Abstract
Background: Estimates of excess mortality associated with body mass index (BMI; in kg/m2) have been calculated for the US population.
Objective: The objective of this article is to compare the excess mortality associated with BMI levels to the excess mortality associated with other anthropometric variables.
Design: For the 1988–1994 Third National Health and Nutrition Examination Survey, estimates of excess deaths were calculated for standard BMI levels and for comparable levels of percentage body fat, waist circumference, hip and arm circumferences, waist-hip ratio, the sum of 4 skinfold thicknesses, and waist-stature ratio. The outcome measure is the percentage of deaths in the full sample in excess of those predicted for the reference category.
Results: For the level equivalent to BMI <18.5, estimates of excess deaths ranged from 0.3% for waist-hip ratio to 2.4% for percentage body fat. All except waist circumference, waist-hip ratio, and waist-stature ratio were significantly greater than zero (P < 0.05). For the level equivalent to BMI 25 to <30, the percentage of excess deaths was 0.1% for percentage body fat and negative for all other variables; estimates were significantly below zero only for circumferences and waist-stature ratio. For the level equivalent to BMI ≥30, estimates ranged from −1.7% for waist circumference to 1.5% for percentage of fat; none were significantly different from zero. Estimates for all-cause mortality, obesity-related causes of death, and other causes of death showed no statistically significant or systematic differences between BMI and other variables.
Conclusion: In this population-based study, attributable fractions of deaths were similar across measures.
See corresponding editorial on page 1003.
INTRODUCTION
Body mass index [BMI; weight (kg)/height (m)2] is a measure of weight adjusted for height. Because weight and height are relatively easy to measure and because BMI is relatively highly correlated with body fat, BMI is often used in epidemiologic studies to assess adiposity. However, it is an imperfect measure because it does not assess body fatness directly (1). Another anthropometric indicator sometimes suggested to be used instead of BMI is waist circumference, which may be more closely related to adiposity, particularly visceral adiposity, than is BMI and thus may be a better indicator of the risk associated with adiposity (2). Another approach to measuring adiposity is the use of skinfold thicknesses (2, 3). Bioelectrical impedance can also provide estimates of body fatness (4). Combinations of different variables such as the ratio of waist circumference to hip circumference can also be used (5).
The Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994) provides a set of standardized measurements of body size and composition in a representative sample of the US population, including BMI, percentage of fat from bioelectrical impedance, skinfold thicknesses, and circumference measurements of waist, hip, and arm. Mortality follow-up data make it possible to assess the extent to which various anthropometric measures can predict mortality risk. These data have been used to estimate the excess deaths associated with different BMI categories (6, 7).
The objective of this study was to compare estimates of excess deaths associated with BMI categories with estimates of excess deaths associated with other possible indicators of body size or composition in a large nationally representative study.
SUBJECTS AND METHODS
NHANES III was conducted from 1988 to 1994 by the National Center for Health Statistics of the Centers for Disease Control and Prevention. A nationally representative cross-sectional sample of the US civilian noninstitutionalized population was selected using a complex, stratified, multistage probability cluster sampling design. A description of the plan and operation of the survey has been published (8). NHANES III underwent institutional review board approval and included written informed consent.
Waist circumference, hip circumference, arm circumference, skinfold-thickness measurements, bioelectrical impedance, weight, and height were measured using standardized techniques and equipment (8). Waist circumference measurements were made just above the iliac crest. Hip circumference measurements were made at the largest protuberance of the buttocks. Arm circumference was measured at the midpoint of the arm and BMI was calculated. Percentage body fat was calculated from resistance and reactance measurements using previously published formulas (9, 10). Waist-hip ratio (WHR) was calculated as waist circumference (cm)/hip circumference (m). Skinfold-thickness measurements were made at 4 sites (triceps, subscapula, suprailium, and thigh) and summed together. For the purposes of this study, skinfold values that were above the maximum of 55 mm that could be measured with the calipers used were arbitrarily assigned a higher value of 60 mm. Waist-stature ratio (WSR) was calculated as waist circumference (cm)/height (m).
For mortality data we used the NHANES III Linked Mortality File from the National Center for Health Statistics (11). The National Center for Health Statistics has conducted a mortality linkage of NHANES III to death certificate data found in the National Death Index. The NHANES III Linked Mortality File provides mortality follow-up data from the date of NHANES III survey participation (1988–1994) through 31 December 2000. Linkage of the NHANES III survey participants with the National Death Index provides the opportunity to conduct studies designed to investigate the association of a wide variety of health factors with mortality.
