Summary
Surgical treatment for cancer of the oral cavity can result in dramatic aesthetic and functional sequelae partially avoidable by reconstructive techniques. Many studies concerning quality of life have been carried out in order to retrospectively assess outcomes after such major oncological procedures. Aim of this study was to evaluate, in a prospective fashion, the quality of life as a primary endpoint in patients treated for cancers involving the oral cavity and requiring reconstruction. The study design consisted of a prospective evaluation of pre- and post-operative quality of life at 3, 6, and 12 months to assess variations during follow-up using two different questionnaires: the University of Washington Quality of Life and the Head and Neck Performance Status Scale. Between May 1999 and October 2004, 92 patients with oral cancer requiring reconstruction were treated. All were included in the study, but only 35 (38%) concluded the evaluation protocol at one year after surgery without evidence of disease. The mean pre- and post-operative (3, 6, and 12 months) scores of the questionnaires and the scores of specific University of Washington Quality of Life categories (disfigurement, chewing, swallowing, comprehension of speech) were evaluated. The impact on residual quality of life of different factors such as gender, extension of tongue and mandibular defects, type of reconstruction, and radiotherapy was statistically quantified with a Wilcoxon non-parametric test and logistic regression for multivariate analysis. Comparison of mean pre- and post-operative scores between the University of Washington Quality of Life and Head and Neck Performance Status Scale, showed a similar trend during the study period with a significant decrease at 3 months after surgery and subsequent gradual improvement at 6 and 12 months. The majority of patients (77%) preserved normal or near normal functions at 12 months after surgery. The chewing domain worsened considerably (p < 0.05), with poorer outcome in patients undergoing segmental mandibulectomy (p < 0.05). By multivariate analysis, mandibular resection maintained its statistical significance in the chewing domain (p = 0.038). Moreover, the type of reconstruction was an independent factor (p = 0.038) that influenced the University of Washington Quality of Life total score, with better functional results after free flap reconstruction. Despite the dismal prognosis of patients affected by advanced oral cavity cancer, reconstructive techniques play a crucial role in maintenance of satisfactory quality of life.
Keywords: Oral cavity cancer, Reconstructive surgery, Quality of life
Riassunto
Il trattamento chirurgico del cancro del cavo orale può esitare in drammatiche sequele estetiche e funzionali parzialmente evitabili mediante l’impiego di tecniche ricostruttive. Molti studi riguardanti la qualità della vita (“quality of life”, QoL) sono stati eseguiti al fine di valutare retrospettivamente i risultati ottenuti dopo tali procedure oncologiche maggiori. Scopo del presente lavoro è quello di valutare in maniera prospettica come obiettivo principale la QoL in pazienti trattati per cancro del cavo orale che abbia richiesto un tempo ricostruttivo. La pianificazione dello studio ha incluso una valutazione prospettica della QoL pre-operatoriamente e post-operatoriamente a 3, 6 e 12 mesi al fine di valutarne le variazioni durante il follow-up usando due diversi questionari: l’University of Washington Quality of Life (UW-QoL) e l’Head and Neck Performance Status Scale (PSS-HN). Tra il maggio 1999 e l’ottobre 2004, 92 pazienti con cancro del cavo orale sono stati trattati presso la nostra Clinica mediante chirurgia seguita da un tempo ricostruttivo. Tutti sono stati inclusi nello studio, ma soltanto 35 (38%) hanno portato a termine il protocollo di valutazione ad 1 anno dall’intervento senza alcuna evidenza di ripresa della malattia. I punteggi medi pre- e post-operatori a 3, 6 e 12 mesi e quelli delle specifiche categorie dell’UW-QoL (disestetismo, masticazione, deglutizione e comprensibilità dell’eloquio) sono stati valutati. L’impatto di diversi fattori, quali il sesso, l’estensione del difetto linguale e mandibolare, il