Abstract
Background: Food insecurity is associated with nutrient inadequacy and a variety of unfavorable health outcomes. However, little is known about whether food security is associated with lower cognitive function in the elderly.
Objective: We investigated the prevalence of food insecurity in a representative sample of 1358 Puerto Ricans aged 45–75 y living in Massachusetts in relation to cognitive function performances.
Design: Food security was assessed with the US Household Food Security Scale. Cognitive function was measured to capture general cognition with a battery of 7 tests: Mini-Mental State Examination (MMSE), word list learning (verbal memory), digit span (attention), clock drawing and figure copying (visual-spatial ability), and Stroop and verbal fluency tests (fluency executive functioning).
Results: The overall prevalence of food insecurity during the past 12 mo was 12.1%; 6.1% of the subjects reported very low food security. Food insecurity was inversely associated with global cognitive performance, as assessed by the MMSE score. The adjusted difference in the MMSE score was −0.90 (95% CI: −1.6, −0.19; P for trend = 0.003) for a comparison of participants with very low food security with those who were food secure, after adjustment for age, smoking, education, poverty status, income, acculturation, plasma homocysteine, alcohol, diabetes, and hypertension. Food insecurity was significantly associated with lower scores for word-list learning, percentage retention, letter fluency, and digit span backward tests.
Conclusions: Very low food security was prevalent among the study subjects and was associated with lower cognitive performance. Further studies, both observational and experimental, are warranted to clarify the direction of causality in this association.
INTRODUCTION
Food insecurity is defined as “limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways” (1). According to the latest national survey, 10.9% of US households experienced food insecurity in 2006 and, among them, 4% were in the category of “very low food security” (2). The prevalence of food insecurity was particularly high among low-income populations, ethnic minorities, and households with elders (2).
Hispanics are the largest minority group in the United States, accounting for 12.5% of the total population (US Census Bureau). We previously showed that Puerto Rican elders in Massachusetts had a significantly greater prevalence of depression, lower diet quality, and other chronic conditions than did a comparison group of non-Hispanic whites living in the same neighborhoods (3–9). However, to our knowledge, no studies have been conducted to examine the prevalence of food insecurity in this population of older Puerto Ricans living in the northeastern region of the country.
Food insecurity has been shown to be associated with nutrient inadequacy and a variety of unfavorable health outcomes, including obesity, anxiety, depression, and suicide (10–15). However, little is known about whether food security is associated with lower cognitive function among elders. Several studies, both animal and human, have shown that depression and anxiety contribute to cognitive impairment (16). Alternatively, if cognitive impairment leads to unfavorable labor market outcomes, lower incomes, or difficulty in acquiring food stamps or other social safety net services, the impairment could lead to food insecurity. Examining the relation between food insecurity and cognitive function could be particularly important for Hispanic elders, because this population is more likely to develop Alzheimer disease than are non-Hispanic whites (17, 18). To the extent that poor nutritional status contributes to cognitive decline, exploring these associations could provide a practical method for preventing cognitive impairment among low-income populations.
We therefore investigated the prevalence of food insecurity in a representative sample of Puerto Ricans aged 45–75 y living in areas around Boston, MA, and examined whether the prevalence of food insecurity was associated with lower cognitive function.
SUBJECTS AND METHODS
Subjects
Since 2004, we identified participants from areas of high Hispanic density in the Boston, MA, metropolitan and surrounding area, as indicated by the year 2000 Census. Blocks were selected at random for enumeration from the sampling frame, which consisted of all census blocks with ≥10 Hispanic persons aged ≥45 y. After door-to-door block enumeration, households with at least one Puerto Rican adult between the ages of 45 and 75 y were identified, and one person per household was selected randomly for participation. Most (80.4%) participants were identified in this way. An additional 8.9% were identified by random approach at major Puerto Rican events, such as the Boston Puerto Rican Festival, and the remainder in response to media (4.6%) or personal referral (6.1%). Only those participants who were unable to answer questions because of serious health conditions or who were not able to provide reliable information for other reasons, such as dementia or obvious alcoholism, were excluded from participation. We worked closely with the communities to inform them about the study, with the assistance of our collaborating community institution La Alianza Hispana. La Alianza Hispana has extensive contacts throughout the Puerto Rican community in Massachusetts.
In total, 2016 Puerto Rican adults were located and invited to participate; ≈86.2% (n = 1737) agreed to participate. After excluding those who had a Mini-Mental State Examination (MMSE) score ≤10 (n = 10) and those with temporary exclusions (n = 32) for reasons such as being currently busy or having upcoming vacations, there were 1695 eligible participants. Of these, 38 (2.2%) were lost to follow-up, 19 (1.1%) dropped out, and 251 (14.8%) did not participate after several scheduling attempts; 1387 (81.8% of those who were eligible) participants completed the baseline interview. Interviews were conducted in the home by bilingual interviewers in either Spanish or English, as preferred by the participant. Compared with those who completed the baseline interview, those who declined participation tended to be male (20.1% compared with 15.6%; P = 0.06) and lived on the US mainland, on average, for fewer years (32.1y ± 13.1 compared with 34.1 y ± 11.8; P = 0.07). The Institutional Review Board of Tufts University, New England Medical Center, approved the protocol. Participants gave written informed consent before participating.
