Abstract
Primitive neuroectodermal tumour (PNET) is a rare tumour mainly found in children under ten years old. It may be broadly categorised into those occurring from the central or peripheral nervous system of which the majority arise centrally. We report a 61 year-old lady who had previous lobular breast cancer presenting with a rapidly expanding lesion in her anterior right upper abdominal wall. Clinically it appeared to be benign, however, histopathology of the excised lesion revealed a localised PNET. This case is an unusual case of a PNET in an adult that is peripheral in nature arising from subcutaneous tissue in the abdominal wall.
Background
PNETs are rare tumours that are more prevalent in children than adults and occurirng more commonly in the central nervous system than peripheral. Peripheral PNETs are similar to Ewing's sarcoma [1]. We present a case of a peripheral PNET occurring in the subcutaneous abdominal wall.
Case presentation
A 61 year-old lady presented to clinic with a lesion in her anterior abdominal wall. It was present for four weeks and initially thought to be a sebaceous cyst but had rapidly expanded in that time frame. She had no other symptoms of note. On clinical examination the patient had a lesion measuring 4 × 3 cm firm, fixed, hemispherical with a smooth edge. There was a punctum and some indurated fat around it.
Her past history was of a right-sided breast cancer, she underwent a wide local excision and axillary dissection for a grade 1 lobular carcinoma with no nodal involvement. She underwent adjuvant treatment with radiotherapy and tamoxifen.
She was initially referred due to concern that this lesion was related to her previous breast cancer, however clinically it appeared benign and she underwent elective excision of the lesion under local anaesthesia.
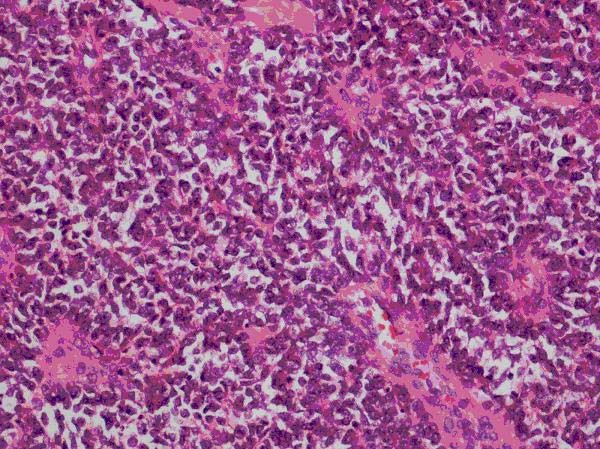
Histopathology revealed a tumour growing as solid sheets diffusely infiltrating the dermis and subcutaneous fat with significant areas of necrosis. The tumour was monomorphic with intermediate sized cells with scanty cytoplasm. There was a hint of rosette formation (Figure 1) but no other differentiating features relating to pigment, gland formation or mucin. Special stains showed cytoplasmic glycogen (Figure 2) and immunohistochemistry showed strong expression of CD99, focal expression of CD56 and focal dot-like expression of cytokeratins, expression of S100 but no expression of other melanoma markers. The combination of morphology and immunochemistry was consistent of the spectrum of primitive neuroectodermal tumours.
Figure 1.
Rosette formation in cells.
Figure 2.
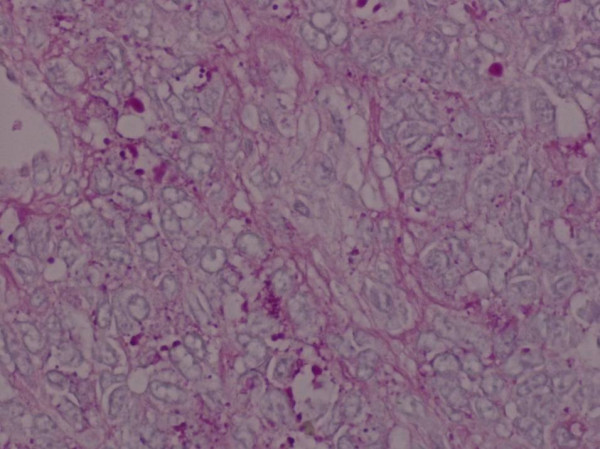
Glycogen in cells.
