Abstract
Purpose: This study determined the psychometric properties of a variety of anxiety measures administered to older adults receiving home care services. Design and Methods: Data were collected from 66 adults aged 65 years and older who were receiving home care services. Participants completed self-report and clinician-rated measures of anxiety and diagnostic interviews for generalized anxiety disorder (GAD). Results: Most measures demonstrated acceptable psychometric properties. All of the measures showed excellent interrater reliability to support verbal administration, which is the typical mode of assessment in home care. The ease of use for each measure (e.g., time of administration) was also evaluated. The Geriatric Anxiety Inventory (GAI) demonstrated the strongest and the Beck Anxiety Inventory the weakest psychometric properties. The GAI and the GAD screening questions from The Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire (PHQ) demonstrated the greatest utility in screening for anxiety disorders (either GAD or anxiety disorder not otherwise specified). Implications: These data support the use of anxiety measures within a geriatric home care setting. The strengths and weaknesses of each measure are discussed to facilitate selection of the optimal measure depending upon assessment goals and available resources.
Keywords: Anxiety, Home care, Assessment
Policies for elder care increasingly emphasize the importance of “aging in place,” and this has led to the expansion of community resources for home care (Marek & Rantz, 2000; Mollica, 2003). Mental health services in home care, however, are often lacking (Zeltzer & Kohn, 2006), and additional research is needed on this topic to enhance service delivery. To date, most mental health services in home care have focused on the assessment and treatment of depression (e.g., Bruce, Van Citters, & Bartels, 2005; Bruce et al., 2002), despite data suggesting that anxiety disorders are more common than depressive disorders in this setting (Préville, Côté, Boyer, & Hébert, 2004). Anxiety symptoms are also often comorbid with depression, and so-called anxious depression has been associated with more severe symptoms and impairments and poorer prognosis (Diefenbach & Goethe, 2006). Anxiety symptoms also increase the risk for suicidality among older depressed adults (Lenze et al., 2000).
The importance of assessing anxiety in recipients of home care services is highlighted further by data suggesting that anxiety is common among older disabled adults (Brenes, Guralnik, Williamson, Fried, & Penninx, 2005) and is a significant predictor of progressing disability (Brenes, Guralnik, Williamson, Fried, Simpson, et al., 2005), cognitive decline (Sinoff & Werner, 2003), and nursing home placement (Gibbons et al., 2002). Nursing home care is not only more costly, but elders in nursing homes also report higher distress and lower life satisfaction compared with community-dwelling elderly persons (Gueldner et al., 2001). Thus, recognition and treatment of anxiety among elderly people receiving home care services is particularly important to potentially reduce the risk for nursing home placement.
Research to determine optimal screening measures for late-life anxiety disorders is needed to facilitate referrals for treatment. Most of the previous research on this topic has been conducted in primary care with promising results (Stanley, Diefenbach, et al., 2003; Webb et al., 2008; Wetherell, Birchler, Ramsdell, & Unutzer, 2007). However, it is an empirical question whether the validity of these measures will translate to older adults receiving home care services. Home care not only has a unique organizational system, but patients receiving home care are also likely to present with more severe medical, functional, or cognitive disability, or all, which could affect assessment. Therefore, it is important to validate the screening and assessment measures of anxiety within the home care system. Research suggests that unstructured global assessments by home care workers are poor predictors of psychiatric disorders, including anxiety disorders (E. L. Brown, McAvay, Raue, Moses, & Bruce, 2003; Préville et al., 2004). Préville and colleagues (2004) found that administration of a standardized general distress measure improved ability to accurately detect a diagnosis of an anxiety or a depressive disorder among home care recipients. However, sensitivity of this measure was found to be in only the adequate range. Additional research is needed to explore the psychometric properties of other screening measures, which may provide improved sensitivity for detecting anxiety disorders among home care recipients.
The aim of this study was to determine the most useful screening and assessment measures for anxiety to be administered in a home care setting. A variety of general anxiety/worry and symptom-specific measures of generalized anxiety disorder (GAD) were administered. Measures of GAD were administered given that this disorder is one of the most common late-life anxiety disorders (Beekman et al., 1998). Generalized anxiety disorder is characterized by excessive and uncontrollable worry accompanied by three or more of the following hyperarousal symptoms: restlessness, fatigue, concentration problems, irritability, muscle tension, and sleep disturbance (American Psychiatric Association, 1994). Clinically significant anxiety symptoms that do not meet full diagnostic criteria for an anxiety disorder are even more common among elderly people (Carter, Wittchen, Pfister, & Kessler, 2001; Smalbrugge, Jongenelis, Pot, Beekman, & Eefsting, 2005), and GAD symptoms are the most common anxiety symptoms among older adults (Heun, Papassotiropoulos, & Ptok, 2000; Lenze et al., 2003).
In this study, we established the internal consistency, test–retest reliability, and interrater reliability of measures. Convergent, divergent, and discriminant validity also were determined. Receiver-operating characteristic (ROC) curves were used to obtain optimal cutoff scores for measures to screen for clinically significant generalized anxiety (GA; defined as meeting diagnostic criteria for GAD or subthreshold GAD, which was diagnosed as anxiety disorder not otherwise specified [NOS]). A useful measure in this setting will need to be brief and easy to administer as well as psychometrically valid. Thus, data on the ease of use of each measure (e.g., time of administration, prevalence of confusion, prevalence of difficulty) are also presented descriptively.
Methods
Participants
Participants were 66 adults (n = 55, 83.3% women) aged 65 years and older (age M = 76.64, SD = 7.04, range = 65–92) recruited through a community care management organization. Four participants (6.1%) identified their ethnicity as Hispanic/Latino. Racial distribution of the participants was 74.2% White (n = 49), 19.7% Black (n = 13), and 6.1% (n = 4) reporting multiple or other racial affiliations. The majority of participants were unemployed (e.g., retired, on disability) (n = 65, 98.5%) and either widowed or divorced/separated (n = 48, 72.8%). The sample reported an average of 11.93 years of education (SD = 2.89). Thirty-eight (57.6%) were currently prescribed psychotropic medication. The typical participant reported four chronic physical health problems (M = 3.86, SD = 1.94). The most frequently reported health problems were hypertension (n = 47, 71.2%), rheumatoid or osteoarthritis (n = 44, 66.7%), other heart disease (n = 28, 42.4%), and diabetes (n = 21, 31.8%). Descriptive information on the type and frequency of functional disability in the sample is reported in Table 1.
Table 1.