Assessment of food security
Information on food security was assessed with the 10 household- and adult-referenced questions in the US Food Security Scale (Appendix A) (1). The food security questions referred to circumstances over the 12 mo preceding the survey. Participants with ≥3 affirmative answers to the 10 questions were considered “food insecure” (1). Food-insecure adults were further classified as having either low food security (if they had 3–5 affirmative answers) or very low food security (if they had ≥6 affirmative answers) (1, 2).
APPENDIX A.
Items on the food security scale
| Item | Affirmative answers |
| (I/We) worried whether (my/our) food would run out before (I/we) got money to buy more. | Frequently or sometimes |
| The food that (I/we) bought just didn't last, and (I/we) didn't have money to get more. | Frequently or sometimes |
| (I/we) couldn't afford to eat balanced meals. | Frequently or sometimes |
| In the past 12 mo, since last (name of current month), did (you/you or other adults in your household) ever cut the size of your meals or skip meals because there wasn't enough money for food? | Yes |
| If YES (above): How often did this happen? Almost every month, some months but not every month, or in only 1 or 2 mo? | Almost every month or some months |
| In the past 12 mo, did you ever eat less than you felt you should because there wasn't enough money to buy food? | Yes |
| In the past 12 mo, were you ever hungry but didn't eat because you couldn't afford enough food? | Yes |
| In the past 12 mo, did you lose weight because you didn't have enough money for food? | Yes |
| In the past 12 mo, did (you/you or other adults in your household) ever not eat for a whole day because there wasn't enough money or food? | Yes |
| If YES (above): How often did this happen? Almost every month, some months but not every month, or in only 1 or 2 mo? | Almost every month or some months |
Assessment of cognitive function
Participants were given a comprehensive battery of cognitive tests in their choice of either Spanish (98% of participants) or English. Seven cognitive tests were conducted. We used the MMSE (19) to assess general cognitive function with a range of scores from 0 to 30, with 30 as the best score. We used the 16-word list learning test (20) over the course of 5 trials to assess verbal memory and the digit span forward and backward test (20) to assess attention and working memory. We also administered the Stroop test (20), which involved naming a color rather than the text of words, and the verbal fluency test (20), in which we asked participants to name as many words as they could that start with a given letter; the clock drawing (21) and figure copying (22) tests were administered to assess executive function. Scores for the figure copying test were weighted for the complexity of the figure copied: 1 point for easy figures and 4 points for the most difficult.
All subjects underwent a detailed neuropsychological examination by a research assistant who had been trained in test administration and whose reliability has been established. Initial training and reliability were conducted in the standard manner recommended in the manuals for each of the individual tests being administered. Research assistants were trained by a neuropsychologist. To maintain a high degree of interrater reliability, the neuropsychologist observed (and co-scored, where appropriate) one subject for each research assistant every 6 mo. She also reviewed the data for quality control, and “spot checks” were made on scoring of tests and scales.
In the current analyses, the MMSE scores were considered the primary outcome because this test measures general cognition. In secondary analyses, we examined the association between food security and each individual cognitive assessment. Using principal component analysis methods, we further identified 3 cognitive function factors (executive function, memory, and attention factor; Appendix B), and examined whether food security was associated with these factors.
APPENDIX B.
Pearson's correlation coefficients for the relation between individual cognitive test scores and major cognitive function factors in a sample of Puerto Ricans living in Massachusetts1
| Individual test | Factor 1 (executive function) | Factor 2 (memory) | Factor 3 (attention) |
| Letter fluency | 0.49 | — | 0.42 |
| Figure copying | 0.60 | — | 0.30 |
| Digits forward | — | — | 0.78 |
| Digits backward | 0.29 | — | 0.70 |
| Clock drawing | 0.63 | — | — |
| Stroop 1 | 0.73 | — | — |
| Stroop 2 | 0.82 | — | — |
| Stroop 3 | 0.75 | — | — |
| Word list learning sum score | 0.27 | 0.78 | — |
| Recognition | — | 0.77 | — |
| Short-term recall facilitated | — | 0.87 | — |
| Long-term recall facilitated | — | 0.88 | — |
| Mini-Mental State Examination, attention | — | — | 0.48 |
Correlation coefficients <0.25 were omitted for simplicity.
