Abstract
Objective
The aim of this study was to analyze the computed tomographic (CT) findings of atypical adenomatous hyperplasia (AAH) in the lung.
Materials and Methods
The CT findings of AAHs in eight patients were retrospectively reviewed. The CT findings of each AAH lesion were evaluated for multiplicity, location, shape, size and internal density of the lesion, the interface between the normal lung and the lesion, the internal features within the lesion and any change of the lesion on the follow-up CT scans (range: 33 to 540 days; average: 145.3 days).
Results
The eight patients consisted of three men and five women (age range: 43-71 years). Six of eight patients were asymptomatic. Four of them (50%) had synchronous malignancies in the lung: adenocarcinoma of the lung (n = 3), and metastatic squamous cell carcinoma from the uterus (n = 1). We could identify and evaluate eleven AAH nodules in seven patients on the CT scans. Three patients had multiple AAHs. Seven of the 11 lesions (64%) were located in the upper lobe. All the AAHs showed a well-defined oval or round shape and pure ground-glass opacity (GGO) without any solid component (size: 3.9×3 mm to 19×17 mm; internal attenuation: -467 to -785 HU). All the AAHs showed no change of their size and internal density on the follow-up CT scans.
Conclusion
Atypical adenomatous hyperplasia is often associated with malignancy. This tumor is shown on CT as persistent well-defined oval or round nodular GGOs without solid components, and it does not change on the follow-up CT.
Keywords: Lung, CT; Lung, diseases; Ground-glass opacity; Atypical adenomatous hyperplasia
Atypical adenomatous hyperplasia of the lung (AAH) is defined as a peripheral focal proliferation of atypical cuboidal or columnar epitheial cells along the alveoli and respiratory bronchioles (1). Its morphological similarity and recent molecular biological analysis have suggested that AAH could be a precursor lesion or even an early lesion of well-differentiated adenocarcinoma of the peripheral lung (2-6). In past, the AAH that could not be detected on the radiologic examinations before surgery was discovered incidentally in the surgically resected specimens from lung cancer patients, and this lesion was predominantly seen in adenocarcinoma patients (7). However, the number of radiologically detected AAH lesions has been increasing in Japan due to the wide-spread use of CT in clinical practice and also because of the mass screening for early lung cancer (8). Since mass screening for early lung cancer using CT is prevalent in other countries, including Korea, the radiologically detected AAH will increase dramatically as it did in Japan.
To the best of our knowledge, some investigators have reported the radiologic and clinical features or the pathologic characteristics of AAH, but there are few reports in the radiologic literature that give a comprehensive assessment about AAH in the radiologic literature. Moreover, there is no report about AAH occurring in the Korean population. Thus, the aim of this study was to analyze the CT findings of AAH.
MATERIALS AND METHODS
Between May 2004 and July 2005, AAHs were pathologically confirmed in eight patients at our institution. Five patients had undergone standard thoracotomy either by lobectomy (n = 2), segmentectomy (n = 1), or wedge resection (n = 2), and three patients had video-assisted thoracic surgery (VATS) performed on them. This study was conducted retrospectively with these eight patients.
Clinical Features of the AAH Patients
We reviewed the medical records using the electronic medical records system of our hospital. The following clinical features of AAH patients were recorded: gender, age, smoking history, the presence of symptom, a past history of diseases including any kind of malignancies or respiratory disease, and the presence and histologic type of synchronous malignancy.
CT Scanning
Unenhanced CT was performed with two kinds of multidetector helical CT scanners (Light Speed Ultra, GE Medical Systems, Milwaukee, WI; Sensation-16, Siemens Medical Systems, Forchheim, Germany) in all the eight patients. Specific parameters are given for the following settings: for the Light Speed Ultra CT scanner that was used for five patients, the peak tube voltage was 120 kVp, the tube current was 400 mAs, the rotation time was 0.6 seconds, the reconstruction thickness was 1.25 mm and the detector configuration was 8-detector rows with a pitch of 0.875; for the Sensation-16 CT scanner that was used for the remaining three patients, the peak tube voltage was 140 kVp, the tube current was 250 mAs, the rotation time was 0.5 seconds, the reconstruction thickness was 1.00 mm and the detector configuration was 16-detector rows with a pitch of 1.00. Each patient underwent chest CT examination for an average of 2.25 times (range: one to three times) before surgery, and seven patients had follow-up chest CT performed. The interval between the initial scan and the last CT scan before surgery was 33 to 540 days, with an average of 145.3 days.