To estimate relative risks, we used baseline data from NHANES III (1988–1994) and mortality data from the NHANES III Linked Mortality File through 2000. Baseline age was age at the time of the examination. We calculated relative risks of mortality using Cox proportional hazard models with age as the time scale (12). We fit models separately in 4 age–sex strata for men and women aged 25–<70 and 70+ y. The model included levels of the specified anthropometric variable (low, reference, intermediate, or high), smoking status (never, former, or current), race (white, black, or other), and alcohol consumption categories in ounces per day (none, <0.07, 0.07–<0.35, or ≥0.35).
The sample of respondents aged ≥25 y examined in the mobile examination center in NHANES III included 6920 men and 7627 nonpregnant women with complete BMI data and mortality follow-up data. Of these, 327 men and 414 women had missing values for waist circumference and an additional 364 men and 523 women had missing values for resistance from the bioelectrical impedance measures. The final analytic sample included 12,919 men and nonpregnant women who had complete data for BMI and other anthropometric variables. However, for statistical pairwise comparisons of variables, all available data for the 2 variables being compared were used.
Categorical estimates
For categorical analyses, we grouped BMI as follows: <18.5 (underweight), 18.5–<25 (reference category), 25–<30 (overweight), and ≥30 (obesity). These followed federal guidelines (13).
When comparing the results from levels of BMI values with levels of other anthropometric variables, differences might be introduced simply because the categories reflect different points in the distribution. To control for this effect, researchers not infrequently divide all variables into quintiles or other comparable categories of equal size for all variables (14–23). We followed a similar procedure, except that, instead of quintiles, we used the standard BMI cutoffs to form categories and then created levels for the other anthropometric variables that were prevalence matched to the standard BMI cutoffs. In other words, these categories were created by using cutoffs that would identify the same proportion of the population as did the standard BMI cutoffs. For purposes of analysis, these levels are termed low (corresponding to BMI <18.5), reference (corresponding to BMI 18.5–<25), intermediate (corresponding to BMI 25–<30), and high (corresponding to BMI ≥30).
Estimation of excess deaths
We calculated the number of excess deaths associated with different levels of each anthropometric variable individually (including BMI itself) by using similar methods to those described previously (6, 24). Because many indicators, such as percentage body fat or waist circumference, display marked differences by sex, we allowed relative risks to vary by sex and age. We calculated excess deaths within each sex–age group and summed them over the whole sample. This approach has the advantage of providing a metric that can be summed over age and sex groups to obtain a sample total while still allowing for variation in relative risks by sex and age. It uses sex- and age-specific information on the prevalence of the given anthropometric level and mortality, combined with relative risk information, to estimate the sample burden of mortality associated with the given anthropometric level, which cannot be assessed from relative risk estimates alone. For these analyses, unlike our previous work (6, 7) we did not extrapolate the results to national mortality data. The estimates presented here are for the (weighted) NHANES III sample. In part because of the high correlations among anthropometric variables, this methodology is not suited to making excess death calculations for ≥2 variables simultaneously.
We express the excess deaths as a percentage of total sample deaths. Although this methodology is a form of attributable fraction methodology, this is a measure of association and does not necessarily indicate a causal relation. Within each level of a given anthropometric variable, we divided the number of excess deaths by the total number of deaths in the sample to create an estimate of population attributable fraction for each anthropometric level. For a given anthropometric level, this can be interpreted as the percentage of total deaths in the sample that are in excess of (or fewer than) those that would be predicted if people in that anthropometric level instead had been in the reference level for that variable, with the other covariates of age group, sex, race or ethnic group, smoking, and alcohol consumption all held constant.
All analyses were conducted using the SAS System for Windows (release 9.1; SAS Institute, Cary, NC) and Research Triangle Institute's SUDAAN (release 9.0; Research Triangle Institute, Research Triangle Park, NC) software programs. All analyses included sample weights that account for the varying probabilities of selection due to sampling and nonresponse. Standard errors were calculated by applying a delta method for complex sample designs that takes into account uncertainties in the relative risks for the levels of an anthropometric variable, the distribution of the anthropometric variable in the sample, the distribution of covariates, and the estimated effects of covariates, as well as the added variability due to the complex sample design of the NHANES surveys (24, 25). Statistical testing of the difference between excess deaths associated with levels of one anthropometric variable and excess deaths associated with the corresponding levels of another anthropometric variable were determined by t tests in which the denominator of the test statistic was the SE of the difference obtained from the delta method. These t tests used 49 df, which is equal to the number of primary sample units minus the number of sample strata. To partially account for multiple comparisons, statistical significance was set at the P < 0.0024 level to test the 21 pairwise differences within a given level of the anthropometric variables without additionally adjusting for the 4 levels, which would have led to a smaller P value.