Assessment of covariates
Body weight was measured with a Seca balance scale (Seca Corporation, Columbia, MD) with a capacity of 150 kg. Height was measured with a Harpenden pocket stadiometer (Holtain Ltd, Crosswell, United Kindom). Body mass index (BMI) was calculated as weight (kg)/height squared (m). We measured blood pressure at 3 time points during the home interview. Hypertension was defined as a mean systolic blood pressure ≥140 mm Hg and/or a mean diastolic blood pressure ≥90 mm Hg. Subjects were identified as having type 2 diabetes if they had a fasting plasma glucose concentration >7.0 mmol/L or reported the use of medications for diabetes (insulin or oral medicines) (23). Fasting (12 h) blood samples were drawn in the home by a certified phlebotomist on the day after the home interview or as soon as possible thereafter. Total homocysteine in plasma was measured by using an adaptation of the method described by Araki and Sako (24). The CV for this assay in our laboratory is 6.0%.
Information on age, years of education, household income, smoking, alcohol intake, and acculturation was collected with a questionnaire. Poverty status was computed by using the poverty guidelines released each year by the Department of Health and Human Services (http://aspe.hhs.gov/poverty/index.shtml). A subject's total annual household income was compared with the poverty guideline for the subject's family size and for the year of interview. If the total household income was less than this guideline, the subject was considered to be below the poverty line. An indicator of acculturation for Puerto Ricans was obtained from a set of 7 questions on the use of English and/or Spanish for speaking, reading, and listening while engaging in activities such as reading, watching television, and talking to friends and family members. We constructed a scale that ranged from 0% to 100%, with 100% indicating the use of only English for all activities and 0% indicating the use of only Spanish for all activities (25). We administered the Center for Epidemiologic Studies Depression Scale (CES-D) to measure symptoms of depression. The CES-D has been widely used in epidemiologic studies and has been shown to have good consistency and validity in older adults (26). It has also been used in Hispanics (27) and has been shown to have good reliability (28).
Statistical analyses
Statistical analyses were completed with SAS version 9.1 (SAS Institute Inc, Cary, NC). We examined whether individuals who reported food insecurity had lower cognitive performance than did those who reported that they were food secure. Subjects were divided into 3 categories on the basis of food security status, as described above. Means were compared by using the general linear models procedure in SAS, with Tukey's adjustment for multiple comparisons. In secondary analyses, we used multiple logistic regression models to estimate odds ratios (ORs) of cognitive impairment, defined as an MMSE score <24. Analyses were adjusted for age (y; as a continuous variable), sex, BMI (<25, 25–29.9, or ≥30), education (<5th grade, 5th–8th grade, 9th–12th grade, college, or graduate school), poverty (yes or no), smoking (current, former, or never), alcohol use (current, former, or never), presence of hypertension or diabetes (yes or no for each), plasma homocysteine concentration (μmol/L), and acculturation score. These potential confounders were either statistically associated with both food security and cognitive function, or had been suggested by previous studies to be relevant to the exposure and outcome.
We examined the interaction of food security with other important risk factors for cognitive impairment, including age (<60 y or ≥60 y), sex, current smoking status (yes or no), current alcohol use (yes or no), obesity (BMI < 30 or ≥ 30), and depression (yes or no, based on a cutoff score of 16 on the CES-D). To test significance for interaction, we included multiplicative terms in the regression models and adjusted for other potential confounders. We also conducted subgroup analyses to examine the associations between food security and the MMSE score after stratification by these 6 factors. To test whether our results were robust, we conducted 2 sensitivity analyses, excluding participants who did not use Spanish during the interview and those with type 2 diabetes.
RESULTS
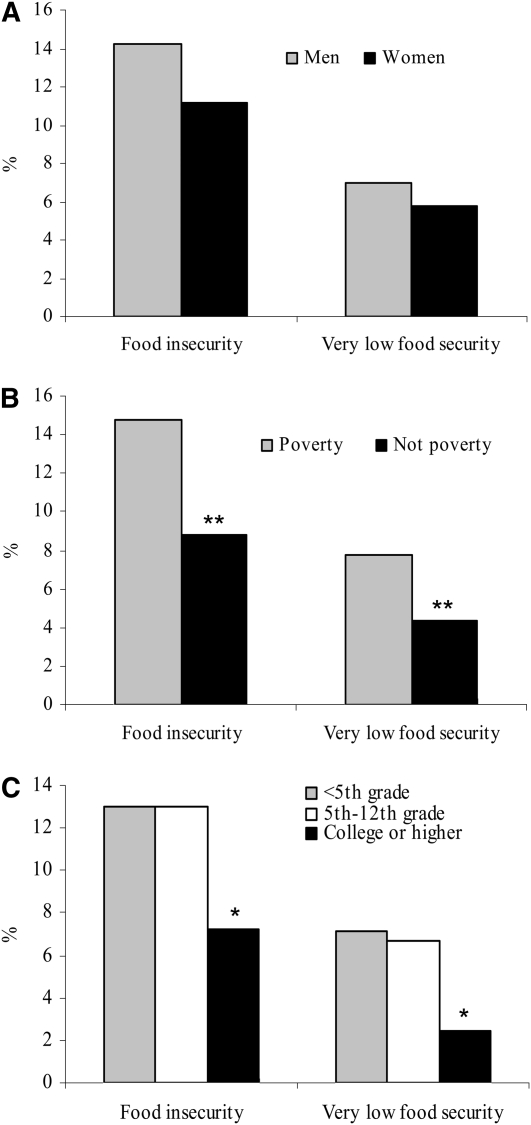
In this sample of 1358 Puerto Rican adults aged 45–75 y, 12.1% reported food insecurity during the past the 12 mo, and 6.1% reported very low food security. The prevalence of household food insecurity was not significantly different for men (14.2%) and women (11.2%) (P = 0.3), but was significantly greater among participants with annual household incomes below the US poverty line than in those with lower education levels (Figure 1). Participants who experienced very low food security were more likely to smoke and to have higher depression (CES-D) scores than were those who were food secure (Table 1). No clear relations were observed between food security status and other characteristics.