tipo di ricostruzione utilizzata e l’impiego della radioterapia, sulla QoL è stato quantificato mediante un test non parametrico di Wilcoxon ed una regressione logistica con analisi multivariata. Il confronto dei punteggi medi pre- e post-operatori tra l’UW-QoL ed il PSS-HN ha mostrato un andamento simile durante il periodo di studio, con un significativo peggioramento della QoL a 3 mesi dall’intervento ed un successivo, graduale miglioramento a 6 e a 12 mesi. La maggior parte dei pazienti (77%) ha preservato funzioni normali o quasi normali a 12 mesi dall’intervento. La masticazione è peggiorata in modo significativo (p < 0,05), con risultati peggiori in quei pazienti sottoposti a mandibulectomia segmentaria (p < 0,05). All’analisi multivariata, la resezione mandibolare ha mantenuto il suo livello di significatività statistica per quanto riguarda il punteggio della masticazione (p = 0,038). Inoltre, il tipo di ricostruzione impiegato si è dimostrato un fattore indipendente (p = 0,038) nell’influenzare il punteggio totale dell’UW-QoL, con risultati funzionali migliori dopo ricostruzione mediante lembi liberi. Nonostante la prognosi infausta dei pazienti affetti da cancro del cavo orale in stadio avanzato, le tecniche ricostruttive giocano un ruolo cruciale nel mantenimento di una soddisfacente QoL post-operatoria.
Introduction
Surgical treatment for cancer of the oral cavity has important effects on the quality of life (QoL), which has been defined as the perceived discrepancy between the actual status and the ideal standards of the patient 1. Aesthetic and functional sequelae due to surgical incision and cancer resection, often associated with pre- or post-operative radiotherapy (RT), always modify the patient’s self-perception and the ability to interact with others in daily social life. While body scars and alterations are usually hidden during social activities, and dramatic situations such as permanent colostomy or vascular shunt for dialysis can be easily managed in public, head and neck cancer patients cannot hide post-treatment functional changes and must, therefore, deal with the subsequent negative impact on self-esteem and confidence in all realms 2.
Remarkable advances in head and neck reconstructive techniques have greatly improved aesthetic and functional results and the main goal in the management of such cases is to treat the patient while preserving a QoL that is compatible with satisfactory self-acceptance and interpersonal social relationships 3.
Aim of this prospective study was to evaluate changes in the QoL from pre-operative levels during the 12-month post-operative period using specific questionnaires of well-known acceptability, responsiveness, and validity, with special emphasis on domains such as chewing, swallowing, speech, and disfigurement. Moreover, the impact on QoL of different factors such as gender, mandibular and tongue resection, pre- and/or post-operative RT, and type of reconstruction was statistically evaluated.
Patients and methods
From May 1999 to October 2004, 92 patients (67 male, 25 female; mean age 58 years; range 35-79) affected by cancer of the oral cavity underwent surgical treatment including primary reconstruction with flap transposition at the Department of Otorhinolaryngology – Head and Neck Surgery of the University of Brescia, Italy. The lesion only involved the oral cavity in 55 (59.8%) cases and extended to the oropharynx in 37 (40.2%). A total of 46 (50%) patients underwent salvage surgery following previous treatment (for recurrence in 26 patients, persistence in 17, and a second tumour in 3). Overall, 44 (48%) patients were submitted to post-operative adjuvant RT or concomitant chemo-RT. All lesions were diagnosed as squamous cell carcinoma (SCC), except for one case of adenoid cystic carcinoma (ACC). Tumour stage was assessed according to the latest edition of the TNM Staging System 4. The pT category was as follows: T1 in 8 cases, T2 in 28, T3 in 11, T4a in 41, and T4b in 4. The surgical approach was a mandibular swing in all cases, except one in which a “pull-through” technique was applied. Mandibular resection was performed in 32 (35%) patients (marginal in 15 cases and segmental in 17).