RESULTS
Basic descriptive information about the sample is shown in Table 1. Correlation coefficients for the different variables with each other and with height are shown in Table 2. Most of the variables were highly correlated with each other.
TABLE 1.
Descriptive information about the analytic sample
| Men | Women | |
| Unweighted sample size | 5833 | 6107 |
| Weighted percentage | 48.9 | 51.1 |
| Deaths (n)1 | 1064 | 789 |
| Mean age (y) | 46.3 (0.4) 2 | 48.7 (0.6)3 |
| Height (cm) | 175.6 (0.2) | 161.8 (0.2)3 |
| Weight (kg) | 81.7 (0.3) | 68.6 (0.5)3 |
| Mean BMI (kg/m2) | 26.4 (0.1) | 26.2 (0.2) |
| Mean fat (%) | 21.1 (0.2) | 31.4 (0.3)3 |
| Mean waist circumference (cm) | 95.6 (0.2) | 88.5 (0.4)3 |
| Mean hip circumference (cm) | 99.3 (0.1) | 101.8 (0.3)3 |
| Mean arm circumference (cm) | 32.9 (0.1) | 30.6 (0.1)3 |
| Mean waist-hip ratio (cm/m) | 96.0 (0.2) | 86.7 (0.2)3 |
| Sum of 4 skinfolds (mm) | 70.4 (0.6) | 101.4 (1.2)3 |
| Mean waist-stature ratio (cm/m) | 54.4 (0.1) | 54.8 (0.3) |
Mortality data are from the Third National Health and Nutrition Examination Survey Linked Mortality File (11).
SE in parentheses (all such values).
Mean value for women is significantly different from mean value for men (P < 0.001) on the basis of a 2-sample t test for complex sample survey data (25).
TABLE 2.
Correlations between measurements by sex1
| BMI | Percentage of fat | Waist circumference | Hip circumference | Arm circumference | WHR | Sum of 4 skinfolds | WSR | Height | |
| Men | |||||||||
| BMI | 1.00 | 0.712 | 0.892 | 0.872 | 0.852 | 0.532 | 0.802 | 0.882 | 0.062 |
| Percentage of fat | 1.00 | 0.742 | 0.662 | 0.552 | 0.542 | 0.702 | 0.762 | −0.01 | |
| Waist circumference | 1.00 | 0.852 | 0.722 | 0.762 | 0.772 | 0.942 | 0.202 | ||
| Hip circumference | 1.00 | 0.802 | 0.312 | 0.782 | 0.732 | 0.382 | |||
| Arm circumference | 1.00 | 0.332 | 0.712 | 0.632 | 0.282 | ||||
| WHR | 1.00 | 0.432 | 0.812 | −0.092 | |||||
| Sum of 4 skinfolds | 1.00 | 0.732 | 0.142 | ||||||
| WSR | 1.00 | −0.132 | |||||||
| Height | 1.00 | ||||||||
| Women | |||||||||
| BMI | 1.00 | 0.872 | 0.882 | 0.912 | 0.912 | 0.392 | 0.862 | 0.882 | −0.082 |
| Percentage of fat | 1.00 | 0.832 | 0.832 | 0.822 | 0.432 | 0.832 | 0.822 | −0.052 | |
| Waist circumference | 1.00 | 0.822 | 0.832 | 0.702 | 0.782 | 0.972 | 0.02 | ||
| Hip circumference | 1.00 | 0.852 | 0.182 | 0.832 | 0.762 | 0.162 | |||
| Arm circumference | 1.00 | 0.372 | 0.862 | 0.792 | 0.052 | ||||
| WHR | 1.00 | 0.312 | 0.722 | −0.162 | |||||
| Sum of 4 skinfolds | 1.00 | 0.752 | 0.01 | ||||||
| WSR | 1.00 | −0.232 | |||||||
| Height | 1.00 |
WHR, waist-hip ratio; WSR, waist-stature ratio.
Significantly different from zero.
Cutoffs for categorization of anthropometric variables
The percentile values for waist circumference and other variables that correspond, in the sense of identifying the same proportion of the distribution, to the specified BMI cutoffs are shown in Table 3. Because of rounding, the values are not always exactly the identical percentile, but they are close. For example, for women, a percentage fat value of <16.0% or a waist circumference value of <67.1 cm produces prevalence estimates similar to a BMI <18.5 (see Table 3). In this sample, 3.29% of women had BMI values <18.5, 3.31% had percentage fat values <16.0%, and 3.22% had waist circumference values <67.1 cm.
