Abstract
Animal and preliminary human studies of adult cell therapy following acute myocardial infarction have shown an overall improvement of cardiac function. Myocardial and vascular regeneration have been initially proposed as mechanisms of stem cell action. However, in many cases the frequency of stem cell engraftment and the number of newly generated cardiomyocytes and vascular cells, either by transdifferentiation or cell fusion, appear too low to explain the significant cardiac improvement described. Accordingly, we and others have advanced an alternative hypothesis: the transplanted stem cells release soluble factors that, acting in a paracrine fashion, contribute to cardiac repair and regeneration. Indeed, cytokines and growth factors can induce cytoprotection and neovascularization. It has also been postulated that paracrine factors may mediate endogenous regeneration via activation of resident cardiac stem cells. Furthermore, cardiac remodeling, contractility, and metabolism may also be influenced in a paracrine fashion. This article will review the potential paracrine mechanisms involved in adult stem cell signaling and therapy.
Keywords: adult stem cells, paracrine signaling, cytoprotection, neovascularization, regeneration
Introduction
Despite major advances in our understanding as well as treatment of coronary artery disease, acute myocardial infarction (AMI) still represents a significant cause of mortality and morbidity worldwide. Indeed, following AMI, cardiomyocytes begin to die and if blood supply is not timely restored all the cardiac tissue served by the infarcted related artery undergoes necrosis or apoptosis, leading to chronic sequelae of ischemic cardiomyopathy and congestive heart failure. The endogenous regenerative capacity of the heart seems unable to replenish a significant loss of tissue like after AMI1, 2. However, the recent discovery of resident cardiac stem cells (CSCs)3 together with the demonstration of bone marrow (BM)-derived stem cells able to home in the heart and transdifferentiate into cardiomyocytes4, 5 have suggested the fascinating possibility that therapeutic myocardial regeneration might be achieved using adult stem cells (ASCs). Over the past several years, ASC therapy of the heart has generated significant interest in clinical and basic scientific communities. To date, the majority of animal and preliminary human studies of ASC therapy following AMI have demonstrated an overall improvement of cardiac function. The cell types used have included BM- derived mononuclear cells (BM-MNCs), unfractionated BM cells (BMCs), hematopeitic stem cells (HSCs), endothelial progenitor cells (EPCs), mesenchymal stem cells (MSCs)6–9 and CSCs3, 10–12.
Among ASCs, CSCs seem to possess the properties required to achieve cardiac regeneration, since they are autologous, can be expanded ex vivo, show proliferative restraint, and, most importantly, can differentiate into endothelial cells (ECs), vascular smooth muscle cells (VSMCs) and cardiomyocytes13, 14. It has been shown that, when injected into infarcted murine hearts, CSCs regenerate cardiac tissue that appear to become functionally integrated with the surrounding native myocardium3, 11, 12. With regard to BM-derived stem cells, transdifferentiation into cardiomyocytes and into vascular lineage cells has been originally proposed as the principal mechanisms underlying their therapeutic action15–17. For example, Tomita and coworkers showed that transplantation of MSCs pretreated with 5-azacytidine into cryoinjured rat hearts could home and differentiate into cardiac-like muscle cells and improve ventricular function17. Many other groups have confirmed that MSCs possess the ability to differentiate into cardiomyocytes18. Anversa’s laboratory demonstrated that Lin− c-kit+ (HSC-enriched) BM-derived cells injected directly into mouse hearts after AMI were able to engraft, transdifferentiatiate into cardiac cells, and regenerate approximatively 68% of the infarcted area with newly formed cardiomyocytes16.
More recently, other investigators have failed to detect permanent engraftment and transdifferentiation of transplanted BM-derived HSCs19, 20. Furthermore, so far it has not been possible to reproducibly induce a functional cardiac phenotype in BM-derived ASCs in vitro using physiological growth factors or non-toxic chemical compounds. These negative results have questioned the plasticity of both endogenous and transplanted BM-derived stem cells and the scientific debate is still ongoing. Recently, cell fusion of BM-derived donor cells with recipient cardiomyocytes has been reported21–23 and suggested to be a contributory mechanism. However, the frequency of cell fusion is also debated24.
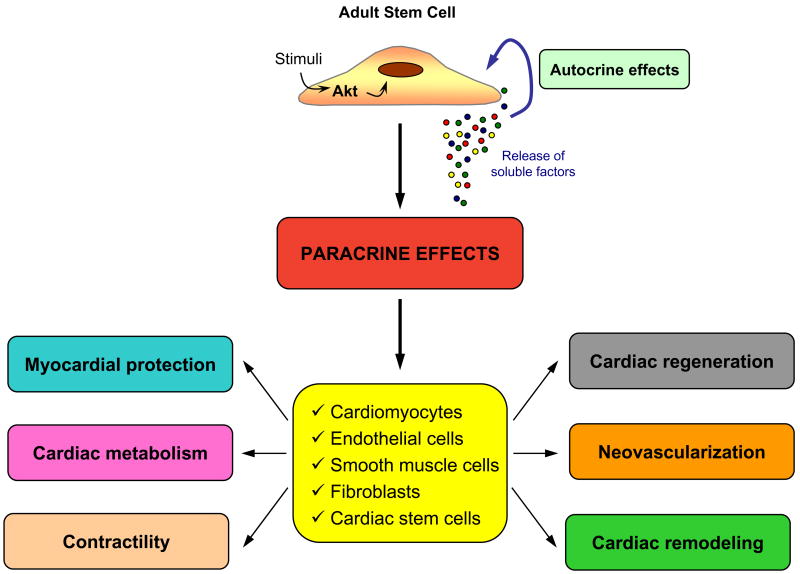
Regardless of whether stem cells transdifferentiate via fusion-dependent or -independent mechanism, it has been shown that in some settings the number of newly generated cardiomyocytes is too low to explain significant functional improvement. Therefore, we and others have proposed that the functional benefits observed after stem-cell transfer in animal models of cardiac injury might be related to secretion of soluble factors that, acting in a paracrine fashion, protect the heart, attenuate pathological ventricular remodeling, induce neovascularization and promote regeneration25–27. Accordingly, the 3 main established mechanisms of ASC’s action in heart repair are: cardiomyocyte regeneration, vasculogenesis and paracrine actions (Figure 1). In this review, we will focus our attention on stem cell paracrine actions in heart repair.
Figure 1. Proposed mechanisms of adult stem cell action in cardiac repair.
Transdifferentiation and cell fusion of transplanted stem cells lead to cardiac regeneration and vasculogenesis. Paracrine effects can positively influence many processes, among them cardiomyogenesis and neovascularization (see text for details). Cardiac regeneration, vasculogenesis and paracrine effects lead to cardiac repair.
Paracrine mechanisms
There is a growing body of evidence supporting the hypothesis that paracrine mechanisms mediated by factors released by the ASCs play an essential role in the reparative process observed after stem cell mobilization or injection into infarcted hearts. It has been shown that ASCs, particularly MSCs, produce and secrete a broad variety of cytokines, chemokines, and growth factors that may potentially be involved in cardiac repair (Table 1)28. Furthermore, hypoxic stress increases the production of several of these factors29. Tissue concentrations of proteins such as vascular endothelial growth factor (VEGF), basic fibroblast growth factor (b-FGF), hepatocyte growth factor (HGF), insulin growth factor I (IGF-I) and adrenomedullin, just to name some, are significantly increased in injured hearts treated with MSCs or multipotent human BM stem cells (hBMSCs)30, 31. Strong support of paracrine mechanism for cardiac repair come from experimental studies where the administration of conditioned medium (CM) from ASCs is able to recapitulate the beneficial effects observed after stem cell therapy. We have demonstrated that CM from MSCs, particularly from genetically modified MSCs overexpressing Akt-1 (Akt-MSCs), exerts cardiomyocyte protection25, 26. Takahashi and colleagues32 injected CM from BM-MNCs into acutely infarcted hearts and observed increased capillary density, decreased infarct size, and improved cardiac function compared with controls.
Table 1.
Putative paracrine factors secreted by adult stem cells
| Putative secreted factor | Abbreviation | Proposed Function |
|---|---|---|
| Adrenomedullin | ADM | Cytoprotection |
| Angio-associated migratory protein | AAMP | Angiogenesis |
| Angiogenin | ANG | Angiogenesis, cell proliferation |
| Angiopoetin-1 | AGPT1 | Cell migration, vessel stabilization |
| Bone morphogenetic protein-2 | BMP2 | Development |
| Bone morphogenetic protein-6 | BMP6 | Cell differentiation, growth |
| Connective tissue growth factor | CTGF | Angiogenesis, cell growth |
| Endothelin-1 | EDN1 | Cytoprotection, cell proliferation |
| Fibroblast growth factor-2 | FGF2 | Cell proliferation and migration |
| Fibroblast growth factor-7 | FGF7 | Cell proliferation and stabilization |
| Hepatocyte growth factor | HGF | Cytoprotection, angiogenesis, cell migration |
| Insulin-like growth factor-1 | IGF-1 | Cytoprotection, cell migration, contractility |
| Interleukin-1 | IL-1 | VEGF induction |
| Interleukin-6 | IL-6 | VEGF induction |
| Interleukin-11 | IL-11 | Cytoprotection |
| Kit ligand/Stem cell factor | KITLG (SCF) | Cell proliferation and migration |
| Leukemia inhibitory factor | LIF | Cell proliferation, cytoprotection |
| Macrophage migration inhibitory factor | MIF | Cell proliferation, inflammatory response |
| Matrix metalloproteinase-1 | MMP1 | Loosens matrix, tubule formation |
| Matrix metalloproteinase-2 | MMP2 | Loosens matrix, tubule formation |
| Matrix metalloproteinase-9 | MMP9 | Loosens matrix |
| Monocyte chemoattractant protein-1 | MCP-1 | Monocyte migration |
| Macrophage-specific colony-stimulating factor | M-CSF | Monocyte proliferation/migration |
| Placental growth factor | PGF | Cell proliferation |
| Plasminogen activator | PA | Degrading matrix molecules |
| Platelet-derived growth factor | PDGF | Cell proliferation and migration |
| Pleiotrophin | PTN | Cell proliferation |
| Secreted frizzled-related protein-1 | SFRP1 | Development |
| Secreted frizzled-related protein-2 | SFRP2 | Development |
| Stem cell-derived factor-1 | SDF-1 | Progenitor cell homing |
| Thrombospondin-1 | THBS1 | Cell migration |
| Thymosin-β4 | TMSB4 | Cell migration, cytoprotection |
| Tissue inhibitor of metalloproteinase-1 | TIMP-1 | Cell migration |
| Tissue inhibitor of metalloproteinase-2 | TIMP-2 | Cell migration |
| Transforming growth factor-β | TGF-β | Vessel maturation, cell proliferation |
| Tumor necrosis factor-α | TNF-α | Degrade matrix molecules, cell proliferation |
| Vascular endothelial growth factor | VEGF | Cytoprotection, proliferation, migration, angiogenesis |
The paracrine factors may influence adjacent cells and exert their actions via several mechanisms. Myocardial protection and neovascularization are the most extensively studied. Furthermore, the post infarction inflammatory and fibrogenic processes, cardiac metabolism, cardiac contractility, and/or endogenous cardiac regeneration may also be positively influenced in a paracrine fashion (Figure 2). It is likely that the paracrine mediators are expressed/released in a temporal and spatial manner exerting different effects depending on the microenvironment after injury. In addition, these released factors may have autocrine actions on the biology of stem cells themselves33 (Figure 2). Thus, the paracrine/autocrine hypothesis extends the traditional concept of stem cell niche to include the influence of stem cell released factors on the microenvironment modulating stem cell biology and tissue response.