In order to correctly evaluate post-operative functional outcomes, surgical defects of the tongue, floor of mouth, soft palate, oropharynx, and mandible were quantified using the classification proposed by Urken et al. 3. Tongue defects were classified as less than 25%, between 25% to 50% (hemiglossectomy), and more than 50% up to total glossectomy. Even though the base of the tongue is an oropharyngeal subsite, and the mobile tongue an oral subsite, we considered them as a single functional entity. Floor of mouth defects were subdivided into lateral, anterior, and antero-lateral on the basis of an ideal transversal line passing through the lingual carunculae. Mandibulectomy was defined as either marginal (rim mandibulectomy) or segmental. The latter was further classified into anterior, lateral limited to the mandibular body, lateral without condylar involvement, and lateral with condyle resection. Soft palate defects were classified as more or less than 50%. Oropharyngeal resections were limited to the lateral wall and tonsillar fossa or extended to the posterior wall.
All patients underwent a swallow and speech rehabilitation programme starting from post-operative day 7 if the post-operative course was uncomplicated. The study consisted of prospective evaluation of pre- and post-operative (at 3, 6, and 12 months) QoL using two questionnaires submitted to the patients in an interview format administered by the physician, namely the University of Washington Quality of Life Questionnaire (UW-QoL) 5 and the Head and Neck Performance Status Scale (PSS-HN) 6. The UW-QoL questionnaire assesses 9 specific domains (pain, disfigurement, activity, recreation-entertainment, employment, speech, chewing, swallowing, and shoulder disability), and a composite score is calculated by adding together the 9 partial scores from 195 to 900. Due to its easier and quicker format, it was preferred to the UW-QoL version 2, which is characterized by adjunctive items and importance-ratings 7. The PSS-HN tests 3 areas (normalcy of diet, speech, and eating in public) with a score ranging from 0 to 100 for each domain. The use of two different tools allowed us to cross-verify the reliability of each by a separate evaluation of the trend of scores for both questionnaires during the study period.
All 92 patients were evaluated in terms of pre-operative QoL. However, data could be collected from only 35 (38%) of these who were alive, without evidence of disease, during the entire study period (12 months). Four patients, alive with disease at the end of the study period, were excluded from the performance evaluation due to the possible interaction between neoplastic symptoms and functional results. The final study population thus included 21 males and 14 females, ranging in age from 36 to 79 years (mean, 58). The tumour was limited to the oral cavity in 26 patients and extended to the oropharynx in 9. All the lesions were diagnosed as SCC except for one ACC. Of these cases, 18 (51%) underwent salvage surgery following previous treatment (RT in 10 cases, chemotherapy in 2, and surgery in 6). Furthermore, in 28 (80%) patients the lesion was at an advanced stage (Stage III in 7 cases and Stage IVa in 21). The distribution of patients by pT and pN categories is shown in Table I. The surgical approach included a mandibular swing in all cases.
Table I. pT and pN staging of 34 patients with SCC (1 patient with ACC was excluded).
| pN0 | pN1 | pN2b | pN2c | ||
| pT1 | - | 1 | - | - | 1 (3%) |
| pT2 | 7 | 2 | 3 | - | 12 (35%) |
| pT3 | 3 | 1 | 2 | - | 6 (18%) |
| pT4a | 7 | 5 | 2 | 1 | 15 (44%) |
| 17 (50%) | 9 (27%) | 7 (20%) | 1 (3%) | 34 |
Soft tissues defects were classified as follows: tongue, less than 25% in 14 cases, 25% to 50% defect in 17, and more than 50% in 3; floor of mouth, lateral in 14 cases, anterior in 3, antero-lateral in 6, and total in 1; soft palate, less than 50% in 6 cases and more than 50% in one. Surgical resection was extended to the lateral wall and tonsillar fossa in 15 cases and to the posterior wall in one. Mandibular resection, performed in 13 patients, was marginal in 5 (14%) cases and segmental in 8 (23%). Segmental resection was anterior in 4 cases, limited to the horizontal branch in one, and lateral with condylar preservation in 2.
