Abstract
Objective
The present study was undertaken to evaluate the effectiveness of transforaminal epidural steroid injection (TFESI) with using a preganglionic approach for treating lumbar radiculopathy when the nerve root compression was located at the level of the supra-adjacent intervertebral disc.
Materials and Methods
The medical records of the patients who received conventional TFESI at our department from June 2003 to May 2004 were retrospectively reviewed. TFESI was performed in a total of 13 cases at the level of the exiting nerve root, in which the nerve root compression was at the level of the supra-adjacent intervertebral disc (the conventional TFESI group). Since June 2004, we have performed TFESI with using a preganglionic approach at the level of the supra-adjacent intervertebral disc (for example, at the neural foramen of L4-5 for the L5 nerve root) if the nerve root compression was at the level of the supra-adjacent intervertebral disc. Using the inclusion criteria described above, 20 of these patients were also consecutively enrolled in our study (the preganglionic TFESI group). The treatment outcome was assessed using a 5-point patient satisfaction scale and by using a VAS (visual assessment scale). A successful outcome required a patient satisfaction scale score of 3 (very good) or 4 (excellent), and a reduction on the VAS score of > 50% two weeks after performing TFESI. Logistic regression analysis was also performed.
Results
Of the 13 patients in the conventional TFESI group, nine showed satisfactory improvement two weeks after TFESI (69.2%). However, in the preganglionic TFESI group, 18 of the 20 patients (90%) showed satisfactory improvement. The difference between the two approaches in terms of TFESI effectiveness was of borderline significance (p = 0.056; odds ratio: 10.483).
Conclusion
We conclude that preganglionic TFESI has the better therapeutic effect on radiculopathy caused by nerve root compression at the level of the supra-adjacent disc than does conventional TFESI, and the diffence between the two treatments had borderline statistical significance.
Keywords: Spine, interventional procedure; Spine, therapeutic radiology
The epidural space has historically been accessed inferiorly by using a caudal approach or it has been accessed posteriorly by using an interlaminar approach, and this procedure is often done without fluoroscopic aid (1-2). Interlaminar and caudal epidural injections require relatively large volumes of injectate to deliver the steroid to the presumed pathologic site, and these types of injections also introduce the risk of extraepidural and intravascular needle placement. Thus, transforaminal epidural steroid injection (TFESI) under fluoroscopic guidance has emerged as the preferred approach to the epidural space (3-5).
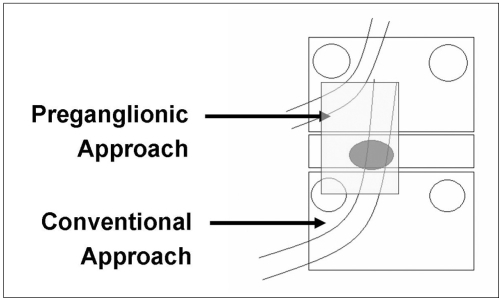
In some cases of lumbosacral radiculopathy that are secondary to stenosis or a herniated disc, the site of impingement can lie at the level of the supra-adjacent intervertebral disc, which is rostral to the conventional lumbar TFESI bevel position. Lew et al. (6) have suggested that because one cannot always guarantee a rostral spread of injectate to bathe the epidural/preganglionic portion of the nerve root, a preganglionic approach at the level of the supra-adjacent intervertebral disc (for example, the L4-5 disc level for a L5 nerve root) could be helpful (Fig. 1). Theoretically, by utilizing the preganglionic approach for TFESI, the injectate can be placed closer to the site of neural impingement and so provide a more effective washout of inflammatory disc material. However, the above suggestion is not based on any clinical study. To the best of our knowledge, based on a comprehensive MEDLINE literature review, no published study has yet assessed the effectiveness of TFESI with using a preganglionic approach when the site of impingement lies at the level of the supraadjacent intervertebral disc. The present study was undertaken to evaluate the effectiveness of TFESI with using a preganglionic approach for lumbar radiculopathy when the nerve root compression is located at the level of the supra-adjacent intervertebral disc.
Fig. 1.
Schematic description for transforaminal epidural steroid injection with the preganglionic approach versus the conventional approach.