TABLE 3.
Cutoffs for anthropometric variables that correspond to BMI categories
| BMI category (in kg/m2) |
||||
| Low | Reference | Intermediate | High | |
| (<18.5) | (18.5 to <25) | (25 to <30) | (≥30) | |
| Men | ||||
| Fat (%) | <6.0 | 6.0 to <19.9 | 19.9 to <26.5 | ≥26.5 |
| Waist circumference (cm) | <72.0 | 72.0 to <92.0 | 92.0 to <106.1 | ≥106.1 |
| Hip circumference (cm) | <82.8 | 82.8 to <96.7 | 96.7 to <105.9 | ≥105.9 |
| Arm circumference (cm) | <24.7 | 24.7 to <32.0 | 32.0 to <36.1 | ≥36.1 |
| Waist-hip ratio (cm/m) | <81.6 | 81.6 to <94.0 | 94.0 to <102.1 | ≥102.1 |
| Sum of 4 skinfolds (mm) | <21.9 | 21.9 to <60.2 | 60.2 to <90.1 | ≥90.1 |
| Waist-stature ratio (cm/m) | <40.7 | 40.7 to <52.4 | 52.4 to <60.5 | ≥60.5 |
| Women | ||||
| Fat (%) | <16.0 | 16.0 to <31.9 | 31.9 to <37.9 | ≥37.9 |
| Waist circumference (cm) | <67.1 | 67.1 to <86.5 | 86.5 to <99.1 | ≥99.1 |
| Hip circumference (cm) | <85.4 | 85.4 to <99.8 | 99.8 to <108.5 | ≥108.5 |
| Arm circumference (cm) | <23.6 | 23.6 to <30.0 | 30.0 to <33.7 | ≥33.7 |
| Waist-hip ratio (cm/m) | <73.6 | 73.6 to <85.9 | 85.9 to <92.5 | ≥92.5 |
| Sum of 4 skinfolds (mm) | <42.0 | 42.0 to <93.3 | 93.3 to <125.1 | ≥125.1 |
| Waist-stature ratio (cm/m) | <41.5 | 41.5 to <53.6 | 53.6 to <61.5 | ≥61.5 |
Although the prevalence is the same, an individual might fall into one BMI category and not into the matched category of the other variable. For example, of men in the BMI category of 18.5–<25, 69% fell into the corresponding percentage fat category of 6.0–<19.9, 2% fell into a lower percentage fat category, and 29% fell into a higher percentage fat category. The overall proportion of people who fall into the corresponding categories of each pair of the other anthropometric variables is shown in Table 4. In most cases, from 50% to 75% of people were classified similarly across variables. However, for WHR the percentage of agreement tended to be lower.
TABLE 4.
Percentage agreement between categories formed using cutoffs in Table 3
| BMI | Percentage of fat | Waist circumference | Hip circumference | Arm circumference | Waist-hip ratio | Sum of 4 skinfolds | Waist-stature ratio | |
| Men | ||||||||
| BMI | 100.0 | 60.0 | 72.0 | 69.2 | 69.2 | 50.3 | 64.0 | 72.0 |
| Percentage of fat | 100.0 | 61.5 | 55.5 | 49.9 | 50.9 | 60.0 | 61.1 | |
| Waist circumference | 100.0 | 67.2 | 57.9 | 63.2 | 62.5 | 79.7 | ||
| Hip circumference | 100.0 | 63.7 | 43.3 | 63.0 | 57.4 | |||
| Arm circumference | 100.0 | 43.5 | 59.2 | 53.1 | ||||
| Waist-hip ratio | 100.0 | 48.7 | 67.3 | |||||
| Sum of 4 skinfolds | 100.0 | 58.5 | ||||||
| Waist-stature ratio | 100 | |||||||
| Women | ||||||||
| BMI | 100.0 | 72.5 | 67.3 | 69.9 | 73.4 | 41.9 | 66.6 | 67.6 |
| Percentage of fat | 100.0 | 63.1 | 67.0 | 62.9 | 42.1 | 64.1 | 61.8 | |
| Waist circumference | 100.0 | 60.8 | 60.7 | 53.9 | 56.9 | 79.9 | ||
| Hip circumference | 100.0 | 64.0 | 37.1 | 63.3 | 55.0 | |||
| Arm circumference | 100.0 | 42.1 | 65.6 | 58.3 | ||||
| Waist-hip ratio | 100.0 | 40.0 | 55.2 | |||||
| Sum of 4 skinfolds | 100.0 | 55.4 | ||||||
| Waist-stature ratio | 100 |
Excess deaths
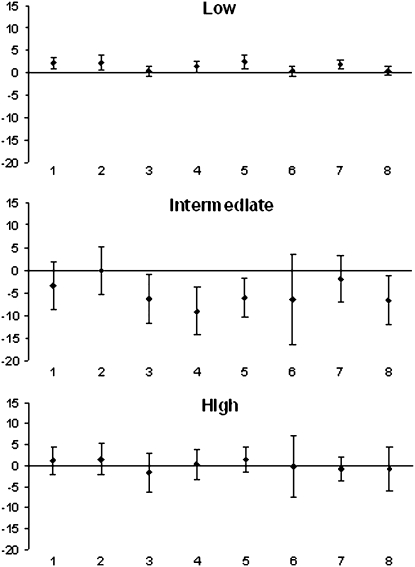