Figure 2. Paracrine-autocrine mechanisms in stem cell signaling and therapy.
ASCs release biologically active substances in a temporal and spatial manner in response to specific environmental stimuli such as ischemia. These factors influence the microenvironment by exerting paracrine actions on different cell types leading to tissue protection, repair and regeneration. The putative factors may also exert autocrine actions modulating the biology of stem cells including self-renewal and proliferation.
Myocardial protection
An immediate paracrine effect of stem cells in an ischemic environment is the release of cytoprotective molecules that increase cardiomyocyte survival (Figure 3). Our group characterized the spectrum of BM stem cell paracrine actions and demonstrated that MSCs exert direct cytoprotective action on ischemic cardiomyocytes. In particular, we showed that cell culture medium conditioned by hypoxic MSCs can reduce apoptosis and necrosis of isolated rat cardiomyocytes exposed to low oxygen tension25. The cytoprotective effect was greatly enhanced in MSCs overexpressing the gene Akt-1 (Akt-MSCs) in vitro. To further validate the protective properties of the MSCs, we studied the effect of the CM in vivo, using a rat experimental model of coronary occlusion. Concentrated CM was injected into the heart at the infarct border zone 30 min after left coronary occlusion. After 72 hours, the infarct size and the cardiomyocyte apoptotic index were reduced, albeit modestly, in animals treated with CM from MSCs (MSC-CM) compared with those treated with saline. In contrast, a dramatic reduction of infarct size and cardiac apoptosis was observed after administration of CM from Akt-MSCs (AKT-MSCs-CM). These data showed that MSCs exert cardiac protective effect through the release of paracrine factors and that the activation of the Akt pathway markedly enhances the production/release of these putative molecules. In a follow-up study we confirmed our previous results and documented how the limitation of the infarct size was matched by preservation of cardiac function26. To verify whether Akt overexpression upregulated the expression of secreted factors, we tested by quantitative RT-PCR some candidate genes encoding for molecules known to be released by MSCs. Our data showed that VEGF, bFGF, HGF, insulin growth factor 1 (IGF-1), and thymosin β4 (TB4) were significantly up-regulated in the Akt-MSCs at baseline normoxia and increased further after exposure to hypoxia. After exposure to hypoxia, native MSCs also up-regulated VEGF, bFGF, HGF, and TB4 albeit less than the Akt-MSCs. Recently, our original findings in rodents have been successfully replicated by others also in a large animal model. Indeed, Akt-MSCs injected into pig infarcted hearts led to limitation of infarct size and preservation of heart function34.
Figure 3. Proposed factors and signalling pathways involved in stem cell-mediated myocardial protection9, 26, 90–95.
It has been shown that ASCs mediate cardioprotection by producing and releasing soluble mediators with known cytoprotective properties. Most of these factors act through the activation of the pro-survival PI-3 kinase/Akt pathway. Factors like FGF-2 and EPO can activate the protein kinase C pathway, which has been shown to mediate cardioprotection. Interleukin 11 (IL11) also activates survival signalling cascades in PI3K/Akt and ERK1/2-STAT3 dependent fashion. The mechanisms of action through which Sfrp2 and TB4 lead to cardioprotection are partially undetermined and need to be further clarified. Finally, other factors and pathways are certainly involved but are still unidentified. Abbreviations: IL11, interleukin 11; HGF, hepatocyte growth factor; IGF-1, insulin growth factor 1; VEGF, vascular endothelial growth factor; EPO, erythropoietin; FGF-2, fibroblast growth factor-2; TB4, thymosin beta 4; GF, growth factor; C, cytochrome c; GLUT, glucose transporter; VDAC, voltage-dependent anion channel.
Other groups have confirmed the paracrine cytoprotective effects exerted by BM-derived stem cells on ischemic cardiomyocytes32, 35, 36. Uemura and colleagues recapitulated our in vitro data adopting a different approach35. Freshly isolated adult mouse cardiomyocytes were exposed for 3 hours to hypoxia. Positive annexin V staining and DNA laddering were both indicative of apoptosis. However, if the cardiomyocytes were cocultured with BM-MSCs hypoxia induced apoptosis was significantly reduced. High levels of VEGF, bFGF, IGF-1, and SDF-1 were present in the MSC-CM, especially after exposure to hypoxia. To confirm the cytoprotective effect in vivo, the authors injected GFP-labelled MSCs into infarcted mouse hearts. Three groups were considered: sham, MSCs and hypoxia-preconditioned MSCs. The cells engrafted mostly in the border area. However, the frequency of GFP-positive cardiomyocytes was very low and did not differ between the 2 cell groups. TUNEL staining showed that the number of apoptotic cardiomyocytes was significantly reduced in MSC-treated animals, particularly when preconditioned cells were administered. Accordingly, infarcted area and ventricular remodeling were significantly prevented in animals treated with hypoxic MSCs compared with those receiving normoxic MSCs.
Takahashi and colleagues showed that also rat BM-MNCs produce and release various cytoprotective factors, including VEGF, PDGF, IL-1β, and IGF-1, some of which are significantly upregulated by hypoxia32. Administration of CM from BM-MNCs cultured under normoxia or hypoxia inhibited apoptosis in vitro and reduced infarct size in vivo. Also human BM-MNCs exert potent cytoprotective effects37. Kubal and collaborators exposed muscle cells from the atrial appendage of patient undergoing elective cardiac surgery to hypoxia/reperfusion stress. When cardiac cells were coincubated with BM-MNCs, harvested from the same patients, reduction of cell necrosis and apoptosis was documented. Of note, coincubation with control ECs or keratinocytes did not result in cytoprotection, suggesting that the effect was specific for BM-MNCs. Finally, it has been shown that also hBMSCs induce cardiac protection30.
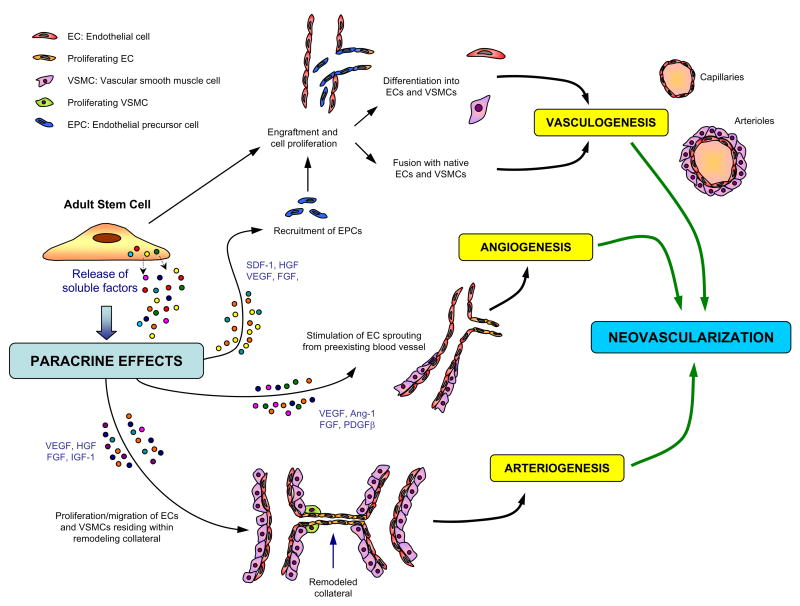
Neovascularization
Another important biological process positively influenced by stem cells in a paracrine fashion is neovascularization. Despite evidences that BM-derived stem or progenitor cells incorporate into vascular structures, several studies suggest that only a small number of vessels contain donor cells. The molecular processes leading to angiogenesis and arteriogenesis involve mediators such as nitric oxide, VEGF, bFGF, HGF, angiopoietin and others. These molecules lead to EC and VSMC migration, proliferation, vessel enlargement and maturation, and synthesis of extracellular matrix. As described earlier, it has been shown that BM stem cells can express proangiogenic molecules29. Accordingly, it has been hypothesized that the release of putative proangiogenic factors may play an important role in determining the increase in capillary density and collateral development observed in ischemic tissues of animals treated with stem cells. For example, it has been reported that the injection of BM-MNCs into a zone of swine heart made ischemic by coronary ligation resulted in a significant increase of regional blood flow and capillary density at 3 weeks38. The authors showed that the BM-MNCs injected expressed bFGF, VEGF, and angiopoietin-1 and that the cardiac levels of these angiogenic ligands were significantly increased 3 weeks after stem cell injection compared with controls. Furthermore, the cardiac levels of interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α) were markedly increased after BM-MNC administration. Since also IL-1β and TNF-α were shown to have angiogenic activity, the authors concluded that the released factors likely contributed to stimulate angiogenesis in BM-MNC treated animals. The proangiogenic paracrine action of BM-MNCs has been validated by the documentation of increased microvessel density in ischemic hearts injected solely with CM from MNCs32.
We and others have demonstrated that MSC represent a source of paracrine proangiogenic and proarteriogenic factors26, 29, 39. Data from Epstein and collaborators have suggested that in vivo local delivery of MSCs augments collateral perfusion through paracrine mechanisms27. These authors injected 1×106 MSCs in the adductor muscle of mice 24 hours after femoral artery ligation. Compared with controls injected with medium or mature ECs, distal limb perfusion improved and conductance vessels increased in number and total cross-sectional area. Surprisingly, labelled MSCs were dispersed between muscle fibers but not seen incorporated into mature collaterals. On the other hand, protein levels of VEGF and bFGF were significantly increased in the muscle of MSC-treated animals compared with controls; furthermore, colocalization of VEGF and transplanted MSCs within adductor tissue was documented. The authors concluded that MSCs contributed to collateral remodeling through paracrine mechanisms. Gene expression profiling of MSCs grown under normal conditions or under hypoxia stimulation allowed to document that these cells express a wide range of arteriogenic cytokines at baseline and that several of them are upregulated by hypoxia29. The gene array data were confirmed using ELISA assays and immunoblotting of the MSC-CM. Furthermore, it was shown that MSC-CM promoted proliferation and migration of ECs and VSMCs in a dose-dependent manner in vitro and enhanced collateral flow recovery and remodeling in a model of hind limb ischemia in vivo. Other studies, testing MSC transplantation in experimental infarcted hearts, reported an increase in capillary density in treated animals compared with controls, despite the presence of few ECs of donor origin40–42. In these cases, even though not directly proven, a proangiogenic paracrine action seems the most reasonable explanation to the effects observed.
Finally, it has been shown that EPCs can enhance angiogenesis by releasing cytokines and chemokines. In particular, VEGF and stromal derived factor 1 (SDF-1) released in the CM by EPCs seem to promote the migration of mature ECs in vitro through differentiation-indipendent mechanisms43. In addition, several reports showed that transplantation of EPCs into ischemic hearts promotes angiogenesis and arteriogenesis in vivo44–46. Taken together, all these reports show that, besides direct vasculogenesis, ASCs improve neovascularization of ischemic tissues through proangiogenic and proarteriogenic paracrine effects (Figure 4).
Figure 4. Mechanisms involved in neovascularization.