In 3 cases (9%), surgical revision with a second flap transposition due to major complications (partial or total necrosis and oro-cutaneous fistula) at the first reconstructive attempt was necessary. Of the 38 flaps harvested, 9 (23%) were pedicled (6 myocutaneous pectoralis major, 2 platysma, and one upper trapezius) and 29 (77%) revascularized (20 forearm, 6 fibula, one antero-lateral thigh, one rectus abdominis, and one lateral arm).
A total of 22 patients (63%) received post-operative adjuvant treatment: conventional RT in 19 cases, chemotherapy in one patient previously treated with conventional RT, and concomitant chemo-RT in 2.
To simplify the UW-QoL evaluation and subsequent comparisons, the total scores were arbitrarily subdivided into 3 major categories: group 1, as normal or near normal, for values ranging from 900 to 700; group 2, as mild disability, from 699 to 500; and group 3, as severe disability, from 499 to 195. The score of each domain of the UW-QoL questionnaire was also divided into 3 groups: group 1, as normal or near normal, from 100 to 75; group 2, as mild disability, 50 or 60; and group 3, as severe disability, 25 or 20. In this way, it was possible to better compare functional results and evaluate their trends during the study period.
At the time of enrolment in the study, patients’ specific concerns regarding residual QoL were noted in order to identify the domains considered more crucial in the post-treatment and rehabilitation period. Findings emerging from these data prompted the authors to specifically focus the analysis on the following UW-QoL domains: disfigurement, chewing, swallowing, and comprehension of speech. Moreover, the impact on such domains of the same variables were evaluated (gender for disfigurement and pre- or post-operative RT, amount of tongue resection, mandibular defect, and type of reconstruction for the other domains) at the end of the study period. These domains were specifically chosen since they were considered crucial by the majority of patients and more directly related to the previously mentioned variables. Statistical analysis was performed using a Wilcoxon non-parametric test with 3x3 cross tables and logistic regression for multivariate analysis.
Results
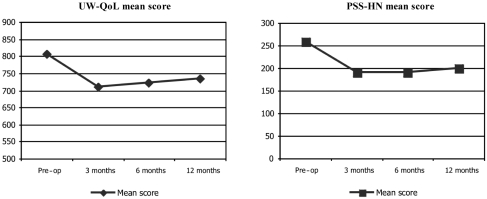
Patients invariably had a poorer QoL after surgery, which dramatically decreased during the first 3 months after treatment. At one year, most patients reported an improvement in functions, except those who presented low pre-operative and early post-operative scores. Nevertheless, pre-operative scores were never exceeded, nor reached. This trend was observed for both questionnaires confirming their good cross-relations and satisfying inter-reliability (Fig. 1). On account of the more detailed structure and precise analysis of domains such as disfigurement, chewing, swallowing, and speech, the UW-QoL was chosen for subsequent statistical evaluations.
Fig. 1.
Mean scores of both questionnaires during study period.
Although statistical significance was not reached in the UW-QoL total scores even in relation to pre- or post-operative RT, tongue resection, mandibular resection, and type of reconstruction, “chewing” domain was statistically significant in the pre-operative vs. 12-month post-operative comparison in a 3x3 cross table (p < 0.05). In particular, this specific function significantly decreased when starting from normal or near normal conditions, while it improved when starting from severe disability (Table II). Moreover, a significant worsening of chewing function was detected in relation to mandibular resection when comparing patients with preserved mandible or submitted to marginal resection with those submitted to segmental resection (p < 0.05). In contrast, tongue resection did not statistically influence chewing, swallowing, and speech, that was intelligible by phone for all patients and considered normal or near normal by 94% of them. No statistically significant difference was reported in terms of disfigurement between males and females.