MATERIALS AND METHODS
Patients
One radiologist retrospectively reviewed the medical records of the patients who received TFESI using the conventional approach at our department during a 1-year period, from June 2003 to May 2004. This involved performing TFESI at the location of the exiting nerve root, regardless of the level of the nerve root compression. For example, TFESI for L5 radiculopathy was performed at the neural foramen of L5-S1 even when the L5 nerve root compression was in the paracentral or subarticular region at the level of the L4-5 disc. After a consensus meeting between three radiologists who were unaware of the clinical results after TFESI, we selected those cases treated by conventional TFESI with supra-adjacent nerve root impingement. The inclusion criteria were (a) the presence of lumbar radiculopathy, (b) nerve root compression in the paracentral or subarticular region at the level of the supra-adjacent intervertebral disc (for example, at the L4-5 disc level for the L5 nerve root), (c) one level TFESI from L1 to S1, (d) no prior therapeutic TFESI, (e) no prior surgery, and (f) clear identification of the nerve root compression by using a cross-sectional imaging study (either computed tomography or magnetic resonance imaging). Thirteen patients who met all the criteria were included and they were referred to as the conventional TFESI group.
However, since June 2004, we have used TFESI with the preganglionic approach at the supra-adjacent intervertebral disc (for example, at the neural foramen of L4-5 for a L5 nerve root) if the nerve root compression was at the level of the supra-adjacent intervertebral disc. Using the same inclusion criteria as mentioned above, a total of 20 patients were consecutively enrolled and they were referred to as the preganglionic TFESI group.
Technique
Ttransforaminal epidural steroid injection using the conventional approach was conducted under biplane fluoroscopic guidance by two radiologists who were very experienced in spinal interventions. All the treatments were performed as outpatient procedures, and written informed consents were obtained from all the patients. With a patient lying in the prone position, the tube was rotated obliquely to ensure injection at the neural foramen. The goal of positioning was to allow a perpendicular needle tract toward the classic injection site underneath the pedicle, in the so-called "safe triangle" (5, 7). The safe triangle was defined by the pedicle superiorly, the lateral border of the vertebral body laterally, and the outer margin of the spinal nerve medially. After disinfecting the skin, local anesthetic was administered by using a 25-gauge needle. Under fluoroscopic guidance, a 12-cm 22-gauge spinal needle was then advanced into the safe triangle. At the same time, a lateral view was obtained to verify that the anterior-posterior position of the needle tip was appropriate. The needle position was checked by biplane fluoroscopy, and this was followed by the injection of about 1 mL of contrast material (Omnipaque 300 [IOHEXOL, 300 mg of iodine per milliliter]; Amersham Health, Princeton, NJ). The posteroanterior and lateral spot radiographs were obtained to document the distribution of the contrast material. Bupivacaine hydrochloride (0.5 ml, Marcaine Spinal 0.5% Heavy; AstraZeneca, Westborough, MA) and 40 mg (1 mL) of triamcinolon acetonide suspension (Tamcelon; Hanall, Seoul, Korea) were slowly injected.
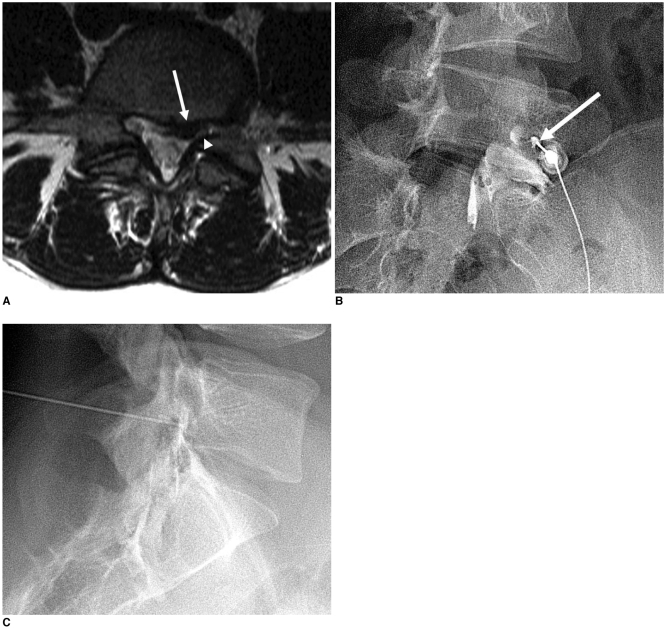
In terms of TFESI with using the preganglionic approach, the goal of positioning the needle tip was medial and inferior to that used in the conventional approach. In our department, we target injections just lateral to the pars interarticularis on the oblique view during the preganglionic approach (Fig. 2).
Fig. 2.