In contrast to the embryonic heart vasculature, the adult heart vessels are quiescent. Only when under stress or in the presence of pathologic conditions, like myocardial infarction, the coronary vascular bed expands. ASCs are involved in postnatal neovascularization which encompasses 3 different mechanisms: the first is referred to as postnatal vasculogenesis, that consists in the assembly of new blood vessels by fusion and differentiation of endothelial precursor cells originating from the bone marrow. The second mechanism is angiogenesis and consists in the sprouting of new vessels from pre-existing vessels. The third mechanism is collateral enlargement and muscolarization, namely arteriogenesis. The release of proangiogenic and proarteriogenic factors by transplanted stem cells positively influences neovascularization in a paracrine fashion.
Cardiac remodeling
Beside cytoprotection and neovascularization, paracrine factors released by transplanted stem cell may alter the extracellular matrix, resulting in more favorable post-infarction remodeling and strengthening of the infarct scar. It has been shown that direct hMSC injection into ischemic rat hearts decreases fibrosis, apoptosis and left ventricular dilatation while increases myocardial thickness; this results in the preservation of systolic and diastolic cardiac function without evidence of myocardial regeneration47. In animal models, MSC transplantation decreases fibrosis in the heart31 and other organs such as lung48, liver49 and kidney50. It has been show that MSCs express a number of molecules involved in biogenesis of extracellular matrix such as collagens, metalloproteinases (MMPs), serine proteases and serine protease inhibitors, suggesting that transplanted MSCs can inhibit the fibrosis through paracrine actions39. Xu and colleagues evaluated the effects of grafting MSCs on extracellular matrix in infracted rat hearts51. They showed that MSC transplantation significantly attenuated the increased cardiac expression of collagen types I and III, tissue inhibitor of metalloproteinase-1 (TIMP-1), and tumor growth factor beta (TGF-β) observed in infarcted control hearts. Nagaya’s group52 found that MSC-CM significantly attenuated cardiac fibroblast proliferation and inhibited type I and type III collagen expression in cardiac fibroblasts; in addition, they showed that collagen activity in the MSC-CM was as high as the activity in the medium conditioned by cardiac fibroblasts. The authors concluded that MSCs exerted paracrine anti-fibrotic effects at least in part through inhibition of cardiac fibroblast proliferation and types I and III collagen synthesis.
Important data supporting the anti-remodeling effect exerted via paracrine action by BM-derived cells come from studies testing stem cell therapy to treat nonischemic cardiomyopathy. Nagaya and collaborators injected BM-MSCs into the myocardium of rats in which dilated cardiomyopathy was produced by inducing experimental myocarditis31. Compared with vehicle injection, MSC administration significantly increased capillary density and, most importantly, decreased the collagen deposition in the myocardium, resulting in decreased left ventricular end-diastolic pressure and increased left ventricular maximum dP/dt. The importance of paracrine mechanisms in this particular experimental model was underscored by the limited number of MSC-derived cardiomyocytes, which was clearly insufficient to result in the recovery of cardiac function reported. Of note, relative quantification of cardiac proteins showed that MMP-2 and MMP-9 significantly increased in DCM whereas in MSC treated hearts MMP level were comparable to sham. Even though the underlying mechanism remains unclear, taken together these data suggest that BM-derived ASC transplantation may influence extracellular remodeling in heart failure.
Stem cells may also produce and release local signaling molecules that limit local inflammation when injected into injured tissues. This hypothesis seems to be supported by the fact that expression profiling of adult progenitor cells has revealed expression of genes typically associated with enhanced DNA repair, antioxidant enzymes, and genes linked with detoxifier systems53. Ohnishi and coworkers54 demonstrated that MSC transplantation into a rat model of acute myocarditis attenuated the increase in CD68+ inflammatory cells and monocyte chemoattractant protein-1 (MCP-1) expression in the myocardium and improved cardiac function. Isolated adult rat cardiomyocytes (ARVCs) cultured in standard conditions were injured by MCP-1, which may play an important role in myocarditis55; in contrast, in the presence of MSC-CM the MCP-1-induced injury was significantly attenuated.
Cardiac contractility and metabolism
Some evidences suggest that the administration of ASCs positively influences also cardiac contractility. For example, with regard to the early functional improvement of acutely infarcted hearts after injection of Akt-MSC-CM, the effect may be the consequence of myocardial protection leading to infarct size limitation and/or the direct action of inotropic factors released by the cells. As for the former mechanism, it has been well documented that therapies able to limit myocardial infarct size can prevent ventricular dysfunction56. In support of the latter, we observed, in the presence of the CM from hypoxic Akt-MSCs, a marked increase in spontaneous contractile activity in ARVCs exposed to prolonged hypoxia26. Such contractile activity was very different from the typical spontaneous contractility observed when the ARVCs are maintained in standard growth conditions. In this case, the vigorous and synchronized contraction observed may suggest the presence of inotropic factors in the CM able to positively influence the contractile properties of ARVCs. Preliminary experiments on freshly isolated adult rat cardiomyocytes exposed to standard growth medium or to different concentrations of MSC-CM or Akt-MSC-CM seem to confirm that MSCs do release inotropic factors that positively modulate cell contractility. Indeed, using an edge-to-edge detection system we observe that cell shortening, maximal rate of relenghtening (+dL/dt), and maximal rate of shortening (−dL/dt) are significantly improved in the presence of CM from hypoxic MSCs, particularly Akt-MSCs, compared with standard conditions (unpublished data). Results from other groups would confirm the paracrine action of BM-derived stem cells on cardiomyocyte contractility. For example, Takahashi and collaborators showed that CM from BM-MNCs preserved the contractility capacity of ARVCs32. Fractional shortening and ± dL/dt of ARVCs cultivated for 72 hours in standard growth medium were significantly lower compared with those recorded at baseline. Conversely, cell contractility parameters did not decrease significantly when ARVCs were cultured in the presence of CM from BM-MNCs pre-exposed to normoxia or hypoxia. Of note, the supernatant from hypoxic BM-MNCs was more effective compared with CM from normoxic cells in preserving ARVC contractility. This observation further suggests that production and release of the factors mediating inotropic paracrine effects are increased under hypoxia. More detailed experiments are needed in order to elucidate the pathways and the mediators involved. At the moment, the nature and identity of putative molecules can only be hypothesized. For example, it is known that, in addition to its growth-promoting and anti-apoptotic actions, IGF-I can increase cardiomyocyte contractility in vitro57 and improve myocardial function both in normal and infarcted adult rat hearts58, 59. The possibility of nonpeptidic molecules mediating this effect cannot be excluded.
Interestingly, Dhein and collaborators have reported that administration of BM-derived stem cells in doxorubicine induced decompensated rabbit hearts significantly limited the down-regulation of β-adrenoceptor normally present in this heart failure model and significantly increased cardiac contractility measured in vivo60. It is well known that β-adrenoceptors couple to adenylate cyclase and mediate positive inotropic effects of catecholamines. In this particular case, the positive and significant correlation between β-adrenoceptor density and contractility described would support the hypothesis on a relationship between these two parameters. Interestingly, in failing hearts receiving BM cell transplantation β-adrenoceptor density was nearly normalized in the septum while was still below the normal level in the left ventricle. Considering that the cells were injected in the free wall and that the number of engrafted cells was low, the authors proposed that the effects observed might be due to paracrine action. However, it cannot be excluded that the improved hemodynamic situation resulted in decreased catecholamine levels, and that this consequently led to attenuation of β-adrenoceptor down-regulation. Experiments on isolated cardiomyocytes cocultured with BM-derived stem cells or in the presence of CM may help to clarify this issue.
It has also been suggested that administration of BM-derived cells may positively affect cardiac metabolism in ischemic hearts. Feygin et al. examined whether mesenchymal stem cell transplantation-induced beneficial effects are secondary to paracrine-associated improvements in left ventricular (LV) contractile performance, wall stress, and myocardial bioenergetics in hearts with postinfarction LV remodeling in pigs. They demonstrated that hearts in the AMI group developed severe contractile dyskinesis in the infarct zone and border zone, while MSC transplantation significantly improved contractile performance from dyskinesis to active contraction. Border zone systolic wall stress was severely increased in infarcted hearts but significantly improved after MSC transplantation. The border zone demonstrated profound bioenergetic abnormalities in infarcted hearts, which were attenuated after MSC transplantation. Because of low cell engraftment, the authors postulated that MSCs did not provide a structural contribution to the damaged heart and concluded that the observed beneficial effects likely resulted from paracrine repair mechanisms61.
Cardiac regeneration
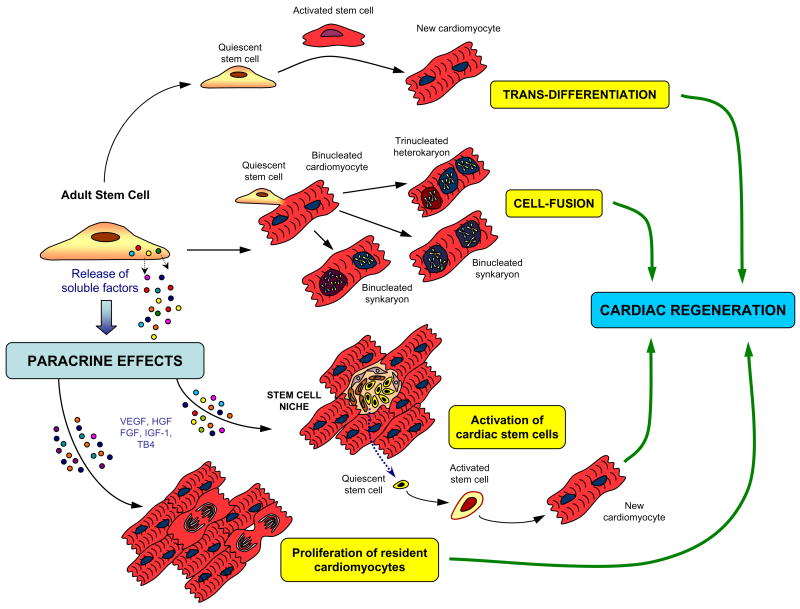
It has been proposed that ASCs, when injected into the injured myocardium, can proliferate and transdifferentiate into cardiomyocytes or fuse with native cardiomyocytes thereby regenerating the lost myocardium7. Some investigators have recently proposed a further intriguing hypothesis: exogenous stem cell transplantation may activate resident CSCs and/or stimulate cardiomyocyte replication via paracrine action, thus enabling endogenous cardiac regeneration (Figure 5). It is indeed conceivable that some of the factors released by transplanted ASCs may enhance proliferation, mobilization, differentiation, survival, and function of endogenous cardiac progenitors or even restoration of stem cell niches.
Figure 5. Mechanisms involved in cardiac regeneration.
Potentially, ASCs may lead to cardiac regeneration via different mechanisms. Transdifferentiation into newly formed cardiomyocytes has been the first proposed way. Cell fusion of stem cells with native cardiomyocytes represents a second possibility but the biological meaning of this event remains unclear. Finally, soluble paracrine factors released by the stem cells may induce activation, migration and differentiation of CSCs and/or enhance proliferation of resident cardiomyocytes.