Attributable fractions for excess deaths were calculated for levels of BMI and for the corresponding levels of other variables formed from the cutoffs shown in Table 3. The estimated attributable fractions of all-cause mortality, relative to the reference category, for low, intermediate, and high categories of each variable, with 95% CIs, are shown in Figure 1. The attributable fractions were generally similar for the low level of all variables. All were small and positive, ranging from 0.3% (95% CI: −0.8, 1.4) for WHR to 2.5% (95% CI: 1.1, 3.9) for arm circumference. The 95% CI included zero only for waist circumference, WHR, and WSR. The fractions suggest that anywhere from 0.3% to 2.5% more deaths occurred in the sample than would have been expected if the individuals at the low level had been in the reference level instead.
FIGURE 1.
Estimated attributable fractions and 95% CIs for all-cause mortality for different anthropometric and body composition variables. 1, BMI; 2, percentage of fat; 3, waist circumference; 4, hip circumference; 5, arm circumference; 6, waist-hip ratio; 7, sum of skinfolds; and 8, waist-stature ratio.
For the intermediate level, relative to the reference level, the only positive association was for percentage body fat, at 0.1% (95% CI: −5.2, 5.4). For all other variables, the association was negative, ranging from −1.8% (95% CI: −7.0, 3.3) for the sum of skinfolds to −9% (95% CI: −14.2, −3.8) for hip circumference. For circumference measures of waist, hip, and arm and for WSR, the estimates were significantly below zero, but this was not the case for the other measures. These estimates suggest that anywhere from +0.1% to −7% fewer deaths occurred in the sample than would have been expected if the individuals at the intermediate level instead had been in the reference level. Attributable fraction estimates for the high level, relative to the reference level, ranged from weakly negative [−1.7% (95% CI: −6.4, 2.9) for waist circumference] to weakly positive [1.5% (95% CI: −2.2, 5.1) for percentage fat]. All CIs included zero. Pairwise statistical tests comparing estimates of excess deaths based on different variables with each other showed no significant differences between estimates of excess deaths for any pair of variables at any level based on a P value <0.0012 for the 28 pairwise comparisons at each level; for the obese level, only 1 of the 21 differences would have been significant at a P value of 0.05.
Excess deaths in a higher-risk group
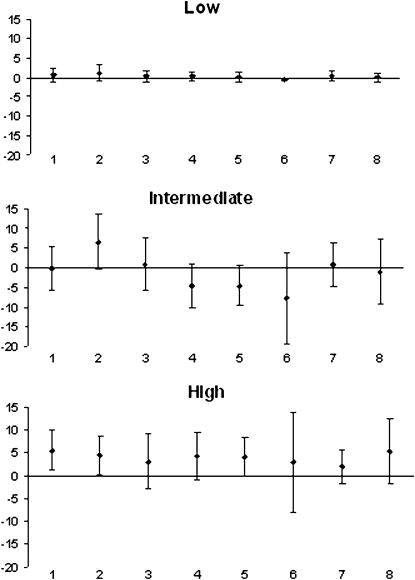
To try to isolate a higher-risk group that might show more clearly any differences between anthropometric measures and create an outcome variable more strongly associated with adiposity, we calculated attributable fractions for deaths from a group of conditions that included cardiovascular disease, obesity-related cancers (colon cancer, breast cancer, esophageal cancer, uterine cancer, ovarian cancer, kidney cancer, or pancreatic cancer) and diabetes or kidney disease, which are all conditions shown previously to be associated with excess mortality among the obese (7, 17). The results for deaths from these causes are shown in Figure 2. The attributable fractions for these selected conditions associated with the low level, relative to the reference level, were all quite small and close to zero; only the estimate for WHR differed significantly from zero (−0.5%, 95% CI: −0.8, −0.1).