Number and Percentage of Participants (n = 66) Requiring Assistance in Activities of Daily Living and Instrumental Activities of Daily Living
| Number (%) requiring assistance | |
| Activities of daily living | |
| Bathing | 37 (56.1) |
| Stair climbing | 24 (36.4) |
| Dressing | 23 (34.8) |
| Mobility | 19 (28.8) |
| Walking | 7 (10.6) |
| Wheeling | 7 (10.6) |
| Bladder | 4 (6.1) |
| Transfer | 3 (4.5) |
| Eating/feeding | 3 (4.5) |
| Bowel | 3 (4.5) |
| Toileting | 1 (1.5) |
| Instrumental activities of daily living | |
| Housework | 53 (80.3) |
| Shopping | 51 (77.3) |
| Meal preparation or planning | 48 (72.7) |
| Travel from residence | 44 (66.7) |
| Medication administration | 33 (50.0) |
| Laundry | 29 (43.9) |
| Money management | 27 (40.9) |
| Telephoning | 1 (1.5) |
The community care management organization is a private nonprofit organization whose mission is to conduct needs and eligibility assessments, provide referrals to connect clients with needed services, and maintain ongoing coordination of home care services (e.g., meal delivery, nursing care) to allow low-income, functionally disabled older adults to continue living at home. Thus, care managers do not provide the home care services but instead develop, institute, and manage a care plan for clients. This organization is contracted with the state Department of Social Services to serve as an “access agency” to the public home care program. They also provide services for those who do not meet the state eligibility criteria in a fee-for-service program. Recruitment for this study was conducted only with those clients eligible for services paid for by the state.
Clients undergo an annual psychosocial assessment as part of the regular operating procedures of the community care management organization. Data from the most recent psychosocial assessment were used to exclude participants with substance abuse (and this criterion was confirmed during the study interview using the semistructured diagnostic assessment described subsequently), severe visual or hearing loss, inability to complete assessment without an interpreter, cognitive impairment (see description of criteria subsequently), moderate or more severe suicidality, or moderate or more severe aggressive/assaultive behavior. In addition, participants with psychosis were excluded as assessed during the study interview using the semistructured diagnostic interview described subsequently. Participants were excluded for cognitive impairment if they received a score of 8 or below on the Mental Status Questionnaire (Pfeiffer, 1975) in the psychosocial assessment database or a score of 20 or below on the Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975) administered during the study assessment.
Participants were initially selected using a stratified random sampling procedure to obtain 50% of participants who screened positive for anxiety (i.e., rated as having moderate or severe problem with anxiety/worry by care managers in the psychosocial assessment) and 50% who screened negative for anxiety. To obtain an adequate sample of participants with anxiety disorders, however, this procedure was changed to oversample those who screened positive for anxiety. The final sample consisted of 55% who screened positive and 45% who screened negative for anxiety.
Two hundred fifty clients were invited by staff of the care management organization to participate. Of these, 175 declined participation. The most common reason for declining was “health problems,” reported by 20.6% of declining participants (n = 36). Another common reason for declining was belief that the interview would be upsetting or stressful, or that the information would not be kept confidential (n = 21, 12%). Twenty-eight (16%) of declining participants did not give a reason, and the remaining participants gave varied other reasons for declining, such as family advising against participation or feeling that the study would take too much time (all remaining reasons reported by ≤5% of participants). The participants who declined did not differ from those who agreed to participate on age, ethnicity, or race. A significantly higher proportion of participants who screened positive for anxiety (n = 120, 74.5%) than those who screened negative for anxiety (n = 53, 60.9%) declined participation, χ2(1, N = 248) = 4.96, p < .05 (data on anxiety screening status were unavailable for two participants). Given that no other data were collected from declining participants, we were unable to compare those who agreed and declined on any other demographic or clinical variables. Of the 75 participants who enrolled in the study, two were excluded (both due to psychosis), and an additional seven discontinued the study prior to completing all study measures. One participant discontinued due to the length of the interview, one due to fatigue, and the remaining five did not provide a reason. Participants who completed the study did not differ from those who discontinued on any demographic variable. Data from the remaining 66 participants are presented here.
Measures
Anxiety Disorder Interview Schedule for DSM-IV.—
The GAD, major depressive disorder (MDD), substance abuse, and psychosis sections of the Anxiety Disorders Interview Schedule (ADIS-IV; T. A. Brown, DiNardo, & Barlow, 1994) for the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), were administered. Only these sections were administered to all participants to reduce participant burden. Supplemental sections of the ADIS-IV were administered on a case-by-case basis if core features of other anxiety disorders (e.g., the presence of panic attacks, history of trauma, identification of an acute stressor at onset of symptoms) were identified during the assessment. A random sample of 16 audiotaped interviews (24% of included participants) was rated by a second interviewer for interrater reliability. Interrater agreement was good for anxiety disorder diagnosis (Κ = .846). Specifically, interrater agreement was good for diagnosis of GAD (Κ = .818), and there was perfect agreement for diagnosis of all other anxiety disorders (Κ = 1.0). There was also perfect agreement for diagnosis of depressive disorders (Κ = 1.0).
Generalized Anxiety Disorder Questionnaire for DSM-IV.—
The Generalized Anxiety Disorder Questionnaire for the DSM-IV (GADQ-IV) is a self-report measure designed to screen for DSM-IV–defined GAD (Newman et al., 2002). In the current study, participants completed all items; however, scoring was computed using the discontinue rule suggested by the developers of the scale (Newman et al., 2002; psychometric properties were similar for the GADQ-IV scoring with and without using the discontinue rule. Thus, only the scoring as proposed by the scale’s developers using the discontinue rule is reported here). The GADQ-IV demonstrates good test–retest reliability, convergent and divergent validity, and good sensitivity and specificity for classification of younger adults with GAD using a cutoff score of 5.7 (Newman et al., 2002). The GADQ-IV demonstrated less utility as a screening measure for older primary care patients with GAD using an optimal cutoff score of 4.5 (Webb et al., 2008).
Penn State Worry Questionnaire.—
The Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990) is the most widely used self-report measure of trait worry and demonstrates good internal consistency and superior convergent validity relative to other anxiety self-report measures among older adults (J. G. Beck, Stanley, & Zebb, 1995; Stanley, Novy, Bourland, Beck, & Averill, 2001). Sixteen items are rated on a 5-point scale from 1 = not at all typical to 5 = very typical. Five items are reverse scored. An abbreviated version of the PSWQ (PSWQ-A) has demonstrated psychometric properties comparable to the full version (Hopko et al., 2003). Good sensitivity and specificity have been found in identifying GAD among older primary care patients using the PSWQ and PSWQ-A (Stanley, Diefenbach, et al., 2003). These results were replicated in a second sample of older primary care patients with GAD, although with lower classification accuracy (Webb et al., 2008). In the current study, the full PSWQ was administered, and both the full-scale and abbreviated scoring of the PSWQ were calculated for data analyses.