Currently, there are no studies directly examining the effect of ASC transplantation on endogenous cardiac progenitors. But there are evidences suggesting such effect. For example, it has been shown that intramyocardial administration of HGF and IGF-1 at the infarct border zone induces CSC migration, proliferation, and differentiation62. Since MSCs release both HGF and IGF-1, particularly under hypoxic stimulation26, it is reasonable to hypothesize that MSC injected into ischemic hearts may attract and activate resident CSCs. Indirect evidence supporting this hypothesis has been documented in a study in which MSCs were injected into infarcted pig hearts63. Immunohistochemical analysis performed after 10 days revealed the presence, only in MSC-treated animals, of supposedly newly formed cardiomyocytes, some of which stained positive for c-Kit, a marker expressed by CSCs, and others for Ki67, a marker of cell proliferation. Unfortunately, the co-staining for c-Kit and Ki67 was not performed, so that the true origin of those replicating cardiomyocytes could not be determined. However, the authors concluded that endogenous cardiac regeneration was present. Also hBMSCs may induce proliferation of host cardiomyocytes30. Yoon and coworkers reported that intramyocardial transplantation of hBMSCs after myocardial infarction resulted in robust engraftment of transplanted cells, which transdifferentiated into cardiomyocytes, and proliferation of host cardiomyocytes and ECs. To determine the proliferative fraction of host myocardial cells, the authors administered BrdU to label all cells that entered the S phase of the cell cycle. Appropriate immunohistochemistry analysis revealed, both in the peri-infarct and normal portion of the heart, a significantly higher number of proliferating cardiomyocyte and ECs in sections from hBMSC-transplanted animals compared with controls. Also the staining for Ki67 confirmed that the transplanted hBMSCs augmented proliferation of host myocardial cells. Interestingly, in the same study the paracrine cytoprotective and proangiogenic actions exerted by BM-derived stem cells were further confirmed, and the mRNA levels of HGF, IGF-1, VEGF, and bFGF were significantly upregulated in hBMSC-treated hearts compared with controls.
An in vitro study has shown that EPCs are also able to induce migration and growth of c-Kit+ cardiac progenitor cells by secretion of cytokines such as VEGF, IGF-1 and SDF-143. Although the in vivo experiment remains to be performed, the implication is that the cytokines released locally within the myocardium by the EPCs may activate the regenerative reservoir of the heart and possibly contribute to the beneficial effects observed in infarcted hearts treated with this cell population. The presence of cardiomyocytes or CSCs actively dividing was analyzed also in infarcted hearts treated with HSCs but the results were negative24. The presence and the role of endogenous cardiac regeneration after intramyocardial BM-derived stem cell administration requires further in depth investigation.
Improving our understanding of stem cell biology
The demonstration that stem cells express and release biologically active mediators has important implications in the understanding of stem cell biology and action. As discussed earlier, the release of paracrine cytokines can influence the stem cell microenvironment that is part of the stem cell niche. In addition the paracrine mediators can influence the biology of adjacent parenchymal and stromal cells in normal and pathological conditions. In response to tissue injury, stem cells can express and secrete important paracrine factors in a temporal and spatial manner that can enhance cell survival and activate endogenous mechanisms of endogenous repair and regeneration. There is a dynamic regulation and interaction of stem cell cytokine that influences tissue survival, repair and regeneration including the activation of resident and circulating extracardiac stem cells. Specific studies will need to be carried out to better understand how stem cells mediate their favorable effects. In particular, the factors and the pathways involved should be defined. Studying in detail the temporal and spatial expression of paracrine factors in the heart after stem cell administration will help researchers to understand the complex process of heart protection, remodeling, repair and regeneration. Identifying the complete scope and nature of paracrine factors involved in stem cell-mediated cardiac repair is a demanding task, although extremely relevant and worth pursuing. Our group used combined genomic and proteomic analyses of Akt-MSCs vs native MSCs9 and reported that approximately 650 transcripts were differentially regulated between Akt-MSCs and control MSCs. A sub-analysis of the data, focused on potential cytoprotective genes, revealed 62 transcripts encoding for 51 unique genes potentially contributing to the paracrine effects of Akt-MSCs (Table 2). Among these genes, the secreted frizzled related protein 2 (Sfrp2) was the most dramatically up-regulated9. We then showed that Sfrp2 exerts multiple biologic effects including cardiac protection9, 33. Indeed, we have demonstrated that administration of Sfrp2 alone protects ischemic cardiomyocytes and that the prosurvival effect of Akt-MSCs was markedly attenuated upon knockdown of Sfrp2 with siRNA. Furthermore, we have shown that the mechanism of action of Sfrp2 is through modulation of Wnt signaling pathway. Using the same approach, we have also discovered several novel factors that are expressed in the Akt activated stem cells whose nature and importance are under intense investigation (Table 3). A comprehensive characterization of the paracrine factors and their pathways will allow the identification of possible novel therapeutical targets and/or drugs.
Table 2.
Genes coding for known secreted proteins differentially expressed in Akt-MSC versus control MSC under normoxic or hypoxic conditions
| Gene title | Gene symbol | GO biological process description |
|---|---|---|
| Inhibin beta-B | Inhbb | cell growth and/or maintenance |
| Bone morphogenetic protein 2 | Bmp2 | TGFbeta receptor signaling pathway /// embryonic development /// organogenesis /// cell fate commitment |
| A disintegrin-like and metalloprotease (reprolysin type) with thrombospondin type 1 motif, 5 (aggrecanase-2) | Adamts5 | proteolysis and peptidolysis /// protein amino acid prenylation |
| kit ligand/stem cell factor | Kitl | cell adhesion /// germ-cell development |
| Proliferin | Plf | angiogenesis |
| Lipoprotein lipase | Lpl | lipid metabolism /// lipid catabolism |
| c-fos induced growth factor | Figf | regulation of cell cycle /// angiogenesis /// cell growth and/or maintenance /// cell proliferation |
| Immunoglobulin superfamily containing leucine-rich repeat | Islr | cell adhesion |
| Cysteine-rich motor neuron 1 | Crim1 | regulation of cell growth |
| Fibronectin 1 | Fn1 | acute-phase response /// cell adhesion /// metabolism /// wound healing |
| Secreted protein SST3 | SST3 | --- |
| Latent transforming growth factor beta binding protein 2 | Ltbp2 | extracellular transport /// protein secretion /// protein targeting /// transforming growth factor beta receptor signaling pathway |
| Arginyl aminopeptidase (aminopeptidase B) | Rnpep | proteolysis and peptidolysis |
| Thrombospondin 1 | Thbs1 | cell adhesion /// negative regulation of angiogenesis |
| Matrix metalloproteinase 11 | Mmp11 | proteolysis and peptidolysis /// collagen catabolism |
| Angiogenin | Ang | angiogenesis |
| Thrombospondin 2 | Thbs2 | cell adhesion |
| Mannan-binding lectin serine protease 1 | Masp1 | proteolysis and peptidolysis /// complement activation, classical pathway |
| Fibulin 5 | Fbln5 | cell adhesion |
| Chemokine (C-X-C motif) ligand 12 | Cxcl12 | chemotaxis /// immune response /// brain development /// regulation of cell migration /// T-cell proliferation |
| Carboxypeptidase E | Cpe | proteolysis and peptidolysis |
| Connective tissue growth factor | Ctgf | ossification /// angiogenesis /// regulation of cell growth /// DNA metabolism /// cell adhesion /// cell-matrix adhesion /// integrin-mediated signaling pathway /// FGF receptor signaling pathway /// cell migration |
| Platelet derived growth factor, alpha | Pdgfa | regulation of cell cycle /// cell growth and/or maintenance /// cell proliferation |
| Angiotensinogen | Agt | regulation of blood pressure |
| Chemokine (C-C motif) ligand 7 | Ccl7 | transport /// chemotaxis /// inflammatory response /// immune response /// signal transduction |
| Cysteine-rich protein 61 | Cyr61 | regulation of cell growth /// patterning of blood vessels /// chemotaxis /// cell adhesion |
| Osteoglycin | Ogn | growth factor activity |
| Chemokine (C-C motif) ligand 2 | Ccl2 | chemotaxis /// inflammatory response /// immune response /// signal transduction |
| Angiopoietin-like 4 | Angptl4 | angiogenesis /// cell differentiation /// cellular response to starvation /// multicellular organismal development /// negative regulation of apoptosis /// negative regulation of lipoprotein lipase activity /// positive regulation of angiogenesis /// positive regulation of lipid metabolic process /// response to hypoxia /// signal transduction |
| Insulin-like growth factor binding protein 4 | Igfbp4 | regulation of cell growth |
| Apolipoprotein D | Apod | transport |
| Mesoderm-specific transcript | Mest | proteolysis and peptidolysis /// xenobiotic metabolism /// response to toxin |
| Secreted frizzled-related sequence protein 1 | Sfrp1 | development |
| Angiopoietin 4 | Agpt4 | transmembrane receptor protein tyrosine kinase signaling pathway /// endoderm development |
| Matrix metalloproteinase 13 | Mmp13 | proteolysis and peptidolysis /// collagen catabolism |
| Superoxide dismutase 3, extracellular | Sod3 | superoxide metabolism |
| Sema domain, immunoglobulin domain (Ig), short basic domain, secreted, (semaphorin) 3C | Sema3c | development /// neurogenesis |
| Hepatocyte growth factor | Hgf | cellular morphogenesis /// proteolysis and peptidolysis /// cell proliferation |
| Leucine-rich repeat containing 17 | Lrrc17 | --- |
| Lysyl oxidase-like 2 | Loxl2 | aging /// cell adhesion /// protein modification process |
| Interferon, alpha-inducible protein | G1p2 | immune response |
| Secreted frizzled-related sequence protein 3 | Sfrp3 | development |
| Interferon-inducible GTPase 1 | Iigp1 | cytokine and chemokine mediated signaling pathway |
| Vascular endothelial growth factor A | Vegfa | regulation of cell cycle /// angiogenesis /// cell growth and/or maintenance /// cell proliferation |
| Adrenomedullin | Adm | neuropeptide signaling pathway |
| Adipsin | Adn | proteolysis and peptidolysis /// complement activation, alternative pathway |
| Pleiotrophin | Ptn | ossification /// learning /// cell proliferation /// bone mineralization |
| Serine (or cysteine) proteinase inhibitor, clade E, member 1 | Serpine1 | blood coagulation /// fibrinolysis |
| Secreted frizzled-related sequence protein 2 | Sfrp2 | development |
Table 3.
Genes coding for novel secreted proteins differentially expressed in Akt-MSC versus control MSC under normoxic or hypoxic conditions
| Novel Gene | Molecular weight of protein (kDa) | Putative Function |
|---|---|---|
| Gene 1 | 60 | Angiogenic factor |
| Gene 5 | 15 | ECRG4 (Esophageal Cancer Related Gene 4) |
| Gene 8 | 120 | Extracellular glycoprotein (2 fibronectin domains & Abl3-BP) |
| Gene 12 | 40 | Survival factor (activates novel kinase for AKT) |
| Gene 13 | 7 | Not known |
Finally, these stem cell release factors have been shown to exert autocrine effects on the cells themselves, influencing cell survival, self renewal, cell growth33. The identification and characterization of the autocrine factors may improve our understanding of how stem cells regulate their own fate, behaviour, stemness, lineage commitment and many aspect of their biology. Thus, future research on the autocrine-paracrine paradigm can significantly increase our understanding of the biology and actions of stem cells.