FIGURE 2.
Estimated attributable fractions and 95% CIs for mortality from cardiovascular disease, diabetes, or obesity-related cancers for different anthropometric and body composition variables. 1, BMI; 2, percentage of fat; 3, waist circumference; 4, hip circumference; 5, arm circumference; 6, waist-hip ratio; 7, sum of skinfolds; and 8, waist-stature ratio.
For the intermediate level, BMI, waist circumference, and the sum of skinfold thicknesses were nonsignificantly associated with <1% of either excess or decreased mortality from these selected conditions. Percentage of fat showed a nonsignificantly increased mortality of 6.5% (95% CI: −0.4, 13.5) and the other variables showed a nonsignificantly decreased mortality with the largest negative effect (−7.8%, 95% CI: −19.4, 3.8) shown for WHR. All CIs included zero.
For the high level, the highest estimates were for BMI (5.5%, 95% CI: 1.1, 9.9) and percentage of fat (4.4%; 95% CI: 0.2, 8.6). For all other variables, estimates were also positive and 95% CIs included zero. Despite some apparent differences, pairwise statistical tests comparing estimates of excess deaths on the basis of different variables with each other showed no significant differences between estimates of excess deaths for any pair of variables at any level, based on a P value <0.0012 for the 28 pairwise comparisons at each level; for the obese level, none of the 21 differences would have been significant even at a P value of 0.05.
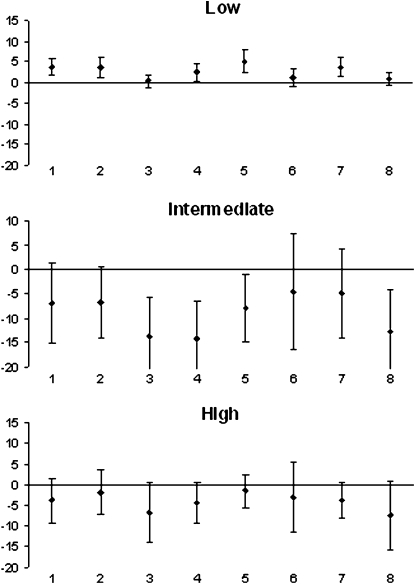
Excess deaths for remaining causes of death
We also examined attributable fractions for the remaining causes of death (all causes except cardiovascular disease, diabetes, and obesity-related cancers) grouped together, with results as shown in Figure 3. Relative to the reference level, the low level tended to be associated with increased mortality from these causes and the intermediate and high levels with decreased mortality from these causes for all variables. Pairwise statistical tests comparing estimates of excess deaths based on different variables with each other were based on a P value <0.0012 for the 28 pairwise comparisons at each level. The only significant difference at any level was between waist circumference and arm circumference at the low level. For the obese level, none of the 21 differences would have been significant at a P value of 0.05.
FIGURE 3.
Estimated attributable fractions and 95% CIs for mortality from all causes other than cardiovascular disease, diabetes, or obesity-related cancers for different anthropometric and body composition variables. 1, BMI; 2, percentage of fat; 3, waist circumference; 4, hip circumference; 5, arm circumference; 6, waist-hip ratio; 7, sum of skinfolds; and 8, waist-stature ratio.
DISCUSSION
BMI is an imperfect measure of adiposity and its use in epidemiologic studies has been criticized (26–28). It is sometimes suggested that weak or negative associations between BMI and mortality are due to the lack of the ability of BMI to discriminate between lean and fat mass and that associations would be strengthened if different measures were used (29). In NHANES III, associations between mortality and elevated BMI were weak, with 1.2% (95% CI: −2.1, 4.4) of deaths associated with BMI in the high (obese) range. However, the associations of the corresponding levels of other anthropometric variables—including waist, hip, and arm circumferences; percentage body fat estimated from bioelectrical impedance; WHR; the sum of 4 skinfold thicknesses, and the WSR—also tended to be weak and in general were quite similar to the association of BMI with mortality. When the mortality outcome was limited to selected causes of death previously shown (7) to be associated with obesity (cardiovascular disease, diabetes, kidney disease, and selected cancers), the association of mortality and BMI in the obese range was stronger, with 5.5% (95% CI: 1.1, 9.9) of deaths from these causes associated with BMI at the high (obese) level. At this level for these causes of death, BMI was associated with a higher percentage of deaths than were the other anthropometric variables considered. These findings do not suggest that the weak adiposity-mortality associations would be stronger if measures of adiposity other than BMI were used.