Patient Health Questionnaire GAD Screening Questions.—
The Primary Care Evaluation of Mental Disorders (PRIME-MD) is a diagnostic interview developed for use in medical settings, which includes screening questions for mental disorders on a self-report Patient Health Questionnaire (PHQ) (Spitzer et al., 1994). There are two GAD screening questions on the PHQ which use a yes/no answer format and query whether the patient has been bothered by “nerves or feeling anxious or on edge” or “worried about a lot of different things” during the past month. The PRIME-MD has good concordance with the Structured Clinical Interview for DSM disorders (Kobak et al., 1997), and the PHQ screening questions have been used successfully to recruit older adults with GAD in previous research (Stanley, Hopko, et al., 2003).
Generalized Anxiety Disorder Severity Scale.—
The Generalized Anxiety Disorder Severity Scale (GADSS; Shear, Belnap, Mazumdar, Houck, & Rollman, 2006) is a clinician-rated measure of GAD severity. The GADSS demonstrates high internal consistency and good validity and sensitivity to change among mixed-age primary care patients (Shear et al.). The GADSS demonstrated acceptable internal consistency, excellent interrater reliability, good convergent validity, poor divergent validity, and poor utility in classifying older patients with and without GAD (Weiss et al., 2009).
The Beck Anxiety Inventory.—
The Beck Anxiety Inventory (BAI) is a widely used symptom measure of anxiety (A. T. Beck, Epstein, Brown, & Steer, 1988) and has established psychometric properties in diverse samples of older adults (e.g., Kabacoff, Segal, Hersen, & Van Hasselt, 1997; Steer, Willman, Kay, & Beck, 1994), including older adults with GAD (Stanley et al., 2001; Wetherell & Gatz, 2005). The BAI includes 21 items that reflect affective (e.g., “terrified,” “nervous,” “fear the worst happening”) and somatic (e.g., “heart pounding or racing,” “difficulty breathing”) symptoms of anxiety rated on a 4-point scale for how much the individual is bothered by these symptoms during the past week: 0 = not at all to 3 = severely.
The Brief Measure of Worry Severity.—
The Brief Measure of Worry Severity (BMWS; Gladstone et al., 2005) is an eight-item measure assessing several aspects of pathological worry (e.g., impairment/distress, uncontrollability, associated negative affect). Items are rated from 0 = not at all true to 3 = definitely true. The BMWS demonstrated excellent internal consistency, good convergent validity, and good discriminant validity (Gladstone et al., 2005). No data on the BMWS among older adults are yet available.
The Geriatric Anxiety Inventory.—
The Geriatric Anxiety Inventory (GAI; Pachana et al., 2007) is a 20-item self-report measure constructed specifically for use with older adults. The GAI uses an agree/disagree response choice format, with the number of agree responses added for a total score. Internal consistency was excellent, and there was good convergent validity and good discriminant validity for patients with and without anxiety disorders (Pachana et al., 2007). An ROC analysis indicated that a cutoff score of 10/11 correctly classified 83% of patients with GAD (74% sensitivity and 84% specificity). The GAI was added midway through data collection in this study; thus, data on the GAI were available on only a subset of the current sample (n = 35).
The Geriatric Worry Scale.—
The geriatric worry scale (GWS) was constructed by the first and second authors for the current study to assess anxiety among older adults. The format of the GWS was modeled after the Geriatric Depression Scale (GDS) using a yes/no response choice and simple concrete language. Five items were included on the scale: “Do you feel worried much of the time?”, “Do you have a problem with nerves?”, “Are you a worrier?”, “Do other people say you worry too much?”, “Are you worried about the future?”, and “Do you feel relaxed most of the time?” Positive responses are given 1 point (except for the last item, which is reverse scored) and added for a total score.
Geriatric Depression Scale.—
The GDS (Yesavage et al., 1983) is a commonly used self-report measure of depressive symptoms among geriatric patients and has demonstrated adequate psychometric properties for use with older adults (Sheikh & Yesavage, 1986; Snyder, Stanley, Novy, Averill, & Beck, 2000; Yesavage, 1988). The GDS demonstrates good divergent validity with measures of anxiety among older adults (Snyder et al., 2000).
Ease of Use Assessment
Data were also collected on the ease of use of each measure. The amount of time for administration was recorded and rounded up to the nearest minute. Participants rated their degree of confusion and difficulty experienced while completing the measures on a 5-point Likert scale from 0 = not at all to 4 = extremely. Interviewers also independently rated the degree of confusion displayed by participants (e.g., choosing numerical values as response choices, which were inconsistent with their verbal descriptions of their response) on a 5-point Likert scale from 0 = not at all to 4 = extremely.
Procedure
Recruited participants gave written informed consent for study participation. Study assessments were completed in participants’ homes by either a licensed clinical psychologist or a postdoctoral fellow under supervision of a licensed clinical psychologist. The ADIS-IV was completed first (the sections were administered in randomized order), followed by the MMSE, and then the self-report measures (administered in a randomized order). The diagnostic interviews were completed first to reduce biasing diagnostic judgments by learning of answers and scores to the self-report measures. Data from the ADIS-IV were presented at a clinical staff meeting with at least two licensed psychologists present where a final diagnostic judgment was made. Self-report questionnaires were administered verbally based upon feedback from the care management organization that this mode of administration would be less burdensome and more typical of real-world assessments in this setting. Participants were provided with large-print visual scales to refer to when making response choices. Similar methodology has been used in previous research with older community-dwelling elderly persons (Nuevo, Montorio, & Borkovec, 2004). In addition, recent research supports the validity of verbal administration of self-report measures to elderly persons, at least when paper copies of measures are provided for review (Senior et al., 2007). A random sample of 16 audiotaped interviews (24% of included participants) was rated by a second interviewer for interrater reliability. A second random sample of participants (n = 16, 24%) completed study measures a second time to assess test–retest reliability. The intervening time period for test–retest was approximately 1–2 weeks (M = 9.69, SD = 2.85, range = 7–16 days).
All participants were provided with verbal feedback about assessment results; psychoeducational materials (i.e., an informational brochure about anxiety); and a community resource list for mental health services. Participants who were diagnosed either with an anxiety or with a mood disorder, scored above previously determined cutoff scores for anxiety or depression screening measures, or evidenced any other symptom indicating a mental health problem were encouraged to discuss their symptoms with their physicians and to seek mental health care services. In addition, a written assessment summary was provided to participants’ care managers and medical doctors with written consent. Of the 75 participants who completed at least part of the assessment, 71 (94.7%) provided written consent for a report to be sent to their care manager or medical doctor, or both. No additional information of the impact of this report on patient care is available.