She was referred to Oncology for adjuvant therapy. Staging CT scan of the chest, abdomen and pelvis revealed ill defined haziness in the subcutaneous fat of the right upper abdomen but no solid or cystic lesions were apparent. No other significant abnormalities were seen. Whole body bone-scan showed no evidence of bony metastases. Bone marrow trephine biopsy showed normocellular marrow with no evidence of neoplasia.
Although the lesion appeared to be completely excised the recommendation was for adjuvant chemotherapy. She was commenced on 6 cycles of Vincristine, Doxorubicin and Cyclophosphamide.
Discussion
Primitive neuroectodermal tumours (PNET) are rare tumours that are more prevalent in children. They may be broadly divided into those occurring in the central nervous system such as non pineal supratentorial PNET, medulloblastoma and pineoblastoma. Those occurring peripherally may resemble soft tissue sarcoma (small round blue cell tumours – SRBCT) and are similar to Ewing's sarcoma as they share common chromosomal change. Although Ewing's sarcomas are more common in bone there are examples of extraosseous tumours that may resemble PNET.
There have been a number of case reports for peripheral PNETs including those in the eye [2,3], maxillo-facial [4-6], peripheral limbs [7,8], gynaecological organs [9-11] and intraabdominal [12,13]. There have been reports of skin and subcutaneous PNETs mainly in children, adolescents and young adults [14] and very few reports specifically regarding abdominal subcutaneous PNET and the only ones have been in children [15,16].
On a histopathology level PNETs are highly cellular showing sheets of small round cells with hyperchromatic nuclei. They the progress with neuron-specific enolase expression then onto rosette formation as demonstrated by this case, cytoplasmic glycogen, phenotypic ganglion cell differentiation and finally neurofilament protein expression. Tumours that are undifferentiated by light microscopy, immunochemistry or electron microscopy have been diagnosed as Ewing sarcoma. The majority of Ewing's sarcomas and PNETs have a t(11;22)(q24;q12) translocation, there are smaller cases of t(21;21)(q21,q12) and t(7,22)(q22,12) translocation. [17]
Treatment of PNETs depends on the type of PNET, position in the body, size of the tumour, spread and the age and health of the patient.
Conclusion
PNETs are a rare form of tumours demonstrating neural differentiation. This case demonstrates an unusual presentation of a PNET in peripheral abdominal subcutaneous tissue in an adult. Treatment involves resection, chemotherapy with or without radiotherapy.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DB Literature searches, writing the paper. BS Performed surgical procedure. RB Performed surgical procedure. KJ Examined surgical specimen, wrote pathological report and provided histological photographic slides. JRS Supervised final revision of the article
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Contributor Information
Dibendu Betal, Email: ulogin2000@yahoo.co.uk.
Behnam Shaygi, Email: bshayegi@yahoo.com.
Ramesh Babu, Email: Ramesh.Babu@iow.nhs.uk.
Kamarul Jamil, Email: Kamarul.Jamil@iow.nhs.uk.
Richard J Sainsbury, Email: Richard.Sainsbury@iow.nhs.uk.
