Summary
Hibernoma is an unusual tumour of brown adipose tissue. Brown adipose tissue is common in mammalian hibernating animals and acts as a thermogenic organ. A first case of hibernoma was reported in 1906 by Merkel. This tumour usually arises in the back, shoulder region, mediastinum, retroperitoneum and in the neck. The neck location of hibernomas is rare and only 18 cases of cervical hibernoma have been reported in the English literature. A 48-year-old male with hoarseness and soft voice, present for 8 months, showed a lesion involving the anterior part of the right vocal fold, with no impaired mobility. This is the first case to be reported of laryngeal hibernoma located in a vocal fold, originating from the white fat tissue of the paraglottic space. Moreover, this report could be evidence of the development of hibernoma from white adipose tissue.
Keywords: Larynx, Benign tumour, Soft tissue tumour, Hibernoma
Riassunto
L’hibernoma è un raro tumore che origina dal tessuto grasso bruno. Il grasso bruno è comunemente presente nei mammiferi ed espleta la funzione di organo termogenico. Il primo caso di hibernoma è stato riportato nel 1906 da Merkel 3. Di solito questo tumore si riscontra a livello della schiena, delle spalle, nel mediastino, nel retroperitoneo e nel collo. La localizzazione cervicale è rara ed ad oggi riportata solo in 18 casi. Riportiamo il caso di un uomo di 48 anni con disfonia da 8 mesi, all’esame obiettivo si evidenziava una lesione laringea a carico della porzione anteriore della corda vocale vera di destra senza alterazioni della mobilità. Questo è il primo caso riportato di hibernoma della corda vocale ad origine dal grasso bianco dello spazio paraglottico. Proprio questa localizzazione particolare potrebbe aiutare a capire meglio la patogenesi dell’hibernoma.
Introduction
Hibernomas are rare, benign, subcutaneous neoplasms originating from immature brown fat. Brown adipose tissue is common in mammalian hibernating animals and acts as a thermogenic organ; in human, it is present at foetal status and decreases with development. Remnants of brown fat may persist in the inter-scapular region, mediastinum, axillae, retroperitoneum and neck.
The neck location of hibernomas is rare, and has been reported as a cervical mass. To date, in the English literature (PUBMED), 18 cases of cervical hibernoma have been reported, and only one of these has been observed in the pre-epiglottic area of the larynx. In this regard, it is worthwhile noting that brown adipose tissue has never been recorded, in this anatomic site before. The present report refers to the first case located in the glottic area, at paraglottic space level.
Case report
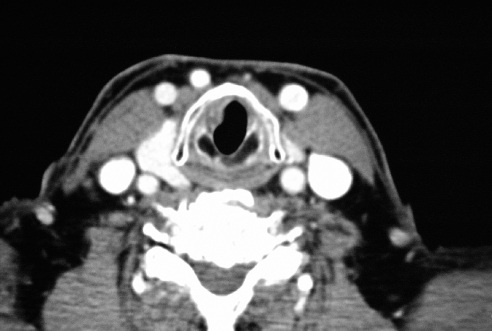
A 48-year-old male with an unremarkable medical history was admitted at the ENT Department with an 8 months’ history of hoarseness and soft voice, without dysphagia and dyspnoea. Clinical examinations, including 70° laryngeal endoscopy and computed tomography (CT) scan (Fig. 1), showed a lesion involving the anterior part of the right vocal fold, with no impaired mobility. There was no evidence of masses in the neck.
Fig. 1.
CT scan shows tumour involving right vocal fold.
A direct microlaryngoscopy was performed under general anaesthesia, and a 2 cm nodular and soft tumour, located in the submucosa of the subglottic and glottic region, was completely removed; the vocal ligament was carefully respected. The patient was discharged the same day without complications.