Results
Diagnoses
Seventeen participants were diagnosed with either GAD (n = 10, 15.2%) or anxiety disorder NOS (n = 7, 10.6%). Participants diagnosed with anxiety disorder NOS were those who reported clinically significant GAD symptoms but failed to meet full diagnostic criteria. Reasons for failing to meet GAD diagnostic criteria included one or more of the following: denied uncontrollable worry (n = 5), failed to reach associated physical symptoms criterion (n = 3), or denied worry more days than not (n = 2). Those with GAD and anxiety disorder NOS did not differ significantly on demographic variables, with the exception that those with GAD reported significantly fewer years of education (M = 10.90, SD = 2.69) than did those with anxiety disorder NOS (M = 14.14, SD = 2.61), t(15) = 2.48, p < .05. In addition, research suggests that current definitions of GAD may be overly restrictive and exclude a sizable number of individuals with clinically significant GA who display similar clinical correlates as those with fully defined DSM-IV GAD (Ruscio et al., 2007). Thus, participants with GAD and anxiety disorder NOS were combined into a single GA group for comparison with the control group and for ROC curve analyses. Comorbid anxiety and depressive disorders in the GA group were MDD and MDD in partial remission (n = 3, 17.6%), depressive disorder NOS (n = 3, 17.6%), panic disorder with agoraphobia (n = 1, 5.9%), and posttraumatic stress disorder (n = 1, 5.9%).
Of the remaining 49 participants, 6 (12.2%) were diagnosed with other anxiety or depressive disorders: one with panic disorder with agoraphobia, one with MDD in partial remission, and four with depressive disorder NOS. The control group consisted of the remaining 43 participants who did not meet diagnostic criteria for any anxiety or depressive disorder diagnoses.
Descriptive Statistics and Reliability Analyses
Table 2 shows score means and standard deviations for the entire sample. Data on reliability including internal consistency (Cronbach’s alpha), interrater agreement (Pearson’s r), and test–retest reliability (Pearson’s r) are also reported in Table 2. Internal consistency for the measures ranged from fair to excellent. Interrater agreement was excellent across all measures. Given that the interrater agreement was calculated on a small subset of participants, 95% confidence intervals (CIs) were also calculated. Results showed that all confidence intervals were small and all estimates were in the excellent range (i.e., ≥.900) with the exception of the GADSS (95% CI = .878–.985). Test–retest reliability ranged from poor to excellent. Again, 95% CIs were calculated, and these are reported in Table 2. The large CIs for test–retest likely reflect a lack of precision in the reliability coefficients due to small sample size.
Table 2.
Descriptive Statistics, Internal Consistency, Interrater Reliability, and Test–Retest Reliability
| Measure | M (SD) | α | Interrater r | Test–retest r (95% confidence interval) |
| GADQ-IV | 3.47 (3.69) | .858 | .992 | .481 (−.019 to .788) |
| PSWQ | 41.59 (11.10) | .794 | .999 | .788 (.480 to .923) |
| PSWQ-A | 18.81 (8.43) | .887 | 1.00 | .760 (.425 to .912) |
| BAI | 11.56 (11.13) | .918 | .982 | .638 (.209 to .861) |
| BMWS | 7.23 (6.90) | .926 | .994 | .527 (.043 to .810) |
| GADSS | 6.38 (5.35) | .903 | .957 | .921 (.783 to .972) |
| GWS | 1.84 (1.89) | .778 | 1.00 | .855 (.624 to .948) |
| GAI | 4.63 (5.57) | .934 | 1.00 | .952 (−.106 to 1.00) |
Notes: GADQ-IV = Generalized Anxiety Disorder Questionnaire for DSM-IV; PSWQ = Penn State Worry Questionnaire; PSWQ-A = Penn State Worry Questionnaire Abbreviated Version; BAI = Beck Anxiety Inventory; BMWS = Brief Measure of Worry Severity; GADSS = Generalized Anxiety Disorder Severity Scale; GWS = geriatric worry scale; GAI = Geriatric Anxiety Inventory. Sample size for mean, standard deviation, and alpha for measures is n = 66, with the exception of the GAI, which is n = 35. Sample size for test–retest reliability is n = 16, with the exception of the GAI, which is n = 4. Sample size for interrater reliability is n = 16, with the exception of the GAI, which is n = 7.
Group Comparisons
Table 3 shows descriptive statistics and independent samples t-test results comparing the participant groups on study measures. (Results were similar when comparing patients diagnosed with GAD only [n = 10] with the control group [n = 43].) Levene’s test for equality of variances was significant (p < .05) for the BAI, BMWS, GADSS, and GWS; thus, corrected t-test values that did not assume equal variances are presented for these measures. Participants in the GA group scored significantly higher than did participants in the control group on all measures, with the exception of the BAI. Between-group effect sizes (Cohen’s d) are also displayed in Table 3. The effect size difference between the groups was large for all measures, except the BAI, which showed a moderate effect size.
Table 3.
Comparison of Participants With and Without Generalized Anxiety on Study Measures
| Measure | Generalized anxiety group M (SD) | Control group M (SD) | t(58) | Cohen's d |
| GADQ-IV | 7.10 (3.17) | 1.87 (2.87) | 6.17* | 1.73 |
| PSWQ | 51.53 (11.43) | 37.28 (8.16) | 5.42* | 1.43 |
| PSWQ-A | 26.47 (7.32) | 15.60 (7.08) | 5.31* | 1.51 |
| BAI | 16.00 (14.94) | 9.30 (8.69) | 1.74 | 0.55 |
| BMWS | 13.63 (7.16) | 4.70 (5.46) | 4.64* | 1.40 |
| GADSS | 12.29 (5.53) | 3.90 (3.34) | 5.84* | 1.84 |
| GWS | 4.00 (1.94) | 1.05 (1.19) | 5.87* | 1.83 |
| GAI | 12.25 (5.80) | 2.00 (2.60) | 6.76* | 2.28 |
Notes: GADQ-IV = Generalized Anxiety Disorder Questionnaire for DSM-IV; PSWQ = Penn State Worry Questionnaire; PSWQ-A = Penn State Worry Questionnaire Abbreviated Version; BAI = Beck Anxiety Inventory; BMWS = Brief Measure of Worry Severity; GADSS = Generalized Anxiety Disorder Severity Scale; GWS = geriatric worry scale; GAI = Geriatric Anxiety Inventory. n = 17 for the generalized anxiety group and n = 43 for the control group for all measures except the GAI. n = 8 for the generalized anxiety group and n = 22 for the control group for the GAI. df = 28 for the GAI.
*p < .001.
Convergent and Divergent Validity
Anxiety measure intercorrelations are shown in Table 4. Convergent validity ranged from poor to good. The GAI (r range = .613–.862) demonstrated the strongest convergent validity, whereas the BAI demonstrated the weakest (r range = .290–.613). Divergent validity was explored by correlating study measures with the GDS. The PSWQ demonstrated the strongest (r = .395) and the GAI the weakest (r = .793) divergent validity. There was moderate correlation between the GDS and the GADSS (r = .638), BAI (r = .629), GADQ-IV (r = .601), BMWS (r = .591), GWS (r = .551), and PSWQ-A (r = .439).
Table 4.