CT Findings and the Pathologic Features of AAH
Four radiologists (C.M.P., H.J.L., C.H.L., and J.M.G.) analyzed all the CT images using the lung setting (a window level of -700 HU and a width of 1,500 HU). Any discrepancies were resolved by consensus. The CT findings of each AAH lesion were recorded as follows: (a) multiplicity, (b) location of the lesion, (c) shape (round, oval, polygonal or irregular), (d) size and internal density of the lesion, (e) interface between the normal lung and the lesion (well-defined or poorly-defined), (f) internal features within the lesion (pure ground-glass opacity [GGO], mixed GGO, solid), and (g) any change of the lesion on the follow-up CT scans.
The size and internal density (HU) of each lesion was measured at the largest section of the lesion by one radiologist (C.M.P.), and a region of interest (ROI) was set on the whole area of the lesion. Great effort was made to avoid the vessels. GGO was defined as a hazy opacity that did not obscure the underlying pulmonary vessels (9). We evaluated the follow-up CT scans by consensus with paying great attention to any change of the lesion, including size, internal density, marginal characteristics and the presence of solid component. This evaluation was conducted by displaying two image sets side by side on a liquid crystal display monitor for the seven patients having follow-up CT images.
The AAH lesions were microscopically evaluated by conventional hematoxylin-eosin (H-E) staining. The cases were diagnosed according to the 1999 WHO classification (10). Pathologic sections of the each resected lesion were compared to the corresponding CT images. These comparisons were performed via a consensus between a pathologist (D.H.C.) and a radiologist (J.M.G.).
RESULTS
The clinical features and CT findings for the eight patients with AAH are summarized in Table 1. Three patients had multiple AAH nodules and five patients had a single AAH.
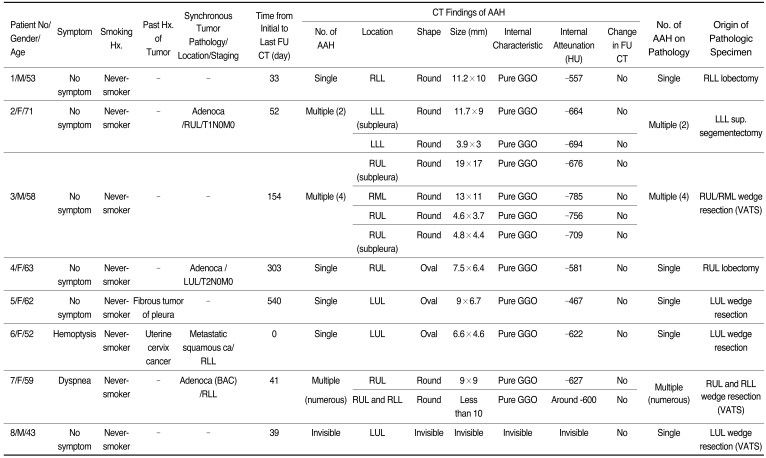
Table 1.
Clinical and CT Features for the Eight Patients with Atypical Adenomatous Hyperplasia
Note.-AAH = atypical adenomatous hyperplasia, VATS = video-assisted thoracic surgery, RUL = right upper lobe, RML = right middle lobe, RLL = right lower lobe, LUL = left upper lobe, sup. = superior, LLL = left lower lobe, GGO = ground-glass opacity, FU = follow-up, adenoca = adenocarcinoma of the lung, squamous ca = squamous cell carcinoma, BAC = bronchioloalveolar carcinoma
Clinical Features of AAH Patients
The eight patients consisted of three men and five women, and their ages ranged from 43 to 71 years (mean age: 57.6 years), and all patients were never-smokers. Six individuals were asymptomatic and their AAH nodules were incidentally detected by the CT screening for lung cancer. Two patients had symptoms, which were bloodtinged sputum and dyspnea, respectively. Two patients had past history of other primary neoplasms; one had uterine cervix cancer, and the other had benign solitary fibrous tumor of the pleura. Four of them (50%) had synchronous malignancies in the lung (Fig. 1); adenocarcinoma of the lung (n = 3), and metastatic squamous cell carcinoma from the uterus (n = 1).