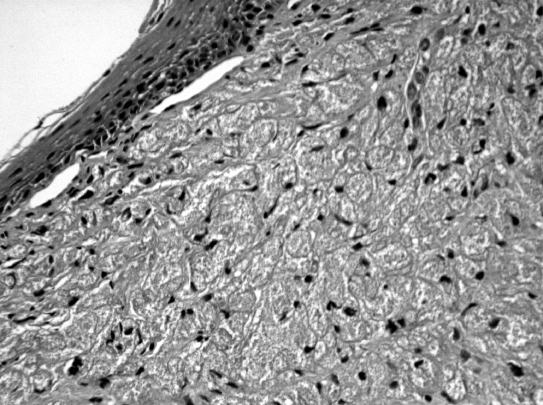
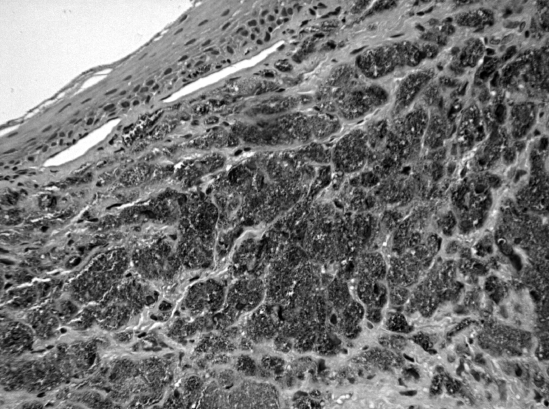
The gross pathology of the tumour was characterized by a homogeneously coloured yellow-brown neoplasm with well-defined borders. The specimen borders were free of disease. The histopathological examination revealed a submucosal tumour consisting of neoplastic cells with large eosinophilic cytoplasm, regular nucleus with small nucleoli (Fig. 2). These neoplastic cells were immunoreactive for S-100 (Fig. 2B) protein and vimentin, and were negative for cytokeratin and actin. A diagnosis of laryngeal hibernoma was made.
Fig. 2.
Tumour consists of diffuse proliferation of large cell characterized by coarsely multi-vacuolated cytoplasms. Neither atypia nor mitotic activity was detected. B: positive test for S100 (A: H&E x 250HPF).
One year after surgery, the patient showed no recurrence, voice was good and stroboscopy showed normal vibration.
Discussion
In 1906, Merkel 1 described the first brown fat tumour as a pseudolipoma of the breast, the term hibernoma was coined in 1914 2 due to a morphologic resemblance to the brown fat of hibernating mammals. Velsch 2, in 1670, described, first, a gland structure that he associated with the thymus; Barkow 2, only in 1846, called it “hibernating gland” and classified it apart from the thymus.
Brown tissue is brown-tan in colour and vascular, the cells are polygonal, multivacuolated, with granular cytoplasm and ovoid nucleus. Brown fat tissue is an important source of non-shivering thermogenesis; accordingly, this fat tissue is rich in blood supply and mitochondria that may increase in size and number. This tissue is present in several mammalian animals, it may also be present in non-hibernating animals, such as mice, rats, monkeys and humans.
In humans, the brown fat tissue observed is mostly in embryos and neonates, where it lies between vessels at the base of the neck or in the inter-scapular region, thigh, arm, axilla, retroperitoneum, mediastinum and perineum. After birth, it decreases, but small islands may persist in the white adipose tissue. Some Authors have suggested that brown tissue represents the early stage of the development of the white fat tissue, whilst others have suggested that brown and white adipose tissue are different types 1–3.