Convergent Validity of Study Measures
| GADQ-IV | PSWQ | PSWQ-A | BAI | BMWS | GADSS | GWS | GAI | |
| GADQ-IV | — | |||||||
| PSWQ | .628** | — | ||||||
| PSWQ-A | .656** | .874** | — | |||||
| BAI | .383* | .290 | .320* | — | ||||
| BMWS | .728** | .645** | .735** | .509** | — | |||
| GADSS | .668** | .538** | .559** | .544** | .636** | — | ||
| GWS | .674** | .674** | .667** | .501** | .728** | .703** | — | |
| GAI | .653** | .794** | .795** | .613** | .777** | .838** | .862** | — |
Notes: GADQ-IV = Generalized Anxiety Disorder Questionnaire for DSM-IV; PSWQ = Penn State Worry Questionnaire; PSWQ-A = Penn State Worry Questionnaire Abbreviated Version; BAI = Beck Anxiety Inventory; BMWS = Brief Measure of Worry Severity; GADSS = Generalized Anxiety Disorder Severity Scale; GWS = geriatric worry scale; GAI = Geriatric Anxiety Inventory. Sample size for measures is n = 66, with the exception of the GAI, which is n = 35.
*p < .01. **p < .001.
ROC Curve Analyses
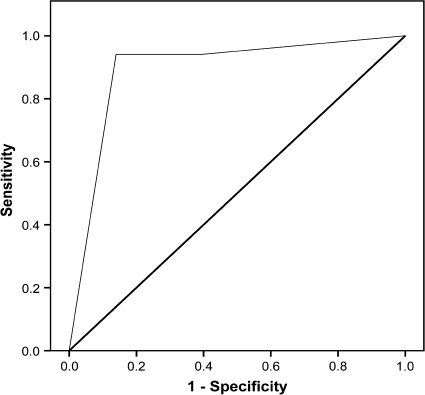
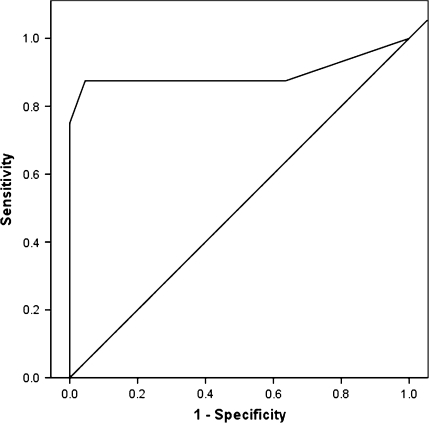
We computed ROC curves and identified optimal cutoff scores maximizing the balance between sensitivity and specificity. Table 5 shows the area under the curve (AUC), optimal cutoff scores, sensitivity (the percentage of participants correctly identified with GAD or anxiety disorder NOS, also called true positives), specificity (the percentage of participants correctly identified without GAD or anxiety disorder NOS, also called true negatives), positive predictive value (PPV; the proportion of participants scoring above the cutoff who were correctly classified with GAD or anxiety disorder NOS, also called precision rate), negative predictive value (NPV; the proportion of participants scoring below the cutoff who were correctly classified without GAD or anxiety disorder NOS), and efficiency (the proportion of cases correctly classified, also called diagnostic accuracy) for each measure. (ROC curves to differentiate patients diagnosed with GAD from those with no diagnoses resulted in superior classification for nearly all measures [with the exception of the BAI] and slightly higher cutoff scores for the BAI [optimal cutoff score = 9], GADSS [optimal cutoff score = 9], GWS [optimal cutoff score = 4], and GAI [optimal cutoff score = 11]. However, only the full results to differentiate the combined GAD–anxiety disorder NOS group from those with no diagnosis is reported here, given that clients identified with clinically significant levels of anxiety, whether these symptoms meet full diagnostic criteria for GAD, would benefit from additional evaluation and treatment. Thus, we are reporting full results from the combined GAD–anxiety disorder NOS group to increase the generalizability and usefulness of these data for practitioners.) The AUC defines how accurately a test predicts diagnostic classification, with an area of 1 representing a perfect test and an area of .5 representing a random test. Overall, the PHQ and GAI demonstrated the most promise as screening measures. The PHQ demonstrated the best sensitivity and NPV. The GAI demonstrated the best specificity, PPV, and efficiency. The ROC curves for the PRIME-MD screener and GAI are presented in Figures 1 and 2, respectively.
Table 5.
Results From Receiver-Operating Characteristic Curves Analyses
| Measure | Area under the curve | Optimal cutoff score | Sensitivity | Specificity | PPV | NPV | Efficiency |
| GADQ-IV | .898 | 4.67 | .824 | .884 | .737 | .927 | .867 |
| PSWQ | .860 | 42 | .824 | .791 | .609 | .919 | .800 |
| PSWQ-A | .861 | 23 | .763 | .860 | .684 | .902 | .833 |
| BAI | .629 | 7 | .765 | .488 | .371 | .840 | .567 |
| BMWS | .834 | 8 | .824 | .791 | .609 | .919 | .800 |
| GADSS | .915 | 7 | .882 | .814 | .652 | .946 | .833 |
| GWS | .886 | 2 | .882 | .744 | .577 | .941 | .783 |
| PHQ | .893 | 2 | .941 | .860 | .727 | .974 | .883 |
| GAI | .895 | 9 | .875 | .955 | .875 | .955 | .933 |
Notes: GADQ-IV = Generalized Anxiety Disorder Questionnaire for DSM-IV; PSWQ = Penn State Worry Questionnaire; PSWQ-A = Penn State Worry Questionnaire Abbreviated Version; BAI = Beck Anxiety Inventory; BMWS = Brief Measure of Worry Severity; GADSS = Generalized Anxiety Disorder Severity Scale; GWS = geriatric worry scale; PHQ = Patient Health Questionnaire GAD screening questions; GAI = Geriatric Anxiety Inventory; PPV = positive predictive value; NPV = negative predictive value. n = 17 for the anxiety group and n = 43 for the control group for all measures except the GAI. n = 8 for the anxiety group and n = 22 for the control group for the GAI.
Figure 1.
Receiver-operating characteristic curve for the GAD screening questions on the Patient Health Questionnaire.
Figure 2.
Receiver-operating characteristic curve for the Geriatric Anxiety Inventory.
Ease of Use
Average measure administration time ranged from approximately 1 to just under 7 min (see Table 6). Table 6 shows the frequency count of participants and clinicians reporting moderate or greater problems with confusion or difficulty for each measure. Visual inspection indicates that most measures were associated, with only a few participants (≤6%) reporting moderate or more severe problems with confusion and difficulty. Two notable exceptions were the PSWQ and the GADQ-IV. The GAI was associated with the least frequently reported problems with confusion and difficulty.
Table 6.