A 20-year-old girl with left leg pain. On the T2-weighted MR images (A), an extruded disc (arrow) was evident at L5-S1. This disc was located in the left central zone and it had migrated inferiorly to compress the left S1 nerve root (arrowhead). We performed transforaminal epidural injection with using the preganglionic approach at the L5-S1 level (B, C). In the oblique view (B), the needle tip was inserted just lateral to the pars interarticularis (arrow). The leg pain had been relieved at the 2-week follow-up.
A fortnight after TFESI, the patients were followed-up at our outpatient department. This length of follow-up has been proposed in the literature and relates to the duration of the therapeutic effect of corticosteroid (7). To check the effect of TFESI, all the patients were recommended not take any drugs or to participate in any physical therapy for their sciatica before this 2-week follow-up.
Review of the Radiologic and Clinical Data
The level and cause of nerve root compression on the CT or MR imaging and the level of radiculopathy were documented in the medical charts before performing TFESI. After retrospectively reviewing medical records, we classified the cause of radiculopathy as being due to a herniated intervertebral disc (HIVD) or it was due to spinal stenosis. The patients' demographic variables were also detailed at the initial clinical evaluation. For statistical analysis, we classified the patients' ages into six age groups; < 29-years-old, 30-39, 40-49, 50-59, 60-69 and > 70. The duration of radiculopathy was also treated as a potential predictive variable, and it was classified as acute or subacute, i.e., < 6 months or chronic (> 6 months) (8).
The effectiveness of TFESI was evaluated two weeks after the procedures. The treatment outcome was assessed using a 5-point patient satisfaction scale, i.e., 0 (poor), 1 (fair), 2 (good), 3 (very good), and 4 (excellent), and by using a VAS (visual assessment scale) that ranged from 0 to 100. A successful outcome required a patient satisfaction score of 3 (very good) or 4 (excellent), and a reduction on the VAS of > 50% two weeks after the TFESI. The patients with a successful outcome were referred to as having received effective treatment and those patients without a successful outcome were referred to as having received ineffective treatment.
Statistics
Logistic regression analysis was performed and the factors included were conventional or preganglionic TFESI, the cause of radiculopathy, the patients' age and gender and the duration of radiculopathy. The Mann-Whitney U test was also used to evaluate for age differences between the two groups (the conventional and preganglionic groups). SPSS, version 10.0 (SPSS, Chicago, IL) was used throughout the analysis. P values < 0.05 were considered statistically significant.
RESULTS
The study subjects were 22 women and 11 men with a mean age of 55.1 years (age range: 17-76, standard deviation [SD]: 14.1). The mean age was 53.9 years (SD: 13.4) in the conventional TFESI group and it was was 55.8 years (SD: 14.8) in the preganglionic TFESI group. There was no statistical difference between the two groups in terms of age.
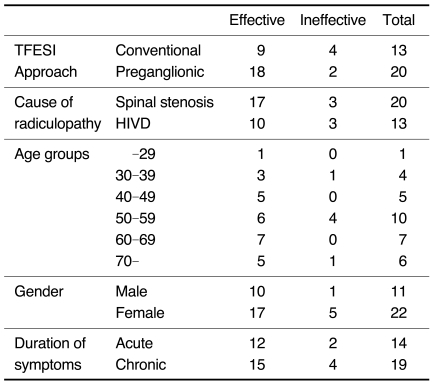
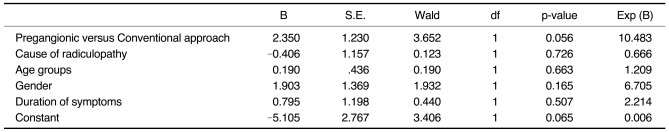
Of the 13 patients in the conventional TFESI group, nine showed effective treatment two weeks after TFESI (69.2%), and 18 of the 20 patients (90%) in the preganglionic TFESI group showed effective treatment, and the difference in the two rates of effective treatment was of borderline significance (p = 0.056; odds ratio 10.483). The cause of radiculopathy, the age of the groups, gender and the duration of symptoms were not found to be statistically related to the effectivness of TFESI (p > 0.05). These results are summarized in Tables 1, 2.
Table 1.
Possible Predictors of Outcome versus the TFESI Effectiveness
Note.-TFESI = transforaminal epidural steroid injection, HIVD = herniated intervertebral disc
Table 2.