Table II. Modifications of chewing function at 12 months after surgery (p < 0.05): numbers in bold indicate patients with poorer function, from normal (1 pre-op) or mild disability (2 pre-op), to mild (2 post-op) or severe disability (3 post-op). In contrast, underlined numbers indicate patients with improved function, from mild (2 pre-op) or severe disability (3 pre-op), to normal (1 post-op) or mild disability (2 post-op).
| 1 post-op (12 months) | 2 post-op (12 months) | 3 post-op (12 months) | |
| 1 pre-op | 3 | 14 | 5 |
| 2 pre-op | 1 | 5 | 3 |
| 3 pre-op | 1 | 2 | 1 |
Multivariate analysis on UW-QoL total scores showed the type of reconstruction (pedicled vs. free flap) to be the only independent factor influencing the overall functional result and better outcomes were seen in patients undergoing free flap reconstruction (p = 0.038) (Table III). Moreo-ver, when multivariate analysis was selectively applied to the chewing domain, segmental mandibulectomy significantly correlated with poorer functional results (p = 0.038) (Table IV).
Table III. Multivariate analysis by logistic regression of UW-QoL total scores, according to mandibular resection, tongue resection, radiotherapy (RT), and type of reconstruction.
| Mandibular resection | p = 0.55 |
| No resection + marginal | |
| Segmental resection | |
| Tongue resection | p = 0.82 |
| T1 M/B | |
| T2 M/B | |
| T3 M/B | |
| RT | p = 0.25 |
| RT pre-op | |
| RT post-op | |
| Type of reconstruction | p = 0.038 |
| Free flap | |
| Pedicled flap |
T1 = Tongue resection less than 25%; T2 = between 25% to 50% (hemiglossectomy); T3 = more than 50% up to total glossectomy; M = mobile tongue; B = base of tongue.
Table IV. Multivariate analysis by logistic regression of chewing domain scores, according to mandibular resection, tongue resection, radiotherapy (RT), and type of reconstruction.
| Mandibular resection | p = 0.038 |
| No resection + marginal | |
| Segmental resection | |
| Tongue resection | p = 0.88 |
| T1 M/B | |
| T2 M/B | |
| T3 M/B | |
| RT | p = 0.32 |
| RT pre-op | |
| RT post-op | |
| Type of reconstruction | p = 0.25 |
| Free flap | |
| Pedicled flap |
T1 = Tongue resection less than 25%; T2 = between 25% to 50% (hemiglossectomy); T3 = more than 50% up to total glossectomy; M = mobile tongue; B = base of tongue.
Discussion
Many studies dealing with QoL in head and neck cancer have been based on heterogeneous groups of patients with respect to the site and stage of tumour, and were often retrospective 1 7–11. Only a few prospective studies have focused on a specific anatomic site 12–16. Other information concerning post-operative QoL adjustments and influencing factors are scattered throughout the literature as personal observations or clinical impressions, although very few have been supported by statistical analysis.
In prospective studies, a marked decrease in terms of cumulative questionnaire scores in the early post-operative period has always been detected, with subsequent light recovery at one year, probably as a result of progressive adaptation and coping processes 15 17–19, with comparable and stable functional results in the subsequent period for long-term survivors 20. Discordant information has also been reported, with stable lower scores during the post-operative period 21.
In patients treated for oral primaries, better results, in terms of residual QoL, have been reported in those not requiring reconstructive flaps and adjuvant RT (i.e., T1 and small T2 lesions), with higher cumulative UW-QoL scores at 6 months and 1 year, yielding fewer problems in terms of disfigurement, chewing, and swallowing 15. Using a single assessing item, Bundgaard et al. 22 reported a higher residual QoL in patients treated with surgery alone compared with those submitted to adjuvant RT. Multimodal treatments obviously increase side-effects with subsequent deterioration of residual QoL. Allal et al. 23 reported a trend towards significantly better scores for emotional, physical, and social functions as well as for pain and dyspnoea symptoms in patients with T3-T4 oro-pharyngeal cancer, alive without disease treated with radical RT (± chemotherapy), compared to patients treated with surgery and adjuvant RT. It is worth noting that objective difficulties exist in evaluating the influence of RT in terms of QoL for lesions in an advanced stage, since post-operative RT is almost invariably performed in patients with advanced disease. Moreover, when comparing patients that were or were not submitted to post-operative RT, other major factors, such as the extent of surgical defect and the need for reconstruction, were frequently hidden as main issues that are responsible for functional outcome.