Future directions in stem cell therapy for the heart
Cell therapy
Despite the encouraging results regarding the therapeutic potential of ASCs to treat heart disease, many obstacles are in the way of broad clinical application. A major issue is represented by the choice of cell type to administer. We believe that this decision should be influenced to a large extent by the nature of the injury. For example, if the goal is to rescue non-necrotic ischemic myocardium, it may be desirable to use an ASC type that secretes cytoprotective factors or to use EPCs to induce vascular regeneration. On the other hand, if the purpose is to regenerate infarcted myocardium, it would be more appropriate to use an undifferentiated cell type with cardiomyogenic and vasculogenic potentiality. However, this choice is complicated by the fact that we still do not clearly know the cardiomyogenic potentiality of each ASC type. As anticipated, certain ASC subsets more readily differentiate to a cardiomyogenic lineage but questions remain about stem cell plasticity and the frequency of cardiac differentiation events. The challenge will be to identify the comprehensive biochemical and environmental cues controlling this process so as to optimize cardiac differentiation. Past studies have relied almost exclusively on morphological and molecular evidence to demonstrate a cell fate change to a cardiomyogenic lineage following manipulation in culture or transplantation into living animals. Future experimental studies, both in vitro and in vivo, will require demonstration that the transplanted cells differentiate, integrate and functionally contribute to improve cardiac function.
Another problem is the extensive loss of the cells once transplanted. Regardless of cell type, many studies have shown that the majority of cells successfully delivered to the heart die within the first weeks19, 23, 40, 64, 65. To overcome this challenge, investigators have transplanted extremely large number of cells in experimental settings. However, translating the same doses of cells in humans would be difficult in some cases. For example, some specific cell populations, like Lin− cKit+ HSCs or SP cells, are extremely rare and cannot be expanded ex vivo. In those cases translating experimental results to the bed side may represent a difficult task. The causes of cell death in AMI setting are multifactorial and are influenced by the ischemic environment, which is devoid of nutrients and oxygen, coupled with the loss of survival signals from matrix attachments and cell-cell interactions. We and others have conceptualized the idea of improving cell survival by overexpressing protective genes. To optimize this approach, in the future, one may use viral vectors encoding multiple cytoprotective genes, acting on different cell death and apoptosis pathways. Recently, it has been proposed that preconditioning of ASCs with different cytokines may result in improved cell engraftment66. The combination of genetic modification and preconditioning may further enhance cell survival and engraftment. An alternative method would be to seed cell ex vivo on a biodegradable polymeric scaffold followed by in vivo engraftment instead of injecting the cells directly into the site of injury67. Improvement of ASC survival will ultimately allow to address cell scalability, and to make cell-based therapies more easily applicable to humans.
Importantly, the question of whether cell administration in patients suffering AMI should be performed immediately after infarction or after the inflammatory process has subsided is not completely resolved. While experimental data would support early administration, data from the largest randomized clinical trial performed so far (the REPAIR-AMI) showed progressive increase in cell-associated recovery of contractile function as the interval between reperfusion therapy and cell infusion increased68. In particular, the beneficial effects of cell infusion on the recovery of contractile function were confined to patients who were treated more than 4 days after infarct reperfusion, whereas no benefit was observed in patients treated up to day 4 after reperfusion. Prospective trials designed specifically to address this important issue are mandatory.
Safety concerns regarding the pro-arrhythmic effects following transplantation of ASCs for cardiac repair must be taken into consideration. So far BM-derived stem cells have not shown pro-arrhythmic effects in early clinical trials. However, it is not known whether increasing the number of cells that survive or the number of the cells injected will provoke an arrythmogenic reaction. Tailored pre-clinical studies should be carried out in small and large animal models with the specific aim to rule completely out that ASCs can induce arrhythmias.
Other unresolved issues are the efficacy and safety concerns surrounding the changes in gene expression and functional properties of ASCs with advancing age and disease69. The properties of self-renewal and lineage potentiality of cells harvested from high-risk patients may be affected. We know that both the age and the presence of disease status adversely influence several aspects of the intrinsic characteristics of ASCs. For instance, EPCs from patients with cardiovascular disease display varying degrees of functional impairment and an inverse correlation has been reported between the number of circulating EPCs and the prevalence of risk factors for CAD70. These deficiencies may limit in some settings the therapeutic application of individualized treatment strategy using the patient’s own isolated cells. To by-pass these problems, using allogenic cells from young and healthy donors or even cells of fetal origin may represent a good solution. Unfortunately, cell rejection would pose a new problem, requiring immunosuppressive therapies. Interestingly, it has been shown that MSCs display an immunoprivileged phenotype and may not be subject to allogeneic rejection in humans and animals18, 71, 72. Manipulation of telomerase may represent a possible strategy to rejuvenate senescent autologous cells73.
Importantly, it should not be overlooked the fact that, in the stem cell analysis, obtaining consistent results among different laboratories still represents a major problem. The use of different cell types, growth conditions, the passaging methods used, and the number of cell passage considered are just some of the variables influencing stem cell research. The introduction of standard operating procedures and nomenclature will be mandatory in order to optimise our understanding of stem cell biology and clarify the mechanisms of stem cell action. Furthermore, standardization of genomic and proteomic methodologies and strategies between different groups of investigators would facilitate the comparability of the results. In addition, the establishment of shared databases able to contain the everincreasing amount of data generated by genomics and proteomics studies of stem cells will be mandatory. Several initiatives were already set up to characterize numerous existing human embryonic stem cell lines using standardized assay conditions to allow unrestrained comparison of the data sets generated74, 75. The NIH Stem Cell Unit adopted its own initiative (http://stemcells.nih.gov/research/nihresearch/scunit). We envision that similar approaches will be considered also for ASCs in the near future. Combined, the various genomic and proteomic approaches will continue to reveal crucial insights into stem cell biology and consequently on their potential use for tissue reparative therapies.
Enhancing beneficial paracrine effects through genetic modification
The observation that BM-derived stem cells, particularly those which are genetically modified, may release of therapeutic paracrine factors provide an important conceptual advancement in that one can enhance stem cell therapeutic actions through gene transfer. In this context, Akt-MSCs revealed themselves as a useful model to identify possible novel therapeutic molecules, suggesting that genetic modification of stem or progenitor cells may represent an important strategic advancement in regenerative medicine. By combining gene with cell therapy, one may be able to enhance stem cell function and viability. Indeed, genetic modification can improve survival, metabolic characteristics, proliferative capacity, or differentiation of the stem cells. Furthermore, the cells may become a vehicle for gene therapy whose secreted gene products can exert paracrine or endocrine actions that may result in further therapeutic benefits. Our group was the first to conceptualize this approach76, 77 and showed that genetically modified EPCs had greater reparative potential and that MSCs overexpressing the prosurvival gene Akt-1 had greater post-implantation survival and functional benefits than did wild-type cells. Thought as a strategy to increase cell viability, the overexpression of Akt turned out to have many more effects on MSCs such as the production of secreted factors capable of protecting ARVCs both in vitro and in vivo. The salutary effects of this approach have been further validated and extended by several groups. BCL-2 engineered MSCs were shown to increase the survival of the MSCs after AMI in rats, leading to higher expression level of VEGF, increased capillary density and smaller infarct size relative to controls78. Tang and collaborators79 found that a higher number of MSCs transduced with heme oxygenase (HO)-1 survived when they are injected into infarcted hearts, leading to more efficient healing compared with control MSCs. Based on the data reported, the beneficial effects obtained with the HO-1-MSCs appear also to be primarily due to paracrine protective action, even though this hypothesis was not directly addressed in this study. Indeed, the low differentiation rate of MSCs into cardiomyocytes suggested by the authors could not alone explain the structural and functional improvements reported. Thus, as in the case of the Akt-MSCs, the original intervention, intended to increase stem cell viability, might have induced paracrine effects on adjacent myocardium. Similarly, HGF80, bFGF81, adrenomedullin82 or VEGF-engineered MSCs83 were shown to survive better and to exert more powerful cytoprotection and/or pro-neovascularization effect compared with control MSCs.
Protein and molecular therapies
The demonstration that stem cells may secrete therapeutic factors provides a potential breakthrough in that, rather than administering cells, one may be able to administer specific proteins produced by these cells for cardiac therapy. It is important to keep in mind that there are therapies currently used to treat post-AMI heart failure leading to improvement of cardiac function without inducing regeneration: angiotensin-converting enzyme inhibitors represent the best example84. On the other hand it is possible that factors released by transplanted cells may influence the microenviroment maintaining stem cell niches in the heart or may activate cardiac progenitors and induce their migration and differentiation. Tailored studies analyzing the fate of both exogenous transplanted cells and resident cardiac progenitors will help to clarify the specific role of these cell populations in heart repair.
Transplantation of stem cells for their paracrine effects still represents a reasonable strategy because the beneficial factors remain partly unidentified and because multiple factors might be functioning synergistically. However, if specific paracrine cell-derived factors that improve cardiac function will be identified, then protein-based therapy might be more easily translated into clinical benefits than cell-based therapy. A known quantity of protein can be administered using intravenous, intra-coronary, or intramyocardial approaches. The most obvious limitation of protein therapy is the necessity to maintain therapeutic concentration in order to induce the desired effect for the necessary length of time. Establishing the threshold concentration and the necessary time remains to be determined and represents a difficult task. Different actions may require different concentrations and timing. Substantial differences between animal models and humans further complicate the scenario. For example, it has been shown that a single dose of specific growth factors is effective in enhancing neovascularization in animals but not in humans85, 86. Protein stability and pharmacokinetic represent other possible hurdles. To overcome these problems a variety of strategies have emerged for manipulating protein properties, stability, specificity, immunogenicity and pharmacokinetic87. Mechanisms for altering these properties include manipulation of primary structure, incorporation of chemical and post-translation modifications and utilization of fusion partner. The protein and peptide therapeutics have already become an important class of drugs due to advancement in molecular biology and recombinant technology. Currently, most of therapeutic proteins are administered by the parenteral route which has many drawbacks. Various delivery strategies have evolved over the past few years to improve delivery of proteins and peptides, including the use of biopolymers and nanomaterials for controlled release of proteins88, 89, and delivery via non-invasive routes such as subcutaneous release or dermal patches. The non-invasive approach remains challenging due to poor absorption and enzymatic instability, pharmacokinetics and pharmacodynamics of protein therapeutics. Development of an oral dosage form for protein therapeutics is still the most desirable one but with greater challenge. Even though the road to reach optimal protein therapy is full of hurdles, we anticipate that the constant development and application of rational protein design technology will enable significant improvements in the efficacy and safety of existing protein therapeutics, as well as allow the generation of entirely novel classes of proteins and mode of action. In this case, curing AMI with a single protein or, most likely, with a cocktail of proteins may become reality.
Conclusion
The demonstration of paracrine/autocrine mechanisms improves our understanding of stem cell biology and stem cell action in tissue repair and regeneration. Although stem cell therapy holds promise in the future treatment of heart disease such as AMI, chronic ischemic heart disease, and congestive heart failure, its current use is significantly hampered by biologic and technologic challenges. Genetic modification of stem cells represents an important advancement because this approach may overcome the issue of cell viability, scalability, immune tolerance and enhanced functions. Furthermore, the recent demonstration that genetically modified cells may secrete novel therapeutic factors provides a potential strategy in that, rather than administering cells, one may be able to administer specific proteins produced by these cells for cardiac therapy.