Logistic Regression Analysis for the Possible Predictors of Outcome for the Effectiveness of TFESI
Note.-TFESI = transforaminal epidural steroid injection, B = regression coefficient, S.E. = standard error, Wald = Wald statistics, df = degree of freedom, Exp (B) = odds ratio
In the conventional TFESI group, seven patients (53.8%) had spinal stenosis and six patients (46.2%) had HIVD, and in the preganglionic TFESI group, 13 patients (65%) had spinal stenosis and seven patients (35%) had HIVD. In the conventional TFESI group, the radiculopathy was acute or subacute in eight patients (61.5%) and chronic in five patients (38.5%); in the preganglionic TFESI group, radiculopathy was acute or subacute in six patients (30%) and it was chronic in 14 patients (70%). In the conventional TFESI group, TFESI at L5-S1 was performed in 10 patients and TFESI at L4-5 was performed in three patients; in the preganglionic TFESI group, TFESI was performed at L5-S1 in five patients, at L4-5 in 14 patients and at L3-4 in one patient.
DISCUSSION
Lumbosacral radiculopathy is a common and costly medical disease, and its lifetime prevalence has been estimated to be 40-60% (9). Based on the recent concepts of pain generation in the sciatic condition, it's believed that concomitant chemical irritation of the nerve root that's caused by disk material is the decisive factor for the development of severe sciatica, rather than the pain being due to mechanical compression alone (10-16). According to this concept, the local application of corticosteroids in the area of the compressed, inflamed nerve root appears to be a reasonable treatment option. Thus, percutaneous injection based therapies, including TFESI, are being used with increasing frequency to treat the radiculopathy resulting from a herniated disc or degenerative lumbar spinal stenosis (17-19). In contrast to an interlaminar or a caudal epidural steroid injection, TFESI provides a low volume of concentrated medication to a selected nerve root.
It is important to clarify the terminology used to describe epidural injections. Medical journals and texts often incorrectly refer to transforaminal epidural injections as "selective epidural injections", "selective nerve root blocks", or "nerve root sleeve injections". However, the International Spinal Intervention Society (ISIS), has promoted the used of a nomenclature based on precise anatomic descriptors, and it recommends the term "transforaminal" (5). Gajraj (4) mentioned that to be selective, a nerve root block should be performed extraforaminally and distal to the division of the ventral and dorsal rami; otherwise, the dorsal ramus and its innervated structures would also be anesthetized. Therefore, they suggested that the therapeutic procedure be referred to as a 'transforaminal epidural steroid injection' and that the diagnostic procedure should be referred to as a 'selective spinal nerve block' or a 'selective ventral ramus block.'
In the case of TFESI with using the conventional approach, the spinal needle is positioned within the "safe triangle" (bordering the pedicle, the exiting nerve root and the lateral border of the vertebral body), with the bevel placed below the inferior aspect of the pedicle (5, 7). Using this conventional approach, the injectate typically bathes the epidural space around the dorsal root ganglion and then it descends along the distal aspect of the nerve root. Ideally, if there is no stenosis and the needle tip is appropriately positioned, the injectate may spread rostrally to the epidural portion of the preganglionic nerve root as well. However, for most cases of lumbosacral radiculopathy that are secondary to stenosis or a herniated disc, the site of impingement usually lies at the level of the supra-adjacent intervertebral disc, which is rostral to the conventional lumbar TFESI bevel position. In addition, one cannot always guarantee a rostral spread of injectate to the epidural/preganglionic portion of the nerve root. Thus, performing preganglionic TFESI at the supra-adjacent level may be a more effective method to deliver injectate to a target site.
For the preganglionic approach, it is important that the injectate distributes itself predominantly in the epidural space at the disc level (more inferior than that for the conventional approach), and that it does not excessively spread along the spinal nerve at the supra-adjacent level, which is not inflamed or compressed. Lew et al. (6) inserted the needle into the inferior and anterior neural foramen for performing preganglionic TFESI, and we use a modification of this method. The landmark we use for needle insertion is just lateral to the pars interarticularis on the oblique view; this is medial and inferior to that used for the conventional approach (Fig. 2B). Using this approach, we can inject drugs almost to the epidural space.
The present study has several limitations. First, it is not a controlled, randomized prospective study; thus, it has the limitations of a retrospective study and so a randomized, prospective study is warranted. Second, the study is based on only the short-term therapeutic effect. Third, other factors that probably influenced the therapeutic effect were not included.
In conclusion, preganglionic TFESI was found to have a better therapeutic effect on the radiculopathy caused by compression at the supra-adjacent level than did conventional TFESI, and this result had borderline statistical significance.