FIGURE 1.
Prevalence of food insecurity and very low food security in Puerto Rican adults according to sex (A), poverty (B), and education level (C). *P < 0.05 and **P < 0.01, adjusted for age and sex (men, poverty, and education <5th grade were used as references). Logistic regression was used to test differences in prevalence across categories.
TABLE 1.
Characteristics of participants according to food security status1
| Food insecure |
|||
| Food secure (n = 1194) | Low food security (n = 81) | Very low food security (n = 83) | |
| Age (y) | 57.8 ± 0.22 | 56.9 ± 0.8 | 56.7 ± 0.8 |
| Female (%) | 71.1 | 64.2 | 66.3 |
| BMI (kg/m2) | 31.9 ± 0.2 | 32.2 ± 0.7 | 30.2 ± 0.7 |
| Past smoker (%) | 30.4 | 31.3 | 15.93 |
| Current smoker (%) | 22.8 | 30.0 | 46.33 |
| Past drinker (%) | 30.1 | 32.1 | 31.3 |
| Current drinker (%) | 39.3 | 31.3 | 42.2 |
| Presence of diabetes (%) | 41.3 | 30.4 | 40.0 |
| Presence of hypertension (%) | 69.3 | 61.3 | 63.4 |
| Plasma homocysteine (μmol/L) | 8.5 ± 1.0 | 8.2 ± 1.0 | 8.3 ± 1.1 |
| CES-D score | 19.2 ± 0.4 | 26.4 ± 1.44 | 27.3 ± 1.44 |
| Acculturation score | 24.3 ± 0.6 | 22.0 ± 2.4 | 23.0 ± 2.3 |
CES-D, Center for Epidemiologic Studies Depression Scale. Means were compared by using the general linear model procedure in SAS (SAS Institute Inc, Cary, NC), with Tukey's adjustment for multiple comparisons.
Mean ± SE adjusted for age and sex (all such values).
Significantly different from food secure: 3P < 0.05, 4 P < 0.01.
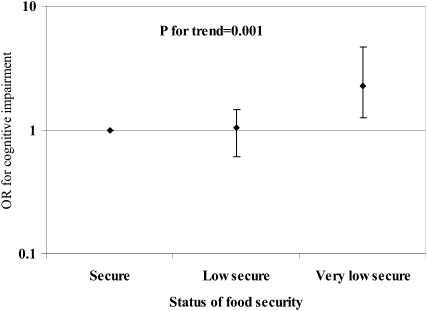
Food insecurity was inversely associated with global cognitive performance, as assessed by MMSE score (Table 2). The difference in MMSE scores was −0.90 (95% CI: −1.6, −0.19; P for trend = 0.003) for the comparison of participants with very low food security with those who were food secure, after adjustment for age, sex, BMI, education, poverty status, smoking, alcohol use, acculturation score, plasma homocysteine, and presence of hypertension or diabetes. The difference was equivalent to the difference observed between participants who were 8 y apart in age in this population. When we further adjusted for depression score, the difference was attenuated to −0.66, but the P for trend remained significant (P = 0.04). Very low food insecurity was also associated with a higher likelihood of having cognitive impairment, as evidenced by an MMSE score <24 (adjusted OR: 2.28; 95% CI: 1.26, 4.12; P for trend = 0.001; Figure 2).
TABLE 2.