Patients with extensive defects, especially when reconstructed by pedicled flaps, reported worse functional results 16 24. Vaughan et al. 25 reported functional improvement and better social adaptation after the introduction of free flaps, but did not validate these data using a questionnaire. Their observations were nonetheless confirmed by our study, which identified the type of reconstruction as the only significant variable at the multivariate analysis, with better functional results and higher scores after free flap reconstruction. In fact, thin and pliable free flaps harvested for soft tissue reconstruction, such as the forearm or antero-lateral thigh not only allow better adaptation to the three-dimensional geometry of the surgical defect, but also optimize residual function of spared anatomical structures.
In this perspective, some authors have focused on residual tongue mobility, a factor which in terms of functional outcome is much more crucial than the amount of preserved tongue 24. These data were confirmed also by our results. In fact, the amount of tongue resection did not statistically influence functional outcomes in chewing, swallowing, and speech domains. It is our policy to preserve residual tongue mobility as much as possible using thin and pliable forearm free flap. In contrast, when a large portion of the base of the tongue was resected, we chose perforated fascio-cutaneous rectus abdominis or antero-lateral thigh flap, especially in the event of laryngeal preservation, because of their thickness allowing bulky reconstruction with better swallowing results.
The chewing domain was dramatically compromised in our series. Many authors previously stressed the crucial role of residual dental status 19, mandibular reconstruction by bony free flaps such as the fibula or the iliac crest 26, and osteo-integrated dental rehabilitation 27. In contrast, in our series, pre-operatively edentulous patients also reported poorer chewing during the post-operative period. In fact, dental status and prosthetic rehabilitation play only a partial role in chewing ability, which is also strongly influenced, for oral bolus management, by residual tongue mobility and oral sensitivity. Moreover, especially for advanced cancers of the retromolar trigone extending to the tonsillar region, resection of the pterygoid muscles always leads to heavy trismus that, in many cases, is irreversible and extremely invalidating. Regarding osteo-integrated dental rehabilitation, it is our policy to start this procedure at least 18 months after surgery for oncologic reasons, high risk of mandibular fracture and infection due to pre- or post-operative RT, and high costs. For all these reasons, none of the patients, in the present series, were submitted to osteo-integrated dental rehabilitation during the 12-month study period.
In terms of aesthetic results and disfigurement, the large majority of patients (89%), with no statistical difference between males and females, considered their appearance as normal or near normal, confirming the low aesthetic impact of the mandibular swing approach and cervicotomy for neck dissection 2. Perception of severe disfigurement for head and neck surgery was traditionally reported for non-reconstructed anterior mandibulectomy, causing the so-called “Andy Gump” deformity 28.
The prospective study, reported here, has clarified and statistically confirmed some principles on residual QoL for patients treated by surgical resection and flap reconstruction for cancer of the oral cavity already presented in the literature. However, many previous studies failed to identify a statistically significant relationship between clinical para-meters and functional outcomes, probably on account of the cross-sectional design and grouping of different head and neck sites and treatment modalities. The results and trends described are limited by the small sample of patients completing questionnaires at one year after surgery. However, improvement in terms of QoL due to free flap transfer introduction was confirmed. Moreover, the chewing domain was heavily compromised in this subset of patients, especially when mandibular segmental resection was performed. Taking into account our previously reported observations on the high prevalence of segmental mandibulectomies without evidence of bone infiltration (53%) 29, segmental resection, in the case of a documented uninvolved mandible, should be performed only when safe oncologic resection into the surrounding soft tissues cannot be otherwise obtained.
Conclusions
We are in agreement with Maher et al. that there is always a significant discrepancy between perceptions concerning the daily impact of post-operative disabilities on QoL 30. The trend in physicians is to overestimate the more objective “treatable” symptoms and to underestimate more subjective problems. Our data may be useful in a pre-operative setting, during patient counselling, offering the possibility to provide more detailed information concerning transient or persistent symptoms and disabilities resulting from treatment, always bearing in mind that prolongation of a patient’s life always has a price in terms of residual QoL.