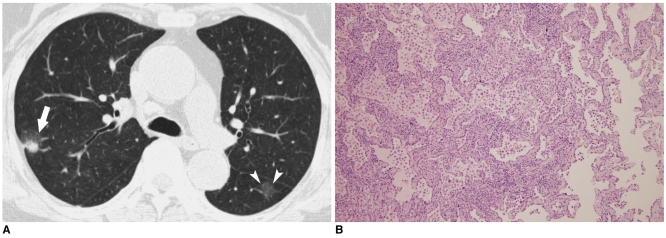
Fig. 1.
A 71-year-old woman with adenocarcinoma in the right upper lobe and atypical adenomatous hyperplasia in the left lower lobe.
A. The transverse thin section CT scan shows an 11.7×9 mm well-defined round nodule (arrowheads) with pure ground-glass opacity in the left lower lobe and a 30×27 mm mixed ground-glass opacity lesion (arrow) in the right upper lobe. Note the solid portion of the right upper lobe lesion.
B. Photomicrograph of the left lower lobe superior segmentectomy specimen (H & E staining,×40) shows atypical epithelial cell proliferation along the thickened alveolar septa, which is consistent with atypical adenomatous hyperplasia.
CT Findings and the Pathologic Features of AAH
By means of CT, we could identify and evaluate 11 pathologically proven AAH nodules in seven patients. In one patient, thin section CT could not demonstrate a 2 mm subpleural AAH. Three patients had multiple nodular GGOs that were representative of multiple AAHs. Seven AAH lesions (64%) were located in the upper lobe. In all cases, the AAHs appeared as round or oval shapes, the interface between the AAHs and the normal lung parenchyma was well-defined and the margin was smooth (Fig. 2). Vascular convergency or pleural retraction was not detected. The lesion sizes were measured as 3.9×3 mm to 19×17 mm, and internal densities were measured as -467 to -785 HU with a mean of -648.9 HU on their initial diagnostic images, and all the AAHs showed pure GGO without any solid component in it. There were no changes in the AAH lesions for the seven patients with follow-up CT.
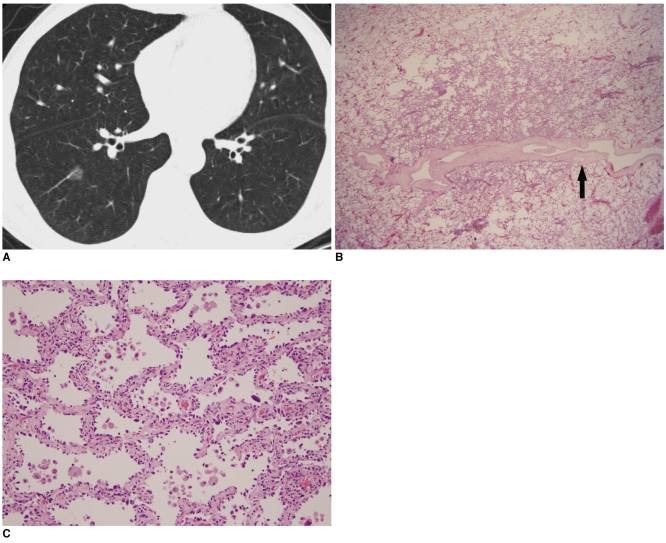
Fig. 2.
A 53-year-old woman with a single atypical adenomatous hyperplasia in the right lower lobe.
A. Transverse thin section CT scan shows an 11.2×10 mm well defined round nodule with pure ground-glass opacity in the right lower lobe. Note the pulmonary vessel penetrates the ground-glass opacity lesion without any vascular compromise.
B. Photomicrograph (H & E staining, ×10) shows that the boundary between the atypical adenomatous hyperplasia and the underlying lung parenchyma is distinct. Note the pulmonary vessel penetrating the AAH lesion (black arrow).
C. High power photomicrograph (H & E staining, ×100) shows atypical epithelial cell proliferation along the thickened alveolar septa, which is consistent with atypical adenomatous hyperplasia.
In patient 7, there were disseminated nodular GGOs in the bilateral lungs (Fig. 3). One of the nodular GGO lesions in the right lower lobe was diagnosed as bronchioloalveolar carcinoma (BAC) and the other lesions were diagnosed as multiple AAHs in the right upper lobe and in the right lower lobe wedge-resection specimen. Because the pure GGO nodules seen on the CT scan and the AAHs in the pathologic specimen were numerous, lesion by lesion comparison was possible for only one AAH in the right upper lobe.