Cognitive test performance according to food security status1
| Food insecure |
||||
| Food secure (n = 1194) | Low security (n = 81) | Very low security (n = 83) | P for trend | |
| MMSE | ||||
| Age- and sex-adjusted | 23.4 ± 0.10 | 23.2 ± 0.37 | 21.9 ± 0.372 | <0.0001 |
| Multivariate-adjusted | 23.4 ± 0.10 | 23.3 ± 0.34 | 22.5 ± 0.353 | 0.003 |
| Further adjusted for depression score | 23.4 ± 0.09 | 23.4 ± 0.35 | 22.7 ± 0.35 | 0.04 |
| Major cognitive function factors4 | ||||
| Executive function | −0.004 ± 0.03 | −0.10 ± 0.11 | −0.21 ± 0.11 | 0.003 |
| Memory | 0.03 ± 0.03 | 0.10 ± 0.12 | −0.08 ± 0.13 | 0.32 |
| Attention | −0.002 ± 0.03 | −0.21 ± 0.12 | 0.04 ± 0.13 | 0.81 |
Values are means ± SEs. MMSE, Mini-Mental State Examination. Means were compared by using the general linear model procedure in SAS (SAS Institute Inc, Cary, NC), with Tukey's adjustment for multiple comparisons.
Significantly different from food secure: 2P < 0.05, 3P < 0.001.
Adjusted for age (y), sex, BMI (in kg/m2; <25, 25–29.9, or ≥30), education (<5th grade, 5th–8th grade, 9th–12th grade, college, or graduate school), poverty (yes or no), acculturation score, smoking (never, past, or current), use of alcohol (never, past, or current), presence of diabetes and hypertension (each, yes or no), and plasma homocysteine (μmol/L).
FIGURE 2.
Multivariate-adjusted odds ratios (ORs) and 95% CIs for cognitive impairment according to status of food security. Cognitive impairment was defined as a Mini-Mental State Examination score <24. Logistic regression was used to calculate ORs, adjusted for age (y), sex, BMI (in kg/m2; <25, 25–29.9, or ≥30), education (<5th grade, 5th–8th grade, 9th–12th grade, college, or graduate school), poverty (yes or no), acculturation score, smoking (never, past, or current), use of alcohol (never, past, or current), presence of diabetes and hypertension (each, yes or no), and plasma homocysteine (μmol/L).
We also found a significant inverse association between food insecurity and the executive function factor (P for trend = 0.003), but there was no significant association with the memory or attention factors (P for trend > 0.3 for both; Table 2). When we further examined associations between food insecurity and individual cognitive tests, we found that participants with food insecurity had lower scores for word-list learning, percentage retention, letter fluency, and digit span backward (Table 3).
TABLE 3.
Individual cognitive test performance results according to food security status1
| Food insecure |
||||
| Food secure (n = 1194) | Low security (n = 81) | Very low security (n = 83) | P for trend | |
| Word list learning | 0.03 ± 0.03 | 0.03 ± 0.10 | −0.29 ± 0.112 | 0.02 |
| Recognition | 0.03 ± 0.03 | 0.10 ± 0.11 | −0.15 ± 0.11 | 0.55 |
| Percentage retention3 | 0.03 ± 0.03 | −0.08 ± 0.11 | −0.20 ± 0.11 | 0.01 |
| Stroop test | −0.0006 ± 0.03 | −0.02 ± 0.11 | −0.09 ± 0.11 | 0.24 |
| Letter fluency | 0.007 ± 0.03 | −0.06 ± 0.10 | −0.21 ± 0.11 | 0.03 |
| Digit span forward | 0.005 ± 0.03 | −0.10 ± 0.11 | 0.007 ± 0.11 | 0.72 |
| Digit span backward | 0.009 ± 0.03 | −0.14 ± 0.11 | −0.21 ± 0.11 | 0.006 |
| Clock drawing | 0.005 ± 0.03 | −0.23 ± 0.11 | −0.07 ± 0.10 | 0.07 |
| Figure copying | −0.01 ± 0.03 | 0.004 ± 0.10 | −0.08 ± 0.10 | 0.19 |
Values are means ± SEs and adjusted for age (y), sex, BMI (in kg/m2; <25, 25–29.9, or ≥30), education (<5th grade, 5th–8th grade, 9th–12th grade, college, or graduate school), poverty (yes or no), acculturation score, smoking (never, past, or current), use of alcohol (never, past, or current), presence of diabetes and hypertension (each, yes or no), and plasma homocysteine (μmol/L). z Scores are presented for standardizing purposes. Means were compared by using the general linear model procedure in SAS (SAS Institute Inc, Cary, NC), with Tukey's adjustment for multiple comparisons.
Significantly different from food secure, P < 0.05.
Calculated by dividing the number of words recalled after delay by the number of correct responses on the fifth learning trial.
We found a significant interaction between food security and age (<60 y or ≥60 y) in relation to MMSE score (P for interaction = 0.04). The association between food insecurity and MMSE score was stronger in older than in younger adults, but inverse trends were seen in both subgroups. The differences in MMSE scores between participants with very low security and those who were food secure were −1.75 (95% CI: −3.0, −0.5; P for trend = 0.0003) for older adults and −0.48 (95% CI: −1.33, 0.38; P for trend = 0.2) for younger adults. No significant interactions were observed between food security and sex, BMI, smoking status, alcohol use, or depression (P for interaction > 0.1 for all), and similar inverse associations were seen among each subgroup. When we included only participants who used Spanish or who did not have type 2 diabetes, we found similar significant associations between food insecurity and MMSE score (P for trend < 0.01 for both).