References
- 1.Morton RP. Evaluation of quality of life assessment in head and neck cancer. J Laryngol Otol 1995;109:1029-35. [DOI] [PubMed] [Google Scholar]
- 2.Breitbart W, Holland J. Psychosocial aspects of head and neck cancer. Semin Oncol 1988;15:61-9. [PubMed] [Google Scholar]
- 3.Urken ML, Buchbinder D, Weinberg H, Vickery C, Sheiner A, Parker R, et al. Functional evaluation following microvascular oromandibular reconstruction of the oral cancer patient: a comparative study of reconstructed and nonreconstructed patients. Laryngoscope 1991;101:935-50. [DOI] [PubMed] [Google Scholar]
- 4.Green FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC Cancer Staging Manual. 6th edition. New York: Springer; 2002. [Google Scholar]
- 5.Hassan SJ, Weymuller EA. Assessment of quality of life in head and neck cancer patients. Head Neck 1993;15:485-90. [DOI] [PubMed] [Google Scholar]
- 6.List MA, Ritter-Sterr C, Lansky SB. A performance status scale for head and neck cancer patients. Cancer 1990;66:564-8. [DOI] [PubMed] [Google Scholar]
- 7.Deleyiannis FW, Weymuller EA. Outcomes research in head and neck oncology. Curr Opin Otolaryngol Head Neck Surg 1996;4:73-7. [Google Scholar]
- 8.Gotay CC, Moore TD. Assessing quality of life in head and neck cancer. Qual Life Res 1992;1:5-17. [DOI] [PubMed] [Google Scholar]
- 9.Jones E, Lund VJ, Howard DJ, Greenberg MP, McCarthy M. Quality of life of patients treated surgically for head and neck cancer. J Laryngol Otol 1992;106:238-42. [DOI] [PubMed] [Google Scholar]
- 10.Long SA, D’Antonio LL, Robinson EB, Zimmerman G, Petti G, Chonkich G. Factors related to quality of life and functional status in 50 patients with head and neck cancer. Laryngoscope 1996;106:1084-8. [DOI] [PubMed] [Google Scholar]
- 11.McDonough EM, Varvares MA, Dumphy FR, Dunleavy T, Dumphy CH, Boyd JH. Changes in quality of life scores in a population of patients treated for squamous cell carcinoma of the head and neck. Head Neck 1996;18:487-93. [DOI] [PubMed] [Google Scholar]
- 12.Deleyiannis FW, Weymuller EA, Coltrera MD. Quality of life in disease-free survivors of advanced (stage III or IV) oropharyngeal cancer. Head Neck 1997;19:466-73. [DOI] [PubMed] [Google Scholar]
- 13.Hammerlid E, Mercke C, Sullivan M, Westin T. A prospective quality of life study of patients with oral or pharyngeal carcinoma treated with external beam irradiation with or without brachytherapy. Oral Oncol 1997;33:189-96. [DOI] [PubMed] [Google Scholar]
- 14.List MA, Ritter-Sterr CA, Baker TM, Colangelo LA, Matz G, Pauloski BR, et al. Longitudinal assessment of quality of life in laryngeal cancer patients. Head Neck 1996;18:1-10. [DOI] [PubMed] [Google Scholar]
- 15.Rogers SN, Lowe D, Brown JS, Vaughan ED. The University of Washington head and neck cancer measure as a predictor of outcome following primary surgery for oral cancer. Head Neck 1999;21:394-401. [DOI] [PubMed] [Google Scholar]
- 16.Schliephake H, Ruffert K, Schneller T. Prospective study of the quality of life of cancer patients after intraoral tumor surgery. J Oral Maxillofac Surg 1996;54:664-9. [DOI] [PubMed] [Google Scholar]
