scheme the decline appeared more pronounced for men (a 21.9% decline between 2001 and 2005) than for women (a 9.3% decline). Possible reasons for that are a changing sex ratio of infections in the late 1990s, but also gender differences in the access to resources for financing treatment. Following the launch of the free ART program, the declines in AIDS mortality have been similar for both sexes.
While these are generally encouraging results, substantial AIDS mortality remains. An important question, therefore, is whether the decline in AIDS mortality can be sustained, and whether that can be accomplished via supply-side improvements in the provision of ART alone. More proactive HIV diagnosis strategies might be necessary to improve both coverage of ART programs and the timeliness of enrollment. Many deaths currently occur just before or shortly after the initiation of ART, and this indicates that patients do not present for treatment until their prognosis is grim [35, 36]. Further study of the background characteristics of residual AIDS deaths and their treatment history may suggest how to best target groups who do not benefit from the current availability of ART [37]. Population-based data are an important source of evidence for that, but they are not commonly available in populations that are severely affected by HIV/AIDS (South Africa and a few populations covered by a demographic surveillance being the exception) [38, 39]. In this article we rely on data from an ongoing surveillance of burials to substitute for deficient vital registration. Burial surveillance is logistically simple because it taps into an existing infrastructure of cemeteries Another advantage of our approach is that it does not require continuous VA collection for estimating cause-specific mortality: once anchored, lay reports can be used to estimate cause-specific mortality fractions for periods when no VA data are available. Periodic re-anchoring of lay reports may be necessary.
Acknowledgments
The Addis Ababa Mortality Surveillance Project has been made possible with financial support from the AIDS Foundation of Amsterdam (grant nr. 7022), the World Health Organization (WHO/Second Generation Surveillance on HIV/AIDS, Contract No. SANTE/2004/089-735), the Centers for Disease Control and Prevention (EPHA-CDC Cooperative Agreement No. U22/CCU022179), a Mellon Foundation pilot project grant to the Population Studies Center of the University of Pennsylvania, a Hewlett Foundation grant to the University of Colorado at Boulder for the African Population Studies Research and Training Program. The project receives institutional support from the Faculty of Medicine of Addis Ababa University and the Ethiopian Public Health Association. Religious leaders and the Addis Ababa Labour and Social Affairs Bureau facilitated our access to the burial sites. We thank Drs. Getachew Tizazu, Sisay Yifru, Ashenafi Bekele, Desalegn Negatu, Mikyas Demisse, Yayeh Negash, Mihila Zebenegus, and Dagne Muluneh for the review of verbal autopsy interviews, and Doug Ewbank, Jane Menken, Eric Udjo, the late Etienne van de Walle, Susan Watkins, and the journal’s reviewers for comments on earlier drafts. Nancy Dawson Mann edited the manuscript and was supported by the NICHD-funded University of Colorado Population Center (R21 HD51146). The content of this publication is the sole responsibility of the authors and does not represent the views of the supporting institutions.
Footnotes
Baytewar is an Ethiopian Amharic word used to refer to a stranger or someone who is socially isolated.
Author contributions
ES and TA initiated the burial surveillance. The study design was conceptualized by all authors. TA and GR were the fieldwork coordinators for the burial surveillance and verbal autopsy interviews, respectively. GR and NN carried out the analysis, and GR wrote the first draft of the manuscript. All authors contributed to the drafting of the manuscript and approved the final version.