References
- 1.Robecchi A, Capra R. Hydrocortisone (compound F); first clinical experiments in the field of rheumatology. Minerva Med. 1952;43:1259–1163. [PubMed] [Google Scholar]
- 2.Benzon HT. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986;24:277–295. doi: 10.1016/0304-3959(86)90115-6. [DOI] [PubMed] [Google Scholar]
- 3.Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002;27:11–16. doi: 10.1097/00007632-200201010-00005. [DOI] [PubMed] [Google Scholar]
- 4.Gajraj NM. Selective nerve root blocks for low back pain and radiculopathy. Reg Anesth Pain Med. 2004;29:243–256. doi: 10.1016/j.rapm.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 5.Sitzman BT. Epidural injections. In: Fenton DS, Czervionke LF, editors. Image-guided spine intervention. Philadelphia: Saunders; 2003. pp. 99–126. [Google Scholar]
- 6.Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2004;83:378. doi: 10.1097/00002060-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Pfirrmann CW, Oberholzer PA, Zanetti M, Boos N, Trudell DJ, Resnick D, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness-a study with patients and cadavers. Radiology. 2001;221:704–711. doi: 10.1148/radiol.2213001635. [DOI] [PubMed] [Google Scholar]
- 8.Sontag MJ. A theoretical overview of the diagnosis and management of low back pain: acute vs chronic pain and the mind/body continuum. In: Cole AJ, Herring SA, editors. The low back pain handbook: a guide for the practicing clinician. 2nd ed. Philadelphia: Hanley & Belfus; 1993. pp. 39–48. [Google Scholar]
- 9.Anderson GBJ. Epidemiology of spinal disorders. In: Frymoyer JW, editor. The adult spine: principles and practice. New York: Raven; 1997. pp. 93–141. [Google Scholar]
- 10.Takahashi H, Suguro T, Okazima Y, Motegi M, Okada Y, Kakiuchi T. Inflammatory cytokines in the herniated disc of the lumbar spine. Spine. 1996;21:218–224. doi: 10.1097/00007632-199601150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Kanemoto M, Hukuda S, Komiya Y, Katsuura A, Nishioka J. Immunohistochemical study of matrix metalloproteinase-3 and tissue inhibitor of metalloproteinase-1 human intervertebral discs. Spine. 1996;21:1–8. doi: 10.1097/00007632-199601010-00001. [DOI] [PubMed] [Google Scholar]
- 12.Kawakami M, Weinstein JN, Spratt KF, Chatani K, Traub RJ, Meller ST, et al. Experimental lumbar radiculopathy: Immunohistochemical and quantitative demonstrations of pain induced by lumbar nerve root irritation of the rat. Spine. 1994;19:1780–1794. doi: 10.1097/00007632-199408150-00001. [DOI] [PubMed] [Google Scholar]
- 13.Roberts S, Caterson B, Menage J, Evans EH, Jaffray DC, Eisenstein SM. Matrix metalloproteinases and aggrecanase: their role in disorders of the human intervertebral disc. Spine. 2000;25:3005–3013. doi: 10.1097/00007632-200012010-00007. [DOI] [PubMed] [Google Scholar]
- 14.Delamarter RB, Bohlman HH, Dodge LD, Biro C. Experimental lumbar spinal stenosis. Analysis of the cortical evoked potentials, microvasculature, and histopathology. J Bone Joint Surg (Am) 1990;72:110–112. [PubMed] [Google Scholar]
- 15.Olmarker K, Holm S, Rosenqvist A. Experimental nerve root compression. A model of acute, graded compression of the porcine cauda equina and an analysis of neural and vascular anatomy. Spine. 1991;16:61–69. [PubMed] [Google Scholar]
- 16.Schonstrom N, Bolender NF, Spen-gler DM, Hansson TH. Pressure changes within the cauda equina following constriction of the dural sac. An in vitro experimental study. Spine. 1984;9:604–607. doi: 10.1097/00007632-198409000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Johnnsson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptive c-fibers. Acta Anesthesiol Scand. 1990;34:335–338. doi: 10.1111/j.1399-6576.1990.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 18.Kantrowitz F, Robinson DR, McGuire MB, Levine L. Corticosteroids inhibit prostaglandin production by rheumatoid synovia. Nature. 1975;258:737–739. doi: 10.1038/258737a0. [DOI] [PubMed] [Google Scholar]
- 19.Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy: An outcome study. Spine. 1989;14:431–437. doi: 10.1097/00007632-198904000-00018. [DOI] [PubMed] [Google Scholar]