Acknowledgments
This work was supported by grants from the National Heart, Lung, and Blood Institute (RO1 HL35610, HL81744, HL72010, and HL73219 to Victor J. Dzau), the Edna Mandel Foundation and the Foundation Leducq (to Victor J. Dzau). Massimiliano Gnecchi is supported by the Fondazione IRCCS Policlinico San Matteo Pavia, Italy and by grants from the Ministero Italiano dell’Università e della Ricerca (MIUR), from the Ministero Italiano della Sanità, from the Fondazione Cariplo, and from the Fondazione Banca del Monte di Lombardia.
Footnotes
Disclosure: None
References
- 1.Quaini F, Urbanek K, Beltrami AP, Finato N, Beltrami CA, Nadal-Ginard B, Kajstura J, Leri A, Anversa P. Chimerism of the transplanted heart. N Engl J Med. 2002;346:5–15. doi: 10.1056/NEJMoa012081. [DOI] [PubMed] [Google Scholar]
- 2.Beltrami AP, Urbanek K, Kajstura J, Yan SM, Finato N, Bussani R, Nadal-Ginard B, Silvestri F, Leri A, Beltrami CA, Anversa P. Evidence that human cardiac myocytes divide after myocardial infarction. N Engl J Med. 2001;344:1750–1757. doi: 10.1056/NEJM200106073442303. [DOI] [PubMed] [Google Scholar]
- 3.Beltrami AP, Barlucchi L, Torella D, Baker M, Limana F, Chimenti S, Kasahara H, Rota M, Musso E, Urbanek K, Leri A, Kajstura J, Nadal-Ginard B, Anversa P. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell. 2003;114:763–776. doi: 10.1016/s0092-8674(03)00687-1. [DOI] [PubMed] [Google Scholar]
- 4.Deb A, Wang S, Skelding KA, Miller D, Simper D, Caplice NM. Bone marrow-derived cardiomyocytes are present in adult human heart: A study of gender-mismatched bone marrow transplantation patients. Circulation. 2003;107:1247–1249. doi: 10.1161/01.cir.0000061910.39145.f0. [DOI] [PubMed] [Google Scholar]
- 5.Jackson KA, Majka SM, Wang H, Pocius J, Hartley CJ, Majesky MW, Entman ML, Michael LH, Hirschi KK, Goodell MA. Regeneration of ischemic cardiac muscle and vascular endothelium by adult stem cells. J Clin Invest. 2001;107:1395–1402. doi: 10.1172/JCI12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caplice NM, Deb A. Myocardial-cell replacement: the science, the clinic and the future. Nat Clin Pract Cardiovasc Med. 2004;1:90–95. doi: 10.1038/ncpcardio0051. [DOI] [PubMed] [Google Scholar]
- 7.Dimmeler S, Zeiher AM, Schneider MD. Unchain my heart: the scientific foundations of cardiac repair. J Clin Invest. 2005;115:572–583. doi: 10.1172/JCI24283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Melo LG, Pachori AS, Kong D, Gnecchi M, Wang K, Pratt RE, Dzau VJ. Molecular and cell-based therapies for protection, rescue, and repair of ischemic myocardium: reasons for cautious optimism. Circulation. 2004;109:2386–2393. doi: 10.1161/01.CIR.0000128597.37025.00. [DOI] [PubMed] [Google Scholar]
- 9.Mirotsou M, Zhang Z, Deb A, Zhang L, Gnecchi M, Noiseux N, Mu H, Pachori A, Dzau V. Secreted frizzled related protein 2 (Sfrp2) is the key Akt-mesenchymal stem cell-released paracrine factor mediating myocardial survival and repair. Proc Natl Acad Sci U S A. 2007;104:1643–1648. doi: 10.1073/pnas.0610024104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith RR, Barile L, Cho HC, Leppo MK, Hare JM, Messina E, Giacomello A, Abraham MR, Marban E. Regenerative potential of cardiosphere-derived cells expanded from percutaneous endomyocardial biopsy specimens. Circulation. 2007;115:896–908. doi: 10.1161/CIRCULATIONAHA.106.655209. [DOI] [PubMed] [Google Scholar]
- 11.Messina E, De Angelis L, Frati G, Morrone S, Chimenti S, Fiordaliso F, Salio M, Battaglia M, Latronico MV, Coletta M, Vivarelli E, Frati L, Cossu G, Giacomello A. Isolation and expansion of adult cardiac stem cells from human and murine heart. Circ Res. 2004;95:911–921. doi: 10.1161/01.RES.0000147315.71699.51. [DOI] [PubMed] [Google Scholar]
- 12.Oh H, Bradfute SB, Gallardo TD, Nakamura T, Gaussin V, Mishina Y, Pocius J, Michael LH, Behringer RR, Garry DJ, Entman ML, Schneider MD. Cardiac progenitor cells from adult myocardium: homing, differentiation, and fusion after infarction. Proc Natl Acad Sci U S A. 2003;100:12313–12318. doi: 10.1073/pnas.2132126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parmacek MS, Epstein JA. Pursuing cardiac progenitors: regeneration redux. Cell. 2005;120:295–298. doi: 10.1016/j.cell.2005.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Leri A, Kajstura J, Anversa P. Cardiac stem cells and mechanisms of myocardial regeneration. Physiol Rev. 2005;85:1373–1416. doi: 10.1152/physrev.00013.2005. [DOI] [PubMed] [Google Scholar]
- 15.Kawamoto A, Gwon HC, Iwaguro H, Yamaguchi JI, Uchida S, Masuda H, Silver M, Ma H, Kearney M, Isner JM, Asahara T. Therapeutic potential of ex vivo expanded endothelial progenitor cells for myocardial ischemia. Circulation. 2001;103:634–637. doi: 10.1161/01.cir.103.5.634. [DOI] [PubMed] [Google Scholar]
- 16.Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, Pickel J, McKay R, Nadal-Ginard B, Bodine DM, Leri A, Anversa P. Bone marrow cells regenerate infarcted myocardium. Nature. 2001;410:701–705. doi: 10.1038/35070587. [DOI] [PubMed] [Google Scholar]
- 17.Tomita S, Li RK, Weisel RD, Mickle DA, Kim EJ, Sakai T, Jia ZQ. Autologous transplantation of bone marrow cells improves damaged heart function. Circulation. 1999;100:II247–256. doi: 10.1161/01.cir.100.suppl_2.ii-247. [DOI] [PubMed] [Google Scholar]
- 18.Pittenger MF, Martin BJ. Mesenchymal stem cells and their potential as cardiac therapeutics. Circ Res. 2004;95:9–20. doi: 10.1161/01.RES.0000135902.99383.6f. [DOI] [PubMed] [Google Scholar]
- 19.Balsam LB, Wagers AJ, Christensen JL, Kofidis T, Weissman IL, Robbins RC. Haematopoietic stem cells adopt mature haematopoietic fates in ischaemic myocardium. Nature. 2004;428:668–673. doi: 10.1038/nature02460. [DOI] [PubMed] [Google Scholar]
- 20.Murry CE, Soonpaa MH, Reinecke H, Nakajima H, Nakajima HO, Rubart M, Pasumarthi KB, Virag JI, Bartelmez SH, Poppa V, Bradford G, Dowell JD, Williams DA, Field LJ. Haematopoietic stem cells do not transdifferentiate into cardiac myocytes in myocardial infarcts. Nature. 2004;428:664–668. doi: 10.1038/nature02446. [DOI] [PubMed] [Google Scholar]
- 21.Alvarez-Dolado M, Pardal R, Garcia-Verdugo JM, Fike JR, Lee HO, Pfeffer K, Lois C, Morrison SJ, Alvarez-Buylla A. Fusion of bone-marrow-derived cells with Purkinje neurons, cardiomyocytes and hepatocytes. Nature. 2003;425:968– 973. doi: 10.1038/nature02069. [DOI] [PubMed] [Google Scholar]
- 22.Nygren JM, Jovinge S, Breitbach M, Sawen P, Roll W, Hescheler J, Taneera J, Fleischmann BK, Jacobsen SE. Bone marrow-derived hematopoietic cells generate cardiomyocytes at a low frequency through cell fusion, but not transdifferentiation. Nat Med. 2004;10:494–501. doi: 10.1038/nm1040. [DOI] [PubMed] [Google Scholar]
- 23.Noiseux N, Gnecchi M, Lopez-Ilasaca M, Zhang L, Solomon SD, Deb A, Dzau VJ, Pratt RE. Mesenchymal stem cells overexpressing Akt dramatically repair infarcted myocardium and improve cardiac function despite infrequent cellular fusion or differentiation. Mol Ther. 2006;14:840–850. doi: 10.1016/j.ymthe.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Kajstura J, Rota M, Whang B, Cascapera S, Hosoda T, Bearzi C, Nurzynska D, Kasahara H, Zias E, Bonafe M, Nadal-Ginard B, Torella D, Nascimbene A, Quaini F, Urbanek K, Leri A, Anversa P. Bone marrow cells differentiate in cardiac cell lineages after infarction independently of cell fusion. Circ Res. 2005;96:127–137. doi: 10.1161/01.RES.0000151843.79801.60. [DOI] [PubMed] [Google Scholar]
- 25.Gnecchi M, He H, Liang OD, Melo LG, Morello F, Mu H, Noiseux N, Zhang L, Pratt RE, Ingwall JS, Dzau VJ. Paracrine action accounts for marked protection of ischemic heart by Akt-modified mesenchymal stem cells. Nat Med. 2005;11:367–368. doi: 10.1038/nm0405-367. [DOI] [PubMed] [Google Scholar]
- 26.Gnecchi M, He H, Noiseux N, Liang OD, Zhang L, Morello F, Mu H, Melo LG, Pratt RE, Ingwall JS, Dzau VJ. Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. Faseb J. 2006;20:661–669. doi: 10.1096/fj.05-5211com. [DOI] [PubMed] [Google Scholar]
- 27.Kinnaird T, Stabile E, Burnett MS, Shou M, Lee CW, Barr S, Fuchs S, Epstein SE. Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation. 2004;109:1543–1549. doi: 10.1161/01.CIR.0000124062.31102.57. [DOI] [PubMed] [Google Scholar]
- 28.Caplan AI, Dennis JE. Mesenchymal stem cells as trophic mediators. J Cell Biochem. 2006;98:1076–1084. doi: 10.1002/jcb.20886. [DOI] [PubMed] [Google Scholar]
- 29.Kinnaird T, Stabile E, Burnett MS, Lee CW, Barr S, Fuchs S, Epstein SE. Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ Res. 2004;94:678–685. doi: 10.1161/01.RES.0000118601.37875.AC. [DOI] [PubMed] [Google Scholar]
- 30.Yoon YS, Wecker A, Heyd L, Park JS, Tkebuchava T, Kusano K, Hanley A, Scadova H, Qin G, Cha DH, Johnson KL, Aikawa R, Asahara T, Losordo DW. Clonally expanded novel multipotent stem cells from human bone marrow regenerate myocardium after myocardial infarction. J Clin Invest. 2005;115:326–338. doi: 10.1172/JCI22326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nagaya N, Kangawa K, Itoh T, Iwase T, Murakami S, Miyahara Y, Fujii T, Uematsu M, Ohgushi H, Yamagishi M, Tokudome T, Mori H, Miyatake K, Kitamura S. Transplantation of mesenchymal stem cells improves cardiac function in a rat model of dilated cardiomyopathy. Circulation. 2005;112:1128–1135. doi: 10.1161/CIRCULATIONAHA.104.500447. [DOI] [PubMed] [Google Scholar]