- 17.de Graeff A, de Leeuw JRJ, Ros WJG, Hordijk GJ, Blijham GH, Winnubst JAM. A prospective study on quality of life of patients with cancer of the oral cavity or oropharynx treated with surgery with or without radiotherapy. Oral Oncol 1999;35:27-32. [DOI] [PubMed] [Google Scholar]
- 18.Rogers SN, Humphris G, Lowe D, Brown JS, Vaughan ED. The impact of surgery for oral cancer on quality of life as measured by the medical outcomes short form 36. Oral Oncol 1998;34:171-9. [DOI] [PubMed] [Google Scholar]
- 19.Rogers SN, Lowe D, Fisher SE, Brown JS, Vaughan ED. Health-related quality of life and clinical function after primary surgery for oral cancer. Br J Oral Maxillofac Surg 2002;40:11-8. [DOI] [PubMed] [Google Scholar]
- 20.Rogers SN, Hannah L, Lowe D, Magennis P. Quality of life 5-10 years after primary surgery for oral and oro-pharyngeal cancer. J Craniomaxillofac Surg 1999;27:187-91. [DOI] [PubMed] [Google Scholar]
- 21.Markkanen-Leppänen M, Mäkitie AA, Haapanen ML, Suominen E, Asko-Seljavaara S. Quality of life after free-flap reconstruction in patients with oral and pharyngeal cancer. Head Neck 2006;28:210-6. [DOI] [PubMed] [Google Scholar]
- 22.Bundgaard T, Tandrup O, Elbrond O. A functional evaluation of patients treated for oral cancer. A prospective study. Int J Oral Maxillofac Surg 1993;22:28-34. [DOI] [PubMed] [Google Scholar]
- 23.Allal AS, Nicoucar K, Mach N, Dulguerov P. Quality of life in patients with oropharynx carcinomas: assessment after accelerated radiotherapy with or without chemotherapy versus radical surgery and postoperative radiotherapy. Head Neck 2003;25:833-40. [DOI] [PubMed] [Google Scholar]
- 24.Schliephake H, Schmelzeisen R, Schonweiler K, Schiller T, Henbernd C. Speech, deglutition and life quality after intra-oral tumour resection: a prospective study. Int J Maxillofac Surg 1998;27:99-105. [DOI] [PubMed] [Google Scholar]
- 25.Vaughan ED, Bainton R, Martin IC. Improvements in morbidity of mouth cancer using microvascular free flap reconstructions. J Craniomaxillofac Surg 1992;20:132-4. [DOI] [PubMed] [Google Scholar]
- 26.Wilson KM, Rizk NM, Armstrong SL, Gluckman JL. Effects of hemimandibulectomy on quality of life. Laryngoscope 1998;108:1574-7. [DOI] [PubMed] [Google Scholar]
- 27.Rogers SN, McNally D, Mahmoud M, Chan M, Humphris GM. The psychological response of the edentulous patient following primary surgery for oral cancer: a cross-sectional study. J Prosthet Dent 1999;82:317-21. [DOI] [PubMed] [Google Scholar]
- 28.Dropkin MJ, Malgady RG, Scott DW, Oberst MT, Strong EW. Scaling of disfigurement and dysfunction in postoperat-ive head and neck patients. Head Neck Surg 1983;6:559-70. [DOI] [PubMed] [Google Scholar]
- 29.Bolzoni A, Cappiello J, Piazza C, Peretti G, Maroldi R, Farina D, et al. Diagnostic accuracy of magnetic resonance imaging in the assessment of mandibular involvement in oral-oropharyngeal squamous cell carcinoma. A prospective study. Arch Otolaryngol Head Neck Surg 2004;130:837-43. [DOI] [PubMed] [Google Scholar]
- 30.Maher EJ, Goodman S, Jefferis A. Decision-making in the management of advanced cancer of the head and neck. Differences in perspective between doctor and patients: future avenues for research. Palliat Med 1990;4:185-9. [Google Scholar]