DISCUSSION
In a representative sample of Puerto Rican older adults living in Massachusetts, 12.1% reported food insecurity during the past 12 mo, and 6.1% were classified as having very low food security. The presence of food insecurity, especially of very low food security, was associated with lower cognition and a greater likelihood of cognitive impairment. These associations were independent of smoking, education, acculturation, plasma homocysteine, and other well-known risk factors for cognitive impairment. Strengths of the study include the use of a standard food security questionnaire and multiple measurements of cognitive function. Furthermore, similar strong associations between food insecurity and cognitive function were seen in sensitivity analyses, which suggests the robustness of our findings.
The prevalence of very low food security (6.1%) in this study was similar to the prevalence that has been reported among Hispanic households in the United States (5.7%) and was higher than the general prevalence reported among all households in the United States (4.0%) or among all households in Massachusetts (3%) (2). On the other hand, the prevalence of food insecurity in this study (12.1%) was lower than the prevalence among Hispanic households in the United States (19.5%), similar to the prevalence among all households in the United States (10.9%), and higher than the prevalence among all households in Massachusetts (8.1%) (2).
The mechanisms underlying the observed association between food insecurity and lower cognitive function are likely to be complex and involve multiple pathways. Food insecurity may lead to chronic stress and depression, which activates the hypothalamic-pituitary-adrenal axis and triggers the secretion of glucocorticoids in the adrenal gland. This is consistent with the observation that adjustment for depression score attenuated the association between food insecurity and cognitive performance. Glucocorticoids can cross the blood-brain barrier; bind to receptors in the hippocampus, amygdale, and frontal lobes; and, consequently, impair memory and executive function (16). A recent meta-analysis showed that depression was associated with worse performance on tests of executive function, episodic memory, processing speed, and semantic memory in elders (29). Animal studies have shown that chronic stress caused impairment of visual and spatial memory performance (30, 31).
Food insecurity could be associated with poor diet quality (32), which may influence cognitive function (33). However, in the multivariate models, we adjusted for plasma homocysteine, a biomarker of intake of B vitamins, and for the intake of fruit and vegetables (7), which did not attenuate the relation. There is a possibility that other aspects of nutritional inadequacy caused by food insecurity may have effects on cognition.
Alternatively, it is possible that participants with lower cognitive function have less favorable labor market outcomes and household incomes or are less likely to obtain food stamps or other food support. Previous studies reported that mental illness was strongly associated with impairment in vocational and social functioning and with less likelihood of employment and earnings (34–37).
The associations between food insecurity and cognitive function were stronger in older than in younger participants, possibly because aging increases the vulnerability of the brain. Older adults have smaller hippocampal volumes and, therefore, are more likely to have cognitive deficits when exposed to stress (16). Decreases in sex hormone concentrations, both estrogens and androgens, in elders could be another potential mediator. Men with lower concentrations of androgen have been shown to have a higher likelihood of becoming depressed (38, 39). Animal studies have also shown that castration increases hypothalamic-pituitary-adrenal activity (40). In women, estrogen has been shown to be protective against the deleterious effects of stress and depression on cognitive function (41). However, although the interaction between sex and food insecurity on cognitive function has biological explanations, chance or interactions with other factors remain plausible explanations.
Our study had several limitations. Because of the cross-sectional nature, the direction of causation cannot be inferred. However, biological plausibility suggests a possibility that food insecurity may contribute to impairment of cognitive function. Although we adjusted for several potential confounders, we cannot exclude the possibility of residual confounding due to unknown factors.
Further studies, both observational and experimental, are warranted to clarify the direction of causality between food insecurity and lower cognitive function. In either case, the association may have public policy implications. In Massachusetts, the Elder Nutrition Program uses reduced cognitive function as one of the eligibility criteria, allowing elders who are unable to attend congregate meals sites to receive home-delivered meals, regardless of income status (42). Concerning the federal Food Stamp Program, recently renamed the Supplemental Nutrition Assistance Program, low rates of participation among eligible immigrant populations and elder populations have been a concern for many years. In 2002, the US Department of Agriculture funded “Elderly Nutrition Demonstrations” in six states, which changed Food Stamp Program rules and practices at the county level to investigate three options for outreach to elders. An application assistance option was deemed to be more promising for serving elders with cognitive impairments, although with additional administrative costs (43).
In conclusion, we found a high prevalence of very low food security among Puerto Rican adults, which was strongly associated with lower cognitive performance. The difference in global cognitive scores between participants with very low food security and those with food security was equivalent to accelerating cognitive aging by ≈8 y. If food insecurity contributes to limitations in cognitive function through a biological mechanism, it provides another reason to recommend ensuring that this population has full access to nutrition program benefits (44). If cognitive function influences food security through economic mechanisms, then targeting food assistance benefits to the particularly high level of need in this population remains a significant issue.