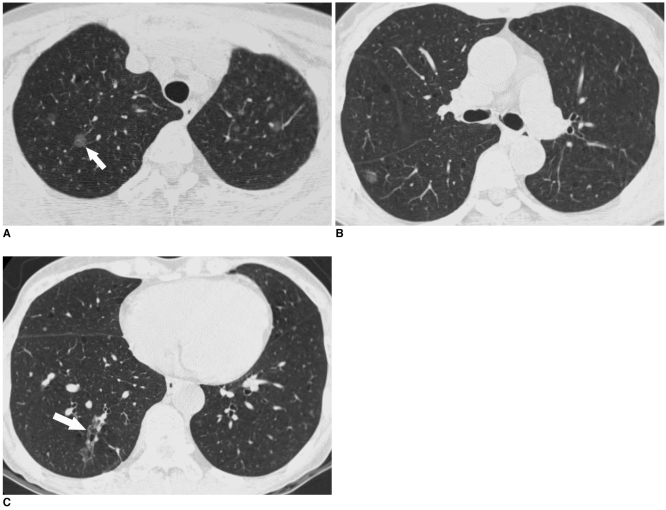
Fig. 3.
A 59-year-old woman with disseminated nodular ground-glass opacitys in the bilateral lungs. Wedge resections for the right upper lobe and the right lower lobe were conducted for making the diagnosis for these lesions.
A, B. Transverse thin section CT shows numerous round nodular ground-glass opacitys smaller than 10 mm in the bilateral lungs, and especially in the bilateral upper lobes. On the wedge resection specimen, these lesions, including a 9×9 mm sized well-defined round ground-glass opacity (arrow), were diagnosed as multiple atypical adenomatous hyperplasias.
C. The irregular ground-glass opacity lesion (arrow) was confirmed as bronchioloalveolar carcinoma on the pathologic specimen.
In patient 8, the screening CT that was done for detecting lung cancer discovered a 6 mm well-defined solid nodule in the left upper lobe; left upper lobe wedge resection was done for this lesion. Pathologic examination revealed a focal atelectatic lung for this lesion, and a 2 mm AAH in the subpleural area was also incidentally detected.
DISCUSSION
Since the introduction of mass screening for lung cancer using spiral CT, small pulmonary nodules have been detectable, and previously, these could not discovered by plain radiography; further, small peripheral lung cancer has been detected more easily and frequently (3, 11, 12). However, as performing screening CT has shown an increasing number of small indeterminate nodules, an emerging concern is whether or not these lesions require additional diagnostic steps such as follow-up, and also whether they require pathology-confirming procedures such as resection. AAH is now the focus of this issue.
In the clinicopathologic literature, the incidence of AAH is 2.8% in the over-all age group (13) and it is 6.6% in the elder group (14). Additionally, this tumor occurs much more frequently in the cancer populations, and especially lung cancer patients, and the incidence ranges from 10% to 23.2% (14-16). However, according to Kawakami et al.'s prospective study (17), AAH is very rare in asymptomatic individuals, and its incidence is about 0.05%. This discrepancy in the incidence could be explained in that only limited detection of AAH is based on radiologic methods, including thin section CT, and most AAH lesions are very small in size and they have low contrast on the radiologic images. Actually, Kawakami et al. (17) identified the AAH lesions that could be detected on HRCT. We could detect a 3.9×3 mm sized AAH lesion on CT, yet one 2 mm subpleural AAH was not identified. According to Ishikawa (18) the detection rate of AAH lesions greater than 3 mm in diameter is 57%, while that of the lesions smaller than 2 mm in diameter was 35%.
In this study, all the AAH patients were never-smokers, and this correlates well with a previous study (19). AAH patients are usually asymptomatic (19), while two patients in our study had symptoms; one had dyspnea and the other had blood tinged sputum. The patient with dyspnea had disseminated lesions throughout the bilateral lungs. The other patient with blood tinged sputum had metastatic squamous cell carcinoma from the uterine cervix in the contralateral lung.