Ease of Use Assessment for Anxiety Measures
| Measure | Time to administer, in minutes | Participants reporting ≥ moderate confusion, n (%) | Participants reporting ≥ moderate difficulty, n (%) | Clinician rating participants with ≥ moderate confusion, n (%) |
| GADQ-IV | 4.18 (2.07) | 3 (5) | 8 (12) | 6 (9) |
| PSWQ | 4.34 (2.34) | 10 (15) | 8 (12) | 28 (42) |
| BAI | 2.91 (1.41) | 2 (3) | 3 (5) | 2 (3) |
| BMWS | 1.95 (0.99) | 2 (3) | 4 (6) | 3 (5) |
| GADSS | 6.76 (3.66) | 4 (6) | 2 (3) | 4 (6) |
| GWS | 1.17 (0.67) | 2 (3) | 2 (3) | 0 (0) |
| PHQ | 1.02 (0.12) | 3 (5) | 3 (5) | 2 (3) |
| GAI | 2.85 (1.30) | 0 (0) | 2 (3) | 0 (0) |
Notes: GADQ-IV = Generalized Anxiety Disorder Questionnaire for DSM-IV; PSWQ = Penn State Worry Questionnaire; PSWQ-A = Penn State Worry Questionnaire Abbreviated Version; BAI = Beck Anxiety Inventory; BMWS = Brief Measure of Worry Severity; GADSS = Generalized Anxiety Disorder Severity Scale; GWS = geriatric worry scale; PHQ = Patient Health Questionnaire GAD screening questions; GAI = Geriatric Anxiety Inventory.
Discussion
Results support the use of anxiety assessment measures when administered to older adults in home care. Notably, all the measures showed excellent interrater reliability to support verbal administration, which is the typical mode of assessment in home care. In addition, most measures demonstrated other acceptable psychometric properties. The choice of the optimal measure to use, however, will depend largely upon the goals of the assessment.
The GADSS and the GADQ-IV would be the most appropriate measures for an assessment of the presence and severity of GAD diagnostic symptoms. The psychometric properties of these measures were roughly similar, with the exception of poor test–retest reliability for the GADQ-IV. In addition, the utility of the GADQ-IV may be limited by wording and format that is confusing or difficult. The scoring of the GADQ-IV is also not user friendly and thus may be less suitable for integrating into a home care setting. The GADSS showed good psychometric properties in the current study, and these were superior to those found among older primary care patients (Weiss et al., unpublished manuscript). The feasibility of the GADSS in home care may be limited, however, because it is a semistructured clinician-rated severity scale, which may require more training in administration than is needed for administration of self-report measures.
To assess trait worry symptoms, the PSWQ and BMWS would be most appropriate. Given that these measures showed similar patterns of psychometric support, the choice of the measure may be based upon ease of use. The PSWQ took longer to administer and was relatively more confusing and difficult for patients to complete. These data are consistent with factor analytic research, which demonstrates a unique factor for reverse-scored items (e.g., J. G. Beck et al., 1995). Ad hoc review indicated that the reverse-scored items were the most common reason for causing confusion. Unfortunately, data on the ease of use were not obtained for the abbreviated PSWQ. Nevertheless, it is recommended that the abbreviated version (Hopko et al., 2003) of the PSWQ be used in place of the original version to reduce the administration time and confusion related to reverse-scored items.
The GAI and GWS were two of the newer measures constructed specifically for use with older adults. Both measures assess a range of general cognitive and affective anxiety symptoms. The GWS demonstrated acceptable psychometric properties and thus may be a promising measure for late-life anxiety assessment. The GAI received stronger psychometric support with excellent reliability and strong convergent validity and high utility in classification of patients with and without GA. However, the GAI also displayed poor divergent validity with a self-report measure of depression.
The goal of identifying patients with clinically significant GA (i.e., those diagnosed with GAD or anxiety disorder NOS) is necessary to make appropriate treatment referrals. Both the PHQ and the GAI displayed high utility as screening measures and showed good balance of sensitivity and specificity. Specifically, the PHQ displayed stronger sensitivity and weaker specificity than the GAI; however, this may be an appropriate trade-off when using the measure for screening purposes. The PHQ may also be more feasible for home care use given the brevity of the measures (2 items on the PHQ vs. 20 items on the GAI).
Of all the measures, the only one to show inadequate psychometric support was the BAI. Although the BAI showed excellent internal consistency and interrater agreement, test–retest reliability was only in the moderate range. Convergent validity was generally poor, and the BAI was unable to distinguish between participants with and without GA. This is likely due to the high comorbidity of health complaints among older adults in home care and confounding of somatic symptoms on the BAI (e.g., Wetherell & Gatz, 2005).
Taken together, these results show that the GAI demonstrates significant promise as a screening and assessment measure of late-life GA. However, conclusions about the GAI are also the most tentative owing to a smaller sample completing the measure and problems with divergent validity. Anxiety and depression are highly comorbid among older adults (Beekman et al., 2000) and are especially difficult to distinguish in this cohort (Parmelee, Katz, & Lawton, 1993). Unfortunately, the rates of depression diagnosis were too limited to address the issue of divergent validity further in the current study. It is recommended that additional research be conducted to validate the GAI with respect to differentiation of anxiety and depression. The length of the GAI could also present a feasibility concern in a home care setting. Thus, it is also recommended that future research determine whether an abbreviated version of the GAI can be administered with comparable psychometric properties.
Results need to be interpreted within several study limitations. Participants did not complete comprehensive diagnostic assessments. Thus, the degree of psychiatric comorbidity and any impact of this comorbidity on the utility of assessments could not be determined. In addition, diagnostic interviews were completed prior to other assessments. This study design was used to reduce biasing of diagnostic judgments by the interviewer learning of scores on assessment measures. Nevertheless, this design also creates the possibility of order effects and bias from the diagnostic interviews influencing the participant’s responses on later assessments. Another major limitation of the study was the substantial refusal rate for participation. Participants who refused did not differ from those who completed assessments on basic demographic characteristics. However, the refusal rate was higher for those participants who screened positive for anxiety, and it is unknown whether there were other systematic differences between those who refused and those who participated that were not assessed. Although this study included a wide range of assessment measures, this investigation was not exhaustive. For example, the Hospital Anxiety and Depression Scale was a useful screening measure for older adults with GAD in primary care (Wetherell et al., 2007) and may prove to be so in future research with older adults in home care. Participants were classified with clinically significant GA (i.e., diagnosis of GAD or anxiety disorder NOS) rather than strictly defined GAD. There is substantial debate regarding the validity of GAD criteria (Ruscio et al., 2007), and this is perhaps especially true among older adults, where diagnosis is generally more challenging (Jeste, Blazer, & First, 2005). Thus, although this strategy may be a limitation for informing assessment of DSM-IV–defined GAD, this broader categorization strategy likely increases the generalizability and relevance of the findings for a geriatric home care setting.