Acknowledgments
The authors' responsibilities were as follows—XG, LMF, and KLT: study concept and design; TS, LMF, and KLT: acquisition of data; XG, TS, LMF, PEW, and KLT: analysis and interpretation of data; XG, PEW, and KLT: draft of the manuscript; XG, TS, LMF, PEW, and KLT: critical revision of the manuscript for important intellectual content; XG, TS, and PEW: statistical analysis; LMF and KLT: obtained funding; TS, PEW, and KLT: administrative, technical, or material support; and KLT: study supervision. No conflicts of interest were reported.
REFERENCES
- 1.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. Alexandria, VA: Food and Nutrition Service, USDA, 2000 [Google Scholar]
- 2.Nord M, Andrews M, Carlson S. Household food security in the United States, 2006. Washington, DC: Economic Research Service, USDA, 2007 [Google Scholar]
- 3.Tucker KL. Stress and nutrition in relation to excess development of chronic disease in Puerto Rican adults living in the Northeastern USA. J Med Invest 2005;52(suppl):252–8 [DOI] [PubMed] [Google Scholar]
- 4.Tucker KL, Bermudez O, Castaneda C. Type 2 diabetes is prevalent in poorly controlled among Hispanic elders of the Caribbean origin. Am J Public Health 2000;90:1288–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falcon LM, Tucker KL. Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. J Gerontol B Psychol Sci Soc Sci 2000;55:S108–16 [DOI] [PubMed] [Google Scholar]
- 6.Tucker KL, Falcon LM, Bianchi LA, Cacho E, Bermudez OI. Self-reported prevalence and health correlates of functional limitation among Massachusetts elderly Puerto Ricans, Dominicans, and non-Hispanic white neighborhood comparison group. J Gerontol A Biol Sci Med Sci 2000;55:M90–7 [DOI] [PubMed] [Google Scholar]
- 7.Gao X, Bermudez OI, Tucker KL. Plasma C-reactive protein and homocysteine concentrations are related to frequent fruit and vegetable intake in Hispanic and non-Hispanic white elders. J Nutr 2004;134:913–8 [DOI] [PubMed] [Google Scholar]
- 8.Gao X, Martin A, Lin H, Bermudez OI, Tucker KL. alpha-Tocopherol intake and plasma concentration of Hispanic and non-Hispanic white elders is associated with dietary intake pattern. J Nutr 2006;136:2574–9 [DOI] [PubMed] [Google Scholar]
- 9.Gao X, Nelson ME, Tucker KL. Television viewing is associated with prevalence of metabolic syndrome in Hispanic elders. Diabetes Care 2007;30:694–700 [DOI] [PubMed] [Google Scholar]
- 10.Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 2006;118:e859–68 [DOI] [PubMed] [Google Scholar]
- 11.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security, and child health status. Pediatrics 2004;113:298–304 [DOI] [PubMed] [Google Scholar]
- 12.Holben DH. Position of the American Dietetic Association: food insecurity and hunger in the United States. J Am Diet Assoc 2006;106:446–58 [DOI] [PubMed] [Google Scholar]
- 13.Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J Nutr 2008;138:604–12 [DOI] [PubMed] [Google Scholar]
- 14.Cook JT, Frank DA. Food security, poverty and human development in the United States. Ann N Y Acad Sci 2008;1136:193–209 [DOI] [PubMed] [Google Scholar]
- 15.Wilde PE, Peterman JN. Individual weight change is associated with household food security status. J Nutr 2006;136:1395–400 [DOI] [PubMed] [Google Scholar]
- 16.Lupien SJ, Maheu F, Tu M, Fiocco A, Schramek TE. The effects of stress and stress hormones on human cognition: Implications for the field of brain and cognition. Brain Cogn 2007;65:209–37 [DOI] [PubMed] [Google Scholar]
- 17.Tang M, Stern Y, Marder K, et al. The apoE-[epsilon]4 allele and the risk of Alzheimer's disease among African Americans, whites, and Hispanics. JAMA 1998;279:751–5 [DOI] [PubMed] [Google Scholar]
- 18.Tang MX, Maestre G, Tsai WY, et al. Relative risk of Alzheimer's disease and age-at-onset based on APOE genotypes among elderly African Americans, Caucasians and Hispanics in New York City. Am J Hum Genet 1996;58:574–84 [PMC free article] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98 [DOI] [PubMed] [Google Scholar]
- 20.Artiola i Fortuny L, Hermosillo D, Heaton RK, Pardee RE., III Manual de normas y procedimientos para la batería Neuropsicológica en Español. [Manual of norms and procedures for a neuropsychological battery in Spanish.] Tucson, AZ: m Press, 1999(in Spanish) [Google Scholar]