Atypical adenomatous hyperplasia has been thought to be closely associated with malignancy and especially lung cancer (14, 15). In our study, four of eight patients had synchronous malignancies, particularly adenocarcinoma of the lung, which is consistent with the other previous reports (2, 14, 15). In recent years, multiple AAH lesions have been thought to be closely associated with adenocarcinoma and particularly multiple adenocarcinomas (15, 20); this could suggest that AAH is a precursor lesion of adenocarcinoma, and it supports the concept of the multistep carcinogenesis process from AAH to adenocarcinoma of the lung. In this study, two of three multiple AAH patients (67%) had adenocarcinoma, and two of three adenocarcinoma patients had multiple AAH lesions.
Seven AAH lesions that were demonstrated on CT (64%) were located in the upper lobe, and on the pathologic specimens, the predilection of upper lobe for AAH was more distinct. In two previous studies (7, 17) that both had less than ten cases each, a predilection for the upper lobe was also demonstrated, although the reason for this is not clear. Nakahara et al. (15) also reported that AAH lesions were most frequently located in the upper lobes in their study of 118 AAH cases. In our case with disseminated nodular GGOs, these lesions were discovered throughout the whole lungs with predominance for the upper lung. Many of the nodular GGOs that remained undiagnosed were probably mostly AAHs but some of them could have been BACs, the same as the one nodule in the right lower lobe.
We had four AAH lesions greater than 10 mm in size. Some authors (20) insisted that the persistent nodular GGO greater than 10 mm were carcinoma without exception; however, other authors (17) have reported the case of an AAH greater than 10 mm in size, as was seen in our study. Although AAH is usually smaller than adenocarcinoma or BAC, the lesion size can not be used as the diagnosis criteria.
Atypical adenomatous hyperplasia has been described as a focal nodular GGO lesion on CT (7, 17, 18). GGO of AAH is thought to represent the unique replacement growth pattern of the lesion. Our results in this study are totally consistent with those of the previous studies that AAH shows well-defined oval or round GGO without any central solid component (11, 20) and the internal density of AAHs in our study was similar with the result of a previous study (17). However, nodular GGO is one of the prevalent findings detected by CT. Meticulous evaluation of the shape and border of the focal GGO and particularly, the lesional change on the follow-up CT could be helpful to differentiate AAH from other benign diseases that manifest as focal GGOs. A recent study has suggested that these nodular GGOs can be found with the aid of computer systems (21).
In conclusion, AAH is often associated with malignancy. It is observed as persistent, well-defined oval or round nodular GGOs without solid components on CT, and it does not change on the follow-up CT.
Footnotes
This study is supported by KISTEP, Ministry of Science and Technology, Korea.
References
- 1.Weng S, Tsuchiya E, Satoh Y, Kitagawa T, Nakagawa K, Sugano H. Multiple atypical hyperplasia of type II pneumocytes and bronchioloalveolar carcinoma. Histopathology. 1990;16:101–103. doi: 10.1111/j.1365-2559.1990.tb01073.x. [DOI] [PubMed] [Google Scholar]
- 2.Carey FA, Wallace WA, Fergusson RJ, Kerr KM, Lamb D. Alveolar atypical hyperplasia in association with primary pulmonary adenocarcinoma: a clinicopathological study of 10 cases. Thorax. 1992;47:1041–1043. doi: 10.1136/thx.47.12.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colby TV, Wistuba II, Gazdar A. Precursors to pulmonary neoplasia. Adv Anat Pathol. 1998;5:205–215. doi: 10.1097/00125480-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Yokozaki M, Kodama T, Yokose T, Matsumoto T, Mukai K. Differentiation of atypical adenomatous hyperplasia and adenocarcinoma of the lung by use of DNA ploidy and morphometric analysis. Mod Pathol. 1996;9:1156–1164. [PubMed] [Google Scholar]