When the mortality outcome was limited to other causes of death (ie, excluding deaths due to cardiovascular disease, diabetes, kidney disease, and selected cancers), the associations of BMI with mortality at the intermediate (overweight) or high (obese) level were much weaker and generally negative, although not significantly so.
Each of these measures of body size or composition has its limitations. All are highly correlated with each other, which suggests that they are inevitably collinear. As body size, assessed by BMI, increases, percentage of fat tends to increase, body circumferences increase, and skinfold thicknesses increase. In all 3 sets of analyses, all variables had generally similar patterns of excess deaths. No one variable consistently gave higher or lower results than the others. Pairwise comparisons showed no significant differences between variables for the estimates at any level. These findings make it appear unlikely that in these population studies the use of BMI produces appreciably lower or higher estimates of excess mortality than would other measures of adiposity or body size. However, in the NHANES III data, all associations were weak. It is possible that in a sample with stronger associations between body composition and mortality there would be clearer differences between these anthropometric variables.
The reasons for associations between BMI and mortality are imperfectly understood. It is often assumed that any associations are due to the accumulation of adipose tissue, whether overall adiposity or site-specific adiposity. However, the actual mechanism or mechanisms are not clear. Part of the association may be related to incidence and part to survival, and the body size or composition factors related to incidence may differ from those that affect survival outcomes. In addition, the body size and composition factors that affect the incidence of, or survival under, certain conditions may differ across conditions. Given the likely complexity of these associations, it may not be surprising to find that results vary across studies conducted in different populations at different times or with different outcomes.
Results in the literature generally compare relative risks rather than absolute risks and are somewhat mixed. In a large case-control study of survivors of myocardial infarctions, Yusuf et al (22) found that WHR was a better predictor of the risk of myocardial infarctions than were either BMI or waist circumference. In contrast, in a meta-analysis of data on incident diabetes, Vazquez et al (30) found that results for waist circumference, BMI, and WHR were all similar. In our analyses of the NHANES III data, use of the WHR did not result in any systematic differences from BMI or other individual variables. WHR has been found in several studies to be a good predictor of mortality or of incident cardiovascular disease. However, its interpretation is somewhat uncertain. Both waist and hip circumferences are highly correlated with BMI or percentage body fat individually, but their ratio is less correlated. Some evidence suggests that the waist and hip have opposite effects on risk (31). In addition, visceral adiposity may be strongly related to risk, and measures such as BMI, waist circumference, or WHR may be better measures of total body fat than of visceral adiposity (32).
Relative risks compare the risks at lower and higher levels of a variable, but do not provide estimates of the overall contribution of these levels to mortality. For example, it is possible that the highest 10% of any variable identifies a group with similarly elevated absolute risks but that the relative risks are higher for one variable than for another because of differences in the absolute risk in the reference category. The estimates presented here use relative risk estimates as part of the calculations but also take into account other factors to provide an estimate of the sample burden of mortality, which cannot be assessed from relative risks alone. These results suggest that, in terms of the associations with excess deaths, a variety of measurements give similar results to those found for BMI.
Acknowledgments
We thank David Williamson, Emory University, and Mitchell Gail, National Cancer Institute, for their helpful comments.
The authors' responsibilities were as follows—KMF and BIG: participated in developing and drafting the manuscript, conducting statistical analyses, and reviewing the manuscript for scientific content. The authors had no conflicts of interest.