- 32.Takahashi M, Li TS, Suzuki R, Kobayashi T, Ito H, Ikeda Y, Matsuzaki M, Hamano K. Cytokines produced by bone marrow cells can contribute to functional improvement of the infarcted heart by protecting cardiomyocytes from ischemic injury. Am J Physiol Heart Circ Physiol. 2006;291:H886–893. doi: 10.1152/ajpheart.00142.2006. [DOI] [PubMed] [Google Scholar]
- 33.Deb A, Davis BH, Guo J, Ni A, Huang J, Zhang Z, Mu H, Dzau VJ. SFRP2 regulates cardiomyogenic differentiation by inhibiting a positive transcriptional autofeedback loop of Wnt3a. Stem Cells. 2008;26:35–44. doi: 10.1634/stemcells.2007-0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim SY, Kim YS, Ahn Y, Jeong MH, Hong MH, Joo SY, Nam KI, Cho JG, Kang PM, Park JC. The effects of mesenchymal stem cells transduced with Akt in a porcine myocardial infarction model. Cardiovasc Res. 2006;70:530–542. doi: 10.1016/j.cardiores.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 35.Uemura R, Xu M, Ahmad N, Ashraf M. Bone marrow stem cells prevent left ventricular remodeling of ischemic heart through paracrine signaling. Circ Res. 2006;98:1414–1421. doi: 10.1161/01.RES.0000225952.61196.39. [DOI] [PubMed] [Google Scholar]
- 36.Xu M, Uemura R, Dai Y, Wang Y, Pasha Z, Ashraf M. In vitro and in vivo effects of bone marrow stem cells on cardiac structure and function. J Mol Cell Cardiol. 2007;42:441–448. doi: 10.1016/j.yjmcc.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kubal C, Sheth K, Nadal-Ginard B, Galinanes M. Bone marrow cells have a potent anti-ischemic effect against myocardial cell death in humans. J Thorac Cardiovasc Surg. 2006;132:1112–1118. doi: 10.1016/j.jtcvs.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 38.Kamihata H, Matsubara H, Nishiue T, Fujiyama S, Tsutsumi Y, Ozono R, Masaki H, Mori Y, Iba O, Tateishi E, Kosaki A, Shintani S, Murohara T, Imaizumi T, Iwasaka T. Implantation of bone marrow mononuclear cells into ischemic myocardium enhances collateral perfusion and regional function via side supply of angioblasts, angiogenic ligands, and cytokines. Circulation. 2001;104:1046–1052. doi: 10.1161/hc3501.093817. [DOI] [PubMed] [Google Scholar]
- 39.Ohnishi S, Yasuda T, Kitamura S, Nagaya N. Effect of hypoxia on gene expression of bone marrow-derived mesenchymal stem cells and mononuclear cells. Stem Cells. 2007;25:1166–1177. doi: 10.1634/stemcells.2006-0347. [DOI] [PubMed] [Google Scholar]
- 40.Jiang S, Haider H, Idris NM, Salim A, Ashraf M. Supportive interaction between cell survival signaling and angiocompetent factors enhances donor cell survival and promotes angiomyogenesis for cardiac repair. Circ Res. 2006;99:776–784. doi: 10.1161/01.RES.0000244687.97719.4f. [DOI] [PubMed] [Google Scholar]
- 41.Nagaya N, Fujii T, Iwase T, Ohgushi H, Itoh T, Uematsu M, Yamagishi M, Mori H, Kangawa K, Kitamura S. Intravenous administration of mesenchymal stem cells improves cardiac function in rats with acute myocardial infarction through angiogenesis and myogenesis. Am J Physiol Heart Circ Physiol. 2004;287:H2670–2676. doi: 10.1152/ajpheart.01071.2003. [DOI] [PubMed] [Google Scholar]
- 42.Tomita S, Mickle DA, Weisel RD, Jia ZQ, Tumiati LC, Allidina Y, Liu P, Li RK. Improved heart function with myogenesis and angiogenesis after autologous porcine bone marrow stromal cell transplantation. J Thorac Cardiovasc Surg. 2002;123:1132–1140. doi: 10.1067/mtc.2002.120716. [DOI] [PubMed] [Google Scholar]
- 43.Urbich C, Aicher A, Heeschen C, Dernbach E, Hofmann WK, Zeiher AM, Dimmeler S. Soluble factors released by endothelial progenitor cells promote migration of endothelial cells and cardiac resident progenitor cells. J Mol Cell Cardiol. 2005;39:733–742. doi: 10.1016/j.yjmcc.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 44.Aicher A, Brenner W, Zuhayra M, Badorff C, Massoudi S, Assmus B, Eckey T, Henze E, Zeiher AM, Dimmeler S. Assessment of the tissue distribution of transplanted human endothelial progenitor cells by radioactive labeling. Circulation. 2003;107:2134–2139. doi: 10.1161/01.CIR.0000062649.63838.C9. [DOI] [PubMed] [Google Scholar]
- 45.Kawamoto A, Tkebuchava T, Yamaguchi J, Nishimura H, Yoon YS, Milliken C, Uchida S, Masuo O, Iwaguro H, Ma H, Hanley A, Silver M, Kearney M, Losordo DW, Isner JM, Asahara T. Intramyocardial transplantation of autologous endothelial progenitor cells for therapeutic neovascularization of myocardial ischemia. Circulation. 2003;107:461–468. doi: 10.1161/01.cir.0000046450.89986.50. [DOI] [PubMed] [Google Scholar]
- 46.Wu Y, Ip JE, Huang J, Zhang L, Matsushita K, Liew CC, Pratt RE, Dzau VJ. Essential role of ICAM-1/CD18 in mediating EPC recruitment, angiogenesis, and repair to the infarcted myocardium. Circ Res. 2006;99:315–322. doi: 10.1161/01.RES.0000235986.35957.a3. [DOI] [PubMed] [Google Scholar]
- 47.Berry MF, Engler AJ, Woo YJ, Pirolli TJ, Bish LT, Jayasankar V, Morine KJ, Gardner TJ, Discher DE, Sweeney HL. Mesenchymal stem cell injection after myocardial infarction improves myocardial compliance. Am J Physiol Heart Circ Physiol. 2006;290:H2196–2203. doi: 10.1152/ajpheart.01017.2005. [DOI] [PubMed] [Google Scholar]
- 48.Ortiz LA, Gambelli F, McBride C, Gaupp D, Baddoo M, Kaminski N, Phinney DG. Mesenchymal stem cell engraftment in lung is enhanced in response to bleomycin exposure and ameliorates its fibrotic effects. Proc Natl Acad Sci U S A. 2003;100:8407–8411. doi: 10.1073/pnas.1432929100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oyagi S, Hirose M, Kojima M, Okuyama M, Kawase M, Nakamura T, Ohgushi H, Yagi K. Therapeutic effect of transplanting HGF-treated bone marrow mesenchymal cells into CCl4-injured rats. J Hepatol. 2006;44:742–748. doi: 10.1016/j.jhep.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 50.Ninichuk V, Gross O, Segerer S, Hoffmann R, Radomska E, Buchstaller A, Huss R, Akis N, Schlondorff D, Anders HJ. Multipotent mesenchymal stem cells reduce interstitial fibrosis but do not delay progression of chronic kidney disease in collagen4A3-deficient mice. Kidney Int. 2006;70:121–129. doi: 10.1038/sj.ki.5001521. [DOI] [PubMed] [Google Scholar]
- 51.Xu X, Xu Z, Xu Y, Cui G. Effects of mesenchymal stem cell transplantation on extracellular matrix after myocardial infarction in rats. Coron Artery Dis. 2005;16:245–255. doi: 10.1097/00019501-200506000-00006. [DOI] [PubMed] [Google Scholar]
- 52.Ohnishi S, Sumiyoshi H, Kitamura S, Nagaya N. Mesenchymal stem cells attenuate cardiac fibroblast proliferation and collagen synthesis through paracrine actions. FEBS Lett. 2007;581:3961–3966. doi: 10.1016/j.febslet.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 53.Ramalho-Santos M, Yoon S, Matsuzaki Y, Mulligan RC, Melton DA. Stemness”: transcriptional profiling of embryonic and adult stem cells. Science. 2002;298:597–600. doi: 10.1126/science.1072530. [DOI] [PubMed] [Google Scholar]
- 54.Ohnishi S, Yanagawa B, Tanaka K, Miyahara Y, Obata H, Kataoka M, Kodama M, Ishibashi-Ueda H, Kangawa K, Kitamura S, Nagaya N. Transplantation of mesenchymal stem cells attenuates myocardial injury and dysfunction in a rat model of acute myocarditis. J Mol Cell Cardiol. 2007;42:88–97. doi: 10.1016/j.yjmcc.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 55.Fuse K, Kodama M, Hanawa H, Okura Y, Ito M, Shiono T, Maruyama S, Hirono S, Kato K, Watanabe K, Aizawa Y. Enhanced expression and production of monocyte chemoattractant protein-1 in myocarditis. Clin Exp Immunol. 2001;124:346–352. doi: 10.1046/j.1365-2249.2001.01510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990;81:1161–1172. doi: 10.1161/01.cir.81.4.1161. [DOI] [PubMed] [Google Scholar]
- 57.Freestone NS, Ribaric S, Mason WT. The effect of insulin-like growth factor-1 on adult rat cardiac contractility. Mol Cell Biochem. 1996;163–164:223–229. doi: 10.1007/BF00408662. [DOI] [PubMed] [Google Scholar]
- 58.Cittadini A, Stromer H, Katz SE, Clark R, Moses AC, Morgan JP, Douglas PS. Differential cardiac effects of growth hormone and insulin-like growth factor-1 in the rat. A combined in vivo and in vitro evaluation. Circulation. 1996;93:800–809. doi: 10.1161/01.cir.93.4.800. [DOI] [PubMed] [Google Scholar]
- 59.Duerr RL, Huang S, Miraliakbar HR, Clark R, Chien KR, Ross J., Jr Insulin-like growth factor-1 enhances ventricular hypertrophy and function during the onset of experimental cardiac failure. J Clin Invest. 1995;95:619–627. doi: 10.1172/JCI117706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dhein S, Garbade J, Rouabah D, Abraham G, Ungemach FR, Schneider K, Ullmann C, Aupperle H, Gummert JF, Mohr FW. Effects of autologous bone marrow stem cell transplantation on beta-adrenoceptor density and electrical activation pattern in a rabbit model of non-ischemic heart failure. J Cardiothorac Surg. 2006;1:17. doi: 10.1186/1749-8090-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feygin J, Mansoor A, Eckman P, Swingen C, Zhang J. Functional and bioenergetic modulations in the infarct border zone following autologous mesenchymal stem cell transplantation. Am J Physiol Heart Circ Physiol. 2007;293:H1772–1780. doi: 10.1152/ajpheart.00242.2007. [DOI] [PubMed] [Google Scholar]