- 5.Pueblitz S, Hieger LR. Expression of p53 and CEA in atypical adenomatous hyperplasia of the lung [letter] Am J Surg Pathol. 1997;21:867–868. doi: 10.1097/00000478-199707000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Kitamura H, Kameda Y, Ito T, Hayashi H. Atypical adenomatous hyperplasia of the lung. Implications for the pathogenesis of peripheral lung adenocarcinoma. Am J Clin Pathol. 1999;111:610–622. doi: 10.1093/ajcp/111.5.610. [DOI] [PubMed] [Google Scholar]
- 7.Kushihashi T, Munechika H, Ri K, Kubota H, Ukisu R, Satoh S, et al. Bronchioalveolar adenoma of the lung: CT-pathologic correlation. Radiology. 1994;193:789–793. doi: 10.1148/radiology.193.3.7972826. [DOI] [PubMed] [Google Scholar]
- 8.Sone S, Takashima S, Li F, Yang Z, Honda T, Maruyama Y, et al. Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet. 1998;351:1242–1245. doi: 10.1016/S0140-6736(97)08229-9. [DOI] [PubMed] [Google Scholar]
- 9.Austin JH, Muller NL, Friedman PJ, Hansell DM, Naidich DP, Remy-Jardin M, et al. Glossary of terms for CT of the lung: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology. 1996;200:327–331. doi: 10.1148/radiology.200.2.8685321. [DOI] [PubMed] [Google Scholar]
- 10.Travis WD, Brambilla E, Juller-Hermelink HK, Harris CC. Pathology and genetics of tumours of the lung, pleura, thymus and heart. 1st ed. Lyon: IARC Press; 2004. pp. 73–75. [Google Scholar]
- 11.Kaneko M, Eguchi K, Ohmatsu H, Kakinuma R, Naruke T, Suemasu K, et al. Peripheral lung cancer: screening and detection with low-dose spiral CT versus radiography. Radiology. 1996;201:798–802. doi: 10.1148/radiology.201.3.8939234. [DOI] [PubMed] [Google Scholar]
- 12.Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, et al. Early lung cancer action project: overall design and findings from baseline screening. Lancet. 1999;354:99–105. doi: 10.1016/S0140-6736(99)06093-6. [DOI] [PubMed] [Google Scholar]
- 13.Yokose T, Doi M, Tanno K, Yamazaki K, Ochiai A. Atypical adenomatous hyperplasia of the lung in autopsy cases. Lung Cancer. 2001;33:155–161. doi: 10.1016/s0169-5002(01)00198-2. [DOI] [PubMed] [Google Scholar]
- 14.Yokose T, Ito Y, Ochiai A. High prevalence of atypical adenomatous hyperplasia of the lung in autopsy specimens from elderly patients with malignant neoplasms. Lung Cancer. 2000;29:125–130. doi: 10.1016/s0169-5002(00)00101-x. [DOI] [PubMed] [Google Scholar]
- 15.Nakahara R, Yokose T, Nagai K, Nishiwaki Y, Ochiai A. Atypical adenomatous hyperplasia of the lung: a clinicopathological study of 118 cases including cases with multiple atypical adenomatous hyperplasia. Thorax. 2001;56:302–305. doi: 10.1136/thorax.56.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takigawa N, Segawa Y, Nakata M, Saeki H, Mandai K, Kishino D, et al. Clinical investigation of atypical adenomatous hyperplasia of the lung. Lung Cancer. 1999;25:115–121. doi: 10.1016/s0169-5002(99)00055-0. [DOI] [PubMed] [Google Scholar]
- 17.Kawakami S, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y, et al. Atypical adenomatous hyperplasia of the lung: correlation between high-resolution CT findings and histopathologic features. Eur Radiol. 2001;11:811–814. doi: 10.1007/s003300000790. [DOI] [PubMed] [Google Scholar]
- 18.Ishikawa H. Pathologic/high-resolution CT correlation of focal lung lesions 5 mm or less in diameter: detection and identification by multidetector-row CT. Nippon Igaku Hoshasen Gakkai Zasshi. 2002;62:415–422. [PubMed] [Google Scholar]
- 19.Nakata M, Saeki H, Takata I, Segawa Y, Mogami H, Mandai K, et al. Focal ground-glass opacity detected by low-dose helical CT. Chest. 2002;121:1464–1467. doi: 10.1378/chest.121.5.1464. [DOI] [PubMed] [Google Scholar]
- 20.Kishi K, Homma S, Kurosaki A, Tanaka S, Matsushita H, Nakata K. Multiple atypical adenomatous hyperplasia with synchronous multiple primary bronchioloalveolar carcinomas. Intern Med. 2002;41:474–477. doi: 10.2169/internalmedicine.41.474. [DOI] [PubMed] [Google Scholar]
- 21.Kim KG, Goo JM, Kim JH, Lee HJ, Min BG, Bae KT, et al. Computer-aided diagnosis of localized ground-glass opacity in the lung at CT: initial experience. Radiology. 2005;237:657–661. doi: 10.1148/radiol.2372041461. [DOI] [PubMed] [Google Scholar]