References
- 1.UNAIDS. 2006 Report on the global AIDS epidemic. Geneva: UNAIDS; 2006. [Google Scholar]
- 2.Gill CJ, Hamer DH, Simon JL, Thea DM, Sabin LL. No room for complacency about adherence to antiretroviral therapy in sub-Saharan Africa. AIDS. 2005;19:1243–1249. doi: 10.1097/01.aids.0000180094.04652.3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mills EJ, Nachea JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America. JAMA. 2006;296:679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 4.Akileswaran C, Lurie M, Flanigan TP, Mayer KH. Lessons learned from use of highly active antiretroviral therapy in Africa. CID. 2005;41:376–385. doi: 10.1086/431482. [DOI] [PubMed] [Google Scholar]
- 5.UNAIDS. 2007 AIDS epidemic update. Geneva: UNAIDS/WHO; 2007. [Google Scholar]
- 6.Mathers CD, Ma Fat D, Inoue M, Chalapati R, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–177. [PMC free article] [PubMed] [Google Scholar]
- 7.Diaz T, Loth G, Whitworth J, Sutherland D. Surveillance methods to monitor the impact of HIV therapy programmes in resource-constrained countries. AIDS. 2005;19:S31–37. doi: 10.1097/01.aids.0000172875.67262.21. [DOI] [PubMed] [Google Scholar]
- 8.Setel PW, Macfarlane SB, Szreter S, Mikkelsen L, Jha P, Stout S, AbouZahr C. A scandal of invisibility: making everyone count by counting everyone. Lancet. 2007;370:1569–1577. doi: 10.1016/S0140-6736(07)61307-5. [DOI] [PubMed] [Google Scholar]
- 9.CSA. Results for Addis Ababa, Vol. I – Statistical report. Addis Ababa: Central Statistical Authority; 1995. The 1994 population and housing census of Ethiopia. [Google Scholar]
- 10.Lester FT, Ayehunie S, Zewdie D. Acquired immunodeficiency syndrome: Seven cases in Addis Ababa hospital. Ethiop Med J. 1988;26:139–145. [PubMed] [Google Scholar]
- 11.MOH. Single point HIV prevalence estimate. Addis Ababa: Ministry of Health; 2007. [Google Scholar]
- 12.CSA and ORC Macro. Ethiopia Demographic and Health Survey 2005. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ORC Macro; 2006. [Google Scholar]
- 13.MOH. Sixth report. Addis Ababa: Federal Ministry of Health; 2006. AIDS in Ethiopia; p. 51. [Google Scholar]
- 14.Reniers G, Araya T, Sanders EJ. Life table estimates of adult HIV/AIDS mortality in Addis Ababa. Ethiop J Health Dev. 2006;20:3–9. [Google Scholar]
- 15.Kloos H, Haile Mariam D, Lindtjorn B. The AIDS epidemic in a low income country: Ethiopia. Hum Ecol Rev. 2007;14:39–55. [Google Scholar]
- 16.IBRD. World development indicators. Washington, DC: IBRD/The World Bank; 2005. [Google Scholar]
- 17.HAPCO. [Accessed 1 December 2007];Ethiopia’s free ART eligibility criteria revised (press release) http://www.etharc.org/press/ethfreeartrevisedpress.htm.
- 18.MOH-HAPCO. [Accessed 4 November 2008];Monthly HIV care and ART update. http://www.etharc.org/arvinfo/index.htm.
- 19.Sanders EJ, Araya T, Kebede D, Schaap AJ, Nagelkerke Nico D, Coutinho RA. Mortality impact of AIDS in Addis Ababa, Ethiopia. AIDS. 2003;17:1209–1216. doi: 10.1097/00002030-200305230-00013. [DOI] [PubMed] [Google Scholar]
- 20.Araya T, Reniers G, Schaap A, Kebede D, Kumie A, Nagelkerke N, et al. Lay diagnosis of cause of death for monitoring AIDS mortality in Addis Ababa, Ethiopia. Trop Med Int Health. 2004;9:178–186. doi: 10.1046/j.1365-3156.2003.01172.x. [DOI] [PubMed] [Google Scholar]
- 21.Reniers G, Araya T, Schaap A, Kumie A, Kebede D, Nagelkerke N, et al. Monitoring cause-specific adult mortality in developing countries: a comparison of different data sources for Addis Ababa and their implications for policy and research. Soc Sci Med. 2005;61:1952–1957. doi: 10.1016/j.socscimed.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 22.Ford BL. An overview of hot-deck procedures. In: Madow WG, Olkin I, Rubin DB, editors. Incomplete data in sample surveys. New York: Academic Press; 1983. pp. 185–207. [Google Scholar]