- 62.Linke A, Muller P, Nurzynska D, Casarsa C, Torella D, Nascimbene A, Castaldo C, Cascapera S, Bohm M, Quaini F, Urbanek K, Leri A, Hintze TH, Kajstura J, Anversa P. Stem cells in the dog heart are self-renewing, clonogenic, and multipotent and regenerate infarcted myocardium, improving cardiac function. Proc Natl Acad Sci U S A. 2005;102:8966–8971. doi: 10.1073/pnas.0502678102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amado LC, Saliaris AP, Schuleri KH, St John M, Xie JS, Cattaneo S, Durand DJ, Fitton T, Kuang JQ, Stewart G, Lehrke S, Baumgartner WW, Martin BJ, Heldman AW, Hare JM. Cardiac repair with intramyocardial injection of allogeneic mesenchymal stem cells after myocardial infarction. Proc Natl Acad Sci U S A. 2005;102:11474–11479. doi: 10.1073/pnas.0504388102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Norol F, Bonnet N, Peinnequin A, Chretien F, Legrand R, Isnard R, Herodin F, Baillou C, Delache B, Negre D, Klatzmann D, Vernant JP, Lemoine FM. GFP-transduced CD34+ and Lin− CD34− hematopoietic stem cells did not adopt a cardiac phenotype in a nonhuman primate model of myocardial infarct. Exp Hematol. 2007;35:653–661. doi: 10.1016/j.exphem.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 65.Nakamura Y, Wang X, Xu C, Asakura A, Yoshiyama M, From AH, Zhang J. Xenotransplantation of long-term-cultured swine bone marrow-derived mesenchymal stem cells. Stem Cells. 2007;25:612–620. doi: 10.1634/stemcells.2006-0168. [DOI] [PubMed] [Google Scholar]
- 66.Pasha Z, Wang Y, Sheikh R, Zhang D, Zhao T, Ashraf M. Preconditioning enhances cell survival and differentiation of stem cells during transplantation in infarcted myocardium. Cardiovasc Res. 2008;77:134–142. doi: 10.1093/cvr/cvm025. [DOI] [PubMed] [Google Scholar]
- 67.Davis ME, Hsieh PC, Grodzinsky AJ, Lee RT. Custom design of the cardiac microenvironment with biomaterials. Circ Res. 2005;97:8–15. doi: 10.1161/01.RES.0000173376.39447.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schachinger V, Erbs S, Elsasser A, Haberbosch W, Hambrecht R, Holschermann H, Yu J, Corti R, Mathey DG, Hamm CW, Suselbeck T, Assmus B, Tonn T, Dimmeler S, Zeiher AM. Intracoronary bone marrow-derived progenitor cells in acute myocardial infarction. N Engl J Med. 2006;355:1210–1221. doi: 10.1056/NEJMoa060186. [DOI] [PubMed] [Google Scholar]
- 69.Rossi DJ, Bryder D, Zahn JM, Ahlenius H, Sonu R, Wagers AJ, Weissman IL. Cell intrinsic alterations underlie hematopoietic stem cell aging. Proc Natl Acad Sci U S A. 2005;102:9194–9199. doi: 10.1073/pnas.0503280102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dzau VJ, Gnecchi M, Pachori AS, Morello F, Melo LG. Therapeutic potential of endothelial progenitor cells in cardiovascular diseases. Hypertension. 2005;46:7–18. doi: 10.1161/01.HYP.0000168923.92885.f7. [DOI] [PubMed] [Google Scholar]
- 71.Ryan JM, Barry FP, Murphy JM, Mahon BP. Mesenchymal stem cells avoid allogeneic rejection. J Inflamm (Lond) 2005;2:8. doi: 10.1186/1476-9255-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barry FP, Murphy JM, English K, Mahon BP. Immunogenicity of adult mesenchymal stem cells: lessons from the fetal allograft. Stem Cells Dev. 2005;14:252–265. doi: 10.1089/scd.2005.14.252. [DOI] [PubMed] [Google Scholar]
- 73.Shay JW, Wright WE. Use of telomerase to create bioengineered tissues. Ann N Y Acad Sci. 2005;1057:479–491. doi: 10.1196/annals.1356.037. [DOI] [PubMed] [Google Scholar]
- 74.Rao MS, Civin CI. Translational research: toward better characterization of human embryonic stem cell lines. Stem Cells. 2005;23:1453. doi: 10.1634/stemcells.2005-ed.4. [DOI] [PubMed] [Google Scholar]
- 75.Andrews PW, Benvenisty N, McKay R, Pera MF, Rossant J, Semb H, Stacey GN. The International Stem Cell Initiative: toward benchmarks for human embryonic stem cell research. Nat Biotechnol. 2005;23:795–797. doi: 10.1038/nbt0705-795. [DOI] [PubMed] [Google Scholar]
- 76.Kong D, Melo LG, Mangi AA, Zhang L, Lopez-Ilasaca M, Perrella MA, Liew CC, Pratt RE, Dzau VJ. Enhanced inhibition of neointimal hyperplasia by genetically engineered endothelial progenitor cells. Circulation. 2004;109:1769–1775. doi: 10.1161/01.CIR.0000121732.85572.6F. [DOI] [PubMed] [Google Scholar]
- 77.Mangi AA, Noiseux N, Kong D, He H, Rezvani M, Ingwall JS, Dzau VJ. Mesenchymal stem cells modified with Akt prevent remodeling and restore performance of infarcted hearts. Nat Med. 2003;9:1195–1201. doi: 10.1038/nm912. [DOI] [PubMed] [Google Scholar]
- 78.Li W, Ma N, Ong LL, Nesselmann C, Klopsch C, Ladilov Y, Furlani D, Piechaczek C, Moebius JM, Lutzow K, Lendlein A, Stamm C, Li RK, Steinhoff G. Bcl-2 engineered MSCs inhibited apoptosis and improved heart function. Stem Cells. 2007;25:2118–2127. doi: 10.1634/stemcells.2006-0771. [DOI] [PubMed] [Google Scholar]
- 79.Tang YL, Tang Y, Zhang YC, Qian K, Shen L, Phillips MI. Improved graft mesenchymal stem cell survival in ischemic heart with a hypoxia-regulated heme oxygenase-1 vector. J Am Coll Cardiol. 2005;46:1339–1350. doi: 10.1016/j.jacc.2005.05.079. [DOI] [PubMed] [Google Scholar]
- 80.Duan HF, Wu CT, Wu DL, Lu Y, Liu HJ, Ha XQ, Zhang QW, Wang H, Jia XX, Wang LS. Treatment of myocardial ischemia with bone marrow-derived mesenchymal stem cells overexpressing hepatocyte growth factor. Mol Ther. 2003;8:467–474. doi: 10.1016/s1525-0016(03)00186-2. [DOI] [PubMed] [Google Scholar]
- 81.Song H, Kwon K, Lim S, Kang SM, Ko YG, Xu Z, Chung JH, Kim BS, Lee H, Joung B, Park S, Choi D, Jang Y, Chung NS, Yoo KJ, Hwang KC. Transfection of mesenchymal stem cells with the FGF-2 gene improves their survival under hypoxic conditions. Mol Cells. 2005;19:402–407. [PubMed] [Google Scholar]
- 82.Jo J, Nagaya N, Miyahara Y, Kataoka M, Harada-Shiba M, Kangawa K, Tabata Y. Transplantation of genetically engineered mesenchymal stem cells improves cardiac function in rats with myocardial infarction: benefit of a novel nonviral vector, cationized dextran. Tissue Eng. 2007;13:313–322. doi: 10.1089/ten.2006.0133. [DOI] [PubMed] [Google Scholar]
- 83.Matsumoto R, Omura T, Yoshiyama M, Hayashi T, Inamoto S, Koh KR, Ohta K, Izumi Y, Nakamura Y, Akioka K, Kitaura Y, Takeuchi K, Yoshikawa J. Vascular endothelial growth factor-expressing mesenchymal stem cell transplantation for the treatment of acute myocardial infarction. Arterioscler Thromb Vasc Biol. 2005;25:1168–1173. doi: 10.1161/01.ATV.0000165696.25680.ce. [DOI] [PubMed] [Google Scholar]
- 84.Khalil ME, Basher AW, Brown EJ, Jr, Alhaddad IA. A remarkable medical story: benefits of angiotensin-converting enzyme inhibitors in cardiac patients. J Am Coll Cardiol. 2001;37:1757–1764. doi: 10.1016/s0735-1097(01)01229-3. [DOI] [PubMed] [Google Scholar]
- 85.Hughes GC, Post MJ, Simons M, Annex BH. Translational physiology: porcine models of human coronary artery disease: implications for preclinical trials of therapeutic angiogenesis. J Appl Physiol. 2003;94:1689–1701. doi: 10.1152/japplphysiol.00465.2002. [DOI] [PubMed] [Google Scholar]
- 86.Post MJ, Laham R, Sellke FW, Simons M. Therapeutic angiogenesis in cardiology using protein formulations. Cardiovasc Res. 2001;49:522–531. doi: 10.1016/s0008-6363(00)00216-9. [DOI] [PubMed] [Google Scholar]
- 87.Malik DK, Baboota S, Ahuja A, Hasan S, Ali J. Recent advances in protein and peptide drug delivery systems. Curr Drug Deliv. 2007;4:141–151. doi: 10.2174/156720107780362339. [DOI] [PubMed] [Google Scholar]
- 88.Zhang G, Nakamura Y, Wang X, Hu Q, Suggs LJ, Zhang J. Controlled release of stromal cell-derived factor-1 alpha in situ increases c-kit+ cell homing to the infarcted heart. Tissue Eng. 2007;13:2063–2071. doi: 10.1089/ten.2006.0013. [DOI] [PubMed] [Google Scholar]
- 89.Segers VF, Tokunou T, Higgins LJ, MacGillivray C, Gannon J, Lee RT. Local delivery of protease-resistant stromal cell derived factor-1 for stem cell recruitment after myocardial infarction. Circulation. 2007;116:1683–1692. doi: 10.1161/CIRCULATIONAHA.107.718718. [DOI] [PubMed] [Google Scholar]
- 90.Webster KA. Programmed death as a therapeutic target to reduce myocardial infarction. Trends Pharmacol Sci. 2007;28:492–499. doi: 10.1016/j.tips.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 91.Potapova IA, Gaudette GR, Brink PR, Robinson RB, Rosen MR, Cohen IS, Doronin SV. Mesenchymal stem cells support migration, extracellular matrix invasion, proliferation, and survival of endothelial cells in vitro. Stem Cells. 2007;25:1761–1768. doi: 10.1634/stemcells.2007-0022. [DOI] [PubMed] [Google Scholar]
- 92.House SL, Melhorn SJ, Newman G, Doetschman T, Schultz Jel J. The protein kinase C pathway mediates cardioprotection induced by cardiac-specific overexpression of fibroblast growth factor-2. Am J Physiol Heart Circ Physiol. 2007;293:H354–365. doi: 10.1152/ajpheart.00804.2006. [DOI] [PubMed] [Google Scholar]
- 93.Ferdinandy P, Schulz R, Baxter GF. Interaction of cardiovascular risk factors with myocardial ischemia/reperfusion injury, preconditioning, and postconditioning. Pharmacol Rev. 2007;59:418–458. doi: 10.1124/pr.107.06002. [DOI] [PubMed] [Google Scholar]
- 94.Budas GR, Churchill EN, Mochly-Rosen D. Cardioprotective mechanisms of PKC isozyme-selective activators and inhibitors in the treatment of ischemia-reperfusion injury. Pharmacol Res. 2007;55:523–536. doi: 10.1016/j.phrs.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 95.Hanlon PR, Fu P, Wright GL, Steenbergen C, Arcasoy MO, Murphy E. Mechanisms of erythropoietin-mediated cardioprotection during ischemia-reperfusion injury: role of protein kinase C and phosphatidylinositol 3-kinase signaling. Faseb J. 2005;19:1323–1325. doi: 10.1096/fj.04-3545fje. [DOI] [PubMed] [Google Scholar]