Usually, hibernoma is a benign, subcutaneous, freely movable, non tender mass, ovoid in shape. It may produce symptoms by pressure and displacement. Hibernoma is a well-capsulated neoplasm with intense microvasculature. Microscopically, all tumours are composed partly or principally of coarsely multivacuolated fat cells with small, central nuclei and no atypia. Four morphologic variants of hibernoma have been identified: typical, myxoid, spindle cell, and lipoma-like. “Typical” hibernoma, the most common (82.4%), includes eosinophilic cell, pale cell, and mixed cell types based on the tinctorial quality of the hibernoma cells. The myxoid variant (8.2%) contains a loose basophilic matrix. Spindle cell hibernoma (2.4%) presents features of spindle cell lipoma and hibernoma; all occurring in the neck or scalp. The lipoma-like variant (7%) contains only scattered hibernoma cells. Immunohistochemically, 85% of the tumours are positive for S-100 protein 4–8. A malignant hibernoma may exist, Enterline et al. described a so-called malignant hibernoma with areas resembling a typical hibernoma and areas like a well-differentiated liposarcoma 9.
Hibernomas occur, in adults, during the fourth decade of life, more rarely in childhood (youngest at 6 weeks old), no difference between sex has been observed. Tumour size ranges from 1 to 26 cm. Surgery is the standard treatment, and no cases of recurrence have been reported 10 11.
So far, to our knowledge, only 18 cases have been reported in the neck (Table I), one of which in the larynx, in the pre-epiglottic area. All presented as a cervical mass and surgical treatment was performed 12–15.
Table I. Location of head and neck hibernomas.
| Author(s)/Year (ref.) | Location |
| Lacomme/197310 | Neck |
| Lawson & Biller/197612 | Supraclavicular fossa |
| Simon/195020 | Neck |
| Cox/1954 6 | Neck, mediastinum |
| Vetner/196621 | Carotid sheath |
| Mesera & Batsakis/196722 | Retromandibular |
| Kristensen/198511 | Supraclavicular fossa |
| Abemayor et al./19872 | Supraclavicular fossa |
| Worsey et al./199423 | Neck |
| Hall et al./198819 | Suprahyoid region |
| Sellari Franceschini et al./199316 | Larynx (pre-epiglottic space) |
| Monerris Garcia et al./200315 | Neck |
| Florio et al./200024 | Neck |
| Carinci et al./200125 | Neck |
| Vinayak & Reddy/199313 | Parotid region |
| Minic/199214 | Submental space |
| Attar & Muzzafar/200626 | Submandibular region |
| Minni 2007 | Larynx (paraglottic space) |
Two theories have been proposed in order to explain the origin of hibernoma. According to one of these, the tumour grows starting from some islands of brown adipose tissue that may persist in the white fat tissue; on the contrary, tumoural brown fat cells may develop from white adipose tissue 1–5.
Brown adipose tissue has never been detected in the larynx; nevertheless white fat tissue is present in the pre-epiglottic and paraglottic space. Therefore, it may be possible to find hibernoma in both these laryngeal subsites 16–18. Bearing in mind this hypothesis, the hibernoma, hereby, reported, located in a vocal fold, may have developed from the white fat tissue of the paraglottic space 19, moreover, as a consequence, this case could be evidence of the development of hibernoma from white fat tissue.