REFERENCES
- 1.Wellens RI, Roche AF, Khamis HJ, Jackson AS, Pollock ML, Siervogel RM. Relationships between the body mass index and body composition. Obes Res 1996;4:35–44 [DOI] [PubMed] [Google Scholar]
- 2.Lemieux S, Prud'homme D, Bouchard C, Tremblay A, Despres JP. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr 1996;64:685–93 [DOI] [PubMed] [Google Scholar]
- 3.Roche AF, Sievogel RM, Chumlea WC, Webb P. Grading body fatness from limited anthropometric data. Am J Clin Nutr 1981;34:2831–8 [DOI] [PubMed] [Google Scholar]
- 4.Roubenoff R. Applications of bioelectrical impedance analysis for body composition to epidemiologic studies. Am J Clin Nutr 1996(suppl);64:459S–62S [DOI] [PubMed] [Google Scholar]
- 5.Lindqvist P, Andersson K, Sundh V, Lissner L, Bjorkelund C, Bengtsson C. Concurrent and separate effects of body mass index and waist-to-hip ratio on 24-year mortality in the Population Study of Women in Gothenburg: evidence of age-dependency. Eur J Epidemiol 2006;21:789–94 [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293:1861–7 [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007;298:2028–37 [DOI] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–94. Series 1: programs and collection procedures. Vital Health Stat 1 1994;32:1–407 [PubMed] [Google Scholar]
- 9.Chumlea WC, Guo SS, Kuczmarski RJ, et al. Body composition estimates from NHANES III bioelectrical impedance data. Int J Obes Relat Metab Disord 2002;26:1596–609 [DOI] [PubMed] [Google Scholar]
- 10.Sun SS, Chumlea WC, Heymsfield SB, et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr 2003;77:331–40 [DOI] [PubMed] [Google Scholar]
- 11.National Center for Health Statistics NHANES III Linked Mortality file documentation. Available from: http://www.cdc.gov/nchs/R&D/nchs_datalinkage/nhanes3_data_linkage_mortality_activities.htm (cited 15 October 2008) [Google Scholar]
- 12.Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 1997;145:72–80 [DOI] [PubMed] [Google Scholar]
- 13.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr 1998;68:899–917 [DOI] [PubMed] [Google Scholar]
- 14.Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation 2007;116:2933–43 [DOI] [PubMed] [Google Scholar]
- 15.Dalton M, Cameron AJ, Zimmet PZ, et al. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med 2003;254:555–63 [DOI] [PubMed] [Google Scholar]
- 16.Dey DK, Rothenberg E, Sundh V, Bosaeus I, Steen B. Body mass index, weight change and mortality in the elderly: a 15 y longitudinal population study of 70 y olds. Eur J Clin Nutr 2001;55:482–92 [DOI] [PubMed] [Google Scholar]
- 17.Folsom AR, Kushi LH, Anderson KE, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med 2000;160:2117–28 [DOI] [PubMed] [Google Scholar]
- 18.Ho SC, Chen YM, Woo JL, Leung SS, Lam TH, Janus ED. Association between simple anthropometric indices and cardiovascular risk factors. Int J Obes Relat Metab Disord 2001;25:1689–97 [DOI] [PubMed] [Google Scholar]
- 19.Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AE. Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am J Clin Nutr 2006;84:449–60 [DOI] [PubMed] [Google Scholar]
- 20.See R, Abdullah SM, McGuire DK, et al. The association of differing measures of overweight and obesity with prevalent atherosclerosis: the Dallas Heart Study. J Am Coll Cardiol 2007;50:752–9 [DOI] [PubMed] [Google Scholar]
- 21.Simpson JA, MacInnis RJ, Peeters A, Hopper JL, Giles GG, English DR. A comparison of adiposity measures as predictors of all-cause mortality: the Melbourne Collaborative Cohort Study. Obesity (Silver Spring) 2007;15:994–1003 [DOI] [PubMed] [Google Scholar]
- 22.Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 2005;366:1640–9 [DOI] [PubMed] [Google Scholar]
- 23.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation 2008;117:1658–67 [DOI] [PubMed] [Google Scholar]
- 24.Graubard BI, Flegal KM, Williamson DF, Gail MH. Estimation of attributable number of deaths and standard errors from simple and complex sampled cohorts. Stat Med 2007;26:2639–49 [DOI] [PubMed] [Google Scholar]
- 25.Korn EL, Graubard BI. Analysis of health surveys. New York, NY: John Wiley & Sons, 1999 [Google Scholar]
- 26.Flint AJ, Rimm EB. Commentary: obesity and cardiovascular disease risk among the young and old—is BMI the wrong benchmark? Int J Epidemiol 2006;35:187–9 [DOI] [PubMed] [Google Scholar]
- 27.Franzosi MG. Should we continue to use BMI as a cardiovascular risk factor? Lancet 2006;368:624–5 [DOI] [PubMed] [Google Scholar]
- 28.Kragelund C, Omland T. A farewell to body-mass index? Lancet 2005;366:1589–91 [DOI] [PubMed] [Google Scholar]
- 29.Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet 2006;368:666–78 [DOI] [PubMed] [Google Scholar]
- 30.Vazquez G, Duval S, Jacobs DR, Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol Rev 2007;29:115–28 [DOI] [PubMed] [Google Scholar]
- 31.Seidell JC, Perusse L, Despres JP, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: the Quebec Family Study. Am J Clin Nutr 2001;74:315–21 [DOI] [PubMed] [Google Scholar]
- 32.Harris TB, Visser M, Everhart J, et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition Study. Ann NY Acad Sci 2000;904:462–73 [DOI] [PubMed] [Google Scholar]