References
- Dehner LP. Primitive neuroectodermal tumour and Ewing's sarcoma. Am J Surg Pathol. 1993;17:1–13. doi: 10.1097/00000478-199301000-00001. [DOI] [PubMed] [Google Scholar]
- Shuangshoti S, Menakanit W, Chanwaivit W, Suwanela Primary intraorbital extraocular primitive neuroectodermal tumour. Br J Opthalmo. 1986;70:543–8. doi: 10.1136/bjo.70.7.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamer C, Oksuz H, Hakverdi S, Karazincir S, Balci A, Yaldiz M. Primary peripheral primitive neuroectodermal tumour of the orbit. Can J Opthalmol. 2007;42:138–40. 10.3129/can j ophthalmol.06-095. [PubMed] [Google Scholar]
- Ozer E, Kanlikama M, Karakurum G, Sirikci A, Erkilic S, Aydin A. Primitive neuroectodermal tumour of the mandible. Int J Pediatr Otorhinolaryngol. 2000;65:257–61. doi: 10.1016/S0165-5876(02)00183-0. [DOI] [PubMed] [Google Scholar]
- Alobid I, Bernal-Sprekelsen M, Alos L, Benitez P, Traserra J, Mullol J. Peripheral primitive neuroectodermal tumour of the left maxillary sinus. Acta Otolaryngol. 2003;123:776–8. doi: 10.1080/00016480310001213. [DOI] [PubMed] [Google Scholar]
- Sun G, Li Z, Wang C. Peripheral neuroectodermal tumour of the maxilla. Br J Oral Maxillofac Surg. 2007;45:226–7. doi: 10.1016/j.bjoms.2005.07.028. [DOI] [PubMed] [Google Scholar]
- Quinlan JF, Healy CF, Rotston D, Murray P. PNET of the hallux. Ir Med J. 2004;97:118. [PubMed] [Google Scholar]
- Jayakumar S, Jatavalabulla S, Miller IM. Peripheral neuroectodermal tumour of the hand in an adult. J Hand Surg Eur Vol. 2007;32:460–1. doi: 10.1016/j.jhse.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Pauwels P, Ambrose P, Hattinger C, Lammens M, Dal Cin P, Ribot J, Struyk A, Berghe H van den. Peripheral primitive neuroectodermal tumour of the cervix. Virchows Arch. 2000;436:68–73. doi: 10.1007/PL00008201. [DOI] [PubMed] [Google Scholar]
- Ng SB, Sirrampalam K, Chuah KL. Primitive neruoectodermal tumours of the uterus: a case report with cytological correlation and review of literature. Pathology. 2002;34:455–61. doi: 10.1080/0031302021000009397. [DOI] [PubMed] [Google Scholar]
- McCluggage WG, Sumathi VP, Nucci MR, Hirsch M, Dal Cin P, Wells M, Flanagan AM, Fisher C. Ewing family of tumours involving the vulva and vagina: report of a series of four cases. J Clin Pathol. 2007;60:674–80. doi: 10.1136/jcp.2006.040931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi B, Smith GT. Primitive neruoectodermal tumours arising in the small bowel. Histopathology. 2007;50:665–6. doi: 10.1111/j.1365-2559.2007.02631.x. [DOI] [PubMed] [Google Scholar]
- Alvarez-Laso C, Azcano E, Gonzalez J, Gonzalez-Pinto I. Primitive neuroectodermal tumour of the retroperitoneum. Clin Transl Oncol. 2008;10:380–2. doi: 10.1007/s12094-008-0217-6. [DOI] [PubMed] [Google Scholar]
- Banerjee SS, Agbamu DA, Eyden BP, Harris M. Clinicopathological characteristics of peripheral primitive neuroectodermal tumour of skin and subcutaneous tissue. Histopathology. 1997;31:355–66. doi: 10.1046/j.1365-2559.1997.2770865.x. [DOI] [PubMed] [Google Scholar]
- Taylor GB, Chan YF. Subcutaneous primitive neuroectodermal tumour in the abdominal wall of a child: long-term survival after local excision. Pathology. 2000;32:294–8. doi: 10.1080/713688937. [DOI] [PubMed] [Google Scholar]
- Somers GR, Shago M, Zielenska M, Chan HS, Hgan BY. Primary subcutaneous primitive neuroectodermal tumor with aggressive behavior and an unusual karyotype: case report. Pediatr Dev Pathol. 2004;7:538–45. doi: 10.1007/s10024-004-2024-6. [DOI] [PubMed] [Google Scholar]
- Rosenburg AE. Bones, Joints and Soft Tissue Tumors. In: Kumar V, Abbas A, Fausto N, editor. Robbins and Cotran Pathological Basis of Disease. Elsevier; 2005. pp. 1301–1302. [Google Scholar]