References
- 1.Merkel H. Über ein Pseudolipon der Mamma. Beitr Path Anat Allge Path 1906;39:152-7. [Google Scholar]
- 2.Abemayor E, McLeod PH, Cobb CJ, Hashimoto CH. Hibernomas of the head and neck. Head Neck Surg 1987;9:362-7. [DOI] [PubMed] [Google Scholar]
- 3.Hatai S. On the presence in human embryos of an interscpular gland corresponding to the so-called hibernating gland of lower mammals. Anat Anz 1902;21:369-73. [Google Scholar]
- 4.Seemayer TA, Kannck J, Wang N, Ahmed MN. On the ultrastructure of hibernoma. Cancer 1975;36:1785-93. [DOI] [PubMed] [Google Scholar]
- 5.Dardick I. Hibernoma: a possible model of brown tissue fat histogenesis. Hum Pathol 1978;9:321-9. [DOI] [PubMed] [Google Scholar]
- 6.Cox RW. Hibernoma: the lipoma of immature adipose tissue. J Pathol Bact 1954;68:511-24. [DOI] [PubMed] [Google Scholar]
- 7.Hashimoto C, Cobb C. Cytodiagnosis of hibernoma. Diagn Cytopathol 1987;3:326-9. [DOI] [PubMed] [Google Scholar]
- 8.Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: a clinicopathologic study of 170 cases. Am J Surg Pathol 2001;25:809-14. [DOI] [PubMed] [Google Scholar]
- 9.Enterline HT, Lowry LD, Richman AV. Does malignant hibernoma exist? Am J Surg Pathol 1979;3:265-71. [DOI] [PubMed] [Google Scholar]
- 10.Lacomme Y. Hibernome cervical. Rev Laryngol Otol Rhinol 1973;94:66-70. [PubMed] [Google Scholar]
- 11.Kristensen S. Cervical hibernoma. Review of the literature and a new case. J Laryngol Otol 1985;99:1055-8. [DOI] [PubMed] [Google Scholar]
- 12.Lawson W, Biller HF. Cervical hibernoma. Laryngoscope 1976;86:1258-67. [DOI] [PubMed] [Google Scholar]
- 13.Vinayak BC, Reddy KT. Hibernoma in the parotid region. J Laryngol Otol 1993;107:257-8. [DOI] [PubMed] [Google Scholar]
- 14.Minic AJ. Hibernoma: unusual location in the submental space. J Craniomaxillofac 1992;20:264-5. [DOI] [PubMed] [Google Scholar]
- 15.Monerris Garcia E, Ronda Perez JM, Ortega Pastor E, Sancho Mestre M, Talavera Sanchez J. Hibernoma: a rare case of cervical mass. Acta Otorrinolaringol Esp 2003;54:143-6. [DOI] [PubMed] [Google Scholar]
- 16.Sellari Franceschini S, Segnini G, Berrettini S, Bruschini P, Cagno MC, Testi C. Hibernoma of the larynx. Review of the literature and a new case. Acta Otorhinolaryngol Belg 1993;47:51-3. [PubMed] [Google Scholar]
- 17.Reidenbach MM. The paraglottic space and transglottic cancer: anatomical considerations. Clin Anat 1996;9:244-51. [DOI] [PubMed] [Google Scholar]
- 18.Heaton JM. The distribution of brown adipose tissue in human. J Anat 1972;112:35-9. [PMC free article] [PubMed] [Google Scholar]
- 19.Hall RE, Koonig J, Hartmann L, Del Balso A. Hibernoma: an unusual tumor of adipose tissue. Oral Surg Oral Med Oral Pathol 1988;66:706-10. [DOI] [PubMed] [Google Scholar]
- 20.Simon HE. Posterior cervical tumor of brown fat in man; its relationship to the interscapular gland of hibernating animals. Am J Surg 1950;80:127-30. [DOI] [PubMed] [Google Scholar]
- 21.Vetner MO. Fetal fat cell lipoma (hibernoma). Nord Med 1966;76:1338-40. [PubMed] [Google Scholar]
- 22.Mesera BW, Batsakis J. Hibernomas of the neck. Arch Otolaryngol 1967;85:199-210. [DOI] [PubMed] [Google Scholar]
- 23.Worsey J, McGuirt W, Carrau RL, Peitzman AB. Hibernoma of the neck: a rare cause of neck mass. Am J Otolaryngol 1994;15:152-4. [DOI] [PubMed] [Google Scholar]
- 24.Florio G, Cicia S, Del Papa M, Carni D. Neck hibernoma: case report and literature review. G Chir 2000;21:339-41. [PubMed] [Google Scholar]
- 25.Carinci F, Carls FP, Pelucchi S, Grandi E, Hassanipour A, Pastore A. Hibernoma of the neck. J Craniofac Surg 2001;12:284-6. [DOI] [PubMed] [Google Scholar]
- 26.Attar ZB, Muzzafar S. An unusual case of benign hibernoma in the pediatric age group. J Coll Physicians Surg Pak 2006;16:237-8. [PubMed] [Google Scholar]