Screening for anxiety will be most clinically relevant when the process is integrated into the regular operating procedures of the home care system and translates into improved care. There are several system and client barriers to achieving these goals, such as time constraints, training of home care personnel in mental health assessment and availability and client acceptability of mental health services. Data have suggested success with programs designed to train home care nurses to improve the recognition and referral of clients with depression (Bruce et al., 2007). It may be beneficial to institute similar programs for anxiety in the future. Data from the current study can be used to inform the selection of anxiety screening measures in home care. For example, information on psychometric properties, time of administration, and discussion about level of training needed (e.g., the GADSS is a clinician-rated scale requiring higher levels of training to administer than the self-report measures) can assist with deciding which measure is most feasible in this setting.
However, other barriers to service delivery not addressed in the article include availability of referral sources for specialty mental health services and whether clients would be accepting of such referrals. Additional challenges of integrating empirically supported mental health treatments into home care have been outlined elsewhere (Bruce et al., 2005). Despite these challenges, accumulating research has demonstrated promising results for improving care by integrating empirically supported treatments for depression within home care systems (Gellis, McGinty, Horowitz, & Bruce, 2007; Quijano et al., 2007). Very little data are available on integrating empirically supported treatment for anxiety into home care, and again many challenges are noted (Diefenbach, Tolin, Gilliam, & Meunier, 2008). It will be important for future research to resolve these challenges to improve the care of older home care recipients with anxiety. Nevertheless, the first step to successful intervention is identifying patients in need of services. The data reported in the current study provide valuable information to inform programs designed to screen for anxiety in home care.
Funding
This research was supported by grant R03 MH071575 from the National Institute of Mental Health to the first author.
Acknowledgments
We express our appreciation to the staff of Connecticut Community Care Inc. for supporting our research and conducting the participant recruitment for the current study. We also thank Marisa Edelberg for providing administrative support and assistance with data entry. We also acknowledge Melinda Stanley and Julie Robison for serving as study consultants.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck JG, Stanley MA, Zebb BJ. Psychometric properties of the Penn State Worry Questionnaire in older adults. Journal of Clinical Geropsychology. 1995;1:33–42. [Google Scholar]
- Beekman ATF, Bremmer MA, Deeg DJH, van Balkom AJLM, Smit JH, de Beurs E, et al. Anxiety disorders in later life: A report from the longitudinal aging study Amsterdam. International Journal of Geriatric Psychiatry. 1998;13:717–726. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Beekman ATF, de Beurs E, van Balkom AJLM, Deeg DJH, van Dyck R, van Tilburg W. Anxiety and depression in later life: Co-occurrence and communality of risk factors. American Journal of Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- Brenes GA, Guralnik JM, Williamson J, Fried LP, Penninx B. Correlates of anxiety symptoms in physically disabled older women. American Journal of Geriatric Psychiatry. 2005;13:15–22. doi: 10.1176/appi.ajgp.13.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes GA, Guralnik JM, Williamson J, Fried LP, Simpson C, Simonsick EM, et al. The influence of anxiety on the progression of disability. Journal of American Geriatrics Society. 2005;53:34–39. doi: 10.1111/j.1532-5415.2005.53007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EL, McAvay G, Raue PJ, Moses S, Bruce ML. Recognition of depression among elderly recipients of Home Care Services. Psychiatric Services. 2003;54:208–213. doi: 10.1176/appi.ps.54.2.208. [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. San Antonio, TX: Psychological Corporation; 1994. [Google Scholar]
- Bruce ML, Brown EL, Raue PJ, Mlodzianowski AE, Meyers BS, Leon AC, et al. A randomized trial of depression assessment intervention in home health care. Journal of the American Geriatrics Society. 2007;55:1793–1800. doi: 10.1111/j.1532-5415.2007.01419.x. [DOI] [PubMed] [Google Scholar]
- Bruce ML, McAvay GJ, Raue PJ, Brown EL, Meyers BS, Keohane DJ, et al. Major depression in elderly home health care patients. American Journal of Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- Bruce ML, Van Citters AD, Bartels SJ. Evidenced-based mental health services for home and community. Psychiatric Clinics of North America. 2005;28:1039–1060. doi: 10.1016/j.psc.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Carter RM, Wittchen HU, Pfister H, Kessler RC. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depression and Anxiety. 2001;13:78–88. doi: 10.1002/da.1020. [DOI] [PubMed] [Google Scholar]
- Diefenbach GJ, Goethe J. Clinical interventions for late-life anxious depression. Clinical Interventions in Aging. 2006;1:41–50. doi: 10.2147/ciia.2006.1.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diefenbach GJ, Tolin DF, Gilliam CM, Meunier SA. Extending cognitive-behavioral therapy for late-life anxiety to home care: Program development and case examples. Behavior Modification. 2008; 32:595–610. doi: 10.1177/0145445508314269. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for clinicians. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gellis ZD, McGinty J, Horowitz A, Bruce ML. Problem-solving therapy for late-life depression in home care: A randomized field trial. American Journal of Geriatric Psychiatry. 2007;15:968–978. doi: 10.1097/JGP.0b013e3180cc2bd7. [DOI] [PubMed] [Google Scholar]
- Gibbons LE, Teri L, Logsdon R, McCurry SM, Kukull W, Bowen J, et al. Anxiety symptoms as predictors of nursing home placement in patients with Alzheimer's disease. Journal of Clinical Geropsychology. 2002;8:335–342. [Google Scholar]
- Gladstone GL, Parker GB, Mitchell PB, Malhi GS, Wilhelm KA, Austin M. A brief measure of worry severity (BMWS): Personality and clinical correlates of severe worriers. Journal of Anxiety Disorders. 2005;19:877–892. doi: 10.1016/j.janxdis.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Gueldner SH, Loeb S, Morris D, Penrod J, Bramlett M, Johnson L, et al. A comparison of life satisfaction and mood in nursing home residents and community-dwelling elders. Archives of Psychiatric Nursing. 2001;15:232–240. doi: 10.1053/apnu.2001.27020. [DOI] [PubMed] [Google Scholar]
- Heun R, Papassotiropoulos A, Ptok U. Subthreshold depressive and anxiety disorders in the elderly. European Psychiatry. 2000;15:173–182. doi: 10.1016/s0924-9338(00)00228-5. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Stanley MA, Reas DL, Wetherell JL, Beck JG, Novy DM, et al. Assessing worry in older adults: Confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychological Assessment. 2003;15:173–183. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Blazer D, First MB. Aging-related diagnostic variations: Need for diagnostic criteria appropriate for elderly psychiatric patients. Biological Psychiatry. 2005;58:265–271. doi: 10.1016/j.biopsych.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Kabacoff RI, Segal DL, Hersen M, Van Hasselt VB. Psychometric properties and diagnostic utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with older adult psychiatric outpatients. Journal of Anxiety Disorders. 1997;11:33–47. doi: 10.1016/s0887-6185(96)00033-3. [DOI] [PubMed] [Google Scholar]