- 21.Wolf-Klein GP, Silverstone F, Levy A, Brod M. Screening for Alzheimer's disease by clock drawing. J Am Geriatr Soc 1989;37:730–4 [DOI] [PubMed] [Google Scholar]
- 22.Beery K. The Developmental Test of Visual-Motor Integration manual, revised ed. Cleveland, OH: Modern Curriculum Press, 1989 [Google Scholar]
- 23.American Diabetes Association Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003;26(suppl 1):S5–20 [DOI] [PubMed] [Google Scholar]
- 24.Araki A, Sako Y. Determination of free and total homocysteine in human plasma by high-performance liquid chromatography with fluorescence detection. J Chromatogr 1987;422:43–52 [DOI] [PubMed] [Google Scholar]
- 25.Cuellar I, Harris L, Jasso R. An acculturation scale for Mexican American normal and clinical populations. Hisp J Behav Sci 1980;2:199–217 [Google Scholar]
- 26.Radloff LS, Teri L. Use of the Center for Epidemiological Studies–Depression Scale with older adults. Clin Gerontol 1986;5:119–36 [Google Scholar]
- 27.Moscicki EK, Locke BZ, Rae DS, Boyd JH. Depressive symptoms among Mexican Americans: the Hispanic Health and Nutrition Examination Survey. Am J Epidemiol 1989;130:348–60 [DOI] [PubMed] [Google Scholar]
- 28.Lobell DB, Burke MB, Tebaldi C, Mastrandrea MD, Falcon WP, Naylor RL. Prioritizing climate change adaptation needs for food security in 2030. Science 2008;319:607–10 [DOI] [PubMed] [Google Scholar]
- 29.Herrmann W, Hubner U, Koch I, Obeid R, Retzke U, Geisel J. Alteration of homocysteine catabolism in pre-eclampsia, HELLP syndrome and placental insufficiency. Clin Chem Lab Med 2004;42:1109–16 [DOI] [PubMed] [Google Scholar]
- 30.Mizoguchi H, Yamada K, Mizuno M, et al. Regulations of methamphetamine reward by extracellular signal-regulated kinase 1/2/ETS-like gene-1 signaling pathway via the activation of dopamine receptors. Mol Pharmacol 2004;65:1293–301 [DOI] [PubMed] [Google Scholar]
- 31.Orsetti M, Colella L, Dellarole A, Canonico PL, Ghi P. Modification of spatial recognition memory and object discrimination after chronic administration of haloperidol, amitriptyline, sodium valproate or olanzapine in normal and anhedonic rats. Int J Neuropsychopharmacol 2007;10:345–57 [DOI] [PubMed] [Google Scholar]
- 32.Casey PH, Simpson PM, Gossett JM, et al. The association of child and household food insecurity with childhood overweight status. Pediatrics 2006;118:e1406–13 [DOI] [PubMed] [Google Scholar]
- 33.Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer's disease. Ann Neurol 2006;59:912–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marcotte DE, Wilcox-Gok V. Estimating earnings losses due to mental illness: a quantile regression approach. J Ment Health Policy Econ 2003;6:123–34 [PubMed] [Google Scholar]
- 35.Marcotte DE, Wilcox-Gok V. Estimating the employment and earnings costs of mental illness: recent developments in the United States. Soc Sci Med 2001;53:21–7 [DOI] [PubMed] [Google Scholar]
- 36.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 2000;26:119–36 [DOI] [PubMed] [Google Scholar]
- 37.Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989;262:914–9 [PubMed] [Google Scholar]
- 38.Seidman SN. Androgens and the aging male. Psychopharmacol Bull 2007;40:205–18 [PubMed] [Google Scholar]
- 39.Seidman SN, Araujo AB, Roose SP, McKinlay JB. Testosterone level, androgen receptor polymorphism, and depressive symptoms in middle-aged men. Biol Psychiatry 2001;50:371–6 [DOI] [PubMed] [Google Scholar]
- 40.Handa RJ, Nunley KM, Lorens SA, Louie JP, McGivern RF, Bollnow MR. Androgen regulation of adrenocorticotropin and corticosterone secretion in the male rat following novelty and foot shock stressors. Physiol Behav 1994;55:117–24 [DOI] [PubMed] [Google Scholar]
- 41.Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology 2006;31:151–78 [DOI] [PubMed] [Google Scholar]
- 42.The Executive Office of Elder Affairs. Available from: http://www.mass.gov/?pageID=eldersterminal&L=2&L0=Home&L1=Meals+and+Nutrition&sid=Eelders&b=terminalcontent&f=nutrition_homemeals&csid=Eelders (cited 29 October 2008.
- 43.Cody S, Ohls J. Evaluation of the USDA Elderly Nutrition Demonstrations. Vol 1. Evaluation findings. 2005. Available from: http://www.ers.usda.gov/Publications/CCR9-1/ccr9-1.pdf (cited 29 October 2008)
- 44.Borjas GJ. Food insecurity and public assistance. J Public Econ 2004;88:1421–43 [Google Scholar]