- 23.Urassa M, Boerma JT, Isingo R, Ngalula J, Ng’weshemi J, Mwaluko G, Zaba B. The impact of HIV/AIDS on mortality and household mobility in rural Tanzania. AIDS. 2001;15:2017–2023. doi: 10.1097/00002030-200110190-00015. [DOI] [PubMed] [Google Scholar]
- 24.Clark SJ, Collinson MA, Kahn K, Drullinger K, Tollman SM. Returning home to die: circular labour migration and mortality in South Africa. Scand J Public Health Suppl. 2007;69:35–44. doi: 10.1080/14034950701355619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–245. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stover J. Projecting the demographic consequences of adult HIV prevalence trends: the Spectrum projection package. Sex Transm Infect. 2004;80:i14–18. doi: 10.1136/sti.2004.010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinfu Y. Below-replacement fertility in tropical Africa? Some evidence from Addis Ababa. J Popul Res. 2000;17:63–82. [Google Scholar]
- 28.Sibanda A, Woubalem Z, Hogan DP, Lindstrom DP. The proximate determinants of the decline to below-replacement fertility in Addis Ababa, Ethiopia. Stud Fam Plann. 2003;34:1–7. doi: 10.1111/j.1728-4465.2003.00001.x. [DOI] [PubMed] [Google Scholar]
- 29.Ghys PD, Brown T, Grassly NC, Garnett GP, Stanecki KA, Stover J, Walker N. The UNAIDS Estimation and Projection Package: a software package to estimate and project national HIV epidemics. Sex Transm Infect. 2004;80:i5–i9. doi: 10.1136/sti.2004.010199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fontanet A, Messele T, Dejene A, Enquselassie F, Abebe A, Cutts FT, et al. Age-and sex-specific HIV-1 prevalence in the urban community setting of Addis Ababa, Ethiopia. AIDS. 1998;12:315–322. doi: 10.1097/00002030-199803000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 32.Chiasson MA, Berenson L, Li W, Schwartz S, Singh T, Forlenza S, et al. Declining HIV/AIDS mortality in New York city. J Acquir Immune Defic Syndr. 1999;21:59–64. doi: 10.1097/00126334-199905010-00008. [DOI] [PubMed] [Google Scholar]
- 33.Antunes JL, Waldman EA, Borrell C. Is it possible to reduce AIDS deaths without reinforcing socioeconomic inequalities in health? Int J Epidemiol. 2005;34:586–592. doi: 10.1093/ije/dyi022. [DOI] [PubMed] [Google Scholar]
- 34.Ivers LC, Kendrick D, Doucette K. Efficacy of antiretroviral therapy programs in resource-poor settings: A meta-analysis of the published literature. CID. 2005;41:217–224. doi: 10.1086/431199. [DOI] [PubMed] [Google Scholar]
- 35.Braitstein P, Brinkhof MWG, Dabis F, Schechter M, Boulle A, Miotti P, et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367:817–824. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- 36.Lawn SD, Myer L, Orrell C, Bekker L-G, Wood R. Early mortality among adults accessing a community-based antiretroviral service in South Africa: implications for programme design. AIDS. 2005;19:2141–2148. doi: 10.1097/01.aids.0000194802.89540.e1. [DOI] [PubMed] [Google Scholar]
- 37.Egger M, Boulle A, Schechter M, Miotti P. Antiretroviral therapy in resource-poor settings: scaling up inequalities? Int J Epidemiol. 2005;34:509–512. doi: 10.1093/ije/dyi110. [DOI] [PubMed] [Google Scholar]
- 38.Jahn A, Floyd S, Crampin AC, Mwaungulu F, Mvula H, Munthali F, et al. Population-level effect of HIV on adult mortality and early evidence of reversal after introduction of antiretroviral therapy in Malawi. Lancet. 2008;371:1603–1611. doi: 10.1016/S0140-6736(08)60693-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Egger M, Boulle A. Population effect of scaling up ART in resource-poor settings. Lancet. 2008;371:1558–1559. doi: 10.1016/S0140-6736(08)60669-8. [DOI] [PubMed] [Google Scholar]