- Kobak KA, Taylor LVH, Dottl SL, Greist JH, Jefferson JW, Burroughs D, et al. Computerized screening for psychiatric disorders in an outpatient community mental health clinic. Psychiatric Services. 1997;48:1048–1057. doi: 10.1176/ps.48.8.1048. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Dew MA, Shear MK, Houck P, Pollock BG, et al. Good treatment outcomes in late-life depression with comorbid anxiety. Journal of Affective Disorders. 2003;77:247–254. doi: 10.1016/s0165-0327(02)00177-5. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, Begley AE, et al. Comorbid anxiety disorders in depressed elderly patients. American Journal of Psychiatry. 2000;157:722–728. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- Marek KD, Rantz MJ. Aging in place: A new model for long-term care. Nursing Administration Quarterly. 2000;24:1–11. doi: 10.1097/00006216-200004000-00003. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validity of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mollica RF. Coordinating services across the continuum of health, housing, and supportive services. Journal of Aging and Health. 2003;15:165–188. doi: 10.1177/0898264302239022. [DOI] [PubMed] [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Prezeworski A, Erickson T, et al. Preliminary reliability and validity of the Generalized Anxiety Disorder Questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy. 2002;33:215–233. [Google Scholar]
- Nuevo R, Montorio I, Borkovec TD. A test of the role of metaworry in the prediction of worry severity in an elderly sample. Journal of Behavior Therapy and Experimental Psychiatry. 2004;35:209–218. doi: 10.1016/j.jbtep.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E. Development and validation of the Geriatric Anxiety Inventory. International Journal of Psychogeriatrics. 2007;19:103–114. doi: 10.1017/S1041610206003504. [DOI] [PubMed] [Google Scholar]
- Parmelee PA, Katz IR, Lawton MP. Anxiety and its association with depression among institutionalized elderly. American Journal of Geriatric Psychiatry. 1993;1:46–58. doi: 10.1097/00019442-199300110-00007. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Préville M, Côté G, Boyer R, Hébert R. Detection of depression and anxiety disorders by home care nurses. Aging and Mental Health. 2004;8:400–409. doi: 10.1080/13607860410001725009. [DOI] [PubMed] [Google Scholar]
- Quijano LM, Stanley MA, Peterson NJ, Casado BL, Steinberg EH, Cully JA, et al. Healthy I.D.E.A.S.: A depression intervention delivered by community-based case managers serving older adults. Journal of Applied Gerontology. 2007;26:139–156. [Google Scholar]
- Ruscio AM, Chiu WT, Roy-Byrne P, Stang PE, Stein DJ, Wittchen H, et al. Broadening the definition of generalized anxiety disorder: Effects on prevalence and associations with other disorders in the National Comorbidity Survey Replication. Journal of Anxiety Disorders. 2007;21:662–676. doi: 10.1016/j.janxdis.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senior AC, Kunik ME, Rhoades HM, Novy DM, Wilson NL, Stanley MA. Utility of telephone assessments in an older adult population. Psychology and Aging. 2007;22:392–397. doi: 10.1037/0882-7974.22.2.392. [DOI] [PubMed] [Google Scholar]
- Shear MK, Belnap BH, Mazumdar S, Houck P, Rollman B. Generalized Anxiety Disorder Severity Scale (GADSS): A preliminary validation study. Depression and Anxiety. 2006;23:77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Haworth Press; 1986. (pp. 165–173) [Google Scholar]
- Sinoff G, Werner P. Anxiety disorder and accompanying subjective memory loss in the elderly as a predictor of future cognitive decline. International Journal of Geriatric Psychiatry. 2003;18:951–959. doi: 10.1002/gps.1004. [DOI] [PubMed] [Google Scholar]
- Smalbrugge M, Jongenelis K, Pot AM, Beekman ATF, Eefsting JA. Comorbidity of depression and anxiety in nursing home patients. International Journal of Geriatric Psychiatry. 2005;20:218–226. doi: 10.1002/gps.1269. [DOI] [PubMed] [Google Scholar]
- Snyder AG, Stanley MA, Novy DM, Averill PM, Beck JG. Measures of depression in older adults with generalized anxiety disorder: A psychometric evaluation. Depression and Anxiety. 2000;11:114–120. doi: 10.1002/(sici)1520-6394(2000)11:3<114::aid-da5>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Kroenke K, Linzer M, deGruy FV, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: The PRIME-MD 1000 study. Journal of the American Medical Association. 1994;272:1749–1756. [PubMed] [Google Scholar]
- Stanley MA, Diefenbach GJ, Hopko DR, Novy DM, Kunik ME, Wilson N, et al. The nature of generalized anxiety in older primary care patients: Preliminary findings. Journal of Psychopathology and Behavioral Assessment. 2003;25:273–280. [Google Scholar]
- Stanley MA, Hopko DR, Diefenbach GJ, Bourland SL, Rodriquez H, Wagener P. Cognitive-behavior therapy for late-life generalized anxiety disorder in primary care: Preliminary findings. American Journal of Geriatric Psychiatry. 2003;11:92–96. [PubMed] [Google Scholar]
- Stanley MA, Novy DM, Bourland SL, Beck JG, Averill PM. Assessing older adults with generalized anxiety: A replication and extension. Behaviour Research and Therapy. 2001;39:221–235. doi: 10.1016/s0005-7967(00)00030-9. [DOI] [PubMed] [Google Scholar]
- Steer RA, Willman M, Kay PAJ, Beck AT. Differentiating medical and psychiatric outpatients with the Beck Anxiety Inventory. Assessment. 1994;1:345–351. [Google Scholar]
- Webb SA, Diefenbach G, Wagener P, Novy DM, Kunik M, Rhoades HM, et al. Comparison of self-report measures for identifying late-life generalized anxiety in primary care. Journal of Geriatric Psychiatry and Neurology. 2008;21:223–231. doi: 10.1177/0891988708324936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss BJ, Calleo J, Rhoades HM, Novy DM, Kunik ME, Lenze EJ, et al. The utility of the Generalized Anxiety Disorder Severity Scale (GADSS) with older adults in primary care. Depression and Anxiety. 2009;(1):E10–5. doi: 10.1002/da.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherell JL, Birchler GD, Ramsdell J, Unutzer J. Screening for generalized anxiety disorder in geriatric primary care patients. International Journal of Geriatric Psychiatry. 2007;22:115–123. doi: 10.1002/gps.1701. [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Gatz M. The Beck anxiety inventory in older adults with generalized anxiety disorder. Journal of Psychopathology and Behavioral Assessment. 2005;27:17–22. [Google Scholar]
- Yesavage JA. Geriatric Depression Scale. Psychopharmacology Bulletin. 1988;24:709–711. [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey MB, et al. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Zeltzer BB, Kohn R. Mental health services for homebound elders from home health nursing agencies and home care agencies. Psychiatric Services. 2006;57:567–569. doi: 10.1176/ps.2006.57.4.567. [DOI] [PubMed] [Google Scholar]